Abstract
Rational drug use is a function of prescription practices having medical, social, and economic implications. A household level cross-sectional study was undertaken to determine the prescribing practices and extent of rational therapy in the rural area of 24 pgs (s) South district. Following multistage stratified random sampling, 250 households were selected for the study from 24 pgs South, West Bengal, India. Medical care received by morbid persons was noted as per prescription details, wherever available. The results indicate that of the total of 485 morbid episodes, 302 were treated at some healthcare facility and prescriptions were available for 137 (45.36%) only. Injection use was seen in 9.49% of the prescriptions. In all, 29.20% prescriptions contained at least one antibiotic. This observation was more or less the same among the private and public practitioners (34%). The average number of drugs found was 3.153 per prescription. Overall 63.51% prescriptions were found to be irrational. The prescribing practices and use of drugs have been found to be truly unsatisfactory.
Keywords: Prescription practices, Rational drug use, rural, 24 Pgs(s) in West Bengal, India
INTRODUCTION
Rational use of drugs is multifaceted. Its medical, social, and economic aspects are well reflected in the World Health Organization (WHO) definition: “Rational use of drugs requires that patients receive medications appropriate to their clinical needs, in doses that meet their own individual requirements for an adequate period of time, at the lowest cost to them and their community”.[1]
The National Health Policy 2002 of India[2] also emphsizes on the rational use of drugs within the allopathic system, along with increased access to systems of traditional medicine. However, it has been frequently observed that practitioners in alternative and indigenous systems of medicine are not properly trained and qualified in the practice of allopathic medicine. Moreover, pharmacists working under a doctor, nursing orderlies, and operation theater technicians are also not properly trained. The problem is further compounded by the prevalence of a dispensing practice, wherein written prescriptions are not provided and the patients’ pressure for quick results leads to the prevalent dispensing of steroids and use of injections. Such practitioners, both qualified and unqualified, and practices, are especially common in slums and rural areas, where most public health programs are targeted. The rapidly increasing cost of drugs prescribed across the country is a major concern at the community level. The deleterious impact of poor quality prescriptions, under- and over-dosing, duplication, and multiplicity of drugs on the restricted purse of sick persons, particularly those belonging to the lower socioeconomic strata, also adversely affect their households as a whole in terms of the non-health expenditures such as food, clothing, and education. In view of the plethora of issues associated with drug prescription, a study was conducted in a rural area of 24 pgs south to delineate the prevailing prescribing practices and to identify the extent of rational therapy received by morbid individuals therein.
Current Trends in Practice
Indian markets are flooded with over 70,000 formulations, compared to roughly 350 preparations listed on the WHO Essential Drugs List.[1] There are thousands of drug companies, and several companies manufacture generic preparations using different brand names. In addition, thousands of formulations of vitamins, tonics, and multi-drug combinations that are unique to the Indian market are manufactured and marketed regularly.
A visit to the physician has come to necessarily mean a prescription comprising of a broad-spectrum combination of antibiotics — one or more, an anti pyretic or frequently an unnecessary combination of the two, a multivitamin tonic, and a cough syrup. Intravenous, rehydration, and parenteral medication are also used more frequently.
Tonics and Cough Syrups
According to the Health Action International, ‘More than four out of every five vitamin preparations cannot be recommended; nearly three out of every five is indicated for unproven indications; more than two out of every five contain non-essential or ineffective ingredients; more than one out of every two is irrationally formulated; and nearly one out of every two contains excessive dosage.’[2,16]
Over 80 per cent of cough and cold remedies on the market are irrational, most with ineffective and some with dangerous ingredients.
Vaccines
Vaccinations have become the bread and butter of the pediatrician and parents are rarely offered the ‘option’ in optional vaccines and even vaccines like anti-pneumococcal vaccine and influenza vaccine are being used routinely by some, if not many doctors, although this has no valid justification. Growth cards and schedules are printed by drug companies and used very commonly rather than devised by the Pediatric Unit. Television has begun to routinely carry messages pertaining to vaccinations as advertisements.
