Abstract
Objective(s)
To characterize the longitudinal patterns of antipsychotic treatment and to investigate the relationship between antipsychotic treatment patterns and acute hospitalizations among adults with schizophrenia. We hypothesized that continuous antipsychotic treatment would be associated with fewer hospitalizations and shorter lengths of stay.
Method
Seven years of retrospective Maryland Medicaid administrative data were used to examine inpatient medical encounters and outpatient psychotropic treatment in community-based settings from 1993 through 2000. The sample consisted of 1,727 adults continuously enrolled in the Maryland Medicaid program from July 1992 through June 1994, and diagnosed with schizophrenia. The main outcome measures were a) any schizophrenia hospitalization; b) number of schizophrenia hospitalizations; and c) inpatient days associated with a primary diagnosis of schizophrenia.
Results
The average duration of antipsychotic use was six months in any single year and four and one-half years across the entire study period. Compared to individuals with a more continuous pattern of antipsychotic treatment, individuals with moderate or light use had odds of hospitalization for schizophrenia that were 52 or 72 percent greater (95%CI: 30−75% greater, 49−100% greater respectively). Light users of antipsychotics have an average length of stay per hospitalization that is approximately 20 percent longer than the average for continuous users (95%CI: 2−39% longer).
Conclusions
Findings emphasize the benefit of continuous antipsychotic treatment for individuals with schizophrenia.
Keywords: schizophrenia, Medicaid, longitudinal analysis, severe mental illness, antipsychotic use
1.1 INTRODUCTION
The Schizophrenia Patient Outcomes Research Team (PORT) recommendations support chronic maintenance antipsychotic treatment (Lehman et al. 2004; Lehman et al. 1998). This results in fewer symptoms, a less episodic course (APA 1997), better clinical and functional outcomes for adults with schizophrenia (Lehman et al. 1995; Verdoux et al. 2000), and fewer relapses (Herz et al. 1991; Schooler 2006).
Despite this evidence, research on outpatient utilization spanning 1987−1997 shows that it rarely is continuous in a given year (dosReis et al. 2002; McCombs et al. 1999; Menzin et al. 2003; Mojtabai et al. 2002; Vanelli et al. 2001; Velligan et al. 2003; Williams et al. 1999). Only 12−30% of individuals received continuous antipsychotic treatment over a one year period (McCombs et al. 1999; Williams et al. 1999). From 17−24% of adults with schizophrenia do not receive medication in outpatient settings (dosReis et al. 2002; McCombs et al. 1999). Prescription refills over a nine-month period in 1998−1999 indicate that approximately 30% of individuals discontinue antipsychotic medication within three months after initiating treatment (Vanelli et al. 2001). Following hospital discharge, 37% of adults with schizophrenia discontinue medication within one month (Mojtabai et al. 2002), rising to 60% at three months (Velligan et al. 2003). Continuous outpatient use ranges from four to seven months (dosReis et al. 2002; McCombs et al. 1999; Menzin et al. 2003).
This is important because antipsychotic adherence is correlated with psychiatric hospitalization. Over a one year period, individuals with schizophrenia who consumed less than 80% of their medication (i.e., poor adherers) had a 2.4 greater likelihood of a psychiatric admission relative to those who consumed 80% or more (i.e., good adherers) (Valenstein et al. 2002). Others have reported a similar association between poor antipsychotic adherence and increased hospitalization rates (Gilmer et al. 2004; Weiden et al. 2004). Prior research has examined one to three years of community treatment. However, this may not fully reflect the tolerability, sustainability, and adherence to chronic, maintenance antipsychotic treatment. From this perspective, the present study sought to characterize longitudinal patterns of antipsychotic treatment and to examine the association between antipsychotic patterns and the number and duration of schizophrenia-related hospitalizations. We hypothesize that continuous antipsychotic use will be associated with a lower likelihood of schizophrenia-related hospitalizations, fewer hospitalizations, and shorter lengths of stay than with less continuous treatment.
1.2 EXPERIMENTAL/MATERIALS and METHODS
1.2.1 Patterns and Outcomes of Care Project
The patterns and outcomes of care for severely mentally ill (SMI) Medicaid recipients was a longitudinal study of treatment, outcomes, and the impact of managed care from July 1993 through June 2000. It was conducted in collaboration with the State of Maryland Medical Assistance Program and the Mental Hygiene Administration. The protocol was approved by the Institutional Review Boards for Johns Hopkins Bloomberg School of Public Health and the Maryland State Department of Health and Mental Hygiene. A waiver of informed consent was granted for use of the claims data.
