Abstract
Objectives:
The present research addressed the following important question in pediatric medicine: Can participation in a new family-centered preventive intervention, the Strong African American Families–Teen (SAAF–T) program, deter conduct problems, substance use, substance use problems, and depressive symptoms among rural black adolescents across 22 months?
Methods:
Data were collected from 502 black families in rural Georgia, assigned randomly to SAAF–T or an attention control condition. The prevention condition consisted of 5 consecutive meetings at community facilities with separate, concurrent sessions for caregivers and adolescents followed by a caregiver-adolescent session in which families practiced skills they learned in the separate sessions. Adolescents self-reported conduct problem behaviors, substance use, substance use problems, and depressive symptoms at ages 16 years (pretest) and 17 years 10 months (long-term assessment).
Results:
Adolescents who participated in SAAF–T evinced lower increases in conduct problem behavior, substance use, substance use problems, and depressive symptom frequencies than did adolescents in the attention control condition across the 22 months between pretest and long-term assessment.
Conclusions:
This is the first study to demonstrate efficacy in a prevention program designed to deter conduct problems, substance use, substance use problems, and depressive symptoms among rural black adolescents. Because SAAF–T is a manualized, structured program, it can be easily disseminated to public health agencies, schools, churches, boys’ and girls’ clubs, and other community organizations.
KEY WORDS: adolescent, black, depression, drug-seeking behavior, family intervention, parents, prevention, social adjustment
What’s Known On This Subject:
Conduct problems, substance use, substance use problems, and depressive symptoms increase as black adolescents enter high school. Although family-centered prevention programs deter these problems during middle school, no such programs have been developed and evaluated for black high school students.
What This Study Adds:
This study demonstrates that participation in a family-centered preventive intervention reduces conduct problems, substance use, and substance use problems among black adolescents by more than 30% compared with adolescents in an attention control condition across nearly 2 years.
More than 15 million black families live in the rural southern coastal plain that stretches from South Carolina to Louisiana, one of the most economically disadvantaged areas in the United States,1 in which tax bases are low. Consequently, few pediatric mental health, substance use, or prevention services are available in this area.2 Historically, residence in these rural communities has protected black adolescents from developing the levels of conduct problems, depressive symptoms, and substance use problems that are prevalent in urban areas. Epidemiologic data, however, indicate that black adolescents in rural areas now display rates of these problems that equal or exceed those among adolescents in densely populated inner cities.3 These circumstances and the need they produce for prevention programs designed for this population led to the development of the Strong African American Families–Teen (SAAF–T) program; its primary objective is to deter substance use, conduct problems, and depressive symptoms across adolescence. The purpose of this study was to test empirically the efficacy of SAAF–T in preventing increases in conduct problems, substance use, substance use problems, and depressive symptoms among rural black adolescents.
SAAF–T builds on other family-centered intervention programs that have been found to enhance parent and youth competence while inhibiting children’s and preadolescents’ substance use, delinquent activity, and other co-occurring problems among youth in elementary school and middle school.4–6 For broad public health impact, however, family-centered prevention programs must be available for youth at all developmental stages. Unfortunately, no family-centered prevention programs for adolescents have been developed and tested, despite epidemiologic research that highlights the emergence and escalation of substance use, conduct problems, and depressive symptoms around the time of high school entry.7,8 The development of these problems could be addressed with timely intervention. The development and evaluation of SAAF–T was designed to meet the need for family-centered prevention programs for adolescents in general and for black adolescents in particular.
SAAF–T was developed according to the recommendations set forth by the Institute of Medicine8,9 that longitudinal, epidemiologic research with the target population should guide the selection of malleable protective factors—those that can be modified—to be targeted in prevention programs. Data that we gathered from more than 1000 rural black adolescents and their families for more than a decade were used to identify such factors in the adolescents’ immediate family contexts. In this research, we identified powerful caregiving practices that nurtured the development of adolescent self-regulation, achievement orientation, and negative attitudes toward substance use and other risk behaviors. All of these characteristics were negatively associated with the development of problem behaviors across adolescence.10 Protective caregiving practices include setting limits, monitoring adolescents’ whereabouts and knowing their friends, instilling a sense of racial pride, teaching strategies for dealing with discrimination, monitoring and supporting academic achievement, and solving problems cooperatively. These practices, along with the promotion of adolescent self-regulation, were targeted in SAAF–T.
