Abstract
The hallmark of Parkinson's disease is on-going degeneration of dopaminergic neurons in the substantia nigra, which may be due to various etiologies. Various approaches to alleviate symptoms are available, such as life-long pharmacological intervention, deep brain stimulation, and transplantation of dopaminergic neuron-containing fetal tissue. However, each of these approaches has a disadvantage. Several studies have shown that various kinds of stem cells, induced pluripotent stem cells, and other cells can differentiate into dopaminergic neurons and may be promising for treating Parkinson's disease in the future. Therefore, this review addresses those cells in terms of their prospects in cell therapy for Parkinson's disease. In addition, the need for safety and efficacy studies, various cell delivery modes and sites, and possible side effects will be discussed.
Keywords: Parkinson disease, Stem cells, Substantia nigra, Striatum, Putamen
Introduction
The pathogenesis of Parkinson's disease involves various etiologies, which culminates in the degeneration of dopaminergic neurons in the substantia nigra of the midbrain and causes dysfunction of the nigro-striatal pathway and specific symptoms due to dopamine depletion [1, 2]. Therefore, pharmacological intervention using L-dopa, the precursor to dopamine, may effectively alleviate the symptoms. However, as the disease requires life-long L-dopa administration, the response is no longer satisfactory in the long term, as the remaining dopaminergic neurons continue to degenerate. Another approach is deep brain stimulation that is directed to the subthalamic nucleus or globus pallidus. This approach shows variable results but may relieve symptoms in some advanced cases [3-5].
As the main cause of symptoms is on-going degeneration, attempts to stop degeneration using neuroprotective agents such as glial cell-line derived neurotrophic factor (GDNF) have been conducted and show promising results, although side effects due to off-target responses might appear [6]. Furthermore, the use of cannabinoids to protect dopaminergic neurons may be promising, but further studies are needed to reveal the exact mechanism of action [7].
Therefore, the best approach might be replacement of the degenerated neurons. Before the stem cell era, replacement therapy, which used dopaminergic neuron-containing fetal tissue that was transplanted into the brain, showed variable results [8, 9] due to the inability to standardize the transplanted cells. Moreover, tissue availability is also a problem [10].
Advances in stem cell research have opened a new cell therapy era for Parkinson's disease. Therefore, this review addresses the various kinds of stem cells and other cells that may be suitable for cell therapy, cells requirements for transplant, various cell delivery modes and sites, the possible side effects that may arise, and the need for safety and efficacy studies before application of cell therapy to patients with Parkinson's disease.
Stem Cell Therapy for Parkinson's Disease
Stem cells have self-renewal capacity and multi-lineage plasticity. Therefore, they are a suitable source of various kinds of cells needed for cell therapy.
To date, various studies have succeeded in differentiating various kinds of stem cells into dopamine secreting neurons. These stem cells include human embryonic stem cells (hESCs), induced pluripotent stem cells, and mesenchymal stem cells (MSCs).
Embryonic stem cell therapy for Parkinson's disease
Among all kinds of stem cells, ESCs have the most plasticity, and can differentiate into all types of cells, but they also tend to form tumors/teratomas upon grafting, which poses ethical problems.
Various studies in vertebrate models have revealed that stepwise development of ESCs into dopaminergic neurons involves midbrain cell patterning using Wnt1 and fibroblast growth factor 8 signaling [11], which directs the midbrain floor plate cells to express homeodomain transcription factors, i.e., Lmx1a and Msx1, that induce the proneural protein Ngn2 [12, 13]. Additionally, other homeodomain and paired-box transcription factors Pax2/5 and Engrailed 1 and 2 are expressed [11, 14]. Furthermore, a glycoprotein named sonic hedgehog (SHH) from the midbrain floor plate cells joins the transcription factors to direct them into midbrain neural progenitors that adopt a dopaminergic fate and express Nurr1, ptx3, En-1, Foxa2, as well as dopaminergic genes that are essential for dopamine synthesis and metabolism [14-16].
During cell therapy for Parkinson's disease, ESCs are stepwise differentiated into neural stem cells (NSCs) or neural progenitor cells that may be transplanted into animal models or patients. Further differentiation into dopaminergic neurons may be conducted either in vitro or occur in vivo after transplantation.
Differentiation of ESCs into neural precursor cells (NPCs) and dopaminergic neurons: Efficient methods to differentiate hESCs into midbrain-type neural precursor cells that can be expanded in vitro are available. NPCs can be differentiated further into dopa minergic neurons [17-19]. To eliminate the tumorigenic potential, the NPCs should undergo multiple passages under differentiation-inducing conditions to eradicate the neuroepithelial rosettes that are potentially tumorigenic structures and to eliminate the persistent hESCs that can be proven by the absence of Oct3/4 bearing cells. Studies in rats have shown that grafted multiple-passaged NPCs do not form tumors or teratomas [18]. However, these cells show survival problems during expansion in vitro and after transplantation in vivo [18], or loss of the dopaminergic neuron phenotype after transplantation [20]. Survival problems have been overcome by transgenic expression of Bcl-XL and SHH, without an increase in tumor formation [18]. Another ap proach to overcome the survival problems was developed in rat NPCs using mutant Nurr1 (Nurr1AKT). Expression of mutant Nurr1 prevents its natural degradation and causes differentiation into dopaminergic neurons with better survival and a sustained phenotype, both in vitro and in vivo after transplantation [20].
