Abstract
The current study investigated the main and interactive effects of emotion dysregulation and distress tolerance in relation to panic-relevant variables among daily smokers. The sample consisted of 172 adults (61.2% male; Mage = 31.58, SD = 11.51), who reported smoking an average of 15.99 cigarettes per day (SD = 10.00). Results indicated that both emotion dysregulation and distress tolerance were significantly related to interoceptive fear and agoraphobia. Additionally, emotion dysregulation, but not distress tolerance, was significantly related to anxiety sensitivity. All effects were evident above and beyond the variance accounted for by average cigarettes per day, tobacco-related physical illness, and panic attack history. The interaction between emotion dysregulation and distress tolerance significantly predicted interoceptive and agoraphobic fears as well as the cognitive component of anxiety sensitivity. Such findings underscore the importance of emotion dysregulation and distress tolerance in regard to panic-specific fear and expectancies about anxiety-related sensations among daily smokers.
Keywords: Anxiety, Anxiety Sensitivity, Distress Tolerance, Emotion Dysregulation, Smoking
Approximately 50% of daily smokers have a lifetime history of a psychiatric disorder with such persons consuming a disproportionately large percentage of the overall volume of cigarettes (Lasser et al., 2000). Although smoking has historically been studied in relation to many co-occurring psychopathological conditions (e.g., schizophrenia, depressive disorders; Ziedonis et al., 2008), comparatively less scholarly attention has been focused on anxiety and its disorders. This limitation is unfortunate, as anxiety disorders are among the most common psychiatric conditions. Moreover, some studies indicate rates of smoking are higher among those with anxiety disorders relative to many other psychiatric conditions as well as those with no psychiatric illness (McCabe et al., 2004).
Notably, some of the most robust relations documented between smoking and anxiety disorders have been evident for panic psychopathology (Zvolensky, Feldner, Leen-Feldner, & McLeish, 2005; Zvolensky, Schmidt, & Stewart, 2003). For example, epidemiological (Farrell et al., 2001), community (Hayward, Killen, & Taylor, 1989), and clinical (Pohl, Yeragani, Balon, Lycaki, & McBride, 1992) studies have found individuals with panic attacks are more apt to have a history of smoking compared to individuals without a panic attack history. Numerous other investigations suggest smoking often precedes and increases the subsequent risk for developing panic attacks and panic disorder with and without agoraphobia (Bernstein, Zvolensky, Schmidt, & Sachs-Ericsson, 2007; Breslau & Klein, 1999; Isensee, Wittchen, Stein, Höfler, & Lieb, 2003; Johnson et al., 2000; Zvolensky, Kotov, Antipova, & Schmidt, 2003). Additionally, panic psychopathology can impair success in quitting smoking. For example, Piper and colleagues (2010) recently found that smokers with a history of panic attacks, compared to smokers with no anxiety diagnoses, were significantly less likely to be abstinent at eight weeks and six months post-quit. These data collectively indicate clinically and statistically significant bi-directional relations between smoking and panic psychopathology.
Although there is an established link between smoking and panic psychopathology, little is known about the factors that are related to panic-relevant fear and expectancies about anxiety-related sensations among daily smokers (Ziedonis et al., 2008). This limitation is notable, as integrative models of smoking-panic co-occurrence and empirical evidence suggest that panic-relevant fear (degree of fear of internal and external events; Rapee, Craske, & Barlow, 1995) and expectancies about internal sensations (anxiety sensitivity or beliefs that anxiety-related sensations have negative personal consequences; Taylor, 1999) may each independently contribute to the tendency to be emotionally reactive to smoking-based cues (e.g., bodily sensations) and enhance motivation to smoke for emotion regulatory reasons (e.g., coping-motivated smoking in an effort to down regulate perceived or objective elevations in negative affect or hyperarousal; Zvolensky & Bernstein, 2005; Zvolensky et al., 2003). Specifically, smokers who perceive anxiety-related sensations as harmful or dangerous may be more apt to be fearful of, and emotionally reactive to, internal states that occur during smoking discontinuation. Consequently, a forward-feeding cycle may develop, whereby smoking is used as a coping strategy for managing aversive states in the short term, yet paradoxically confers longer-term risk for the development of panic symptoms. Thus, it is important to isolate the factors that are uniquely related to panic-relevant fear and expectancies about anxiety-related sensations among this population, in order to more effectively target these variables in specialized intervention programs for smokers with co-occurring vulnerabilities for, or existing problems with, panic psychopathology.
Emotion dysregulation represents a promising construct of increasing scholarly interest in anxiety psychopathology and substance use disorder comorbidity research and clinical work (Barlow, Allen, & Choate, 2004; Bonn-Miller, Vujanovic, & Zvolensky, 2008; Kashdan & Steger, 2006; Orsillo & Roemer, 2005). Emotion dysregulation reflects difficulties in the self-regulation of affective states and in self-control over affect-driven behaviors (Carver, Lawrence, & Scheier, 1996). Although there has historically been limited work on emotion dysregulation and anxiety psychopathology, recent studies have found that higher levels of emotion dysregulation are generally related to more frequent and intense anxiety symptoms (Tull, Barrett, McMillan, & Roemer, 2007; Tull & Roemer, 2007; Vujanovic, Zvolensky, & Bernstein, 2008). That is, emotion dysregulation is not-specific to particular anxiety phenotypes or symptoms, but rather, is broadly associated with various types of anxiety symptoms. However, the explanatory utility of emotion dysregulation has not yet been explored in relation to panic-specific fear or expectancies about anxiety-related sensations among daily smokers.
A second construct potentially relevant to bridging gaps in understanding about anxiety-tobacco comorbidity is distress tolerance (Brown, Lejuez, Kahler, Strong, & Zvolensky, 2005). Distress tolerance reflects the perceived and/or actual behavioral capacity to withstand exposure to aversive or threatening experiential states (e.g., negative emotions, uncomfortable physical sensations; Leyro, Zvolensky, & Bernstein, 2010). Distress tolerance has been conceptualized as: (a) the perceived capacity to withstand aversive emotional or physical states (assessed via self-report measures; e.g., Distress Tolerance Scale [DTS; Simons & Gaher, 2005]), and (b) the behavioral act(s) of withstanding distressing internal states elicited by some type of stressor (assessed via the latency to discontinue distressing tasks; e.g., breath-holding task; Zvolensky, Leyro, Bernstein, & Vujanovic, 2011). In fact, numerous studies indicate that there is a minimal association between these two distress tolerance classes (Bernstein, Marshall, & Zvolensky, in press; Marshall-Berenz, Vujanovic, Bonn-Miller, Bernstein, & Zvolensky, 2010; McHugh et al., in press; Leyro, Zvolensky, & Bernstein, 2010). Within the area of smoking research, much of existing work has examined behavioral measures of distress tolerance (e.g., breath-holding duration) in relation to smoking relevant outcomes. Here, past work indicates that lower levels of behavioral distress tolerance are related to problems in abstaining from smoking (e.g., Brown et al., 2009). Other related work suggests that distress tolerance may be an important, yet underrecognized, explanatory factor in terms of emotional reactivity to interoceptive distress (Schmidt, Mitchell, Keough, & Riccardi, 2010). For example, lower levels of perceived distress tolerance for emotional distress and physical stress, and a lesser ability to withstand acute episodes of emotional stress, are significantly related to increased anxiety symptoms and panic attacks (Boelen & Reijntjes, 2009; Bonn-Miller, Zvolensky, & Bernstein, 2009; Daughters et al., 2009; Marshall, Zvolensky, Vujanovic, Gregor, Gibson, & Leyro, 2008) as well as escape behavior in response to somatic arousal (Asmundson & Stein, 1994; Marshall et al., 2008; Telch, Jacquin, Smits, & Powers, 2003). There has not yet been a direct test, however, of the relation between behavioral measures of distress tolerance and panic-specific fear or expectancies about anxiety-related sensations, in general, or among a tobacco using population, in particular.