In many practices, the pediatrician receives a percentage of the MRP of the vaccine — as high as 30%. That means that the more expensive the vaccine is, the greater the incentive to use it. It also gives an indication of the profit margins on vaccines! It is only the newer optional vaccines that are expensive, costing between Rs. 1000 to Rs. 1500 in smaller self-owned practices; the pediatrician stocks the vaccines and may take an even higher percentage as well as a consultation charge, sometimes amounting to over Rs. 500 per patient in one vaccination episode alone. In several practices in a private community healthcare facility catering to middle income groups, the pediatrician gets the usual consultation and has nothing to do with the purchase of vaccines, which is done by the pharmacy.[3]
Antibiotics
There is a great tendency to shift to newer more expensive antibiotics, which do not necessarily provide an advantage. This is of great concern specially where anti-typhoid drugs are being used routinely for mild infections or when drugs used for treating resistant TB, such as, azithromicin and ciprofloxacin, are being used very frequently in other mild situations, which could have been covered by other antibiotics. It also applies to drugs that should be reserved for intensive care.
Drug companies may have an interest in this situation — as overuse creates resistance among organisms and a market for newer drugs — and do everything in their power to increase the number of prescriptions of each drug whether justified or in the interest of the public.
Analgesics
The medical community's response to drugs such as Nimesulide, a drug aggressively promoted in India by pharmaceutical majors for bringing down fever in patients, is also an eye opener. The jury is still out in India as to its safety, especially in children, with many professional organizations declaring it safe and others claiming to have seen children die as a result of liver failure, from its use. The point is that excellent time-tested safe analgesia is available for children and there is no need to take any risks whatsoever. Even as the Drug Control Authority of India has cleared the drug,[4] Delhi-based lawyer group Social Jurist has filed a Public Interest Litigation (PIL) in the Delhi High Court seeking a complete ban on its production and sale. In other countries, the scientific advisory committee of the European Union issued a precautionary advice on the marketing of the drug following some serious complications of the liver, especially in children. Owing to the death of a patient due to liver failure and following reports of other adverse drug reactions, the National Agency for Medicines of Finland, ordered the suspension of the sale of Nimesulide within a short span of 72 hours. Spain followed suit within two months and took quick action by recalling all the stock lying in the distribution channel. Death of two children owing to Reye's syndrome, which reportedly happened after the intake of Nimesulide, led to the Nimesulide pediatric suspension being banned in Portugal in 1999, and Nimesulide has been withdrawn by its innovator Boehringer from Spain and Finland in 2003.[5]
It is interesting to note that the drug was never licensed for use in Canada, the United States, Britain, and Australia. Bangladesh was the last country to ban the drug. However, pediatricians in India continue blissfully to prescribe the drug and drug companies continue to prevail upon them and make it lucrative for the practice to continue.[6]
Indices for Rational Drug Prescription
What are the tools for examining whether prescriptions are generally rational or not in a healthcare setting? The WHO has created a set of the following parameters:[1]
WHO Core Drug Use Indicators to Investigate Drug Use in Healthcare Facilities.
Prescribing indicators[1]
Average number of drugs per encounter (less than two recommended)
Percentage of drugs prescribed by generic name
Percentage of encounters with an antibiotic prescribed
Percentage of encounters with an injection prescribed
Percentage of drugs prescribed from an essential drugs list or formulary
Patient care indicators[1]
Average consultation time
Average dispensing time
Percentage of drugs actually dispensed
Percentage of drugs adequately labeled
Patients’ knowledge of correct dosage
Facility Indicators[1]
Availability of copy of Essential Drug List (EDL) or formulary
Availability of active drugs
Learning from Some Literature Studies
Obviously, figures would vary depending upon the level of care being provided, being certainly higher for specialized care or Intensive Care Units as compared to general practice. Few studies have taken advantage of this tool for patient practice in India.
I. In a recent study conducted in Goa (Patel V, Vaidya R, Naik D, Borker P. Irrational drug use in India: A prescription survey from Goa. J Postgrad Med 2005;51:9-12),[5] 990 prescriptions were collected. The majority (83.9%) were from private practitioners. The quality of the layout of the prescriptions was unsatisfactory. Information to identify the practitioner was incomplete in more than one-third of the prescriptions and information to identify the patient was incomplete in more than half. Clarity of written instructions on how to take the medicines was unsatisfactory in a majority of prescriptions. Polypharmacy was the norm, with more than half (52.7%) the prescriptions containing at least three medicines. Forty percent of the prescriptions included a vitamin or tonic preparation and a quarter of the prescriptions included an antibiotic and an analgesic. Over 90% of prescriptions contained branded medicines only.