1.2.2 Patterns and Outcomes of Care Base Population
The population (N=6,235) was identified from adults enrolled in the state Medicaid program. Inclusion criteria were a) highly probable or probable SMI; b) continuously enrolled from July 1992 through June 1994; c) aged 21 through 62 as of July 1, 1992; and d) residing in one of 12 Maryland counties from July 1992 through June 1994. Highly probable and probable SMI was determined by psychiatric diagnosis in the year prior to the study (July 1992-June 1993) and disability status. The highly probable SMI were a) disabled with at least one claim associated with a diagnosis of schizophrenia; b) disabled with at least one claim with bipolar/major depression diagnoses; or c) non-disabled with at least one claim associated with a diagnosis of schizophrenia. The population was selected from metropolitan Baltimore and lower Eastern Shore regions (i.e., Baltimore City, Anne Arundel, Baltimore, Caroline, Carroll, Dorchester, Harford, Howard, Somerset, Talbot, Wicomico and Worcester counties). Among the 6,235 individuals, 2,392 (38%) were highly probable SMI and had a claim with a schizophrenia diagnosis.
1.2.3 Study Sample
The study sample was the 1,727/2,392 individuals highly probable SMI with schizophrenia who were continuously enrolled from July 1, 1993-June 30, 2000. The 665 excluded due to non-continuous enrollment did not differ in age, gender, or race from the study sample. Continuously-enrolled individuals were more likely to receive an antipsychotic than non-continuously enrolled individuals (93% vs. 77%, p<0.001), which may be due to an underestimate of antipsychotic use during disenrollment periods. The study sample is representative of individuals with schizophrenia who receive chronic treatment in outpatient settings (dosReis et al. 2002; McCombs et al. 1999; Menzin et al. 2003).
1.2.4 Data Sources
Paid claims for medical encounter and pharmacy services from July 1, 1993-June 30, 2000 characterized mental health visits and antipsychotic utilization patterns. Medicaid eligibility files identified enrollment patterns, county of residence, zipcode, age, gender, race, monthly enrollment flags (yes/no), Medicaid eligibility category (i.e., disabled), and Medicare eligibility.
1.2.4.1 Medical Encounter Data
Medical (i.e., physician; non-hospital-based clinics) and institutional (i.e., hospital) claims defined utilization by the place of service, type of procedure, type of facility, ambulatory or inpatient service, and up to four diagnoses (psychiatric or medical). Diagnosis was coded as an International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM). Using a three-digit ICD-9 code, psychiatric diagnoses were grouped as schizophrenia, bipolar/major depression, other SMI disorders (e.g., paranoid states, all other psychiatric illnesses).
Person level information was aggregated as monthly and annual summary variables. Hospitalizations were summarized as the number of admissions, length of stay, and counts of evaluation and management, consultation and mental health procedures. Outpatient services were organized by psychiatric diagnoses (i.e., schizophrenia, bipolar disorder) and overall mental health visits.
1.2.4.2 Pharmacy Claims Data
Psychiatric medications from the pharmacy claims were classified by individual agent and by major psychotropic class. The classes included stimulants, antidepressants, antipsychotics, antiparkinsonian, sedative/hypnotics, anxiolytics, and mood-stabilizers. Antidepressant sub-classes included selective serotonin reuptake inhibitors (SSRI), tricyclic antidepressants (TCA), and other antidepressants. Mood-stabilizing agents used in psychiatry included carbamazepine, valproic acid, gabapentin, lamotrigine, and oxcarbazepine anticonvulsants and lithium.
A previously used method (dosReis et al. 2002) was employed to estimate antipsychotic continuity as treatment days per month and year. This was calculated by summing the days supply of medication across consecutive prescription refills for an antipsychotic with the same active ingredient and dosage, e.g., chlorpromazine 100mg. Consecutive prescription refills were considered the same treatment exposure; otherwise a gap of 14 days or more between refills was considered a separate exposure. This criterion was based on evidence that 4−19 day gaps between refills are common in a given treatment episode (Ascione et al. 1985; Schulz and Gagnon 1982). Total days of use per month and year were the sum of continuous days across different exposure periods. During periods of inpatient hospitalization, pharmacy claims will be absent. Therefore, in addition to total days of use per month and year, we calculated the total days eligible for outpatient pharmacy services by excluding periods of inpatient hospitalization. Duration of decanoate antipsychotics is difficult to estimate, and so we conducted a sensitivity analysis with and without decanoate formulations. Thus, the predictor variable that is used included decanoate days.