Beyond main effects for emotion dysregulation and distress tolerance among daily smokers, there is apt to be clinically-relevant interplay between these factors. Indeed, smokers with higher levels of emotion dysregulation and lower tolerance for interoceptive distress (e.g., aversive physical sensations) may be more likely to manifest greater panic-specific fear and expectancies about anxiety-related sensations. That is, lower levels of tolerance for internal stress (e.g., bodily perturbation) may moderate the relation between emotion dysregulation and panic-specific fear and expectancies about anxiety-related sensations. Specifically, smokers experiencing greater levels of emotion dysregulation, who cannot as effectively tolerate such distress, may interpret distressing symptoms as more severe, thereby increasing reactivity to such symptoms and increasing panic-specific fear (interoceptive fear and agoraphobic fear) and future expectancies about internal sensations (anxiety sensitivity). Conversely, higher levels of an ability to tolerate emotion dysregulation may attenuate the relative risk for more severe panic-specific fear and expectancies about the negative consequences of anxiety-related sensations.
The current study investigated the main and interactive effects of emotion dysregulation and a behavioral measure of distress tolerance (breath-holding duration) in relation to panic-specific fear (interoceptive and agoraphobic fear) and expectancies about anxiety-related sensations (anxiety sensitivity) among a daily smoking population. There were three interrelated sets of hypotheses that were globally driven by the perspective that higher levels of an ability to tolerate emotion dysregulation may attenuate the relative risk for more severe panic-specific fear as well as heightened sensitivity to the physical and cognitive consequences of anxiety-related symptoms among daily smokers. First, it was hypothesized that the main effect of emotion dysregulation would be significantly related to specific fears and expectancies about anxiety-related sensations, as past work has suggested this construct is not specific to one disorder (Tull et al., 2007). Second, it was hypothesized that the main effect of a behavioral index of distress tolerance (breath-holding duration) would be significantly (negatively) related only to the panic-specific fear criterion variables (interoceptive and agoraphobic fear) and the physical and cognitive indices of anxiety sensitivity; thus, it would showcase explanatory specificity to panic-relevant indices (Schmidt et al., 2010). Finally, it was hypothesized that the significant main effects would be qualified by a significant interaction between emotion dysregulation and distress tolerance in terms of only panic-specific fear as well as the physical and cognitive indices of anxiety sensitivity. The hypothesized significant effects were expected to be evident above and beyond the variance accounted for by lifetime panic attack history, daily smoking rate, and lifetime history of tobacco-related medical illness; factors known to covary with emotion dysregulation and distress tolerance (Schmidt et al., 2010; Tull et al., 2007).
1. Method
1.1 Participants
Participants included 172 adult daily smokers (61.2% male; Mage = 31.58, SD = 11.51), who responded to advertisements (e.g. flyers, newspaper ads, radio announcements) to participate in a study examining the efficacy of a 4-session smoking-based behavioral intervention program focused on emotional vulnerability in comparison to standard pharmacological and psychosocial care. In terms of ethnic background, 84.8% of participants identified as Caucasian, 11.4% identified as African-American, 1.1% identified as Hispanic, 1.1% identified as Asian, and 1.6% identified as “other.” Participants reported smoking an average of 15.99 cigarettes per day (SD = 10.00), smoking their first cigarette at 14.37 years of age (SD = 3.10), and smoking regularly at 16.74 years of age (SD = 3.12). The average score on the Fagerstrom Test for Nicotine Dependence (FTND; Heatherton, Kozlowski, Frecker & Fagerstrom, 1991) was 5.01 (SD = 2.34), indicating moderate overall levels of nicotine dependence.
Participants were deemed eligible for enrollment in the present study if they reported smoking an average of 8 or more cigarettes daily for at least one year, provided a Carbon Monoxide breath sample of 10 ppm or higher at baseline session, and were at least 18 years old. Participants were excluded based on the following criteria: (1) current suicidality or homicidality; (2) endorsement of current or past psychotic-spectrum symptoms via structured interview screening; (3) limited mental competency and inability to provide informed, voluntary, written consent; and (4), current use of pharmacotherapy for smoking cessation not provided by researchers during quit attempt.
1.2 Measures
Structured Clinical Interview-Non-Patient Version for DSM-IV (SCID-N/P; First, Spitzer, Gibbon, & Williams, 1994)
Diagnostic assessments were conducted using the SCID-I-NP (Non-Patient Version; First et al., 1994). SCID-I-NP interviews were administered by trained research assistants or doctoral level staff and supervised by independent doctoral-level professionals. Interviews were audio-taped and the reliability of a random selection of 12.5% of interviews were checked (MJZ) for accuracy; no cases of (diagnostic coding) disagreement were noted. The SCID-N/P was employed to document psychopathology for the inclusionary/exclusionary criteria and history of panic attacks.
The Medical Screening Form (MSF; Scheftner & Endicott, 1984)
The MSF is a structured instrument administered by trained interviewers to assess lifetime medical history (Ormel, VonKorff, Ustun, Pini, 1994). This interview has excellent psychometric properties and has been extensively used successfully in previous work for screening physical health problems and medication usage (e.g., Hays, Kallich, Mapes, Coons, & Carter, 1994). In the present study, as in past work (Leventhal, Zvolensky, & Schmidt, in press), a total score was generated by summing the number of endorsed lifetime history of tobacco-related medical problems. Specifically, participants who reported being diagnosed with heart problems, hypertension, respiratory disease, or asthma on this questionnaire were coded as having a tobacco-related disease.
The Smoking History Questionnaire (SHQ; Brown, Lejuez, Kahler, & Strong, 2002)
The SHQ is a self-report questionnaire used to assess smoking history and pattern. The SHQ includes items pertaining to smoking rate, age of onset of smoking initiation, and years of being a daily smoker. The SHQ has been successfully used in previous studies as a measure of smoking history and pattern (Zvolensky, Lejuez, Kahler, & Brown, 2004). The current investigation utilized the following variables from the SHQ: average number of cigarettes smoked per day, age at first cigarette, and age at onset of regular (daily) cigarette smoking.
Fagerstrom Test for Nicotine Dependence (FTND; Heatherton et al., 1991)
The FTND is well-established six-item scale designed to assess gradations in tobacco dependence. This measure exhibits good internal consistency, positive relations with key smoking variables (e.g. salivary cotinine; Heatherton et al., 1991; Payne, Smith, McCracken, McSherry, & Anthony, 1994), and high test-retest reliability (Pomerleau, Carton, Lutzke, Flessland, & Pomerleau, 1994).
Carbon Monoxide
Biochemical verification of smoking status was completed by Carbon Monoxide (CO) analysis of breath samples (10 ppm cutoff; Cocores, 1993). Expired air CO levels were assessed using a CMD/CO Carbon Monoxide Monitor (Model 3110; Spirometrics, Inc.).
Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004)
The DERS was used to assess emotion dysregulation. The scale consists of 36 items, which comprise six subscales, including: (a) nonacceptance of emotional responses, (b) difficulties engaging in goal-directed activities, (c) impulse control difficulties, (d) lack of emotional awareness, (e) limited access to emotion regulation strategies, and (f) lack of emotional clarity.Items are rated on a 5-point Likert-type scale ranging from 1 (“almost never”) to 5 (“almost always”). Consistent with past work (Gratz & Roemer, 2004), the DERS-total score demonstrated good internal consistency in the current sample (Cronbach α = .83). As in past work (Gonzalez, Zvolensky, Vujanovic, Leyro, & Marshall, 2008; Vujanovic et al., 2008), the DERS-total score was employed as a global index of the inability to effectively modulate emotional states.