Adolescents and their families were randomly assigned to either SAAF–T or an attention control program. The use of an attention control group is unique in evaluations of the efficacy of family-centered interventions. Typically, control groups in such evaluations receive either no treatment or minimal information; these designs do not control for nonspecific factors, such as social support from intervention trainers and other group members, which arguably could be responsible for observed intervention effects. To provide a more stringent efficacy evaluation, all families, whether assigned to SAAF–T or the attention control condition, attended a 5-session, 10-hour group prevention program. The control program was designed to promote good nutrition, exercise, and informed consumer behavior among adolescents. The attention control program included no content that referred to or provided information about the protective processes targeted in SAAF–T. We hypothesized that adolescents participating in SAAF–T would manifest lower levels of conduct problems, substance use, substance use problems, and depressive symptoms than would those in the attention control condition across the 22 months that separated the pretest and long-term follow-up assessments.
Methods
Overview
Data on adolescents’ conduct problems, substance use, substance use problems, and depressive symptoms were obtained via self-report at ages 16 years (pretest) and 17 years 10 months (long-term follow-up) from adolescents in the SAAF–T and attention control conditions. A brief description is provided here of participant recruitment and enrollment, intervention implementation and fidelity, and data collection procedures.
Participants
Participants in the trial included 502 black families in rural Georgia; in each family, an adolescent who was 16 years of age at recruitment (51% girls) and the adolescent’s primary caregiver (in most cases the biological mother) provided data. Mean household monthly gross income was $1482.50. Although the caregivers worked an average of 41.5 hours per week (SD = 20.36), 63.8% of the families lived below federal poverty standards and another 18% lived within 150% of the poverty threshold; they can be described as working poor.11
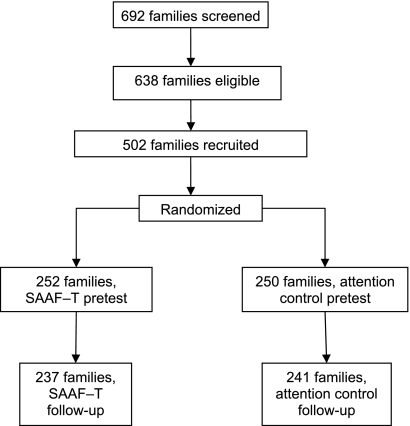
Schools in 6 counties provided lists of 10th-grade students from which participants were selected randomly. During recruitment and before randomization, families were told that they would participate in a 5-session program to build family skills that would promote adolescent well-being. The flow of participants through the trial is presented in Fig 1. Of the 692 families screened, 638 (91%) were eligible to participate. Of the eligible families, 502 (79%) agreed to participate. Of the families recruited, 252 were assigned randomly to SAAF–T and 250 to the attention control group. Of the families who provided data at pretest, 478 (95%) provided data 22 months later at long-term follow-up: 237 in the intervention group and 241 in the control group. No demographic differences emerged between these families and the 24 families who left the study.
FIGURE 1.
Flow of participants through the trial.