Differentiation of ESCs into NSCs and dopaminergic neurons: A study in a cynomolgus monkey Parkinson's disease model showed that transplanting ESC-derived NSCs into the putamen restores dopamine function in the putamen 12 weeks after transplantation. This result suggests dopamine release and differentiation of NSCs into dopaminergic neurons in vivo [21].
Induced pluripotent stem cell therapy for Parkinson's disease
Induced pluripotent stem cells have similar properties to ESCs in terms of their pluripotency and tumor inducing capacity. They are suitable for cell therapy, as they can be generated from the patient's own adult cells to prevent rejection and also will not pose ethical problems. However, methods should be developed to eliminate their tumor inducing property.
A method to differentiate a commercial human induced pluripotent stem (hiPS) cell line, namely IMR90 clone 4, into dopaminergic neuron progenitors is available. Furthermore, transplantation of these progenitors into a Parkinson's disease rat model showed that these progenitors could survive for a long time, and many differentiated into dopaminergic neurons and integrated well into the surrounding tissue. However, nestin positive tumor-like cells were found at the transplant site. Therefore, efforts to purify the progenitors from contaminating undifferentiated hiPS cells are of great importance [22].
A patient-derived hiPS cell line has been developed for Parkinson's disease due to a point mutation in α-synuclein (A53T). The mutation was successfully repaired by zinc finger nuclease genetic editing. The repaired hiPS differentiated into functional dopaminergic neurons [23]. Therefore, this method provides an opportunity for a cure for Parkinson's disease in the future due to a genetic point mutation.
MSCs in cell therapy for Parkinson's disease
MSCs are multipotent stem cells of mesodermal origin that differentiate into various cells of connective tissue, skeletal muscle, and even neurons, when cultured under suitable differentiating conditions. Bone marrow-derived mesenchymal stem cells (BM-MSCs) were the first MSCs studied. They represent <0.01% of all nucleated bone marrow cells and are composed of myriads of adult stem cells [24]. MSCs from various tissues including adipose tissue has been reported.
MSCs, either from bone marrow or adipose tissue, have several advantages. They can be taken from the patients themselves for autotransplantation to avoid rejection, raise no ethical problems, and can be easily expanded. Moreover, the use of MSCs in Parkinson's disease relies upon their immunosuppressive [25] and neuroprotective properties [26], as well as their ability to differentiate into astrocyte-like cells and dopaminergic neurons [27-29].
Immunosuppressive property of MSCs: The immunosuppressive property of MSCs is mediated by inhibiting all of the cells that participate in the immune response cell-cell contact-dependent mechanism as well as by releasing various soluble factors [25]. This immuno suppressive property is supposed to play a role inhibiting the inflammatory response and microglial activation; thus, preventing nigrostriatal dopaminergic neuron degeneration [30].
Neuroprotective property of MSCs: The neuroprotective property is mediated by a subpo pulation of MSCs that produce various neurotrophic factors, such as brain-derived neurotrophic factor (BDNF), beta nerve growth factor, and GDNF [26]. These neurotrophic factors may play a role in protection, functional recovery, regeneration, and survival of remaining as well transplanted dopaminergic neurons and induce the proliferation and differentiation of endogenous NSCs [31].
Moreover, a laboratory has developed a protocol to induce BM-MSCs into neurotrophic factors-secreting cells (NTF-SCs) that secrete BDNF and GDNF. The NTF-SC conditioned medium shows marked protection in a Parkinson's disease cellular model, and transplantation of the NTF-SCs into a rat model posterior to the damage resulted in migration of the transplanted cells into the damaged area and regeneration in the damaged dopaminergic nerve terminal system in the striatum [28].
Differentiation of MSCs into astrocyte-like cells: A method has been developed to differentiate BM-MSCs into GDNF, BDNF, and nerve growth factor-secreting astrocyte-like cells using a special in vitro medium. Transplantation of these astrocyte-like cells into the striatum of a Parkinson's disease rat model showed promising results. Additionally, a histological examination revealed survival of the transplanted cells and regeneration of the damaged dopaminergic nerve terminal network [27].
Differentiation of MSCs into dopaminergic neurons: A standardized xeno-free in vitro protocol has been developed for proliferating and inducing a pure population of BM-MSCs into a neuronal lineage that secretes dopamine. Transplantation of these neuronal lineage cells into a Parkinson's disease animal model showed significant improvement 3 months after transplantation [29].
Bone marrow stem cells (BM-SCs) in cell therapy for Parkinson's disease
BM-SCs consist of various kinds of stem cells, including BM-MSCs and hematopoetic stem cells. They are a suitable source for cell therapy, although the procedure to obtain them is rather invasive and painful.
Transfection of tyrosine hydroxylase and a green fluorescent protein gene (GFP) containing plasmid into BM-SCs showed an 85% efficiency rate. Transfection was followed by culture in neuronal differentiation medium. Injection of the cultured cells into the anterior horn of the lateral ventricle of a Parkinson's disease rat model showed promising results 10 days after injection [32].
NSC therapy for Parkinson's disease
NSCs can be isolated from embryonic nerve tissue, and NSCs isolated from the subventricular zone of E14 rats form neurospheres in vitro. Transplanting NSCs into the substantia nigra pars compacta or striatum of Parkinson's disease rat models resulted in survival of the transplanted cells [33].