Breath-Holding Duration
Breath-holding duration was used as a physical challenge procedure designed to elicit panic-like symptoms (e.g., dizziness, racing heart). This test involves informing each participant to exhale completely, and then, hold his/her breath for as long as possible. The duration of breath-holding is timed by an experimenter in the total number of seconds. As in past work (Asmundson & Stein, 1994), breath-holding duration was assessed during two consecutive trials; these trials were highly interrelated (r = .81, p < .001). Due to the high interrelation between the breath-holding trials, as in past work (Brown et al., 2009), only the second trial was used. In the present study, breath-holding duration was employed as a behavioral index of distress tolerance as persistence on the task assessed the ability to tolerate aversive internal states (Brown, Lejuez, Kahler, Strong, & Zvolensky, 2005). Here, it should be noted that this index of distress tolerance differs from the global measurement of emotion dysregulation in that breath-holding duration measures the physical or actual capacity to withstand internal discomfort whereas emotion dysregulation reflects perceived abilities to effectively modulate emotional states.
Anxiety Sensitivity Index (ASI; Reiss, Peterson, Gursky, & McNally, 1986)
The ASI is a 16-item measure in which respondents indicate, on a 5-point Likert-type scale (0 = “very little” to 4 = “very much”), the degree to which they are concerned about possible negative consequences of anxiety symptoms (e.g., “It scares me when my heart beats rapidly”). The ASI is unique from, and demonstrates incremental predictive validity relative to, trait anxiety (McNally, 2002) and negative affectivity (Zvolensky et al., 2003). In the present investigation, the three ASI subscale scores (physical, cognitive, and social concerns) were employed (range of Cronbach α's = .76 – .90 in the current sample).
Albany Panic and Phobia Questionnaire (APPQ; Rapee, Craske, & Barlow, 1995)
The APPQ is a 27-item self-report questionnaire with a 9-point Likert-type scale ranging from 0 (“no fear”) to 8 (“extreme fear”). Three subscales are generated from the items on the APPQ: interoceptive fear, agoraphobia, and social situational fear (Rapee et al., 1995). The APPQ has demonstrated good to excellent internal consistency and construct validity in past work (Brown, White & Barlow, 2005). In the present study, all three subscales were employed as primary indices of panic-specific (interoceptive fear and agoraphobia) and non-panic specific fear (social situational fear; range of Cronbach α's = .87 – .91 in the current sample).
1.3 Procedure
The current report is based on analyses of data that have not been published or presented previously and were collected during the larger study’s baseline assessment session. The baseline session took place prior to randomization and initiation of the intervention. At the laboratory, participants first completed informed consent, and then were administered the SCID-N/P and completed a baseline battery of self-report and behavioral instruments. Thereafter, participants were paid for their participation.
2. Results
2.1 Data Analytic Strategy
Zero-order correlations were first obtained to examine associations between the predictor and criterion variables. Thereafter, six separate hierarchical regressions were completed. Criterion variables in the hierarchical regression analyses included: 1) ASI-physical; 2) ASI-cognitive; 3) ASI-social concerns; 4) APPQ-interoceptive fear; 5) APPQ-agoraphobia; and, 6) APPQ-social situational fear. The main effects of average number of cigarettes smoked per day (mean-centered), endorsement of tobacco-related medical problems (mean-centered), and SCID-diagnosed panic attack history (dummy coded: no = 1, yes = 2) were entered as a block at step 1. These theoretically-relevant covariates were chosen on an a priori basis as factors that could possibly account for any observed relations between emotion dysregulation and distress tolerance and the criterion variables (Cohen & Cohen, 1983). At step 2, the main effects (mean-centered) of emotion dysregulation (DERS-total) and distress tolerance (breath-holding duration) were simultaneously entered. At step 3, the interaction (mean-centered) term of DERS-total by breath-holding duration was entered. When significant interaction effects emerged, simple slopes were calculated to test whether emotion dysregulation impacted the criterion variables at different levels of distress tolerance (Aiken & West, 1991).
2.2 Zero-Order (or Bi-variate) Correlations for Theoretically-Relevant Variables
Please see Table 1 for a summary of zero-order (or bivariate, as applicable) correlations and descriptive data. As expected, DERS-total was significantly positively correlated with the physical, cognitive, and social concerns subscales of the ASI (range of r’s = .49 – .65, p < .001). Additionally, DERS-total was significantly positively correlated with the agoraphobia (r = .53, p < .001), interoceptive fear (r = .47, p < .001), and social situational fear (r = .67, p < .001) subscales of the APPQ.
Table 1.
Descriptive Data and Zero-Order Relations among Theoretically-Relevant Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Mean or % (SD) |
Observed Range |
|
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. CPD | - | −.02 | −.02 | −.17* | .22** | .15* | .19* | .17* | .19* | .37** | .24** | 15.99 (10.00) | 1–60 |
| 2. MSF | - | −.06 | −.02 | −.02 | .04 | −.06 | .04 | .00 | −.00 | −.10 | 0.28 (0.48) | 0–2 | |
| 3. PA Status | - | −.08 | .29** | .38** | .39** | .35** | .31** | .29** | .26** | 51.7% (Yes) | -- | ||
| 4. BH | - | −.16* | −.16* | −.15* | −.16* | −.27** | −.31** | −.20** | 52.71 (25.78) | 3–130 | |||
| 5. DERS- Total | - | .49** | .65** | .53** | .53** | .47** | .67** | 78.10 (24.04) | 37–156 | ||||
| 6. ASI- Physical | - | .76** | .71** | .52** | .52** | .43** | 9.35 (6.49) | 0–30 | |||||
| 7. ASI- Cognitive | - | .69** | .57** | .53** | .52** | 3.15 (3.21) | 0–16 | ||||||
| 8. ASI- Social | - | .44** | .44** | .47** | 6.18 (3.19) | 0–15 | |||||||
| 9. APPQ- Agoraphobia | - | .70** | .62** | 8.74 (10.83) | 0–64 | ||||||||
| 10. APPQ- Interoceptive | - | .50** | 6.60 (9.01) | 0–54 | |||||||||
| 11. APPQ- Social | - | 16.82 (14.03) | 0–69 |
Note:
p < .05,
p < .01.
CPD = Smoking rate from Smoking History Questionnaire (SHQ; Brown et al., 2002); MSF = Total number of endorsed medial problem from the Medical Screening Form (MSF; Scheftner & Endicott, 1984); PA Status = Two-year history of unexpected, nonclinical panic attacks, dummy-coded (no=1, yes=2) per Structured Clinical Interview-Non-Patient Version for DSM-IV (SCID-N/P; First et al., 1995); BH = Breath-holding duration (second trial measured in seconds); DERS-Total = Difficulties in Emotion Regulation Scale total score (DERS; Gratz & Roemer, 2004); ASI-Cognitive = Anxiety Sensitivity Index, Cognitive subscale (ASI; Reiss et al., 1986); ASI-Physical = Anxiety Sensitivity Index, Physical subscale (ASI; Reiss et al., 1986); ASI-Social = Anxiety Sensitivity Index, Social Concerns subscale (ASI; Reiss et al., 1986); APPQ-Agoraphobia = Albany Panic and Phobia Questionnaire, Agoraphobia subscale score (APPQ; Rapee et al., 1994); APPQ-Interoceptive = Albany Panic and Phobia Questionnaire, Interoceptive Fear subscale score (APPQ; Rapee et al., 1994); APPQ-Social = Albany Panic and Phobia Questionnaire, Social Situational Fear subscale score (APPQ; Rapee et al., 1994).
Also as expected, analyses revealed that breath-holding duration was significantly negatively correlated with the three ASI subscales (range of r’s = −.15 – −.16, p < .05). Further, breath-holding duration was significantly negatively correlated with the three APPQ subscales (range of r’s = −.20 – −.31, p < .01).
Finally, DERS-total was significantly negatively correlated to breath-holding duration (r = −.16, p < .05; 2.5% shared variance); whereas, the ASI subscales were significantly positively related to the APPQ subscales (range of r's = .43 – .57; range of shared variance = 18% – .32%).