Intervention Implementation
The SAAF–T program consisted of 5 consecutive meetings held at community facilities; it included separate caregiver and adolescent skill-building curricula and a family curriculum. Each meeting included separate 1-hour concurrent training sessions for caregivers and adolescents followed by a 1-hour caregiver-adolescent session during which families practiced the skills they learned in the separate sessions. Thus, families received 10 hours of prevention programming. Concurrently with the implementation of SAAF–T, the attention control group participated in a family-centered intervention designed to promote healthful behaviors among adolescents by encouraging good nutrition, exercise, and informed consumer behavior. The school-based FUEL program was adapted into the 5-session family skills format used in SAAF–T. The result was a program structurally similar to SAAF–T that we named Fuel for Families (FF). Black intervention leaders were trained to criterion in the presentation of SAAF–T and FF, both of which were manualized. Fidelity of intervention delivery was confirmed using established procedures.12
In SAAF–T, caregivers were taught consistent use of monitoring and control, adaptive racial socialization approaches that included guidance for dealing with discrimination, establishment of clear norms and expectations about adolescent substance use, provision of academic support, and cooperative caregiver-adolescent problem solving. Adolescents were taught the importance of having and following household rules, strategies to use when encountering racism, the importance of academic success, goal formation, and strategies for attaining educational and occupational goals. To preserve the random nature of the group assignments, data analyses included all families regardless of the number of program sessions they attended, an intent-to-treat analysis. Both SAAF–T and FF families attended an average of 4 of the 5 program sessions.
Data Collection Procedures
Black college students and community members who were blind to group assignments served as field researchers to collect pretest and long-term follow-up data in the families’ homes. Researchers made one visit lasting 2 hours to each family at each assessment. The time from pretest to long-term follow-up averaged 22 months. Informed consent forms were completed at both data collection points. All measures were administered on laptop computers via audio computer-assisted self-interview. Families received $100 at pretest and at long-term follow-up for completing the measures. When completing pretest measures, families had not yet been assigned to SAAF–T or FF.
Measures
Socioeconomic Risk Index
Six dichotomous variables formed a socioeconomic risk index that was used as a control in the data analyses. A score of 1 was assigned to each of the following: family poverty based on federal guidelines, caregiver unemployment, receipt of Temporary Assistance for Needy Families, caregiver single parenthood, caregiver education level less than high school graduation, and caregiver-reported inadequacy of family income. The scores were summed to form the index.
Conduct Problems
Using 14 questions from the National Youth Survey,13 adolescents indicated the frequency during the past 6 months with which they had fought, stolen, been truant from school, or been suspended from school. Adolescents’ responses were summed, and the sum constituted the conduct problems score.13 Internal consistency analyses were not executed because this instrument yields count data.
Substance Use
Items from the public health literature14 and our previous research with rural black youth15–17 were used to evaluate substance use. Adolescents indicated, on a scale ranging from 0 (none) to 6 (30 or more times), how often during the past 3 months they had consumed a drink of alcohol, consumed 3 or more drinks at one time, and smoked marijuana. Adolescents also reported, on a scale ranging from 0 (not at all) to 6 (about 2 packs/day), their cigarette smoking during the past 3 months. Responses were summed to form a substance use composite, a procedure that is consistent with our own and other prior research.18,19
Substance Use Problems
Using the 10-item Minnesota Survey of Substance Use Problems,20 adolescents reported the number of times during the past 12 months they had used substances in hazardous situations; failed to fulfill role obligations because of substance use; or experienced legal, social, or interpersonal problems because of substance use. The response set ranged from 0 (zero) to 6 (11 or more). Responses were summed to yield a substance use problems score. Internal consistency analyses were not executed because this instrument yields count data.
Adolescent Depressive Symptoms
Adolescent depressive symptoms were assessed with the 20-item Center for Epidemiologic Studies Depression Scale,21 a self-rated measure of symptoms occurring during the previous week. The response set ranged from 0 (rarely or none of the time, less than 1 day) to 3 (most of the time, 6–7 days). This scale has been well validated and used extensively with black participants.22 Of the sample, 31% scored above the clinical cutoff of 16, demonstrating a moderate level of depressive symptoms.