II. Private practitioners prescribed significantly greater number of medicines and were more likely to prescribe vitamins, antibiotics, and branded medicines.
A report published in the Indian journal of pediatrics in 2005, from a government hospital in Mumbai (Patterns of prescription and drug dispensing Karande Sunil, Sankhe Punam, Kulkarni Madhuri, Department of Pediatrics, Lokmanya Tilak Municipal Medical College and General Hospital, Sion, Mumbai, India, IJP 2005)[7] also reveals the kind of prescription figures we should expect from a relatively ‘rational pediatric outpatient practice’ and provides comparisons with studies done elsewhere as quoted herewith.
Data were collected prospectively by scrutinizing the prescriptions written by pediatric resident doctors and by interviewing parents of 500 outpatient children. The average number of drugs per encounter was 2.9, out of which 73.4% drugs were prescribed in the generic name. A majority of the drugs prescribed were in the form of syrups (60.8%). Use of antibiotics (39.6% of encounters) was frequent, but injection use (0.2% of encounters) was very low. A high number of drugs prescribed (90.3%) conformed to a model list of essential drugs and were dispensed (76.9%) by the hospital pharmacy. Certain drugs (5.7%) prescribed as syrups were not dispensed, although they were available in tablet form. Most parents (80.8%) knew the correct dosages, but only 18.5% of the drugs were adequately labeled. No copy of an essential drugs list was available. The availability of the key drugs was 85%.
The average number of drugs / injections per encounter is an important index of the scope for educational intervention in prescribing practices. Our figure of 2.9 drugs per encounter is higher than the recommended limit of 2.0. Similar findings have been reported in other Indian studies; and from Burkina Faso, Cambodia, Ethiopia, Ghana, Morocco, Nepal, Nigeria, Pakistan, Tanzania, and Zimbabwe (2.2 to 4.8 drugs per encounter). Even in USA, patients receive 2.7 drugs per encounter. However, studies from Bangladesh and Lebanon have reported rational figures of 1.4 and 1.6, respectively. In the present study three or more drugs have been prescribed in 62.4% of the prescriptions, which increases the risk of drug interactions, of dispensing errors, and of the parent not knowing the dosage schedules. Increasing generic prescribing will rationalize the use and reduce the cost of drugs. Our figure of 73.4% drugs being prescribed by generic name is higher than those reported in all other Indian studies; and those from Ghana, Lebanon, Nepal, and Pakistan (2.9 to 65.0%). However higher figures (75 to 99.8%) of generic prescribing has been reported from Bangladesh, Cambodia, Ethiopia, and Tanzania.
Appropriate use of antibiotics is necessary to prevent the emergence of drug-resistant bacteria. Our figure of 39.6% prescriptions having an antibiotic is lower than that reported in most other Indian studies; and those from Cambodia, Ethiopia, Ghana, Morocco, and Nigeria (47.5 to 100%). However, lesser figures of prescribing antibiotics (17.5 to 35.4%) have been reported from Bangladesh, Lebanon, Nepal, and Tanzania. Most acute gastroenteritis cases are viral and need only oral rehydration therapy. Although in the present study 24.6% of children with acute gastroenteritis were prescribed an antibiotic, this is lower than the figures reported in other Indian studies (64 and 83%); and those from Nigeria, Indonesia, Bangladesh, and Pakistan (58 to 96%). Similarly, most acute respiratory infections are viral and antibiotics need not be prescribed. In the present study 52.8% of the children with acute respiratory infections were prescribed an antibiotic, but this is lower than figures reported from Mexico (77%); and from developed countries such as USA (43%) and Canada (74%).
A better performance in Bangladesh has been highlighted, except in treatment of diarrhea, as part of its overall advance in drug policy, among Asian countries.