2.3 Hierarchical Regression Analyses
Analysis for the ASI-physical subscale revealed that the predictor variables accounted for 33.1% of the overall variance [F(6, 173) = 13.78, p < .001]. Step 1 of the model accounted for 16.9% of the variance, with average cigarettes per day (t = 2.14, β = .15, p < .05) and panic attack history (t = 5.48, β = .38, p < .001) each being significant predictors. Step 2 of the model accounted for an additional 15.3% of the variance, with DERS-total (t = 5.94, β = .41, p < .001) being the only significant predictor. Finally, Step 3 accounted for a non-significant 0.9% of the variance (t = −1.50, β = −.10, p = ns; see Table 2).
Table 2.
Summary of Hierarchical Regression Analyses
| ΔR2 |
t (each predictor) |
β | sr2 | p | |
|---|---|---|---|---|---|
| Criterion Variable: ASI-Physical | |||||
| Step 1 | .17 | ||||
| CPD | 2.14 | .15 | .02 | <.05 | |
| MSF | 1.00 | .07 | .00 | ns | |
| PA Status | 5.48 | .38 | .15 | <.001 | |
| Step 2 | .15 | ||||
| BH | −.79 | −.05 | .00 | ns | |
| DERS-Total | 5.94 | .41 | .14 | <.001 | |
| Step 3 | .01 | ||||
| DERS-Total X BH | −1.50 | −.10 | .01 | ns | |
| Criterion Variable: ASI-Cognitive | |||||
| Step 1 | .18 | ||||
| CPD | 2.59 | .18 | .03 | <.01 | |
| MSF | −.41 | −.03 | .00 | ns | |
| PA Status | 5.61 | .39 | .15 | <.001 | |
| Step 2 | .31 | ||||
| BH | −.29 | −.02 | .00 | ns | |
| DERS-Total | 10.12 | .60 | .31 | <.001 | |
| Step 3 | .01 | ||||
| DERS-Total X BH | −2.12 | −.12 | .01 | <.05 | |
| Criterion Variable: ASI-Social | |||||
| Step 1 | .15 | ||||
| CPD | 2.36 | .17 | .03 | <.05 | |
| MSF | .85 | .06 | .00 | ns | |
| PA Status | 4.97 | .35 | .12 | <.001 | |
| Step 2 | .18 | ||||
| BH | −.90 | −.06 | .00 | ns | |
| DERS-Total | 6.57 | .45 | .17 | <.001 | |
| Step 3 | .00 | ||||
| DERS-Total X BH | −0.81 | −.05 | .00 | ns | |
| Criterion Variable: APPQ-Agoraphobia | |||||
| Step 1 | .14 | ||||
| CPD | 2.89 | .21 | .04 | <.01 | |
| MSF | .22 | .02 | .00 | ns | |
| PA Status | 4.37 | .31 | .10 | <.001 | |
| Step 2 | .20 | ||||
| BH | −2.78 | −.18 | .03 | <.01 | |
| DERS-Total | 6.07 | .42 | .15 | <.001 | |
| Step 3 | .07 | ||||
| DERS-Total X BH | −4.27 | −.27 | .07 | <.001 | |
| Criterion Variable: APPQ-Interoceptive | |||||
| Step 1 | .23 | ||||
| CPD | 5.70 | .39 | .15 | <.001 | |
| MSF | .26 | .02 | .00 | ns | |
| PA Status | 4.32 | .29 | .09 | <.001 | |
| Step 2 | .14 | ||||
| BH | −3.28 | −.21 | .04 | <.001 | |
| DERS-Total | 4.53 | .30 | .08 | <.001 | |
| Step 3 | .04 | ||||
| DERS-Total X BH | −3.32 | −.21 | .04 | <.001 | |
| Criterion Variable: APPQ-Social | |||||
| Step 1 | .13 | ||||
| CPD | 3.34 | .24 | .06 | <.001 | |
| MSF | −1.08 | −.08 | .01 | ns | |
| PA Status | 3.55 | .26 | .07 | <.001 | |
| Step 2 | .34 | ||||
| BH | −1.45 | −.09 | .01 | ns | |
| DERS-Total | 9.77 | .61 | .31 | <.001 | |
| Step 3 | .00 | ||||
| DERS-Total X BH | −.71 | −.04 | .00 | ns | |
Note: β = Standardized beta weight provided for hierarchical multiple regression; sr2 = squared partial correlation; CPD = Smoking rate from Smoking History Questionnaire (SHQ; Brown et al., 2002); MSF = Total number of endorsed medial problem from the Medical Screening Form (MSF; Scheftner & Endicott, 1984); PA Status = Two-year history of unexpected, nonclinical panic attacks, dummy-coded (no=1, yes=2) per Structured Clinical Interview-Non-Patient Version for DSM-IV (SCID-N/P; First et al., 1995); BH = Breath-holding duration (second trial measured in seconds); DERS-Total = Difficulties in Emotion Regulation Scale total score (DERS; Gratz & Roemer, 2004); ASI-Cognitive = Anxiety Sensitivity Index, Cognitive subscale (ASI; Reiss et al., 1986); ASI-Physical = Anxiety Sensitivity Index, Physical subscale (ASI; Reiss et al., 1986); ASI-Social = Anxiety Sensitivity Index, Social Concerns subscale (ASI; Reiss et al., 1986); APPQ-Agoraphobia = Albany Panic and Phobia Questionnaire, Agoraphobia subscale score (APPQ; Rapee et al., 1994); APPQ-Interoceptive = Albany Panic and Phobia Questionnaire, Interoceptive Fear subscale score (APPQ; Rapee et al., 1994); APPQ-Social = Albany Panic and Phobia Questionnaire, Social Situational Fear subscale score (APPQ; Rapee et al., 1994); DERS-Total X BH = BH and DERS-total interaction term.
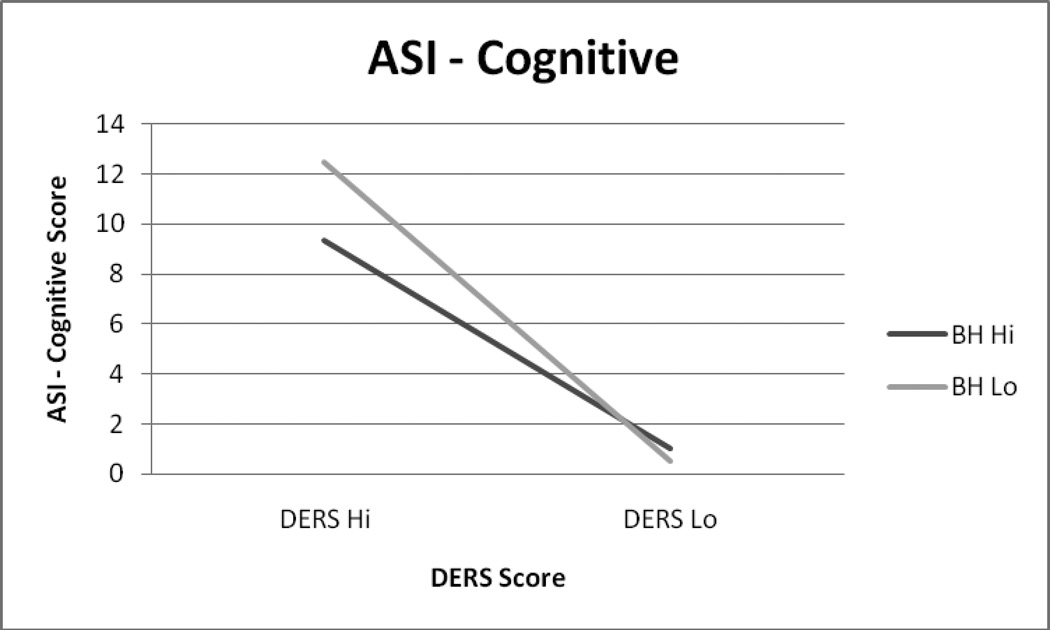
Analyses for the ASI-cognitive subscale revealed that the predictor variables accounted for 51.1% of the overall variance [F(6, 173) = 29.12, p < .001]. Step 1 of the model accounted for 18.4% of the variance, with average cigarettes per day (t = 2.59, β = .18, p < .01) and panic attack history (t = 5.61, β = .39, p < .001) each being significant predictors. Step 2 of the model accounted for an additional 31.4% of the variance, with DERS-total (t = 10.12, β = .60, p < .001) being the only significant predictor. Finally, Step 3 accounted for an additional 1.3% of the variance, with the interaction term of DERS-total by breath-holding duration being a significant predictor (t = −2.12, β = −.12, p < .05; see Table 2). Here, simple slope analyses revealed that higher levels of emotion dysregulation was significantly related to the ASI-cognitive subscale at both low (b = .09, t = 9.19, p < .001) and high levels (b = .06, t = 5.15, p < .001) of distress tolerance (breath-holding duration).