Healthful Behavior
Adolescents’ healthful behaviors were assessed using 6 items from the Youth Risk Behavior Survey (YRBS).23 Adolescents reported how often during the past 7 days they exercised and consumed fruit, vegetables, 100% fruit juices, milk, and carbonated beverages (reverse scored). The response set ranged from 0 (none) to 6 (4 or more times per day). This scale has been used in several national, ethnically diverse surveys and has shown good validity and reliability.23
Intervention Status and Gender
Intervention status and gender were dummy coded. SAAF–T participants were coded 1 and attention control participants were coded 0; male adolescents were coded 1 and female adolescents were coded 0.
Results
Preliminary Analyses
Sample Equivalence
Comparisons between the SAAF–T and attention control conditions on pretest socioeconomic risk, adolescent gender, and pretest assessments of the outcome variables showed no between-group differences.
Descriptive Statistics
Mean prevalence rates for the outcomes at pretest, when the adolescents were 16 years of age, were as follows: M = 6.16 (SD = 13.27) for conduct problems during the past 6 months, M = 0.74 (SD = 1.67) for substance use during the past 3 months, M = 0.52 (SD = 1.80) for substance use problems during the past 12 months, and M = 13.80 (SD = 8.69) for depressive symptoms during the past week. Levels of conduct problems and depressive symptoms were moderate to high, and levels of substance use and substance use problems were low. These rates of problem behaviors for black youth during adolescence are consistent with data from other studies.24
Data Analysis
A Zero-Inflated Poisson (ZIP) regression model25 was used to test the study hypothesis for conduct problems, substance use, and substance use problems. This procedure, which is appropriate for positively skewed data, was selected because it corrects for distributions of count data that contain a large number of zero counts. In the following analyses, the ZIP regression simultaneously examined intervention effects on 2 components of the outcomes: (1) a binary yes or no report indicating that the outcome measure did or did not occur during the reporting period, and (2) the frequency with which outcomes occurred during the reporting period. Ordinary least squares (OLS) regression was used to examine the hypothesis for depressive symptoms. OLS was appropriate for this outcome because the depression assessment yields few, if any, zeroes. Because the distribution of the adolescents’ responses to the depression measure was positively skewed, a logarithmic transformation was performed to create a less-skewed distribution before execution of the OLS model.
Tests of the Study Hypothesis
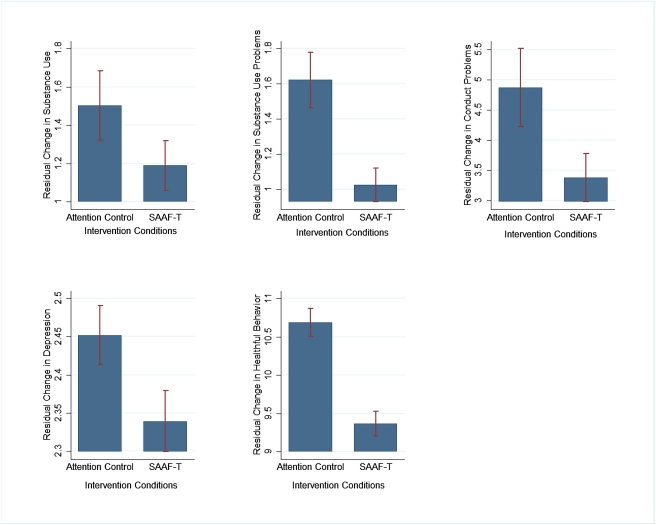
Table 1 presents the tests of the study hypothesis that adolescents in the SAAF–T condition would evince fewer conduct problems, less frequent substance use, fewer substance use problems, and fewer depressive symptoms than would those in the attention control condition across the 22 months between the pretest and long-term follow-up assessments. The analyses for substance use problems included only adolescents who were using substances at baseline because, logically, they are at higher risk for developing such problems. The coefficients in Table 1 for the analyses involving conduct problems, substance use, and substance use problems are odds ratios. Fig 2 presents the estimated changes in the frequency of each outcome for adolescents in the SAAF–T and attention control groups. In each of the analyses presented in Table 1, sociodemographic risk, adolescent gender, and pretest levels of the outcomes were controlled; this allowed each analysis to test the possibility that SAAF–T participation caused differences in the outcomes’ rates of change across time. The ZIP regression analyses for changes in the frequencies of conduct problems, substance use, and substance use problems revealed consistent results. SAAF–T participation caused significant and robust prevention effects (all P < .001), such that participation in SAAF–T, compared with participation in the attention control program, was associated with a 36% decrease (100*[1 − e−0.442]) in the frequency of conduct problems, a 32% decrease in substance use (100*[1 − e−0.637]), and a 47% decrease (100*[1 − e−0.442]) in substance use problems. No intervention effects emerged from the ZIP regression analyses of the binary data.