Skin-derived stem cell therapy for Parkinson's disease
Stem cells can be obtained either from dermis, which is a source of skin-derived precursors, or from hair follicles, which are a source of epidermal neural crest stem cells.
Skin-derived precursors: Skin-derived precursors are neural crest-related stem cells that can be isolated from mammalian dermis. They differentiate into both neural and mesodermal cell lineage cells. Therefore, skin-derived precursors are promising for use as an autologous stem cell source.
A previous study used a synthetic von Hippel-Lindau peptide derived from the elongin BC-binding site that was conjugated to the protein transduction domain of the HIV-TAT protein to facilitate entry into skin derived precursors. The results showed efficient generation of cells with dopaminergic neuronal and proneural markers. Furthermore, transplanting these cells into Parkinson's disease model rats showed promising results, and that the cells generated dopaminergic neuron-like cells [34].
Epidermal neural crest stem cells: Epidermal neural crest stem cells (eNCSCs) are multi potent neural crest cells that reside in the stem cell niche of hair follicles. Implantation of eNCSCs into inflammatory brain injured model rats resulted in differentiation of the cells into immature astrocytes and Schwann cells. As astrocytes secrete neurotrophic factors, eNCSCs may be a promising cell therapy candidate for Parkinson's disease [35].
Other Cell Sources for Parkinson's Disease Therapy
Some cells other than stem cells are suitable for use as supportive cells for neurons, such as amniotic epithelial cells. These cells may be useful as alternative cell therapy sources for Parkinson's disease.
Amniotic epithelial cell therapy for Parkinson's disease
Amniotic epithelial cells are another source for cell therapy. However, donation of amniotic epithelial cell-containing amniotic fluid from pregnant women is needed to obtain these cells. Moreover, rejection problems may arise.
Amniotic epithelial cells secrete neurotrophic factors such as BDNF and neurotophin-3 and show promising results when transplanted into the striatum of Parkinson's disease model rats. Additionally, transplanting amniotic epithelial cells into the lateral ventricle showed that the cells induced increases in dopamine and its metabolites in the striatum, expression of vimentin and nestin in the graft after 5 weeks, increases in tyrosine hydroxylase-positive cells in the substantia nigra after 10 weeks, and a decrease in symptoms after 2 weeks [36].
Retinal pigment epithelium (RPE) as cell therapy for Parkinson's disease
RPE cells are L-dopa containing cells that can be isolated from the retina of human eyes. An in vitro and in vivo study on RPE in a rat model of Parkinson's disease revealed improvement of the symptoms in vivo, which was due to several mechanisms, including secretion of neurotrophic factors, i.e., GDNF and BDNF, that protect dopaminergic neurons in vitro, differentiation of the cells into dopamine secreting cells in vitro, and survival of the cells in the striatum in vivo [37].
Commercial RPE cells that are attached to gelatin microcarriers are available as Spheramine (Bayer Schering Pharma AG, Berlin, Germany). The use of Spheramine without immunosuppression is claimed to be well tolerated and showed promising results in an open label study [37].
Fetal dopamine neurons as cell therapy for Parkinson's disease
Fetal dopamine neurons can be obtained from the fetal midbrain. Fetal dopamine neurons transplanted into the striatum or both the striatum and substantia nigra of patients with Parkinson's disease showed promising clinical results. Noninvasive brain imaging showed the presence of functional dopaminergic neurons at transplantation sites, and post mortem analyses 3-4 years after transplantation showed survival of the transplanted dopaminergic neurons and a mild immune response, though the patients received standard immune suppression for 6 months only. Moreover, the putamen was densely reinnervated with new dopaminergic fibers [38].
Cell Requirements for Cell Therapy in Parkinson's Disease
The cells for cell therapy should fulfill certain requirements, including the identity of the cells and quality control during preparation.
Identity of the cells for cell therapy in Parkinson's disease
Studies on various kinds of stem cells used different protocols to isolate and expand stem cells, as well as various markers to identify the cells, e.g., for NSCs, some studies used Mushashi-1, and other studies used nestin, or sox proteins. Whether the identity of NSCs from a particular study is the same or different from that of another study is unclear [39]. Moreover, nestin or a combination of nestin and Mushashi have also been used to identify human ESC-derived NPCs [18, 19]. Therefore, the term NSC and NPC may refer to the same cell, and to conclude that NSCs and NPCs are the same cells requires further comparative studies.
Many kinds of cells or derivation of cells show promising results in in vitro and animal models. Therefore, the identity of the cells needs to be defined properly. Furthermore, to be translated into cell therapy for Parkinson's disease, the protocols to generate the cells need to be standardized and tested in many laboratories to demonstrate that they are reproducible using xeno-free media.
Quality control
Quality control includes the purity and production of cells according to good manufacturing practices.
Purity: Cell therapy for Parkinson's disease has used fetal ventral mesencephalic tissue, which contains dopaminergic neurons of mixed subtypes; therefore, the functional outcomes were variable. The A9 subtype from the substantia nigra plays an important role in motor performance recovery compared to the A10 subtype from the ventral tegmental area [40]. In some cases, graft-induced dyskinesia may occur, and this side effect is supposed to be due to serotoninergic neuron contamination [41]. Therefore, cell purity should be assured.
Good manufacturing practices: According to the US Food and Drug Administration, cell therapy products consist of two groups, the common "361 products," which require good tissue practices, and the "351 products," which require good manufacturing practices. Cell therapy products for Parkinson's disease fall into the "351 category," which include quality assurance, bioprocess monitoring control, automation, and product transportation [42].