Analyses for the ASI-social subscale revealed that the predictor variables accounted for 33.7% of the overall variance [F(6, 173) = 14.18, p < .001]. Step 1 of the model accounted for 15.1% of the variance, with average cigarettes per day (t = 2.36, β = .17, p < .05) and panic attack history (t = 4.97, β = .35, p < .001) each being significant predictors. Step 2 of the model accounted for an additional 18.4% of the variance, with DERS-total (t = 6.57, β = .45, p < .001) being the only significant predictor. Finally, Step 3 accounted for a non-significant 0.3% of the variance (t = −0.81, β = −.05, p = ns; see Table 2).
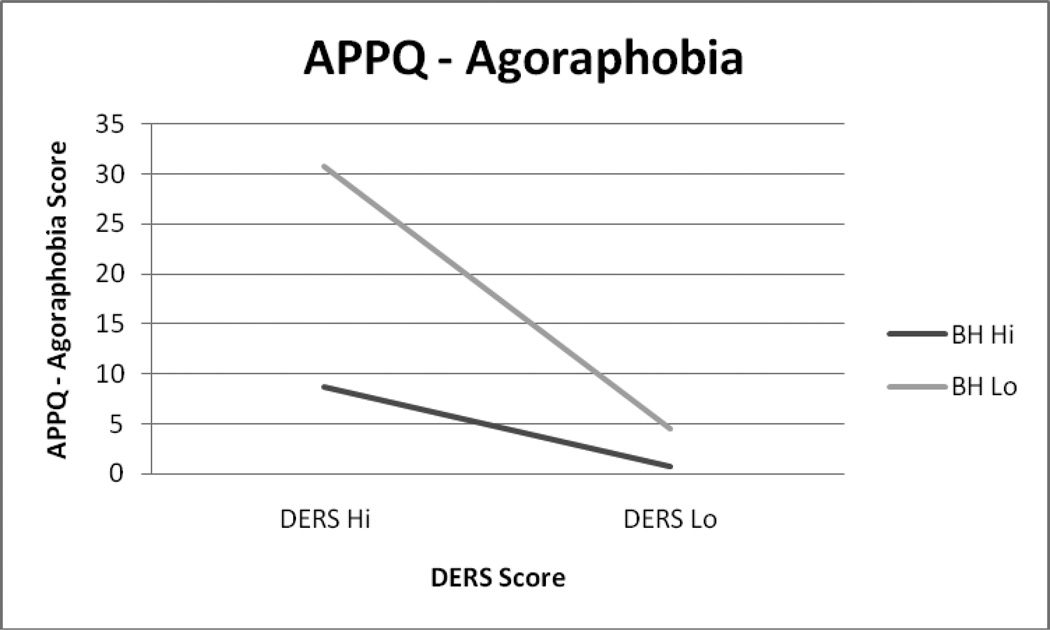
Regarding the APPQ-agoraphobia subscale, results indicated that the predictor variables accounted for 40.5% of the overall variance [F(6, 171) = 18.71, p < .001]. Step 1 of the model accounted for 13.8% of the variance, with average cigarettes per day (t = 2.89, β = .21, p < .01) and panic attack history (t = 4.37, β = .31, p < .001) both being significant predictors. Step 2 of the model accounted for an additional 20.1% of the variance, with breath-holding duration (t = −2.78, β = −.18, p < .01) and DERS-total (t = 6.07, β = .42, p < .001) each being significant predictors. Finally, the Step 3 interaction term of DERS-total by breath-holding duration accounted for a statistically significant additional 6.6% of the variance of the APPQ-agoraphobia subscale (t = −4.27, β = −.27, p < .001; see Table 2). Here, simple slope analyses revealed that emotion dysregulation was more strongly related to the APPQ-agoraphobia subscale among individuals endorsing low (but not high) levels of distress tolerance (breath-holding duration; b = .29, t = 7.63, p < .001).
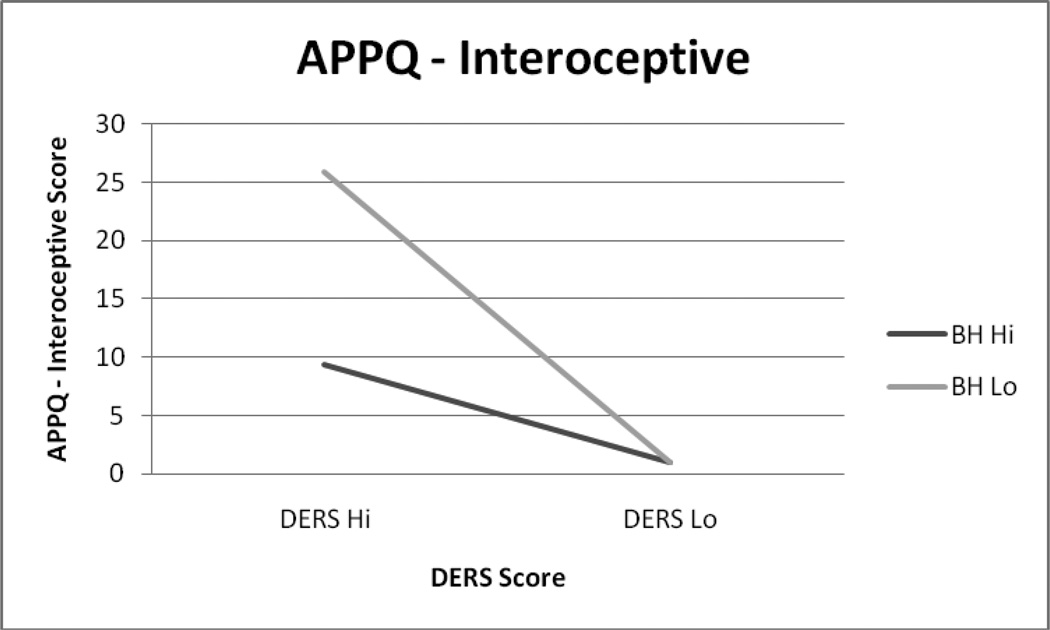
Regarding the APPQ-interoceptive fear subscale, results indicated that the predictor variables accounted for 40.8% of the overall variance [F(6, 171) = 18.94, p < .001]. Step 1 of the model accounted for 23% of the variance, with average cigarettes per day (t = 5.70, β = .39, p < .001) and panic attack history (t = 4.32, β = .29, p < .001) both being significant predictors. Step 2 of the model accounted for an additional 13.8% of the variance, with breath-holding duration (t = −3.28, β = −.21, p < .001) and DERS-total score (t = 4.53, β = .30, p < .001) each being significant predictors. Finally, Step 3 accounted for an additional 4% of the variance, with the interaction term being a significant predictor of the APPQ-interoceptive fear subscale (t = −3.32, β = −.21, p < .001; see Table 2). Once again, simple slope analyses revealed that emotion dysregulation was more strongly related to the APPQ-interoceptive fear subscale among individuals endorsing low (but not high) levels of distress tolerance (breath-holding duration; b = .18, t = 5.71, p < .001).
Finally, analyses for the APPQ-social situational fear subscale revealed that the predictor variables accounted for 46.7% of the overall variance [F(6, 171) = 24.05, p < .001]. Step 1 of the model accounted for 13% of the variance, with average cigarettes per day (t = 3.34, β = .24, p < .001) and panic attack history (t = 3.55, β = .26, p < .001) both being significant predictors. Step 2 of the model accounted for an additional 33.5% of the variance, with DERS-total (t = 9.77, β = .61, p < .001) being the only significant predictor. Finally, Step 3 accounted for a non-significant 0.2% of the variance (t = −.71, β = −.04, p = ns; see Table 2).