1.2.5 Statistical Analyses
T-tests and chi-square tests were used to compare characteristics of the subjects with no antipsychotic use to those with at least one day of use during the study period. Specifically, individuals were compared in terms of age, gender, race, baseline diagnoses, number of schizophrenia-related hospitalizations, annual length of stay and use of lithium, anti-depressants and mood stabilizers.
Primary analyses focused on the subjects with at least one day of antipsychotic use during the study period. Longitudinal multivariate models assessed the temporal association between the likelihood of a hospitalization in the current month and antipsychotic use in the prior 3 months. The dependent variables were schizophrenia-related hospitalization (any vs. none) and the length of stay per hospitalization during the current month.
The time-varying independent variable was a nominal measure of magnitude of antipsychotic use during the prior three month period. Magnitude of use was classified into three mutually exclusive groups: continuous (medication for at least 75% of eligible days), moderate (medication for 50−75% of eligible days) and light (medication for less than 50% of eligible days). Using the medication possession ratio (MPR) to estimate medication consumption, 80% is considered adherent (Valenstein et al. 2004) and anything lower is partial or non-adherent. In addition, the state Medicaid policy requires 75% or more of a medication to be consumed before authorizing a refill. Thus, our classification was based on empirical research and state policy.
Graphical displays summarized the likelihood of schizophrenia-related hospitalization, average length of stay per hospitalization and magnitude of antipsychotic use. Longitudinal logistic and Poisson regression models assessed the odds of any schizophrenia-related hospitalization during the current month and the average length of stay per hospitalization, respectively, across the magnitude of antipsychotic use during the prior three months. The longitudinal logistic regression model included adjustments for any hospitalization within the prior three month period, type of antipsychotic used in the prior three months (first generation, second generation, or both) and age, gender, race, and baseline diagnoses. The longitudinal Poisson regression model adjusted for previous three-month total hospitalization days (0 days; 1−7 days; 8−30 days; and 30 or more days), type of antipsychotic used in the prior three months (first generation, second generation, or both) and age, gender, race, and baseline diagnoses.
The Poisson regression model accounted for the over-dispersion in the data (i.e., greater variability in days of hospitalization relative to the average days of hospitalization). After assessing the correlation in the monthly odds of any schizophrenia-related hospitalization per month and length of stay per hospitalization, the standard errors in the longitudinal models were calculated assuming an exchangeable correlation structure. We assessed the sensitivity of our results to adjustment for the decrease in the average length of stay per hospitalization over the study period. Data were analyzed using SAS® version 9.1 (SAS Institute, Cary, NC).
1.3 RESULTS
1.3.1 Demographic Characteristics of the Sample
Of the 1,727 continuously enrolled individuals with schizophrenia, 93% (n=1,613) had at least one antipsychotic prescription claim during 1993−2000. Age, gender, and race did not differ between individuals with and without any antipsychotic use (Table 1). Individuals with no antipsychotic use were more likely to have a psychiatric diagnosis in addition to schizophrenia.
Table 1.
Summary statistics for demographic and schizophrenia hospitalizations among individuals classified as having schizophrenia at baseline stratified by antipsychotic usea
| Demographic and Schizophrenia-related Hospitalization Measures | Any antipsychotic use (n = 1,613) | No antipsychotic use (n = 114) | p |
|---|---|---|---|
| White | 41% | 48% | 0.49 |
| Male | 50% | 41% | 0.08 |
| Age, years (at baseline) | 40 (± 10) | 41 (± 10) | 0.27 |
| Schizophrenia | 100% | 100% | n/a |
| Bipolar Disorder | 27% | 46% | <0.001 |
| Other Psychiatric Disorderb | 43% | 65% | <0.001 |
| Any hospitalization | 44% | 9% | < 0.001 |
| Average number of hospitalizationsc | 3.7 (± 4.8) | 2.8 (± 2.4) | 0.57 |
| Average annual LOSc | 17 (± 14.3) | 13 (± 17.8) | 0.33 |
Individuals are compared based on having any antipsychotic use vs. no antipsychotic use during 1993 to 2000. Values in the table represent percent for categorical variables and mean (SD) for continuous variables.
Other psychiatric disorder refers to disorders other than schizophrenia or bipolar disorder. Diagnoses were based on the individual's utilization experience in fiscal year 1993.
Among individuals with at least one schizophrenia-related hospitalization.