Mode and Site of Delivery
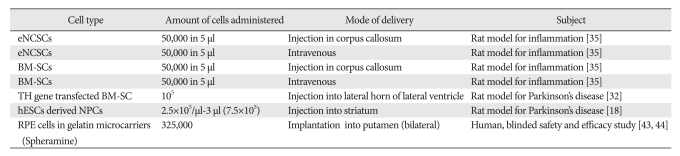
Various modes and sites of delivery for various kinds of cells have been reported, both in animal and in human studies with variable results (Table 1) [18, 32, 35, 43, 44].
Table 1.
Various studies on cell therapy in animal models and patients
eNCSCs, epidermal neural crest stem cells; BM-SCs, bone marrow stem cells; hESCs, human embryonic stem cells; RPE, retinal pigment epithelium.
Intravenous delivery
Various studies in animals and humans have shown that the pathogenesis of Parkinson's disease involves an inflammatory reaction, which may play a role in neuron degene ration. Furthermore, extensive reactive amoeboid micro glial proliferation is found in the substantia nigra of patients with Parkinson's disease [45, 46].
Intravenous administration of BM-MSCs and eNCSCs into rats results in homing of the cells to the inflammatory site in the corpus callosum, which is induced due to inflammatory injury [35]. Therefore, intravenous delivery may be effective in Parkinson's disease as well.
Moreover, MSCs are supposed to migrate to the damaged nigral area in Parkinson's disease animal models due to the release of various chemokines, including stromal-cell derived factor-1α, by the damaged area [47, 48].
Delivery into the corpus callosum
Injection of cells into the corpus callosum distal to the inflammatory site results in migration of the cells toward the inflammatory site [35]. Therefore, the corpus callosum may be used as an alternative cell delivery site in Parkinson's disease.
Delivery into the anterior horn of the lateral ventricle
Injection of GFP-expressing BM-SCs into the anterior horn of the lateral ventricle of Parkinson's disease rat models results in the presence of GFP expressing cells in the brain, suggesting migration of the injected cells through the ventricular wall along the nerve fibers [32].
Delivery into the striatum
Injections of Bcl-XL and SHH expressing hESC-derived NPCs have been performed at two sites in the striatum of Parkinson's disease model rats, resulting in survival, proliferation, and differentiation of the injected cells into mature TH+ cells, extensive neurite outgrowth, and abundant midbrain-dopaminergic-neuron marker expression. Additionally, reduced symptoms were observed in eight of 16 injected rats 8 weeks after the injection [18].
Another study on Parkinson's disease model rats showed that route of delivery by injection of microcarriers-attached to RPE cells showed that the cells survived in the striatum and improved symptoms [2].
Delivery into the putamen
Several small open-label human studies on implanting micro carriers attached to RPE cells in the putamen showed pro mising results in symptom reduction. However, a double-blind phase 2b clinical trial on implanting the cells into the bilateral putamen showed no efficacy beyond the placebo effect [43]. A postmortem analysis of the patient showed that the estimated survival of the implanted cells after 6 months was only 0.036% [44].
Delivery into the substantia nigra
Transplanting enhanced green fluorescent protein (EGFP)-expressing NSCs into the substantia nigra pars compacta or striatum of Parkinson's disease rat models showed EGFP-expressing NSCs at both sites at 1, 2, and 4 months post transplantation. Moreover, the cells transplanted in the substantia nigra pars compacta dispersed, and a significant portion differentiated into tyrosine hydroxylase-positive neurons, whereas the cells transplanted into the striatum migrated ventrally and posteriorly toward the substantia nigra pars compacta and survived there for a long time [33]. Moreover, microtransplantation of dopamine neuroblasts into the substantia nigra of Parkinson's disease model mice showed that the transplanted cells restored the damaged nigrostriatal pathway, increased expression of GDNF in the striatum, and improved symptoms [49].
Possible Side Effects
Possible side effects include tumor formation, migration of injected cells to non-target regions, immune rejection, side effects of immunosuppressant use, graft-induced dyskinesia, and mode of delivery-related adverse effects.
Tumor formation
Multifocal glioneuronal neoplasm was reported in a patient 4 years after he received intracerebellar and intrathecal injections of human fetal NSCs. The neoplasm was derived from the injected cells and came from at least two donors [50].
Immune rejection and immunosuppressant use
Immune rejection of implanted allogeneic MSCs into the striatum has been reported in Parkinson's disease model rats, irrespective of the immunosuppressive property of the MSCs. Though the immune response was insufficient to eliminate the MSCs by 22-24 days after implantation, no beneficial effects were observed. Therefore, studies need to be conducted to clarify the immune response effect on cell survival and function [51]. Should an immunosuppressant be needed, the side effects should be considered.
Graftinduced dyskinesia
Off phase graft-induced dyskinesia has been reported in some animal and human cell therapy studies for Parkinson's disease using fetal tissue or cells. The pathogenesis is supposed to involve serotonergic hyperinnervation in the striatum due to a proportion of serotonergic neurons that contaminated the grafted fetal cells [41, 52, 53].
Mode of delivery related side effects
Mode of delivery related side effects include hemorrhage and infection. Hemorrhage has been reported in a patient with Parkinson's disease who received fetal ventral mid brain cell transplantation into the putamen through a canula. The hemorrhage caused termination of the procedure after the first deposit, but the patient did not show any neurological deficits due the complications during transplantation [38].