2.4 Mapping the Form of the Observed Significant Interactions
The form of the statistically significant interactions were then subsequently examined per recommendations from Cohen and Cohen (1983). First, based on recommendations of Cohen and Cohen (1983; pp. 323, 419), the form of each interaction was examined by inserting specific values for each predictor variable into the regression equation associated with the described analyses. As evident in Figure 1, individuals endorsing higher levels of DERS-total and shorter duration of breath-holding reported the highest levels on the ASI-cognitive subscale. Interestingly, among individuals endorsing low levels of DERS-total, virtually no difference was observed between breath-holding duration (low/high), in terms of the reported levels on the AS-cognitive subscale. Generally similar patterns of findings were observed for the APPQ-agoraphobia and -interoceptive fear subscales (see Figures 1–3).
Figure 1.
ASI-Cognitive score as a function of the interaction between DERS-Total and Breath-Holding Duration among participants 0.5 SD above and/or below the mean.
Figure 3.
APPQ-Interoceptive score as a function of the interaction between DERS-Total and Breath-Holding Duration among participants 0.5 SD above and/or below the mean.
3. Discussion
First, as hypothesized, the main effect of emotion dysregulation was significantly incrementally related to all of the criterion variables. The size of the observed effects were generally medium to large (Cohen, 1988; see Table 2). These findings are broadly consistent with past work that has shown emotion dysregulation is generally related to more frequent and intense anxiety symptoms (i.e., it is non-specific to particular anxiety phenotypes or symptoms; Tull et al., 2007; Tull & Roemer, 2007; Vujanovic et al., 2008) and extends this program of research in regard to numerous indices of specific types of fear. Importantly, the observed effects cannot be attributed to smoking rate, tobacco-related physical illnesses, or a history of panic attacks. Thus, emotion dysregulation evidences a strong and consistent relation to specific types of fears among a tobacco using population.
Second, as hypothesized, the main effect of distress tolerance (as measured by breath-holding duration) was significantly related to agoraphobic and interoceptive fear, but not social fears, among daily smokers. Yet, contrary to prediction, distress tolerance was not significantly incrementally related to any of the anxiety sensitivity subscales. This finding is somewhat surprising given: (a) the ASI subscale scores were significantly correlated with the APPQ subscales (range of shared variance: 30% – 44%); and, (b) the range of variance accounted for by the covariates was generally similar across the criterion variables (see Table 2). However, these results are consistent with observations that distress tolerance and anxiety sensitivity are not perfectly coupled, but rather, represent distinct constructs (Keough, Riccardi, Timpano, Mitchell, & Schmidt, 2010; Zvolensky, Vujanovic, Bernstein, & Leyro, 2010).
In the present study, the results suggest distress tolerance may be related to panic-specific fears but not expectancies about the negative consequences of anxiety-related sensations (anxiety sensitivity) among daily smokers. Thus, distress tolerance, as measured by breath-holding duration, may be more related to fear than expectancies about aversive internal states per se. Such work is generally consistent with research indicating that lower levels of behavioral measures of distress tolerance (e.g., breath-holding duration) are related to higher rates of panic attacks (Marshall et al., 2008), and extends this line of work in regard to panic-specific fear variables. Similar to the emotion dysregulation effects, the distress tolerance effects were evident above and beyond the variance accounted for by smoking rate, tobacco-related physical illnesses, and panic attacks.
Third, as hypothesized, the interaction between emotion dysregulation and distress tolerance significantly predicted rates of panic-relevant fear in daily smokers above and beyond the individual main effects. The form of the interactions indicated that higher levels of emotion dysregulation combined with lower levels of distress tolerance significantly predicted higher levels of panic-relevant fear (agoraphobia and interoceptive fear). Here, when examining the simple slopes of these significant interactions, we found that emotion dysregulation was more strongly related to panic-specific fear at low, but not high, levels of distress tolerance. Specifically, as levels of distress tolerance decreased the relation between emotion dysregulation and panic-specific fears increased (became more positive).
Partially consistent with study hypotheses, the interaction between emotion dysregulation and distress tolerance only significantly predicted the anxiety sensitivity – cognitive subscale. Simple slope analyses revealed that emotion dysregulation was significantly related to the cognitive facet of anxiety sensitivity at both high and low levels of distress tolerance. Yet, the interaction between emotion dysregulation and distress tolerance did not significantly predict the anxiety sensitivity - physical subscale. This finding is somewhat surprising given that our measure of distress tolerance (breath-holding duration) was designed to assess the behavioral capacity to withstand aversive physical states. However, given the relatively low correlations observed between various indices of distress tolerance (e.g., self-report vs. behavioral; Bernstein, Marshall, & Zvolensky, in press; Marshall et al., 2008; McHugh et al., in press), it could be that other facets (e.g., perceived) distress tolerance are more relevant to understanding expectancies regarding the physical consequences of anxiety-related sensations.
There are a number of interpretative caveats that warrant consideration in the interpretation of the present findings and highlight useful targets for future research. First, the present sample is limited in that it is comprised of a relatively homogenous (e.g., primarily Caucasian) group of adult smokers who volunteered to participate in the study for monetary reward. To rule out potential self-selection bias among persons with these characteristics and increase the generalizability of these findings, it will be important for researchers to draw from other populations and utilize recruitment tactics other than those used in the present study. Second, it may be helpful for future work to employ prospective methodologies to trace changes in the criterion variables over time. This information will help in clarifying the relative stability of the observed effects and could inform prevention efforts. Third, we sampled community-recruited daily smokers. Inspection of the level of nicotine dependence among this sample was relatively low. To enhance the generalizability of the results, it may therefore be useful to replicate and extend the present findings to heavier smoking samples and evaluate if similar patterns emerge. And finally, the present study was correlational in nature. It is therefore necessarily limited because it cannot shed light on processes over time or isolate causal relations between variables.
Overall, the results of the current study broadly highlight the importance of emotion dysregulation and distress tolerance in terms of better understanding panic-relevant fear and expectancies about anxiety-related sensations. Past work suggests that increased fears of, and expectancies about, panic-related symptoms are theoretically and empirically linked to the development and maintenance of panic psychopathology, particularly among daily smokers (Zvolensky & Berstein, 2005). Such research underscores the importance of focusing greater attention on factors that may place smokers at greater risk for the development of anxiety-related fears and expectancies in an effort to prevent panic-related problems. Likewise, addressing emotional dysregulation and distress tolerance may be important to address in terms of aiding efforts to quit smoking (Zvolensky & Bernstein, 2005). Consistent with previous work, the present findings suggest that emotional vulnerability factors such as emotion dysregulation and distress tolerance may be important variables to consider in regard to panic-specific fear and expectancies, particularly those related to the cognitive consequences of anxiety. Thus, assessing levels of emotion dysregulation and distress tolerance may be useful in terms of identifying, and perhaps, clinically assisting adult smokers at risk for panic-related psychopathology and adult smokers with emotional vulnerabilities in their efforts to successfully quit smoking. Notably, the present effects for emotional dysregulation and distress tolerance were observed after accounting for other theoretically-relevant and clinically important factors including, lifetime panic attack history, daily smoking rate, and lifetime history of tobacco-related medical illness. Together, it may be necessary to understand and clinically address the roles of emotion dysregulation and distress tolerance among daily tobacco users in an effort to prevent and treat panic-relevant symptoms and facilitate success in smoking cessation.
Highlights.
We examined the main and interactive effects of emotion dysregulation and distress tolerance in relation to panic-relevant fear
We found that both emotion dysregulation and distress tolerance were significantly related to interoceptive fear and agoraphobia.
Emotion dysregulation, but not distress tolerance, was significantly related to anxiety sensitivity.
