Abstract
Natural killer (NK) cells have innate antibacterial activity that could be targeted for clinical interventions for infectious disease caused by naturally occurring or weaponized bacterial pathogens. To determine a potential role for NK cells in immunity to Bacillus anthracis, we utilized primary human and murine NK cells, in vitro assays, and in vivo NK cell depletion in a murine model of inhalational anthrax. Our results demonstrate potent antibacterial activity by human NK cells against B. anthracis bacilli within infected autologous monocytes. Surprisingly, NK cells also mediate moderate antibacterial effects on extracellular vegetative bacilli but do not have activity against extracellular or intracellular spores. The immunosuppressive anthrax lethal toxin impairs NK gamma interferon (IFN-γ) expression, but neither lethal nor edema toxin significantly alters the viability or cytotoxic effector function of NK cells. Compared to human NK cells, murine NK cells have a similar, though less potent, activity against intracellular and extracellular B. anthracis. The in vivo depletion of murine NK cells does not alter animal survival following intranasal infection with B. anthracis spores in our studies but significantly increases the bacterial load in the blood of infected animals. Our studies demonstrate that NK cells participate in the innate immune response against B. anthracis and suggest that immune modulation to augment NK cell function in early stages of anthrax should be further explored in animal models as a clinical intervention strategy.
INTRODUCTION
Bacillus anthracis is a Gram-positive, spore-forming, rod-shaped bacterium and the etiologic agent of inhalational, cutaneous, and gastrointestinal anthrax infections. Spores from this agent have been used as a bioterrorism weapon and are considered particularly hazardous because of their ability to resist heat, dryness, sunlight, and other factors that limit the viability of bacterial pathogens. The most severe form of the infection (inhalational) presents itself as a cold or flu lasting several days, eventually leading to respiratory failure and death. The availability of preventive or therapeutic measures to combat anthrax in the general public is very limited (3, 8). Vaccination for anthrax in the United States involves a multiple-injection dosing schedule with anthrax vaccine adsorbed (AVA), also known as Biothrax, and is available only to those with a high risk of exposure to B. anthracis (8). Annual booster injections with AVA, an aluminum hydroxide-adsorbed, sterile culture filtrate of B. anthracis, are required to maintain immunity. Additionally, postexposure antibiotics have been utilized as a prophylactic for individuals exposed to or potentially exposed to B. anthracis spores (3). The effectiveness of these antibiotics, however, is dependent on early administration after exposure and patient compliance for a prolonged period of therapy. Thus, there is a need to develop additional and more effective clinical interventions to prevent morbidity and mortality due to Bacillus anthracis infection.
The potential to target the innate immune system through clinical modulation is of interest for reducing infectious disease caused by many pathogens. Natural killer (NK) cells are an important component of the innate immune system and have been extensively examined for contributions to tumor cell eradication and for roles in viral and parasitic clearance (21). More recently, the role and function(s) of NK cells in response to various bacterial infections have begun to be defined. NK cells (which are potent producers of gamma interferon [IFN-γ] and cytotoxic granule proteins) have antibacterial activity and reduce the level of bacteremia or sepsis in bacterially infected hosts (9, 14, 16, 29). Following infection, NK cell action in the innate immune response to tumors or virus occurs through lytic activity against infected or altered host cells. A role for NK cells in the clearance of bacterial pathogens is generally understood to occur via the activation of infected cells (e.g., macrophages) by NK cell-derived IFN-γ or through the cytotoxic attack of infected cells (12, 27). Previous studies of murine splenocyte responses to a laboratory strain of B. anthracis suggested that the activation of NK cell IFN-γ can occur (15), although the induction of IFN-γ in that model was sensitive to the suppressive activity of B. anthracis lethal toxin (LT). Our recent work demonstrated that granulysin, an antimicrobial protein restricted to the granules of human NK cells and cytotoxic lymphocytes, had potent lytic activity against a highly pathogenic B. anthracis isolate (Ames) (10). To date, however, the immune contribution of human NK cells during B. anthracis infection has not been defined. Furthermore, the role of murine NK cells in experimental models used to study human inhalational anthrax has also not been described.