Efficacy and Safety Studies
Various kinds of cells show potential to differentiate into dopaminergic neurons or neurotrophic factor secreting cells. Furthermore, some show efficacy in animal models for Parkinson's disease, and some have been used in human trials. However, translation into therapy in humans requires efficacy and safety assurance.
Therefore, efficacy and safety studies need to be conducted in animal models for the various kinds of cells to understand what happens to the cells after transplantation, their survival, migration, and differentiation into desired cells in the Parkinson's disease model environment. Integration of transplanted cells in a degenerated system might be difficult, and integration into the existing neuronal pathway needs to be confirmed.
It is important to test the efficacy and safety of various cell delivery routes to identify the most efficient route, the number of cells to be delivered, and to detect possible side effects that may arise.
For human trials, tracking injected cells using noninvasive brain imaging is of great importance to monitor the injected cells in term of their growth, their migration either to desired or undesired location, as well as their survival and function [54].
Postmortem analyses on transplanted fetal mesencephalic neurons in patients with Parkinson's disease revealed conflicting results in term of the appearance of Lewy bodies and α-synuclein positivity [9, 55, 56]. These conflicting results may be due to the pathogenesis that underlies the dopaminergic neuronal loss in Parkinson's disease. As Lewy bodies and α-synuclein represent one of the pathological conditions, their appearance in transplanted neurons suggest that the pathological microenvironment may lead to ongoing neuronal death, which may affect transplanted cells [56, 57].
Therefore, studies need to be conducted to reveal the exact cause and microenvironmental pathology in various kinds of Parkinson's disease. This knowledge may be useful to modulate the microenvironment to increase efficacy and to obtain a sustainable effect from cell therapy in the future.
Conclusion
Various kinds of cells are suitable for cell therapy in patients with Parkinson's disease. However, safety and efficacy studies need to be conducted followed by standardized procedures for each type of cell, mode and site of delivery, and type of Parkinson's disease. In addition, modulation of the microenvironment may lead to a sustainable therapeutic effect.
References
- 1.Savitt JM, Dawson VL, Dawson TM. Diagnosis and treatment of Parkinson disease: molecules to medicine. J Clin Invest. 2006;116:1744–1754. doi: 10.1172/JCI29178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ming M, Li X, Fan X, Yang D, Li L, Chen S, Gu Q, Le W. Retinal pigment epithelial cells secrete neurotrophic factors and synthesize dopamine: possible contribution to therapeutic effects of RPE cell transplantation in Parkinson's disease. J Transl Med. 2009;7:53. doi: 10.1186/1479-5876-7-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weaver FM, Follett K, Stern M, Hur K, Harris C, Marks WJ, Jr, Rothlind J, Sagher O, Reda D, Moy CS, Pahwa R, Burchiel K, Hogarth P, Lai EC, Duda JE, Holloway K, Samii A, Horn S, Bronstein J, Stoner G, Heemskerk J, Huang GD CSP 468 Study Group. Bilateral deep brain stimulation vs best medical therapy for patients with advanced Parkinson disease: a randomized controlled trial. JAMA. 2009;301:63–73. doi: 10.1001/jama.2008.929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Frankemolle AM, Wu J, Noecker AM, Voelcker-Rehage C, Ho JC, Vitek JL, McIntyre CC, Alberts JL. Reversing cognitive-motor impairments in Parkinson's disease patients using a computational modelling approach to deep brain stimulation programming. Brain. 2010;133(Pt 3):746–761. doi: 10.1093/brain/awp315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zahodne LB, Okun MS, Foote KD, Fernandez HH, Rodriguez RL, Kirsch-Darrow L, Bowers D. Cognitive declines one year after unilateral deep brain stimulation surgery in Parkinson's disease: a controlled study using reliable change. Clin Neuropsychol. 2009;23:385–405. doi: 10.1080/13854040802360582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gill SS, Patel NK, Hotton GR, O'Sullivan K, McCarter R, Bunnage M, Brooks DJ, Svendsen CN, Heywood P. Direct brain infusion of glial cell line-derived neurotrophic factor in Parkinson disease. Nat Med. 2003;9:589–595. doi: 10.1038/nm850. [DOI] [PubMed] [Google Scholar]