The interaction significantly predicted interoceptive and agoraphobic fears as well as the cognitive component of anxiety sensitivity.
Results suggest that emotion dysregulation and distress tolerance may be important variables to clinically target among adult daily smokers.
Figure 2.
APPQ-Agoraphobia score as a function of the interaction between DERS-Total and Breath-Holding Duration among participants 0.5 SD above and/or below the mean.
Acknowledgements
This research was supported by a National Institute on Health grant awarded to Dr. Michael J. Zvolensky and Dr. Norman B. Schmidt (CHRMS-M06-221 – R01 MH076629-01A1). This research was also supported by a National Institute on Drug Abuse National Research Service Award (5 F31 DA026634-02) awarded to Kirsten A. Johnson.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Asmundson GJG, Stein MB. Triggering the false suffocation alarm in panic disorder patients by using a voluntary breath-holding procedure. The American Journal of Psychiatry. 1994;151(2):264–266. doi: 10.1176/ajp.151.2.264. [DOI] [PubMed] [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA, US: Sage Publications; 1991. [Google Scholar]
- Barlow DH, Allen LB, Choate ML. Toward a Unified Treatment for Emotional Disorders. Behavior Therapy. 2004;Vol 35(2):205–230. doi: 10.1016/j.beth.2016.11.005. [DOI] [PubMed] [Google Scholar]
- Bernstein A, Marshall EC, Zvolensky MJ. Multi-method evaluation of distress tolerance measures and construct(s): Concurrent relations to mood and anxiety psychopathology and quality of life. Journal of Experimental Psychopathology. (in press) [Google Scholar]
- Bernstein A, Zvolensky MJ, Schmidt NB, Sachs-Ericcson N. Developmental course(s) of lifetime cigarette use and panic attack comorbidity: An equifinal phenomenon? Behavior Modification. 2007;Vol 31(1):117–135. doi: 10.1177/0145445506295056. [DOI] [PubMed] [Google Scholar]
- Boelen PA, Reijntjes A. Negative cognitions in emotional problems following romantic relationship break-ups. Stress and Health: Journal of the International Society for the Investigation of Stress. 2009;25(1):11–19. [Google Scholar]
- Bonn-Miller MO, Vujanovic AA, Zvolensky MJ. Emotional dysregulation: Association with coping-oriented marijuana use motives among current marijuana users. Substance Use & Misuse. 2008;Vol 43(11):1653–1665. doi: 10.1080/10826080802241292. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller MO, Zvolensky MJ, Bernstein A. Discomfort intolerance: Evaluation of incremental validity for panic-relevant symptoms using 10% carbon dioxide-enriched air provocation. Journal of Anxiety Disorders. 2009;23(2):197–203. doi: 10.1016/j.janxdis.2008.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N, Klein DF. Smoking and panic attacks: An epidemiologic investigation. Archives of General Psychiatry. 1999;Vol 56(12):1141–1147. doi: 10.1001/archpsyc.56.12.1141. [DOI] [PubMed] [Google Scholar]
- Brown RA, Lejuez CW, Kahler CW, Strong DR. Distress tolerance and duration of past smoking cessation attempts. Journal of Abnormal Psychology. 2002;Vol 111(1):180–185. [PubMed] [Google Scholar]
- Brown RA, Lejuez CW, Kahler CW, Strong DR, Zvolensky MJ. Distress tolerance and early smoking lapse. Clinical Psychology Review. Special Issue: Anxiety and Stress Vulnerability and Substance Problems: Theory. 2005;25(25):713–733. doi: 10.1016/j.cpr.2005.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Lejuez CW, Strong DR, Kahler CW, Zvolensky MJ, Carpenter LL, Niaura, Price LH. A prospective examination of distress tolerance and early smoking lapse in adult self-quitters. Nicotine & Tobacco Research. 2009;Vol 11(5):493–502. doi: 10.1093/ntr/ntp041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA, White KS, Barlow DH. A psychometric reanalysis of the Albany Panic and Phobia Questionnaire. Behavior Research and Therapy. 2005;Vol 43:337–355. doi: 10.1016/j.brat.2004.03.004. [DOI] [PubMed] [Google Scholar]
- Carver C, Lawrence J, Scheier M. A control-process perspective on the origins of affect. In: Martin LL, Tesser A, editors. Striving and feeling: Interactions among goals, affect, and self regulation. Mahway, NJ: Erlbaum; 1996. pp. 11–52. [Google Scholar]
- Cocores J. Nicotine dependence: Diagnosis and treatment. Psychiatric Clinics of North America. 1993;Vol 16(1):49–60. [PubMed] [Google Scholar]
- Cohen J, Cohen P. Applied multiple regression/correlation analysis for the behavioral sciences. 2nd edition. Hillsdale, NJ: Erlbaum; 1983. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd edition. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Daughters SB, Reynolds EK, MacPherson L, Kahler CW, Kanielson CK, Zvolensky MJ, Lejuez CW. Distress tolerance and early adolescent externalizing and internalizing symptoms: The moderating role of gender and ethnicity. Behaviour Research and Therapy. 2009;Vol 47(3):198–205. doi: 10.1016/j.brat.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrell M, Howes S, Bebbington P, Brugha T, Jenkins R, Lewis G, Marsden J, Taylor C, Meltzer H. Nicotine, alcohol and drug dependence and psychiatric comorbidity: Results of a national household survey. British Journal of Psychiatry. 2001;Vol 179(5):432–437. doi: 10.1192/bjp.179.5.432. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV patient edition. New York: Biometrics Research Department; 1994. (SCID-N/P, Version 2.0) [Google Scholar]
- Gonzalez A, Zvolensky MJ, Vujanovic AA, Leyro TM, Marshall EC. An evaluation of anxiety sensitivity, emotional dysregulation, and negative affectivity among daily cigarette smokers: Relation to smoking motives and barriers to quitting. Journal of Psychiatric Research. 2008;Vol 43(2):138–147. doi: 10.1016/j.jpsychires.2008.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment. 2004;Vol 26(1):41–54. [Google Scholar]
- Hays RD, Kallich JD, Mapes DL, Coons SJ, Carter WB. Development of the Kidney Disease Quality of Life (DKQOL) Instrument. Quality of Life Research. 1994;3:329–338. doi: 10.1007/BF00451725. [DOI] [PubMed] [Google Scholar]
- Hayward C, Killen JD, Taylor CB. Panic attacks in young adolescents. The American Journal of Psychiatry. 1989;Vol 146(8):1061–1062. doi: 10.1176/ajp.146.8.1061. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström K. The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance Questionnaire. British Journal of Addiction. 1991;Vol 86(9):1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Isensee B, Wittchen H, Stein MB, Hofler M, Lieb R. Smoking increases the risk of panic: Findings from a prospective community study. Archives of General Psychiatry. 2003;Vol 60(7):692–700. doi: 10.1001/archpsyc.60.7.692. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Pine DS, Klein DF, Kasen S, Brook JS. Association between cigarette smoking and anxiety disorders during adolescence and early adulthood. JAMA: Journal of the American Medical Association. 2000;Vol 284(18):2348–2351. doi: 10.1001/jama.284.18.2348. [DOI] [PubMed] [Google Scholar]
- Kashdan TB, Steger MF. Expanding the Topography of Social Anxiety: An Experience-Sampling Assessment of Positive Emotions, Positive Events, and Emotion Suppression. Psychological Science. 2006;Vol 17(2):120–128. doi: 10.1111/j.1467-9280.2006.01674.x. [DOI] [PubMed] [Google Scholar]