TABLE 1.
Associations Among Intervention, Gender, Cumulative Risk, and Changes in Substance Use, Conduct Problems, Substance Use Problems, Depression, and Healthful Behaviors at Long-term Follow-up
| Substance Use Wave 3 | Substance Use Problems Wave 3 | Conduct Problems Wave 3 | Depression Wave 3 | Healthful Behavior Wave 3 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Logistic Portion | Counts Portion | Logistic Portion | Counts Portion | Logistic Portion | Counts Portion | OLS Regression | OLS Regression | |||||||||
| Predictors | Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE |
| 1. Pretest measure | −1.040*** | 0.22 | 0.111*** | 0.01 | −2.064*** | 0.29 | −0.022 | 0.09 | −1.741*** | 0.29 | 0.009 | 0.09 | 0.507*** | 0.05 | 0.293*** | 0.05 |
| 2. Male gender | 0.222 | 0.25 | 0.669*** | 0.10 | −0.805** | 0.25 | 0.407*** | 0.10 | −0.807** | 0.26 | 0.445*** | 0.10 | 0.041 | 0.06 | 0.660 | 0.44 |
| 3. Cumulative risk | 0.047 | 0.09 | 0.057 | 0.03 | −0.041 | 0.09 | 0.129*** | 0.03 | −0.074 | 0.09 | 0.108*** | 0.03 | 0.034 | 0.02 | 0.080 | 0.16 |
| 4. Intervention | −0.258 | 0.24 | −0.372*** | 0.09 | −0.139 | 0.25 | −0.637*** | 0.09 | −0.126 | 0.26 | −0.617*** | 0.09 | −0.118* | 0.06 | −0.120** | 0.44 |
P < .05
P < .01
P < .001.
FIGURE 2.
Estimated changes in the frequency of each outcome for adolescents in the attention control group and the SAAF–T intervention group.
The OLS regression model of the effects of SAAF–T participation on changes in depressive symptoms is depicted in the far right column of Table 1. With socioeconomic risk, gender, and pretest depression levels controlled, SAAF–T participants experienced fewer depressive symptoms over time than did attention control participants (P < .01). SAAF–T participants evinced a 4.5% decrease in depressive symptoms relative to participants in the attention control program.
Finally, we executed an exploratory analysis to examine the possibility that participation in the attention control program affected adolescents’ healthful behaviors. Using an OLS regression model (see Table 1) with socioeconomic risk, gender, and pretest levels controlled, FF participants reported a larger increase over time in healthful behaviors than did SAAF–T participants (P < .01). FF participants increased their healthful behaviors 14.5% more than did SAAF–T participants.
Discussion
We evaluated a randomized, controlled trial designed to decrease the frequency of conduct problems, substance use, substance use problems, and depressive symptoms among rural black adolescents. This is the only family-centered intervention conducted with black adolescents, and it is the only one of which we are aware in which behavioral, substance use, and emotional risk reduction were evaluated simultaneously. Offrequency particular importance, the evaluation period spanned nearly 2 years, demonstrating that the effects SAAF–T participation produced were not transitory. The results are similar to long-term effects that family-centered prevention programs achieved with white preadolescents residing in the Midwest26,27 and black youth in the rural South.28 These other family-centered programs, however, were designed for preadolescents and do not target the changing risk and protective factors youth experience in midadolescence. SAAF-T, moreover, is unique in addressing depressive symptoms during a time when youths’ vulnerability to mood problems increases. The risk reductions in outcome frequencies associated with SAAF–T participation has important public health and clinical implications. From a public health perspective, the goal of prevention programs for adolescents is to shift the curves for problem behaviors and substance use so that fewer youth in the population distribution use illicit substances and become involved with the legal system. This shift not only leads to decreases in incarceration rates and drunk-driving fatalities, but also reduces other threats that these problems pose for mental health, school completion, and family relationships.