- 7.Jeon P, Yang S, Jeong H, Kim H. Cannabinoid receptor agonist protects cultured dopaminergic neurons from the death by the proteasomal dysfunction. Anat Cell Biol. 2011;44:135–142. doi: 10.5115/acb.2011.44.2.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Freed CR, Greene PE, Breeze RE, Tsai WY, DuMouchel W, Kao R, Dillon S, Winfield H, Culver S, Trojanowski JQ, Eidelberg D, Fahn S. Transplantation of embryonic dopamine neurons for severe Parkinson's disease. N Engl J Med. 2001;344:710–719. doi: 10.1056/NEJM200103083441002. [DOI] [PubMed] [Google Scholar]
- 9.Mendez I, Viñuela A, Astradsson A, Mukhida K, Hallett P, Robertson H, Tierney T, Holness R, Dagher A, Trojanowski JQ, Isacson O. Dopamine neurons implanted into people with Parkinson's disease survive without pathology for 14 years. Nat Med. 2008;14:507–509. doi: 10.1038/nm1752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xi J, Zhang SC. Stem cells in development of therapeutics for Parkinson's disease: a perspective. J Cell Biochem. 2008;105:1153–1160. doi: 10.1002/jcb.21916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joyner AL, Liu A, Millet S. Otx2, Gbx2 and Fgf8 interact to position and maintain a mid-hindbrain organizer. Curr Opin Cell Biol. 2000;12:736–741. doi: 10.1016/s0955-0674(00)00161-7. [DOI] [PubMed] [Google Scholar]
- 12.Ono Y, Nakatani T, Sakamoto Y, Mizuhara E, Minaki Y, Kumai M, Hamaguchi A, Nishimura M, Inoue Y, Hayashi H, Takahashi J, Imai T. Differences in neurogenic potential in floor plate cells along an anteroposterior location: midbrain dopaminergic neurons originate from mesencephalic floor plate cells. Development. 2007;134:3213–3225. doi: 10.1242/dev.02879. [DOI] [PubMed] [Google Scholar]
- 13.Andersson E, Tryggvason U, Deng Q, Friling S, Alekseenko Z, Robert B, Perlmann T, Ericson J. Identification of intrinsic determinants of midbrain dopamine neurons. Cell. 2006;124:393–405. doi: 10.1016/j.cell.2005.10.037. [DOI] [PubMed] [Google Scholar]
- 14.Friling S, Andersson E, Thompson LH, Jönsson ME, Hebsgaard JB, Nanou E, Alekseenko Z, Marklund U, Kjellander S, Volakakis N, Hovatta O, El Manira A, Björklund A, Perlmann T, Ericson J. Efficient production of mesencephalic dopamine neurons by Lmx1a expression in embryonic stem cells. Proc Natl Acad Sci U S A. 2009;106:7613–7618. doi: 10.1073/pnas.0902396106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smidt MP, Burbach JP. How to make a mesodiencephalic dopaminergic neuron. Nat Rev Neurosci. 2007;8:21–32. doi: 10.1038/nrn2039. [DOI] [PubMed] [Google Scholar]
- 16.Rodríguez-Gómez JA, Lu JQ, Velasco I, Rivera S, Zoghbi SS, Liow JS, Musachio JL, Chin FT, Toyama H, Seidel J, Green MV, Thanos PK, Ichise M, Pike VW, Innis RB, McKay RD. Persistent dopamine functions of neurons derived from embryonic stem cells in a rodent model of Parkinson disease. Stem Cells. 2007;25:918–928. doi: 10.1634/stemcells.2006-0386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ko JY, Park CH, Koh HC, Cho YH, Kyhm JH, Kim YS, Lee I, Lee YS, Lee SH. Human embryonic stem cell-derived neural precursors as a continuous, stable, and on-demand source for human dopamine neurons. J Neurochem. 2007;103:1417–1429. doi: 10.1111/j.1471-4159.2007.04898.x. [DOI] [PubMed] [Google Scholar]
- 18.Ko JY, Lee HS, Park CH, Koh HC, Lee YS, Lee SH. Conditions for tumor-free and dopamine neuron-enriched grafts after transplanting human ES cell-derived neural precursor cells. Mol Ther. 2009;17:1761–1770. doi: 10.1038/mt.2009.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cho MS, Lee YE, Kim JY, Chung S, Cho YH, Kim DS, Kang SM, Lee H, Kim MH, Kim JH, Leem JW, Oh SK, Choi YM, Hwang DY, Chang JW, Kim DW. Highly efficient and large-scale generation of functional dopamine neurons from human embryonic stem cells. Proc Natl Acad Sci U S A. 2008;105:3392–3397. doi: 10.1073/pnas.0712359105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jo AY, Kim MY, Lee HS, Rhee YH, Lee JE, Baek KH, Park CH, Koh HC, Shin I, Lee YS, Lee SH. Generation of dopamine neurons with improved cell survival and phenotype maintenance using a degradation-resistant nurr1 mutant. Stem Cells. 2009;27:2238–2246. doi: 10.1002/stem.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Muramatsu S, Okuno T, Suzuki Y, Nakayama T, Kakiuchi T, Takino N, Iida A, Ono F, Terao K, Inoue N, Nakano I, Kondo Y, Tsukada H. Multitracer assessment of dopamine function after transplantation of embryonic stem cell-derived neural stem cells in a primate model of Parkinson's disease. Synapse. 2009;63:541–548. doi: 10.1002/syn.20634. [DOI] [PubMed] [Google Scholar]