In the current studies, we demonstrate that human NK cells are not active against spores but efficiently reduce CFU of B. anthracis when exposed to both infected autologous monocytes (MN) and extracellular bacilli. Furthermore, anthrax lethal toxin (LT) suppresses the NK cell expression of IFN-γ but does not impair proliferative responses, cytotoxic activity, or the expression of the antibacterial protein granulysin. We further observed that murine NK cells also have antibacterial activity against B. anthracis, although the potency is less than that of human NK cells. Results from the in vivo depletion of asialo GM1+ cells show that NK cells contribute to the control of bacteremia in a murine pulmonary anthrax model. Overall, our studies demonstrate that NK cells can have an antibacterial role that contributes to the host defense against B. anthracis, can be investigated further in a relevant animal model of inhalational anthrax, and could be a candidate mechanism to target by immune modulation for clinical intervention in cases of anthrax.
MATERIALS AND METHODS
Bacteria.
Spores were prepared by inoculating B. anthracis (Ames strain) in Schaeffer's sporulation medium (pH 7.0) with 16 g Difco nutrient broth. Prior to inoculation and after filter sterilization, 0.1% glucose, 1 mM Ca(NO3)2, 0.1 mM MnSO4, and 1 μM FeSO4 were added to the medium. Cultures were grown in 50-ml aliquots at 37°C with gentle shaking for 48 h. Subsequently, 100 ml of sterile distilled water was added to dilute the medium and to promote sporulation. After 10 days of continuous shaking, sporulation was confirmed by using phase-contrast microscopy and a modified Wirtz-Conklin spore stain (19, 20) The spores were centrifuged in a sealed-carrier centrifuge at 4°C for 15 min at 630 × g. Spore pellets were then washed four times in Cellgro sterile water and finally resuspended in sterile water. The spore suspension was layered onto a cushion of 58% Hypaque-76 at a ratio of 1:2.5 by volume. The tubes were centrifuged with a JA 25.50 rotor for 45 min at 4°C in an Avanti J-20XPI refrigerated centrifuge. The Hypaque supernatant was decanted, and the pellet was washed with sterile water and resuspended in sterile water. Aliquots of the suspension were then stored at −80°C until they were used to challenge mice in a restricted-access biosafety level 3 (BSL-3) animal facility registered with the Centers for Disease Control and Prevention and inspected by the Department of Defense and the U.S. Department of Agriculture. For in vitro studies, B. anthracis bacilli were cultured by plating 10 μl of the spore stock onto BBL Trypticase soy agar with 5% sheep blood plates (BD, Franklin Lakes, NJ) overnight. A single colony from this plate was then inoculated into 2 ml of LB medium (Sigma, St. Louis, MO) for 12 h at 220 rpm at 37°C. One hundred microliters of this stock was then taken, placed into 10 ml of fresh LB medium, and grown to log phase overnight (22, 23).
Isolation of human blood monocytes and NK cells.
Peripheral blood was obtained by venipuncture from healthy individuals aged 21 to 49 years as approved by the University of Texas Medical Branch (UTMB) Institutional Review Board. Peripheral blood mononuclear cells (PBMCs) were isolated by density gradient centrifugation using Accuprep (Accurate Chemicals, Westbury, NY). Monocytes (MN) were positively selected by using CD14+ MicroBeads (Miltenyi Biotech, Auburn, CA) with the AutoMacs system and cultured with 1,400 U/ml granulocyte-macrophage colony-stimulating factor (GM-CSF) as we have previously described (9). NK cells were negatively selected by using an NK cell isolation kit (Miltenyi Biotech) and cultured with medium alone or recombinant human interleukin-15 (rhIL-15) (15 ng/ml; R&D Systems). In some experiments, monocyte-depleted PBMCs were used to validate the activity of B. anthracis toxins by measuring effects on T cells. T cells were activated by using magnetic bead-bound antibodies to human CD3 and CD28 (Dynabeads; Invitrogen) to activate T cells through the engagement of the T cell receptor, as recommended by the manufacturer. Cells were maintained in complete culture medium, RPMI 1640 supplemented with 10% fetal bovine serum (FBS), 2 mM l-glutamine, 1 mM sodium pyruvate, 0.1 mM nonessential amino acids, and penicillin-streptomycin (cRPMI) (Invitrogen). The determination of NK cell viability for non-toxin-related experiments was performed by an analysis of trypan blue exclusion. Assessments of cell viability due to toxin treatment were performed by using an annexin V-phycoerythrin (PE) apoptosis detection kit (BD Biosciences), and results were read by using a FACSCanto flow cytometer (UTMB Flow Cytometry and Cell Sorting Core Facility).