Although most prescriptions are in generic terms this has been creating a problem. As pharmacies are not stocking generic drugs; the actual brand dispensed is then decided by the pharmacist according to his or her advantage. Circumventing this problem by instructing our in-house pharmacist to dispense the cheapest formulation available unless specifically instructed has been tried. However, the system does not work well unless the physician has a say in what the pharmacist chooses to stock.
Thus generic prescriptions are no use without a formulary approach to stocking and will not work in the private healthcare setting except to the detriment of the patient.
Within this group, no patient required admission or injections. Almost all the patients were followed up by phone or visit and were known to undergo the predictable outcomes of recovery. Subjectively, most patients expressed satisfaction and have not shifted to another physician. Few demanded medication after things were explained to them. However, telephonic consultations for reassurance after consultations, not resulting in medication, were very high, and reviews were also frequent. These were uncharged in this clinic, therefore, a patient may be seen up to thrice for one consultation fee (Rs 150) and of course the telephonic advice is free and return phone calls unpaid for. Many parents get well trained in handling common colds and coughs and do not require more than telephonic reassurance in the subsequent illnesses and therefore cut down on their clinic visits. This does not make for a lucrative practice in the short and medium term!
Clearly, the picture of prescription varies markedly between what is seen in small private practices and what is found in public health services, especially those linked with the academic units. Irrational use of drugs in a system where the doctor does not benefit from his / her irrationality in monetary terms, are related to lack of training, information, and experience and must be distinguished from reasons of economics, to be able to formulate adequate interventions.
Root Causes of Irrational Drug Prescriptions for Patients
Looking at the reasons for the irrational prescription for patients are given in detail:
Reasons not related to monetary benefits to pParental demand and anxiety (built upon by drug companies, media etc., and thus definitely of financial benefit to the companies)
Need for quick relief because of lack of time of both patients and doctors
Doctors lack of experience and training contributing to lack of proper conviction in rational prescribing even if he / she arrives at the right diagnosis
Doctors lack of peer support
Lack of treatment protocols
Lack of audit systems by the doctors’ community and professional associations
Wrong or incomplete information to doctors by drug companies
Increasing litigations with inadequate structures for handling them
Lack of understanding of ill effects of over-prescription among Doctors and Carriers
Self-prescription and over-the-counter (OTC) availability
Reasons related to Monetary Benefits to Prescriber
Doctor's unwillingness to ‘lose a patient’ by defying the trend
Doctor's unwillingness to lose a patient by suggesting a chronic problem like asthma, epilepsy or cerebral palsy, leading to both inadequate and unnecessary treatment
Desire to please drug companies and ‘earn’ kickbacks, conference sponsorships, corporate gifts, CME sponsorships (applicable to doctors in both private and public healthcare systems)
The overall experience or opinion that investments in quality relationships and a non-compromising ethical practice are not seen to allow the making of a ‘decent’ living in the short-term
Interventions
Interventions that have been suggested by the WHO[1] and others, are related to the root causes in the former category and include
Support to countries for implementing and monitoring a national strategy[2] to promote the rational use of drugs by health professionals and consumers
Developing the national standard treatment guidelines, essential drugs lists, educational programs, and other effective mechanisms to promote rational drug use by all qualified health professionals
Establishing effective systems to provide independent and unbiased drug information — including traditional medicine to the general public and to improve drug use by the patient
Advocacy of rational drug use
Identification and promotion of successful rational drug use strategies
Responsible drug promotion should be encouraged
Information support on the use of traditional medicine
Support for problem-based and skill-based ‘In-service Training Programmes’
Establishing drugs and therapeutic committees to maintain rationality
Expanding international technical guidelines and standards on traditional medicine
Implementation of effective systems on drug information.
Public education in rational drug use and patient empowerment
All these interventions relate largely to training and support for better practice and would work well within the public health systems to some extent, but they do not acknowledge the economics of irrational prescription and the monetary benefit from the same to practitioners in both public and private healthcare, and the vested interests of drug companies.
At the very minimum there must be stringent regulation of the drug company — prescriber relationship, which cannot be left to the individual understanding of ethics. The question of whether rational drug prescriptions are compatible with a private pediatric practice where the majority of childhood diseases are self-limiting and require minimal treatment or management, and where simple information to parents can ‘reduce the patient load’ by a large percent, especially among generally well middle class children, demands some greater thought on our part.