From a clinical perspective, the results suggest that an inoculation of protective caregiving and self-regulatory skills during preadolescence may contribute to a self-sustaining trajectory of disinterest in and avoidance of antisocial behavior and substance use during adolescence, when some friends and acquaintances may begin to model and sanction it. An advantage of imparting these protective processes through a universal program such as SAAF–T is the avoidance of stigma. Neither adolescents nor their caregivers are enrolled in SAAF–T on the basis of preexisting adolescent behavior problems or substance use. Caregivers and youth thus take part to promote well-being, a purpose that the families in this study embraced.
The study was also designed to rule out a plausible rival hypothesis, effects of nonspecific factors, to explain the efficacy of family-centered interventions. Control conditions in past evaluations of family-centered preventive intervention did not control for social support within prevention groups; thus, observed changes may not have resulted from the program content per se. The current study is the first randomized, controlled trial of which we are aware in which the family-centered training and group formats were identical in the prevention and control groups, with only the program content differing. Even with this rigorous design, SAAF–T showed robust, long-term prevention effects.
The results also indicated that participation in the attention control program, FF, increased physical activity and healthful eating more than did participation in SAAF–T. This finding, which attests to the validity and efficacy of the attention control condition and its curriculum, is also important to the study population. To our knowledge, there are no efficacious family-centered programs that promote healthful diets and exercise among black adolescents. Future research on FF will indicate its efficacy in increasing exercise and reducing obesity in the black American population. Exercise is a protective factor against, and obesity is a risk factor for, chronic diseases that this population experiences at extraordinarily high rates.29
The self-report nature of the behavioral measures limits the conclusions that can be drawn from them. We attempted to minimize this limitation by using audio computer-assisted self-interview technology. The extent to which the sample was representative constitutes another potential limitation of this research; the sample’s characteristics, however, were consistent with the demographic nature of the population from which it was drawn. Finally, the binary analysis conducted to determine whether adolescents did or did not experience the outcomes during the previous month did not evince intervention effects. This is likely to be because of the epidemiology of problem behaviors among rural African American adolescents, which indicates that these behaviors occur at higher rates during young adulthood. In addition, although SAAF–T was efficacious in deterring the development of depressive symptoms, the effects were weaker than for substance use and conduct problems. The impact of SAAF–T on depressive symptoms is likely to be enhanced by the addition of prevention components that encourage problem-focused coping and attributional styles that decrease self-blame and guilt.
Conclusions
The availability of preventive interventions designed for black adolescents, particularly those in rural areas, is crucial because few, if any, mental health or substance use programs exist for this population. The Institute of Medicine30 has called for family-centered interventions that target adolescent mental health and substance use problems, although, before the research reported herein, no successful interventions existed. We have shown that 10 hours of family-centered prevention programming can be effective in deterring behavioral, substance use, and emotional problems among black adolescents across a period of almost 2 years. Because SAAF–T is a manualized, structured program, it can easily be disseminated to state public health programs, schools, churches, boys’ and girls’ clubs, and other community organizations. The cost of implementing SAAF–T will decrease when state-level agencies implement it, yielding an economy of scale that has emerged for family-centered prevention programs serving preadolescents.31 Its focus on promoting adolescent and family well-being is likely to lead to its wide acceptance.
Acknowledgments
This study was supported by award numbers R01DA021736 and P30DA027827 from the National Institute on Drug Abuse. The content of this article is solely the responsibility of the authors and does not necessarily reflect the official views of the National Institute on Drug Abuse or the National Institutes of Health.