In vitro exposure to toxins.
Protective antigen (PA), lethal factor (LF), and edema factor (EF) were obtained from the Biodefense and Emerging Infections Research Resources Repository (BEI Resources, Manassas, VA) and stored at −80°C prior to use. Purified NK cells were treated with no toxin (NT), the PA component, LT, or edema toxin (ET) as previously described (5). Briefly, NK cells were incubated with PA (2.5 μg/ml), ET (2.5 μg/ml of PA and 0.625 μg/ml of EF), LT (1 μg/ml of PA and 0.2 μg/ml of LF), or both ET and LT for 1 h prior to the addition of medium (control) or rIL-15. Similarly, PBMCs were exposed to toxins for 1 h prior to incubation with human CD3/CD28 bead-conjugated antibodies.
Flow cytometry.
Purified NK cells or PBMCs were harvested at the indicated times and labeled with antibodies (BD Biosciences) specific to human surface markers: CD56-peridinin chlorophyll protein (PerCP-Cy5.5) and CD3-allophycocyanin (APC)-Cy7. Cells were washed and permeabilized by using the BD Cytofix/Cytoperm kit (BD Biosciences), followed by labeling with antibodies (BD Biosciences) to intracellular granulysin-Alexa 488, Ki67-PE or perforin PE, and IFN-γ–APC. Finally, cells were washed and resuspended in 400 μl of 2% ultrapure formaldehyde (Polysciences Inc.). A total of 50,000 cells were acquired on a FACSCanto instrument (BD Biosciences), and compensation for spectral overlap was performed by using FACS DIVA software (BD Biosciences). Isotype- and fluorochrome-matched nonspecific control antibodies were used to determine background fluorescence. Analysis was performed by using FCS Express, version 3 (De Novo Software), as we have previously described (18). Data are presented as results of CD56+ CD3− and CD3+ CD56− gated events corresponding to NK cells and T cells, respectively.
Assessment of human NK cell antibacterial activity.
Isolated MN were divided into aliquots in duplicate wells (105 cells per well) of flat-bottomed 96-well tissue culture plates (Corning) for CFU assessments for each treatment to be studied. Following overnight incubation to allow adherence, supernatants were removed, and cells were carefully washed three times with antibiotic-free medium. MN were then infected at a 1:1 bacterium-to-MN infecting ratio with B. anthracis Ames bacilli in 50 μl of antibiotic-free cRPMI per well, as we have previously described for assessing NK cell activity against mycobacteria (9). Plates were returned to a 37°C incubator for 1 h, at which time the supernatants were gently aspirated and each well was washed three times with RPMI 1640 with 10% fetal bovine serum and 50 μg/ml gentamicin to remove extracellular bacilli. Wells were then refilled with 100 μl of antibiotic-free cRPMI alone or containing NK cells from the same donor. Various ratios of NK cells (5:1, 1:1, 0.5:1, 0.1:1, and 0:1 NK cell/MN ratios and NK cell/bacterium ratios in 100 ml) were added to autologous infected MN and to wells containing 105 CFU of B. anthracis (Ames) bacilli. Following 24 h or coculture, the cells were lysed with 250 μl of 1% Triton X-100 per well. CFU were determined by limiting-dilution growth on blood agar plates, and counts were taken after 48 h of growth as previously described (22). These experiments were repeated by using spores treated with d-histidine and d-alanine to inhibit germination, as previously described (19). Briefly, spores and monocytes were treated with 2 mM d-histidine and 2 mM d-alanine (Sigma) for 1 h, and spores were heated to 65°C for 30 min to inactivate vegetative bacteria. Spores were used to infect monocytes at a 1:1 spore-to-MN ratio added directly to medium. Medium containing d-alanine and d-histidine was used throughout the infection and culture period. Infected MN or free spores were cultured in the presence or absence of a 5:1 effector-to-target (E/T) ratio of NK cells, and the enumeration of heat-resistant CFU was performed by limiting-dilution plating as described above for the enumeration of vegetative bacilli.