1.3.2 Hospitalizations for Schizophrenia
Only 9% of those with no antipsychotic use had one or more schizophrenia-related hospitalization, compared to 44 % of the antipsychotic users (Table 1; p< 0.001). Comparing antipsychotic users with non-users, the average number of schizophrenia-related hospitalizations during the study (3.7 vs. 2.8, respectively; p = 0.57) and the average hospitalization days per year (17 vs. 13, respectively; p = 0.33) were not significantly different.
Among those with at least one antipsychotic prescription during the study period, around 2% had at least one hospitalization per month (Figure 1). The average length of stay from monthly admissions varied from 6−27 days with an average of 11 days across the seven years (Figure 1). We observed no seasonal trends in the likelihood of hospitalization or length of stay; although there was a significant decrease over time by a half a day per year (p = 0.002).
Figure 1.
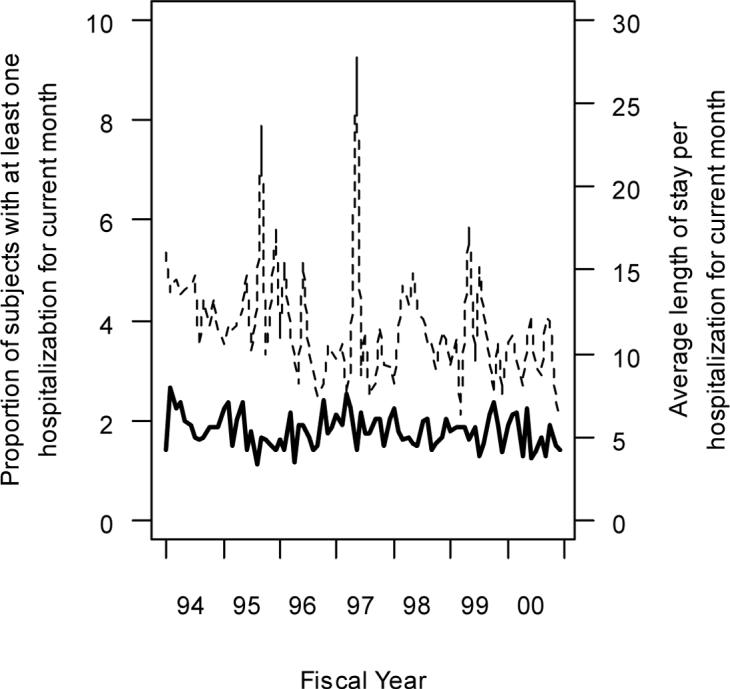
Proportion of subjects with at least one hospitalization and average length of stay per hospitalization within the current month.
1.3.3 Description of Antipsychotic Treatment Patterns
Individuals received antipsychotic medication for an average of 192 (± 87) days in any single year and an average of 1,732 (± 788) days across all seven years. There was no difference between first and second generation antipsychotics.
The longitudinal logistic and Poisson regression models were based on the 1,613 individuals with at least some antipsychotic use (Table 2). There was a statistically significant association between the odds of any monthly hospitalization and prior three month antipsychotic use (p < 0.001). Among individuals with similar history of hospitalization, age, gender, race and co-morbid conditions, the odds of at least one hospitalization among light users are approximately 72% (95%CI: 49−100%) greater than the odds among continuous users. Moderate users have odds of at least one hospitalization per month that are 52% (95%CI: 30−75%) greater than the odds among continuous users.
Table 2.
Longitudinal logistic and Poisson regression analyses for any schizophrenia-related hospitalization and resulting days of hospitalization in the current month for from 1993 to 2000.