- Keough ME, Riccardi CJ, Timpano KR, Mitchell MA, Schmidt NB. Anxiety Symptomatology: The Association With Distress Tolerance and Anxiety Sensitivity. Behavior Therapy. 2010;41(4):567–574. doi: 10.1016/j.beth.2010.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: A population-based prevalence study. JAMA: Journal of the American Medical Association. 2000;Vol 284(20):2606–2610. doi: 10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- Leventhal AM, Zvolensky MJ, Schmidt NB. Smoking-Related Correlates of Depressive Symptom Dimensions in Treatment-Seeking Smokers. Nicotine & Tobacco Research. 2011 doi: 10.1093/ntr/ntr056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyro TM, Zvolensky MJ, Bernstein A. Distress tolerance and psychopathological symptoms and disorders: A review of the empirical literature among adults. Psychological Bulletin. 2010;Vol 136(4):576–600. doi: 10.1037/a0019712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall EC, Zvolensky MJ, Vujanovic AA, Gregor K, Gibson LE, Leyro TM. Panic reactivity to voluntary hyperventilation challenge predicts distress tolerance to bodily sensations among daily cigarette smokers. Experimental and Clinical Psychopharmacology. 2008;16(4):313–321. doi: 10.1037/a0012752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe RE, Chudzik SM, Antony MM, Young L, Swinson RP, Zolvensky MJ. Smoking behaviors across anxiety disorders. Journal of Anxiety Disorders. 2004;Vol 18(1):7–18. doi: 10.1016/j.janxdis.2003.07.003. [DOI] [PubMed] [Google Scholar]
- McHugh RK, Daughters SB, Lejuez CW, Murray HW, Hearon BA, Gorka SM, Otto MW. Shared variance among self-report and behavioral measures of distress tolerance. Cognitive Research and Therapy. doi: 10.1007/s10608-010-9295-1. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNally RJ. Anxiety sensitivity and panic disorder. Biological Psychiatry. 2002;Vol 52(10):938–946. doi: 10.1016/s0006-3223(02)01475-0. [DOI] [PubMed] [Google Scholar]
- Ormel J, VonKorff M, Ustun TB, Pini S, Korten A, Oldehinkel T. Common mental disorders and disability across cultures: Results from the WHO Collaborative Study on Psychological Problems in General Health Care. JAMA: Journal of the American Medical Association. 1994;Vol 272(22):1741–1748. doi: 10.1001/jama.272.22.1741. [DOI] [PubMed] [Google Scholar]
- Orsillo SM, Roemer L. Acceptance and mindfulness-based approaches to anxiety: Conceptualization and treatment. New York, NY: Springer; 2005. [Google Scholar]
- Payne TJ, Smith PO, McCracken LM, McSherry WC, Antony MM. Assessing nicotine dependence: A comparison of the Fagerström Tolerance Questionnaire (FTQ) with the Fagerström Test for Nicotine Dependence (FTND) in a clinical sample. Addictive Behaviors. 1994;Vol 19(3):307–317. doi: 10.1016/0306-4603(94)90032-9. [DOI] [PubMed] [Google Scholar]
- Piper ME, Smith SS, Schlam TR, Fleming MF, Bittrich AA, Brown JL, Leitzke CJ, Zehner ME, Fiore MC, Baker TB. Psychiatric disorders in smokers seeking treatment for tobacco dependence: Relations with tobacco dependence and cessation. Journal of Consulting and Clinical Psychology. 2010;Vol 78(1):13–23. doi: 10.1037/a0018065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pohl R, Yeragani VK, Balon R, Lycaki H, McBride R. Smoking in patients with panic disorder. Psychiatry Research. 1992;Vol 43(3):253–262. doi: 10.1016/0165-1781(92)90058-b. [DOI] [PubMed] [Google Scholar]
- Pomerleau CS, Carton SM, Lutzke ML, Flessland KA, Pomerleau OF. Reliability of the Fagerstrom Tolerance Questionnaire and the Fagerstrom Test for Nicotine Dependence. Addictive Behaviors. 1994;Vol 19(1):33–39. doi: 10.1016/0306-4603(94)90049-3. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Craske M, Barlow DH. Assessment Instrument for Panic Disorder that Includes Fear of Sensation-Producing Activities: the Albany Panic and Phobia Questionnaire. Anxiety. 1995;1:114–122. doi: 10.1002/anxi.3070010303. [DOI] [PubMed] [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety Sensitivity, anxiety frequency, and the prediction of fearfulness. Behaviour Research and Therapy. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Scheftner W, Endicott J. Medical history form II. 1753 West Congress Parkway, Chicago, IL, 60612: Dr. Scheftener at Rush-Presbyterian-St. Luke’s Medical Center; 1984. Available from. [Google Scholar]
- Schmidt NB, Mitchell M, Keough M, Riccardi C. Anxiety and Its Disorders. In: Zvolensky MJ, Bernstein A, Vujanovic A, editors. Distress Tolerance: Theory, Research, and Clinical Applications. Guilford Press; 2010. pp. 105–125. [Google Scholar]
- Taylor S. Anxiety sensitivity: Theory, research, and treatment of the fear of anxiety. Mahwah NJ, US: Lawrence Erlbaum Associates Publishers; 1999. [Google Scholar]
- Telch MJ, Jacquin K, Smits JAJ, Powers MB. Emotional responding to hyperventilation as a predictor of agoraphobia status among individuals suffering from panic disorder. Journal of Behavior Therapy and Experimental Psychiatry. 2003;34(2):161–170. doi: 10.1016/s0005-7916(03)00037-5. [DOI] [PubMed] [Google Scholar]
- Tull MT, Barrett HM, McMillan ES, Roemer L. A preliminary investigation of the relationship between emotion regulation difficulties and posttraumatic stress symptoms. Behavior Therapy. 2007;Vol 38(3):303–313. doi: 10.1016/j.beth.2006.10.001. [DOI] [PubMed] [Google Scholar]
- Tull MT, Roemer L. Emotion regulation difficulties associated with the experience of uncued panic attacks: Evidence of experiential avoidance, emotional nonacceptance, and decreased emotional clarity. Behavior Therapy. 2007;Vol 38(4):378–391. doi: 10.1016/j.beth.2006.10.006. [DOI] [PubMed] [Google Scholar]
- Vujanovic AA, Zvolensky MJ, Bernstein A. The interactive effects of anxiety sensitivity and emotion dysregulation in predicting anxiety-related cognitive and affective symptoms. Cognitive Therapy and Research. 2008;Vol 32(6):803–817. [Google Scholar]
- Ziedonis D, Hitsman B, Beckham JC, Zvolensky M, Adler LE, Audrain-McGovern J, Breslau N, Brown RA, George TP, Williams J, Calhoun PS, Riley WT. Tobacco use and cessation in psychiatric disorders: National Institute of Mental Health report. Nicotine & Tobacco Research. 2008;Vol 10(12):1691–1715. doi: 10.1080/14622200802443569. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Bernstein A. Cigarette smoking and panic psychopathology. Current Directions in Psychological Science. 2005;Vol 14(6):301–305. doi: 10.1177/0963721410388642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zvolensky MJ, Feldner MT, Leen-Feldner EW, McLeish AC. Smoking and panic attacks, panic disorder, and agoraphobia: A review of the empirical literature. Clinical Psychology Review. Special Issue: Anxiety and Stress Vulnerability and Substance Problems: Theory. 2005;25(25):761–789. doi: 10.1016/j.cpr.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Kotov R, Antipova AV, Schmidt NB. Cross cultural evaluation of smokers risk for panic and anxiety pathology: A test in a Russian epidemiological sample. Behaviour Research and Therapy. 2003;Vol 41(10):1199–1215. doi: 10.1016/s0005-7967(03)00031-7. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Lejuez CW, Kahler CW, Brown RA. Nonclinical panic attack history and smoking cessation: An initial examination. Addictive Behaviors. 2004;Vol 29(4):825–830. doi: 10.1016/j.addbeh.2004.02.017. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Schmidt NB, Stewart SH. Panic disorder and smoking. Clinical Psychology: Science and Practice. 2003;Vol 10(1):29–51. [Google Scholar]
- Zvolensky MJ, Vujanovic AA, Bernstein A, Leyro T. Distress tolerance: Theory, measurement, and relations to psychopathology. Current Directions in Psychological Science. 2010;Vol 19(6):406–410. doi: 10.1177/0963721410388642. [DOI] [PMC free article] [PubMed] [Google Scholar]