Assessment of human NK cell cytotoxic activity.
Cytotoxic NK cell activity was measured by using the K562 human leukemia cell line (ATCC 45506) as we have previously described (9). K562 cells were maintained in cRPMI, and 1 day prior to use, 10 μl/ml of DIOC (3,3′-dihexyloxacarbocyanine iodide; Sigma) was added to fluorescently label K562 cells as previously described (9). NK cells were treated with NT, PA, LT, ET, or LT plus ET for 1 h, and 15 ng/ml of IL-15 or carrier (medium) was then added. Following overnight incubation, NK cells were counted and placed into tubes at various E/T ratios (10:1, 5:1, 1:1, 0.1:1, and 0:1) with 20,000 DIOC-labeled K562 cell targets. Propidium iodide (PI) was then added to each tube, and tubes were incubated at 37°C for 2 h. Following incubation, tubes were analyzed immediately by flow cytometry, and cytotoxic T lymphocyte (CTL) activity was determined based on the percentage of nonviable (PI-positive) DIOC-labeled K562 target cells following incubation with NK cells compared to spontaneous death during the 2-h culture period in the absence of NK cells.
Scanning electron microscopy.
To visualize interactions between NK cells and extracellular B. anthracis (Ames), cultures were incubated as described above for 1 or 3 h. The samples were mounted onto Thermanox coverslips coated with 1% poly-l-lysine and then fixed in a mixture of 2% formaldehyde and 2% glutaraldehyde in 0.1 M cacodylate buffer (pH 7.2) for at least 4 to 6 h, postfixed in 1% OsO4 in 0.1 M cacodylate buffer, dehydrated in ethanol, processed through hexamethyldisilazane (HMDS), and air dried. The coverslips were mounted onto the stubs and sputter coated with iridium in an Emitech K575x sputter coater (Ashford, Kent, England) at 20 mA for 20 s. Samples were examined with a Hitachi S-4700 scanning electron microscope (Hitachi High Technologies America, Inc.) at 2 kV.
Transmission electron microscopy.
NK cells and bacteria were cultured as described above for the performance of scanning electron microscopy (SEM). Cell/bacterial pellets were then fixed in a mixture of 2.5% formaldehyde and 0.1% glutaraldehyde in 0.05 M cacodylate buffer (pH 7.2) containing 0.03% trinitrophenol and 0.03% CaCl2 and washed in 0.1 M cacodylate buffer (pH 7.2). The pellets were postfixed in 1% OsO4 in the same buffer, stained en bloc with 2% aqueous uranyl acetate, dehydrated in ethanol, and embedded in Poly/Bed 812 epoxy resin (Polysciences, Warrington, PA). Ultrathin sections were cut on a Reichert-Leica Ultracut S ultramicrotome, stained with lead citrate, and examined with a Philips 201 or CM 100 electron microscope at 60 kV.
Isolation of murine MN and NK cells.