| Logistic Model for any hospitalization1 | Poisson Model for average length of stay per hospitalization2 | ||
|---|---|---|---|
| OR (95% CI) | RR (95% CI) | ||
| Prior 3 mos. antipsychotic use | Light vs. Continuous | 1.72 (1.49, 2.00) | 1.19 (1.02, 1.39) |
| Light vs. Moderate | 1.14 (0.99, 1.32) | 1.15 (1.00, 1.32) | |
| Moderate vs. Continuous | 1.52 (1.30, 1.75) | 1.04 (0.93, 1.16) | |
| Any hosp in prior 3 mos. | Yes vs. No | 3.08 (2.48, 3.82) | |
| Days of hospitalization in prior 3 mos. | 1−7 vs. 0 days | - | 0.91 (0.69, 1.19) |
| 8−30 vs. 0 days | - | 0.96 (0.83, 1.11) | |
| 31+ vs. 0 days | - | 0.74 (0.47, 1.18) | |
| Type of antipsychotic | Atypical vs. Typical | 1.06 (0.89, 1.26) | 1.08 (0.88, 1.32) |
| Typical vs. Both | 1.12 (0.92, 1.39) | 1.20 (0.99, 1.47) | |
| Aypical vs. Both | 1.19 (0.94, 1.51) | 1.30 (1.03, 1.64) | |
| Ethnicity | White vs. Other | 0.78 (0.65, 0.93) | 0.95 (0.80, 1.13) |
| Gender | Male vs. Female | 1.22 (1.02, 1.45) | 0.95 (0.82, 1.11) |
| Age | > 35 vs. ≤ 35 | 0.85 (0.71, 1.01) | 1.26 (1.12, 1.43) |
| Co-morbidities | Bipolar disorder | 1.48 (1.21, 1.80) | 0.94 (0.83, 1.06) |
| Other MH disorder | 1.85 (1.55, 2.20) | 0.86 (0.76, 0.97) |
Statistically significant difference in odds of any hospitalization comparing anti-psychotic use groups (Wald test with 2 df, p < 0.001). No statistically significant difference in odds of any hospitalization comparing type of antipsychotic (Wald test with 2 df, p = 0.35)
Marginally statistically significant difference in average length of stay per hospitalization comparing anti-psychotic use groups (Wald test with 2 df, p = 0.07) and type of antipsychotic (Wald test with 2 df, p = 0.07). No statistically significant difference in average length of stay per hospitalization comparing days of hospitalization during prior three months (Wald test with 3 df, p = 0.51).
Among subjects with at least one hospitalization in a given month, the average length of stay per hospitalization across magnitude of antipsychotic use is presented as the relative rates (RR). We found a marginally significant association between average length of stay per hospitalization and magnitude of antipsychotic use (p = 0.07). The average length of stay per hospitalization in a given month did not differ significantly between light relative to moderate use. However, the estimated average length of stay per hospitalization for light users is approximately 20% (95%CI: 2−39%) longer compared with continuous users. Ignoring hospitalizations with length of stay at least 60 days, i.e., 1% of all hospitalizations, length of stay per hospitalization was statistically significantly associated with magnitude of use (p=0.012). Specifically, compared to continuous users, light users had an average length of stay that was 15% (95%CI: 5−27%) longer.
Associations between type of antipsychotic used and odds of any hospitalization and lengths of stay were not significant. Results were not sensitive to adjustments for trends in the odds of hospitalization or days of hospitalization or when excluding days of decanoate use in defining the antipsychotic use groups.
1.4 DISCUSSION
This study describes longitudinal patterns that represent chronic maintenance antipsychotic treatment. The lower adherence to antipsychotic treatment associated with a greater frequency and longer duration of schizophrenia-related hospitalizations was consistent with prior research that examined adherence over shorter periods of time (Gilmer et al. 2004; Valenstein et al. 2002; Weiden et al. 2004). Also, the significant association between the degree of adherence and the likelihood of psychiatric hospitalization corroborates previously reported research involving partial antipsychotic adherence. Partially adherent individuals (i.e., 50−79% consumption of medication per days eligible) have lower hospitalization rates than non-adherent persons (i.e., 0−49% consumption per days eligible) and slightly higher rates than those adherent (i.e., 80% or more consumed per days eligible) to antipsychotic medication (Gilmer et al. 2004; Weiden et al. 2004). Lastly, the significant difference between light and continuous antipsychotic use when length of hospitalization was less than 60 days suggests more acute relapse with light use.
Research on differences in continuity between first and second generation agents has been mixed. Evidence from the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) suggests that the 74% treatment discontinuation before 18 months was not significantly different between first generation perphenazine and the second generation agents examined (Lieberman et al. 2005), with the exception of olanzapine, which showed a slight advantage in duration of successful treatment. Using the Health Search Database (HSD) containing data for more than 800,000 individuals followed by 550 general practitioners in Italy, from 1999 to 2002 discontinuation was greater for the second generation than for first generation agents (Trifiro et al. 2005). Discontinuation of antipsychotic medication two years after discharge was similar for first and second generation agents (Fleck et al. 2002). Ours and other studies of outpatient community utilization ( Gilmer et al. 2004; Valenstein et al. 2004) have shown no difference between first and second generation antipsychotics, including olanzapine. This may in part be due to differences between community-based studies and clinical trials. Also, methodological differences in defining continuous treatment could also be a factor. Additional factors, such as denial of an illness, may play a key role in treatment discontinuation (Olfson et al. 2006). Nonetheless, the current study may be more representative of community utilization because it captures periodic fluctuation over time.