Glossary
- FF
Fuel for Families
- OLS
ordinary least squares
- SAAF–T
Strong African American Families Teen program
- ZIP
Zero-Inflated Poisson regression
Footnotes
Dr Brody provided substantial contributions to conception and design, interpretation of the data, drafting of the article, critical revision for intellectual content, and final approval of the version to be published; Drs Chen and Yu provided substantial contributions to design, data analysis, and final approval of the version to be published; Dr Kogan provided substantial contributions to conception and design, and final approval of the version to be published; and Drs Molgaard, DiClemente, and Wingood provided substantial contributions to conception and design.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
Funded by the National Institutes of Health (NIH).
References
- 1.Proctor BD, Dalaker J. Poverty in the United States: 2002 (Current Population Reports, P60-222). Washington, DC: US Bureau of the Census; 2003 [Google Scholar]
- 2.Brody GH, Neubaum E, Boyd GM, Dufour M. Health consequences of alcohol use in rural America. In: Robertson EB, Sloboda Z, Boyd GM, Beatty L, Kozel NJ, eds. Rural substance abuse: state of knowledge and issues. Rockville, MD: U.S. Department of Health and Human Services; 1997:137–174. NIDA Research Monograph 168 [PubMed] [Google Scholar]
- 3.Milhausen RR, Crosby R, Yarber WL, DiClemente RJ, Wingood GM, Ding K. Rural and nonrural African American high school students and STD/HIV sexual-risk behaviors. Am J Health Behav. 2003;27(4):373–379 [DOI] [PubMed] [Google Scholar]
- 4.Brody GH, Murry VM, Gerrard M, et al. The Strong African American Families program: translating research into prevention programming. Child Dev. 2004;75(3):900–917 [DOI] [PubMed] [Google Scholar]
- 5.Kumpfer KL, Alvarado R, Whiteside HO. Family-based interventions for substance use and misuse prevention. Subst Use Misuse. 2003;38(11-13):1759–1787 [DOI] [PubMed] [Google Scholar]
- 6.Leigh BC, Stall R. Substance use and risky sexual behavior for exposure to HIV. Issues in methodology, interpretation, and prevention. Am Psychol. 1993;48(10):1035–1045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brody GH, Chen YF, Kogan SM. A cascade model connecting life stress to risk behavior among rural African American emerging adults. Dev Psychopathol. 2010;22(3):667–678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.O'Connell ME, Boat T, Warner KE. Preventing Mental, Emotional, and Behavioral Disorders Among Young People: Progress and Possibilities. Washington, DC: National Academies Press; 2009 [PubMed] [Google Scholar]
- 9.Institute of Medicine Reducing Risks for Mental Disorders: Frontiers for Preventive Intervention Research. Washington, DC: National Academies Press; 1994 [PubMed] [Google Scholar]
- 10.Brody GH, Kogan SM, Grange CM. Translating longitudinal, developmental research with rural African American families into prevention programs for rural African American youth. In: King R, Maholmes V, eds. The Oxford Handbook on Child Development and Poverty. New York, NY: Oxford University Press-USA [Google Scholar]
- 11.Boatright SR. The Georgia County Guide. Athens: The Center for Agribusiness and Economic Development; 2005 [Google Scholar]
- 12.Fisher JD, Fisher WA, Bryan AD, Misovich SJ. Information-motivation-behavioral skills model-based HIV risk behavior change intervention for inner-city high school youth. Health Psychol. 2002;21(2):177–186 [PubMed] [Google Scholar]
- 13.Elliott DS, Ageton SS, Huizinga D. Explaining Delinquency and Drug Use. Beverly Hills, CA: Siegel; 1985 [Google Scholar]
- 14.DiClemente RJ, Wingood GM, Crosby R, et al. Parental monitoring: association with adolescents’ risk behaviors. Pediatrics. 2001;107(6):1363–1368 [DOI] [PubMed] [Google Scholar]