Spleens were harvested from 6- to 8-week-old female Swiss Webster mice (Taconic Farms, Georgetown, NY) following sacrifice as approved by the Institutional Animal Care and Use Committee. Single-cell suspensions were prepared from harvested spleens following tissue disruption as previously described (5), and PBMCs were isolated by density gradient centrifugation as described above for human PBMCs. MN were obtained by allowing 2 h of adherence to tissue culture-treated flasks. Purified mouse NK cells were obtained by magnetic bead-based sorting using the DX5 antibody (Miltenyi). The isolated monocytes were then plated at 105 monocytes/well in 96-well tissue culture plates and provided 1,400 U/ml of recombinant GM-CSF. The determination of antibacterial activity against free bacteria or infected monocytes was performed as described above for human NK cells using a 5:1 ratio of murine NK cells to B. anthracis-infected MN or B. anthracis bacilli.
In vivo NK cell depletion.
Rabbit anti-asialo GM1 antibody (Wako Chemical Company, Richmond, VA) was used to deplete NK cells as previously described (8). The commercial product was reconstituted with 2 ml of sterile water, and a 1:10 dilution was used for injection. Mice were injected with 200 μl (50 μg/mouse) of the anti-asialo GM1 antibody preparation or control rabbit serum (Sigma) via the intraperitoneal (i.p.) route for two doses at 3 days prior to challenge and 2 days postchallenge with B. anthracis Ames spores. Depletion was confirmed by the flow cytometric detection of mouse NK cells, at 2 and 5 days postdepletion, in two uninfected mock-depleted and two uninfected NK cell-depleted animals. Animals were sacrificed, and spleens were processed into single-cell suspensions, as previously described (5). The detection of murine NK cells was performed by the labeling of total splenocytes with the DX5 marker using a directly conjugated fluorescent (fluorescein isothiocyanate [FITC]) antibody by using flow cytometry procedures that were previously described (18).
Animal infections.
Specific-pathogen-free (SPF) 6- to 8-week-old female Swiss Webster mice were purchased from Taconic Farms and housed in the Association for Assessment and Accreditation of Laboratory Animal Care-accredited Animal Resources Center at UTMB. Mice were anesthetized with an i.p. injection of ketamine-HCl (90 mg/kg of body weight) and xylazine-HCl (10 mg/kg). After anesthesia, the mice were suspended by their front incisors to facilitate nasal inoculation. Mice were given 5 50% lethal doses (LD50) (approximately 5.6 × 104 CFU) of B. anthracis Ames strain spores in 40 μl of phosphate-buffered saline (PBS), after which the mice remained suspended for an additional 1 to 2 min to ensure a complete lung inoculation. Subsequently, the mice were returned to their cages for the appropriate incubation time. Two animals per treatment per time point were used in survival studies, while 5 animals from each treatment group were sacrificed at 18 and 36 h for the evaluation of pathology and tissue and blood bacterial loads. All animal experiments were performed in accordance with the regulations of the UTMB Institutional Animal Care and Use Committee and the NIH Office of Laboratory Animal Welfare.
Assessment of tissue bacterial load.
At 18 and 36 h postinfection, infected mice were anesthetized, followed by euthanasia using CO2 narcosis. Cervical dislocation was subsequently performed to ensure death, as approved by the University of Texas Medical Branch Institutional Animal Care and Use Committee. Five hundred microliters of blood was taken first from 5 mice via cardiac puncture and placed into 1.3-ml microtubes coated with EDTA. After blood was collected, lungs were aseptically removed from 5 mice and placed into 1 ml of PBS in 50-ml Kendall tissue homogenizers (Kendall, Mansfield, MA). Following the homogenization of the tissues in the biological safety cabinet in our CDC-approved biological safety level 2 (BSL-2) laboratory or animal BSL-3 facility, serial dilutions of blood and lung samples were prepared in PBS, and 100 μl of each dilution was plated onto 5% sheep blood agar plates (BD Biosciences, Franklin Lakes, NJ). CFU was determined following 48 h of growth as previously described (22). Additionally, an aliquot of blood and disrupted tissue was also used to inoculate liquid growth medium to determine if bacteria were present. Samples were identified as being positive or negative for bacteria following 48 h of growth in liquid media and CFU enumeration on blood agar.