- 22.Cai J, Yang M, Poremsky E, Kidd S, Schneider JS, Iacovitti L. Dopaminergic neurons derived from human induced pluripotent stem cells survive and integrate into 6-OHDA-lesioned rats. Stem Cells Dev. 2010;19:1017–1023. doi: 10.1089/scd.2009.0319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Soldner F, Laganière J, Cheng AW, Hockemeyer D, Gao Q, Alagappan R, Khurana V, Golbe LI, Myers RH, Lindquist S, Zhang L, Guschin D, Fong LK, Vu BJ, Meng X, Urnov FD, Rebar EJ, Gregory PD, Zhang HS, Jaenisch R. Generation of isogenic pluripotent stem cells differing exclusively at two early onset Parkinson point mutations. Cell. 2011;146:318–331. doi: 10.1016/j.cell.2011.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Caplan AI. Why are MSCs therapeutic? New data: new insight. J Pathol. 2009;217:318–324. doi: 10.1002/path.2469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Le Blanc K, Ringdén O. Immunomodulation by mesenchymal stem cells and clinical experience. J Intern Med. 2007;262:509–525. doi: 10.1111/j.1365-2796.2007.01844.x. [DOI] [PubMed] [Google Scholar]
- 26.Crigler L, Robey RC, Asawachaicharn A, Gaupp D, Phinney DG. Human mesenchymal stem cell subpopulations express a variety of neuro-regulatory molecules and promote neuronal cell survival and neuritogenesis. Exp Neurol. 2006;198:54–64. doi: 10.1016/j.expneurol.2005.10.029. [DOI] [PubMed] [Google Scholar]
- 27.Bahat-Stroomza M, Barhum Y, Levy YS, Karpov O, Bulvik S, Melamed E, Offen D. Induction of adult human bone marrow mesenchymal stromal cells into functional astrocyte-like cells: potential for restorative treatment in Parkinson's disease. J Mol Neurosci. 2009;39:199–210. doi: 10.1007/s12031-008-9166-3. [DOI] [PubMed] [Google Scholar]
- 28.Sadan O, Bahat-Stromza M, Barhum Y, Levy YS, Pisnevsky A, Peretz H, Ilan AB, Bulvik S, Shemesh N, Krepel D, Cohen Y, Melamed E, Offen D. Protective effects of neurotrophic factor-secreting cells in a 6-OHDA rat model of Parkinson disease. Stem Cells Dev. 2009;18:1179–1190. doi: 10.1089/scd.2008.0411. [DOI] [PubMed] [Google Scholar]
- 29.Shetty P, Ravindran G, Sarang S, Thakur AM, Rao HS, Viswanathan C. Clinical grade mesenchymal stem cells transdifferentiated under xenofree conditions alleviates motor deficiencies in a rat model of Parkinson's disease. Cell Biol Int. 2009;33:830–838. doi: 10.1016/j.cellbi.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 30.Kim YJ, Park HJ, Lee G, Bang OY, Ahn YH, Joe E, Kim HO, Lee PH. Neuroprotective effects of human mesenchymal stem cells on dopaminergic neurons through anti-inflammatory action. Glia. 2009;57:13–23. doi: 10.1002/glia.20731. [DOI] [PubMed] [Google Scholar]
- 31.Park HJ, Lee PH, Bang OY, Lee G, Ahn YH. Mesenchymal stem cells therapy exerts neuroprotection in a progressive animal model of Parkinson's disease. J Neurochem. 2008;107:141–151. doi: 10.1111/j.1471-4159.2008.05589.x. [DOI] [PubMed] [Google Scholar]
- 32.Zou Z, Jiang X, Zhang W, Zhou Y, Ke Y, Zhang S, Xu R. Efficacy of tyrosine hydroxylase gene modified neural stem cells derived from bone marrow on Parkinson's disease: a rat model study. Brain Res. 2010;1346:279–286. doi: 10.1016/j.brainres.2010.05.071. [DOI] [PubMed] [Google Scholar]
- 33.Zhu Q, Ma J, Yu L, Yuan C. Grafted neural stem cells migrate to substantia nigra and improve behavior in Parkinsonian rats. Neurosci Lett. 2009;462:213–218. doi: 10.1016/j.neulet.2009.07.008. [DOI] [PubMed] [Google Scholar]
- 34.Kubo A, Yoshida T, Kobayashi N, Yokoyama T, Mimura T, Nishiguchi T, Higashida T, Yamamoto I, Kanno H. Efficient generation of dopamine neuron-like cells from skin-derived precursors with a synthetic peptide derived from von Hippel-Lindau protein. Stem Cells Dev. 2009;18:1523–1532. doi: 10.1089/scd.2008.0379. [DOI] [PubMed] [Google Scholar]
- 35.Jackson JS, Golding JP, Chapon C, Jones WA, Bhakoo KK. Homing of stem cells to sites of inflammatory brain injury after intracerebral and intravenous administration: a longitudinal imaging study. Stem Cell Res Ther. 2010;1:17. doi: 10.1186/scrt17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yang XX, Xue SR, Dong WL, Kong Y. Therapeutic effect of human amniotic epithelial cell transplantation into the lateral ventricle of hemiparkinsonian rats. Chin Med J (Engl) 2009;122:2449–2454. [PubMed] [Google Scholar]
- 37.Stover NP, Watts RL. Spheramine for treatment of Parkinson's disease. Neurotherapeutics. 2008;5:252–259. doi: 10.1016/j.nurt.2008.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mendez I, Sanchez-Pernaute R, Cooper O, Viñuela A, Ferrari D, Björklund L, Dagher A, Isacson O. Cell type analysis of functional fetal dopamine cell suspension transplants in the striatum and substantia nigra of patients with Parkinson's disease. Brain. 2005;128(Pt 7):1498–1510. doi: 10.1093/brain/awh510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Okano H, Sawamoto K. Neural stem cells: involvement in adult neurogenesis and CNS repair. Philos Trans R Soc Lond B Biol Sci. 2008;363:2111–2122. doi: 10.1098/rstb.2008.2264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Grealish S, Jönsson ME, Li M, Kirik D, Bjorklund A, Thompson LH. The A9 dopamine neuron component in grafts of ventral mesencephalon is an important determinant for recovery of motor function in a rat model of Parkinson's disease. Brain. 