The current findings are supported by recommendations for continuous antipsychotic treatment (Lehman et al. 2004). Antipsychotic discontinuation is a significant predictor of relapse (Robinson et al. 1999). Our analysis shows that continuous use was associated with fewer and shorter schizophrenia-related hospitalizations compared to light or moderate use. McCombs and colleagues reported a non-significant trend towards lower hospitalization costs with continuous antipsychotic treatment (McCombs et al. 2000). That individuals in this study who received antipsychotic treatment were more likely to have had a hospitalization for schizophrenia relative to those who did not is counter-intuitive. It may be driven by the initiation of antipsychotic treatment during hospitalization for an acute episode of the illness.
Racial disparities in antipsychotic treatment have been reported in several studies (Bagchi et al. 2004; dosReis et al. 2002; Kilbourne and Pincus 2006; Kreyenbuhl et al. 2003; Mallinger et al. 2006). African-Americans are more likely to receive first generation antipsychotic medications relative to Whites or non-African-Americans (Bagchi et al. 2004; Kilbourne and Pincus 2006; Mallinger et al. 2006). Moreover, African-Americans have a shorter duration of treatment and receive higher daily doses compared to Whites (dosReis et al. 2002). In this study non-Whites were more likely to be classified in light or moderate use whereas Whites were primarily classified as continuous use. Others have similarly reported racial differences in antipsychotic adherence (Gilmer et al. 2004; Valenstein et al. 2004; Valenstein et al. 2002). Models such as assertive community treatment (ACT) have successfully reduced hospitalizations in general, including among ethnic minorities who had language and cultural barriers (Yang et al. 2005), but its effect on antipsychotic compliance awaits further study.
There are several limitations to consider. Treatment patterns may only apply to this one state's Medicaid population aged 62 years or younger at the start of the study. Outpatient antipsychotic treatment may not represent the presumably more severe, chronically institutionalized patients. Lack of a standardized diagnostic assessment may have compromised reliability. Because clinical information is not available in Medicaid data, it was not possible to know if discontinuity of antipsychotic use was related to intolerable side effects. Monthly use of other psychotropic medications was not available, and thus not adjusted for in the longitudinal analyses.
These findings may reflect the inadequacy of community-based service systems in effectively promoting and maintaining the continuity of antipsychotic treatment among individuals with schizophrenia. Awareness of long-term utilization patterns could inform clinical and policy decisions that would maximize adherence.
ACKNOWLEDGEMENT
The authors would like to thank Dr. Gail Daumit for her comments on an earlier version of this manuscript. This work would not have been possible without the kind assistance from the Maryland State Department of Health and Mental Hygiene, and, in particular, the Directors of the Maryland Medical Assistance Program.
ABBREVIATIONS
- PORT
Patient Outcomes Research Team
- SMI
severe mental illness
- HSD
Health Search Database
- MPR
medication possession ratio
- SSRI
selective serotonin reuptake inhibitor
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
1.5 REFERENCES
- APA Practice guideline for the treatment of patients with schizophrenia. American Psychiatric Association (APA). American Journal of Psychiatry. 1997;154(4 (Suppl)):1–63. doi: 10.1176/ajp.154.4.1. [DOI] [PubMed] [Google Scholar]
- Ascione FJ, Brown GH, Kirking DM. Evaluation of a medication refill reminder system for a community pharmacy. Patient Education and Counseling. 1985;7(2):157–165. doi: 10.1016/0738-3991(85)90006-0. [DOI] [PubMed] [Google Scholar]