MATERIALS AND METHODS
This enquiry is a component of a larger study on the spectrum of morbidity conducted in the year 2009. A community-based, cross-sectional survey was undertaken in the rural area of 24 pgs South. The 18 Community Development Blocks in that district, had an estimated population of 69 lacs living in 29 blocks and 312 Gram Panchayat villages spread over 8165.05 sq. km. Following a pilot study to calculate the current prevalence of morbidity, 250 households were selected by multistage stratified random sampling. The sociodemographic characteristics of 1522 persons belonging to these households were obtained by interviewing the head or any other responsible household member using a pre-designed and pretested schedule. Medical care received by morbid individuals, sick within 15 days prior to the interview, including morbidity carried over from an earlier period, was recorded as a per prescription detail, wherever available.
Information thus collected was examined for types and number of drugs and the type of healthcare provider. For the purpose of analysis the public health facilities were defined as subcenters, Primary Health Centers (PHC), Community Health Centers (CHC), and government hospitals / dispensaries, and private health care providers, as qualified private practitioners, private hospitals / Nursing Homes Hospitals / dispensaries run by non-governmental organizations. Local unqualified private practitioners, medicine shops, and traditional / spiritual healers were grouped into the category of unqualified practitioners. Rationality was determined on the basis of Standard Treatment Guidelines (STGs) and the guidelines were formulated by the opinion of experts from various medical faculties for morbid conditions whose STGs were not available. The data was analyzed using the Statistical Package for Social Sciences (SPSS version 10.0). In order to draw meaningful inferences, the means and proportions were compared by applying the Student's t-test and Chi-Square test, respectively.
RESULTS
A majority (94.6%) of the households were Hindus by religion, while nearly half (47.4%) belonged to Other Backward Castes, and 23.5% to Scheduled Castes. The average family size was 6.08 with per capita income of 46.3% households being more or less Rs. 3000 per month. Major sources of livelihood of households were agriculture (32.0%), small-scale business (20.7%), and skilled labor (33.3%). In all, 1041 (68.4%) study subjects were literate, with male and female rates being 83.0 and 50.9%, respectively. One-fifth (20.86%) of the households had at least one morbidity, with 1.27 morbid persons per household on an average. The morbid person prevalence was to the extent of 208.6 per 1000 persons. Overall 318 persons experienced 485 morbid episodes, out of which 183 (37.73%) were left without treatment. Unqualified practitioners were the major providers (36.50%) of medical care in the study area, while allopathic was the predominant (91.01%) system of medicine utilized by the sick study subjects. Out of 302 episodes of illness where treatment was obtained from some healthcare facility, prescriptions were available only for 137 (45.36%); 9.49% of these prescriptions had at least one injection, with similar proportions in the public, private, and unqualified healthcare providers. At least one antibiotic was present in 29.20% of the prescriptions, the practice being more common among the private practitioners (34.78%). The practice of prescribing analgesic / anti-inflammatory preparations was equally prevalent across the Private and Unqualified healthcare providers [Table 1] but not predominant in Public sectors.
Table 1.
Prescriptions with at least one type of specified drug according to the type of health care provider
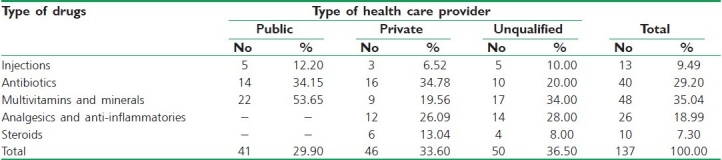
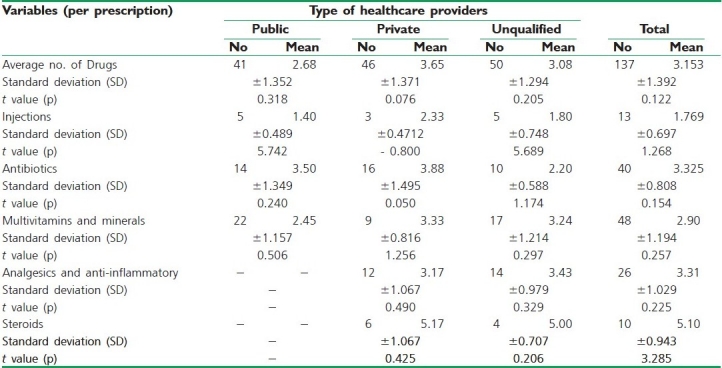
Table 2 shows that 3.153 drugs were prescribed on an average. This was less in public facilities (2.68) compared to unqualified (3.08) and private (3.65) practitioners. Antibiotics per prescription formed a significantly lower proportion for the unqualified practitioners (2.20) relative to public (3.50) and private (3.88) healthcare providers. In the case of Steroid prescription in private (5.17), this practice was significantly higher among the groups of public, similar to unqualified (5.00) practitioners. A same trend was observed for prescription of analgesics and anti-inflammatories.