- 15.Brody GH, Murry VM, Gerrard M, et al. The Strong African American Families program: prevention of youths’ high-risk behavior and a test of a model of change. J Fam Psychol. 2006;20(1):1–11 [DOI] [PubMed] [Google Scholar]
- 16.Wills TA, Gibbons FX, Gerrard M, Brody GH. Protection and vulnerability processes relevant for early onset of substance use: a test among African American children. Health Psychol. 2000;19(3):253–263 [DOI] [PubMed] [Google Scholar]
- 17.Wills TA, Gibbons FX, Gerrard M, Murry VM, Brody GH. Family communication and religiosity related to substance use and sexual behavior in early adolescence: a test for pathways through self-control and prototype perceptions. Psychol Addict Behav. 2003;17(4):312–323 [DOI] [PubMed] [Google Scholar]
- 18.Brody GH, Ge X. Linking parenting processes and self-regulation to psychological functioning and alcohol use during early adolescence. J Fam Psychol. 2001;15(1):82–94 [DOI] [PubMed] [Google Scholar]
- 19.Newcomb MD, Bentler PM. Consequences of Adolescent Drug Use: Impact on the Lives of Young Adults. Thousand Oaks, CA: Sage; 1988 [Google Scholar]
- 20.Harrison PA, Fulkerson JA, Beebe TJ. DSM-IV substance use disorder criteria for adolescents: a critical examination based on a statewide school survey. Am J Psychiatry. 1998;155(4):486–492 [DOI] [PubMed] [Google Scholar]
- 21.Radloff LS. The CES–D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401 [Google Scholar]
- 22.Beach SRH, Kogan SM, Brody GH, Chen YF, Lei M-K, Murry VM. Change in caregiver depression as a function of the Strong African American Families program. J Fam Psychol. 2008;22(2):241–252 [DOI] [PubMed] [Google Scholar]
- 23.Youth Risk Behavior Surveillance System (YRBSS). US Department of Health and Human Services; 2009. Available at: www.cdc.gov/HealthyYouth/yrbs/index.htm Accessed July 11, 2011.
- 24.Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future National Results on Adolescent Drug Use: Overview of Key Findings, 2003. Bethesda, MD: National Institute on Drug Abuse; 2004. NIH Publication No. 04-5506 [Google Scholar]
- 25.Atkins DC, Gallop RJ. Rethinking how family researchers model infrequent outcomes: a tutorial on count regression and zero-inflated models. J Fam Psychol. 2007;21(4):726–735 [DOI] [PubMed] [Google Scholar]
- 26.Spoth RL, Redmond C, Shin C, Azevedo K. Brief family intervention effects on adolescent substance initiation: school-level growth curve analyses 6 years following baseline. J Consult Clin Psychol. 2004;72(3):535–542 [DOI] [PubMed] [Google Scholar]
- 27.Spoth RL, Trudeau L, Guyll M, Shin C, Redmond C. Universal intervention effects on substance use among young adults mediated by delayed adolescent substance initiation. J Consult Clin Psychol. 2009;77(4):620–632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brody GH, Chen YF, Kogan SM, Murry VM, Brown AC. Long-term effects of the Strong African American Families program on youths’ alcohol use. J Consult Clin Psychol. 2010;78(2):281–285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Harper S, Lynch J, Burris S, Davey Smith G. Trends in the black-white life expectancy gap in the United States, 1983-2003. JAMA. 2007;297(11):1224–1232 [DOI] [PubMed] [Google Scholar]
- 30.Institute of Medicine Priority Areas for National Action: Transforming Health Care Quality. Washington, DC: National Academies Press; 2003 [PubMed] [Google Scholar]
- 31.Spoth RL, Greenberg MT. Toward a comprehensive strategy for effective practitioner-scientist partnerships and larger-scale community health and well-being. Am J Community Psychol. 2005;35(3-4):107–126 [DOI] [PMC free article] [PubMed] [Google Scholar]