- Bagchi A, Sambamoorthi U, McSpiritt E, Yanos P, Walkup J, Crystal S. Use of antipsychotic medications among HIV-infected individuals with schizophrenia. Schizophrenia Research. 2004;71(2−3):435–444. doi: 10.1016/j.schres.2004.02.021. [DOI] [PubMed] [Google Scholar]
- dosReis S, Zito JM, Buchanan RW, Lehman AF. Antipsychotic dosing and concurrent psychotropic treatments for Medicaid-insured individuals with schizophrenia. Schizophrenia Bulletin. 2002;28(4):607–617. doi: 10.1093/oxfordjournals.schbul.a006968. [DOI] [PubMed] [Google Scholar]
- Fleck DE, Hendricks WL, DelBello MP, Strakowski SM. Differential prescription of maintenance antipsychotics to African American and white patients with new-onset bipolar disorder. Journal of Clinical Psychiatry. 2002;63(8):658–664. doi: 10.4088/jcp.v63n0802. [DOI] [PubMed] [Google Scholar]
- Gilmer TP, Dolder CR, Lacro JP, Folsom DP, Lindamer L, Garcia P, Jeste DV. Adherence to treatment with antipsychotic medication and health care costs among Medicaid beneficiaries with schizophrenia. American Journal of Psychiatry. 2004;161(4):692–699. doi: 10.1176/appi.ajp.161.4.692. [DOI] [PubMed] [Google Scholar]
- Herz MI, Glazer WM, Mostert MA, Sheard MA, Szymanski HV, Hafez H, Mirza M, Vana J. Intermittent vs maintenance medication in schizophrenia. Two-year results. Archives of General Psychiatry. 1991;48(4):333–339. doi: 10.1001/archpsyc.1991.01810280049007. [DOI] [PubMed] [Google Scholar]
- Kilbourne AM, Pincus HA. Patterns of psychotropic medication use by race among veterans with bipolar disorder. Psychiatric Services. 2006;57(1):123–126. doi: 10.1176/appi.ps.57.1.123. [DOI] [PubMed] [Google Scholar]
- Kreyenbuhl J, Zito JM, Buchanan RW, Soeken KL, Lehman AF. Racial disparity in the pharmacological management of schizophrenia. Schizophrenia Bulletin. 2003;29(2):183–193. doi: 10.1093/oxfordjournals.schbul.a006996. [DOI] [PubMed] [Google Scholar]
- Lehman AF, Kreyenbuhl J, Buchanan RW, Dickerson FB, Dixon LB, Goldberg R, Green-Paden LD, Tenhula WN, Boerescu D, Tek C. The Schizophrenia Patient Outcomes Research Team (PORT): updated treatment recommendations 2003. Schizophrenia Bulletin. 2004;30(2):193–217. doi: 10.1093/oxfordjournals.schbul.a007071. others. [DOI] [PubMed] [Google Scholar]
- Lehman AF, Steinwachs DM, Co-Investigators of the PORT Project At issue: Translating research into practice: The schizophrenia patient outcomes research team (PORT) treatment recommendations. Schizophrenia Bulletin. 1998;24(1):1–10. doi: 10.1093/oxfordjournals.schbul.a033302. [DOI] [PubMed] [Google Scholar]
- Lehman AF, Thompson JW, Dixon LB, Scott JE. Schizophrenia: treatment outcomes research. Schizophrenia Bulletin. 1995;21(4):561–566. doi: 10.1093/schbul/21.4.561. [DOI] [PubMed] [Google Scholar]
- Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, Keefe RS, Davis SM, Davis CE, Lebowitz BD. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. New England Journal of Medicine. 2005;353(12):1209–1223. doi: 10.1056/NEJMoa051688. others. [DOI] [PubMed] [Google Scholar]
- Mallinger JB, Fisher SG, Brown T, Lamberti JS. Racial disparities in the use of second-generation antipsychotics for the treatment of schizophrenia. Psychiatric Services. 2006;57(1):133–136. doi: 10.1176/appi.ps.57.1.133. [DOI] [PubMed] [Google Scholar]
- McCombs JS, Nichol MB, Johnstone BM, Stimmel GL, Shi J, Smith R. Antipsychotic drug use patterns and the cost of treating schizophrenia. Psychiatric Services. 2000;51(4):525–527. doi: 10.1176/appi.ps.51.4.525. [DOI] [PubMed] [Google Scholar]
- McCombs JS, Nichol MB, Stimmel GL, Shi J, Smith RR. Use patterns for antipsychotic medications in Medicaid patients with schizophrenia. Journal of Clinical Psychiatry. 1999;60(Suppl 19):5–11. [PubMed] [Google Scholar]