2010;133(Pt 2):482–495. doi: 10.1093/brain/awp328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barker RA, Kuan WL. Graft-induced dyskinesias in Parkinson's disease: what is it all about? Cell Stem Cell. 2010;7:148–149. doi: 10.1016/j.stem.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 42.Placzek MR, Chung IM, Macedo HM, Ismail S, Mortera Blanco T, Lim M, Cha JM, Fauzi I, Kang Y, Yeo DC, Ma CY, Polak JM, Panoskaltsis N, Mantalaris A. Stem cell bioprocessing: fundamentals and principles. J R Soc Interface. 2009;6:209–232. doi: 10.1098/rsif.2008.0442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Watts RL, Gross RE, Hauser RA, Bakay RA, Reichmann H, Stiver NP, Reissig E, Steiner-Schulze H, Fichte K. A phase 2b study evaluating Spheramine® in patients with advanced Parkinson's disease [Internet] Movement Disorder Virtual University; 2009. [cited 2010 Dec 27]. Available from: http://www.mdvu.org/emove/article.asp?ID=1192. [Google Scholar]
- 44.Farag ES, Vinters HV, Bronstein J. Pathologic findings in retinal pigment epithelial cell implantation for Parkinson disease. Neurology. 2009;73:1095–1102. doi: 10.1212/WNL.0b013e3181bbff1c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gao HM, Hong JS, Zhang W, Liu B. Distinct role for microglia in rotenone-induced degeneration of dopaminergic neurons. J Neurosci. 2002;22:782–790. doi: 10.1523/JNEUROSCI.22-03-00782.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ouchi Y, Yoshikawa E, Sekine Y, Futatsubashi M, Kanno T, Ogusu T, Torizuka T. Microglial activation and dopamine terminal loss in early Parkinson's disease. Ann Neurol. 2005;57:168–175. doi: 10.1002/ana.20338. [DOI] [PubMed] [Google Scholar]
- 47.Li Y, Chen J, Wang L, Zhang L, Lu M, Chopp M. Intracerebral transplantation of bone marrow stromal cells in a 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine mouse model of Parkinson's disease. Neurosci Lett. 2001;316:67–70. doi: 10.1016/s0304-3940(01)02384-9. [DOI] [PubMed] [Google Scholar]
- 48.Chamberlain G, Fox J, Ashton B, Middleton J. Concise review: mesenchymal stem cells: their phenotype, differentiation capacity, immunological features, and potential for homing. Stem Cells. 2007;25:2739–2749. doi: 10.1634/stemcells.2007-0197. [DOI] [PubMed] [Google Scholar]
- 49.Thompson LH, Grealish S, Kirik D, Björklund A. Reconstruction of the nigrostriatal dopamine pathway in the adult mouse brain. Eur J Neurosci. 2009;30:625–638. doi: 10.1111/j.1460-9568.2009.06878.x. [DOI] [PubMed] [Google Scholar]
- 50.Amariglio N, Hirshberg A, Scheithauer BW, Cohen Y, Loewenthal R, Trakhtenbrot L, Paz N, Koren-Michowitz M, Waldman D, Leider-Trejo L, Toren A, Constantini S, Rechavi G. Donor-derived brain tumor following neural stem cell transplantation in an ataxia telangiectasia patient. PLoS Med. 2009;6:e1000029. doi: 10.1371/journal.pmed.1000029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Camp DM, Loeffler DA, Farrah DM, Borneman JN, LeWitt PA. Cellular immune response to intrastriatally implanted allogeneic bone marrow stromal cells in a rat model of Parkinson's disease. J Neuroinflammation. 2009;6:17. doi: 10.1186/1742-2094-6-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Politis M. Dyskinesias after neural transplantation in Parkinson's disease: what do we know and what is next? BMC Med. 2010;8:80. doi: 10.1186/1741-7015-8-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Carta M, Carlsson T, Muñoz A, Kirik D, Björklund A. Role of serotonin neurons in the induction of levodopa- and graft-induced dyskinesias in Parkinson's disease. Mov Disord. 2010;25(Suppl 1):S174–S179. doi: 10.1002/mds.22792. [DOI] [PubMed] [Google Scholar]
- 54.Lindvall O, Björklund A. Cell replacement therapy: helping the brain to repair itself. NeuroRx. 2004;1:379–381. doi: 10.1602/neurorx.1.4.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kordower JH, Chu Y, Hauser RA, Freeman TB, Olanow CW. Lewy body-like pathology in long-term embryonic nigral transplants in Parkinson's disease. Nat Med. 2008;14:504–506. doi: 10.1038/nm1747. [DOI] [PubMed] [Google Scholar]
- 56.Li JY, Englund E, Holton JL, Soulet D, Hagell P, Lees AJ, Lashley T, Quinn NP, Rehncrona S, Björklund A, Widner H, Revesz T, Lindvall O, Brundin P. Lewy bodies in grafted neurons in subjects with Parkinson's disease suggest host-to-graft disease propagation. Nat Med. 2008;14:501–503. doi: 10.1038/nm1746. [DOI] [PubMed] [Google Scholar]
- 57.Lee PH, Park HJ. Bone marrow-derived mesenchymal stem cell therapy as a candidate disease-modifying strategy in Parkinson's disease and multiple system atrophy. J Clin Neurol. 2009;5:1–10. doi: 10.3988/jcn.2009.5.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]