Table 2.
Prescribing pattern by type of health care provide
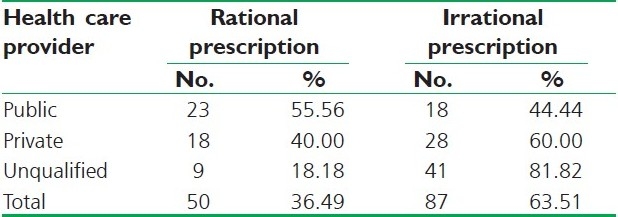
Standard treatment guidelines were available for diagnostic categories mentioned in 27% of the prescriptions, of which 63.51% of the prescriptions were found to be irrational. From among the rest of the prescriptions, analyzed on the basis of expert opinion, only 36.49% were rational.
Overall 63.51% prescriptions were found to be irrational [Table 3]. This figure was the highest for prescriptions from unqualified sources of medical care (81.82%) and lowest (44.44%) for the public sector.
Table 3.
Rationality of prescriptions according to a healthcare provider
DISCUSSION
The outcome of medical care and expenditure therein are sequent to the prescribing practices in a given area. This has drawn the attention of researchers, and prescription audit has become a fascinating field of research. However, the non-availability of prescriptions in a majority of morbid events is a serious handicap for such studies. This situation also, to some extent, reflects the kind of healthcare practice prevailing in the region and the importance given to prescriptions by the rural population in general. Excessive use of injections has been reported by several workers across the country. Contrary to the higher number of prescriptions with at least one injection among the private healthcare providers (65.5%) in Andhra Pradesh,[4] no difference was found between private and unqualified practitioners in this study. According to Christenson and Anokbonggo, 57.3% of the prescriptions contained at least one antibiotic.[8] Lower figures have been observed in this study. However, over-prescription of antibiotics, by private practitioners in particular, may be due to the requirement of the disease itself, or on account of public pressure of expectation of quick relief as also higher monetary gains. High prevalence of multivitamin / mineral prescription is highly questionable in case of the public sector. Furthermore, it unnecessarily increases the number of drugs per prescription and thereby the cost.[14]
The number of drugs per prescription in the study area has been slightly lesser than the reported figure of 3.5 in another study conducted across the state of Uttar Pradesh.[9] However, figures less than the present observation have been documented by researchers in Andhra Pradesh (2.1) and Vellore (2.4).
Antibiotic use in this rural area of 24 pgs South has been much lower than the figure of 58.6% per prescription reported by Reddy and Gupta,[9] in a study on rational drug therapy in Uttar Pradesh.
According to the studies in Vellore[10] and Hyderabad[11] nutritional products, vitamins, and analgesics were the most commonly prescribed drugs. The proportion of drugs of these categories was seen to be very high in prescriptions of unqualified practitioners in this study region also.
Examining the relevance of the drugs prescribed as per STGs is pertinent, but limited in its scope, as STGs are available only for certain diseases for which national programs are in vogue, namely, diarrhea, acute respiratory tract infections, tuberculosis, malaria, and so on. Here the experts of various faculties of medical sciences play a role. The problem is further aggravated by the fact that symptoms and / or diagnosis of a patient are difficult to find even with all the available prescriptions. In fact, as per a study conducted in the PHCs of Varanasi[12] the diagnosis was mentioned in less than two-thirds of the prescriptions. The extent of rationality of the prescriptions has been much below that expressed in a nationwide multicentric study,[13] wherein, 4 to 26% of the prescriptions have been labeled as irrational.