- Menzin J, Boulanger L, Friedman M, Mackell J, Lloyd JR. Treatment adherence associated with conventional and atypical antipsychotics in a large state Medicaid program. Psychiatric Services. 2003;54(5):719–723. doi: 10.1176/appi.ps.54.5.719. [DOI] [PubMed] [Google Scholar]
- Mojtabai R, Lavelle J, Gibson PJ, Sohler NL, Craig TJ, Carlson GA, Bromet EJ. Gaps in the use of antipsychotics after discharge by first-admission patients with schizophrenia, 1989−1996. Psychiatric Services. 2002;53(3):337–339. doi: 10.1176/appi.ps.53.3.337. [DOI] [PubMed] [Google Scholar]
- Olfson M, Marcus SC, Wilk J, West JC. Awareness of illness and nonadherence to antipsychotic medications among persons with schizophrenia. Psychiatric Services. 2006;57(2):205–211. doi: 10.1176/appi.ps.57.2.205. [DOI] [PubMed] [Google Scholar]
- Robinson D, Woerner MG, Alvir JM, Bilder R, Goldman R, Geisler S, Koreen A, Sheitman B, Chakos M, Mayerhoff D. Predictors of relapse following response from a first episode of schizophrenia or schizoaffective disorder. Archives of General Psychiatry. 1999;56(3):241–7. doi: 10.1001/archpsyc.56.3.241. others. [DOI] [PubMed] [Google Scholar]
- Schooler NR. Relapse prevention and recovery in the treatment of schizophrenia. Journal of Clinical Psychiatry. 2006;67(Suppl 5):19–23.. [PubMed] [Google Scholar]
- Schulz RM, Gagnon JP. Patient behavior patterns regarding prescription refills. Contemporary Pharmacy Practice. 1982;5(3):150–155. [PubMed] [Google Scholar]
- Trifiro G, Spina E, Brignoli O, Sessa E, Caputi AP, Mazzaglia G. Antipsychotic prescribing pattern among Italian general practitioners: a population-based study during the years 1999−2002. European Journal of Clinical Pharmacology. 2005;61(1):47–53. doi: 10.1007/s00228-004-0868-3. [DOI] [PubMed] [Google Scholar]
- Valenstein M, Blow FC, Copeland LA, McCarthy JF, Zeber JE, Gillon L, Bingham CR, Stavenger T. Poor antipsychotic adherence among patients with schizophrenia: medication and patient factors. Schizophrenia Bulletin. 2004;30(2):255–264. doi: 10.1093/oxfordjournals.schbul.a007076. [DOI] [PubMed] [Google Scholar]
- Valenstein M, Copeland LA, Blow FC, McCarthy JF, Zeber JE, Gillon L, Bingham CR, Stavenger T. Pharmacy data identify poorly adherent patients with schizophrenia at increased risk for admission. Medical Care. 2002;40(8):630–639. doi: 10.1097/00005650-200208000-00002. [DOI] [PubMed] [Google Scholar]
- Vanelli M, Burstein P, Cramer J. Refill patterns of atypical and conventional antipsychotic medications at a national retail pharmacy chain. Psychiatric Services. 2001;52(9):1248–1250. doi: 10.1176/appi.ps.52.9.1248. [DOI] [PubMed] [Google Scholar]
- Velligan DI, Lam F, Ereshefsky L, Miller AL. Perspectives on medication adherence and atypical antipsychotic medications. Psychiatric Services. 2003;54(5):665–667. doi: 10.1176/appi.ps.54.5.665. [DOI] [PubMed] [Google Scholar]
- Verdoux H, Lengronne J, Liraud F, Gonzales B, Assens F, Abalan F, van Os J. Medication adherence in psychosis: predictors and impact on outcome. A 2-year follow-up of first-admitted subjects. Acta Psychiatrica Scandinavica. 2000;102(3):203–210. doi: 10.1034/j.1600-0447.2000.102003203.x. [DOI] [PubMed] [Google Scholar]
- Weiden PJ, Kozma C, Grogg A, Locklear J. Partial compliance and risk of rehospitalization among California Medicaid patients with schizophrenia. Psychiatric Services. 2004;55(8):886–891. doi: 10.1176/appi.ps.55.8.886. [DOI] [PubMed] [Google Scholar]
- Williams CL, Johnstone BM, Kesterson JG, Javor KA, Schmetzer AD. Evaluation of antipsychotic and concomitant medication use patterns in patients with schizophrenia. Medical Care. 1999;37(4):AS81–AS86. doi: 10.1097/00005650-199904001-00011. [DOI] [PubMed] [Google Scholar]
- Yang J, Law S, Chow W, Andermann L, Steinberg R, Sadavoy J. Best practices: assertive community treatment for persons with severe and persistent mental illness in ethnic minority groups. Psychiatric Services. 2005;56(9):1053–1055. doi: 10.1176/appi.ps.56.9.1053. [DOI] [PubMed] [Google Scholar]