CONCLUSION
The prescribing practices in this region of the country are found to be unsatisfactory, with rational drug therapy being made use of in one-third (36.49%) of the cases only. However, the findings of the present study, based on the analysis of the micro-sample of prescriptions, warrants cautious interpretation. On the one hand this calls for a prescription audit on an adequate sample size in the community at large vis-à-vis at the health facility level and on the other the pertinence of orienting healthcare providers at all levels toward rational drug use and healthy prescribing practices is doubtful.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
REFERENCES
- 1.Geneva: World Health Organization; 1988. WHO. Model list of essential drugs. [Google Scholar]
- 2.National Health Policy 2002. New Delhi: Ministry of Health and Family Welfare, Government of India; [Last accessed on 2002]. Government of India. Available from: http://www.mohfw.nic.in/np2002.htm . [Google Scholar]
- 3.Anand K, Pandav CS, Kapoor SK. Undergraduate Study Team. Injection use in a village in North India. Natl Med J India. 2001;14:143–4. [PubMed] [Google Scholar]
- 4.Hyderabad: Centre for Social Services; 1997. ASCI. National Drug Policy Study: India. With specific reference to Andhra Pradesh State: Final report; p. 40. India: Administrative Staff College of India. [Google Scholar]
- 5.Patel V, Vaidya R, Naik D, Borker P. Irrational drug use in India: A prescription survey from Goa. J Postgrad Med. 2005;51:9–12. [PubMed] [Google Scholar]
- 6.George R, Abraham R. Private health in India. Lancet. 2002;359:1528. doi: 10.1016/S0140-6736(02)08459-3. [DOI] [PubMed] [Google Scholar]
- 7.Karande S, Sankhe P, Kulkarni M. Mumbai, India: IJP; 2005. Department of Pediatrics. [Google Scholar]
- 8.Christensen RO, Anokbonggo WW. Prescribing in hospital outpatient departments and rural health facilities in Uganda: Some clinical and educational implications. Dan Med Bull. 1990;37:375–7. [PubMed] [Google Scholar]
- 9.Reddy DC, Gupta VM. Varanasi: Department of Preventive and social Medicine, Institute of Medical Sciences; 2001. Rational use of drugs: Problems in Indian context. Background material for Workshop on Rational Drug Use, Feb 2001. India: Banaras Hindu University. [Google Scholar]
- 10.Kuruvilla A, George K, Rajaratnam A, John KR. Prescription patterns and cost analysis of drugs in a base hospital in South India. Natl Med J India. 1994;7:167–8. [PubMed] [Google Scholar]
- 11.Krishnaswamy K, Kumar BD, Radhiah GA. A drug survey-Precepts and practices. Eur J Clin Pharmacol. 1985;29:363–70. doi: 10.1007/BF00544095. [DOI] [PubMed] [Google Scholar]
- 12.Mohapatra SC. Thesis for MD (PSM) Varanasi: Institute of Medical Sciences; 1978. Study of medical care provided by three Primary Health Centres of Varanasi district, UP. India: Banaras Hindu University. [Google Scholar]
- 13.Krishnangshu R, Ghosh JM, Chandhri SB, Mandal A, Prasad S. Calcutta: Voluntary Consumer Action Network (V-CAN), Consumer Utility and Trust Society; 1996. Prescription audit analysis-A study of drug prescription practices in India. [Google Scholar]
- 14.Chirmule D, Gupte A. Pune: Bhartiya Agro Industries Foundation; 1997. Factors affecting health seeking and utilization of curative heath care. [Google Scholar]
- 15.Duggal R, Amin S. Bombay: The Foundation for Research in Community Health; 1989. Cost of health care: A household survey in an Indian District. [Google Scholar]
- 16.Phadke A. New Delhi: Sage Publications; 1998. Drug supply and use.Towards a rational policy in India; pp. 110–1. [Google Scholar]