Pathology.
At 18 and 36 h postinfection, the aseptic collection of lungs was performed as described above. The tissues were fixed in 4% paraformaldehyde for 48 h and tested for viable bacteria by plating onto blood agar plates. Tissue sections were routinely processed, embedded in paraffin, sectioned at 5 μm, stained with hematoxylin and eosin (H&E), and evaluated by light microscopy. Tissue lesions were scored based on a severity scale of minimal, mild, moderate, and marked; the scale correlated with estimates of lesion distribution and the extent of tissue involvement (i.e., minimal, 2 to 10%; mild, >10 to 20%; moderate, >20 to 50%; severe, >50%). Acute inflammation indicated the presence of polymorphonuclear leukocytes (PMN). In some sections, bacteria consistent with Bacillus anthracis were present, although bacterial special staining was not performed. This work was performed at the University of Texas M. D. Anderson Cancer Center.
Statistics.
Data are shown as the treatment means ± standard errors of the means (SEM). Statistical differences were determined by using a one-way analysis of variance (ANOVA) followed by Dunnett's multiple-comparison test for group comparisons (GraphPad software v5.0; GraphPad, San Diego, CA).
RESULTS
Human NK cells mediate killing of pathogenic B. anthracis bacilli.
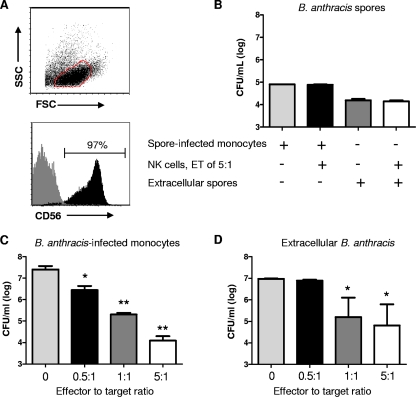
To determine the potential for human NK cells to have a role in the host defense against B. anthracis, peripheral blood NK cells were isolated from healthy human donors. The isolation of NK cells by magnetic bead-based procedures yielded highly purified populations (range of 95 to 99%), as shown by a representative flow plot in Fig. 1A. B. anthracis spores were not sensitive to the effects of NK cells, within either infected monocytes or the extracellular medium, as shown in Fig. 1B. However, NK cells were able to mediate the killing of intracellular and, surprisingly, even extracellular B. anthracis in the vegetative form within 24 h of coculture, as shown in Fig. 1C and D. NK cells in close contact with free B. anthracis bacilli could be observed by scanning and transmission electron microscopy (data not shown). The NK cell reduction of CFU in infected monocytes was substantial, with a 3-log-fold reduction observed at an effector-to-target (E/T) ratio of 5:1. A significant (P < 0.05) reduction of intracellular bacteria was seen for E/T ratios of 5:1, 1:1, and 0. 5:1, and a significant reduction of extracellular bacteria was seen at E/T ratios of 1:1 and 5:1 (Fig. 1C). For subsequent experiments, a 5:1 E/T ratio of NK cells to infected MN or free bacteria was used.
Fig 1.
Antibacterial activity of human NK cells against B. anthracis. Natural killer cells were isolated by use of a magnetic bead-based antibody from PBMCs of healthy human donors. (A) Flow cytometric analysis of NK cell purity, side-scatter (SSC) and forward-scatter (FSC) characteristics of isolated cells, and percentages of isolated cells positive for the human NK marker CD56. (B to D) CFU of B. anthracis (Ames strain) assessed following in vitro coculture of primary human NK cells with spore-infected autologous monocytes or extracellular spores (B), B. anthracis-infected autologous monocytes (C), or extracellular bacilli (D). An effector-to-target (E/T) ratio of 5:1 was used for the determination of antibacterial activity of NK cells (effectors) against spores or spore-infected monocytes (targets). The activity of NK cells against vegetative bacteria within monocytes or growing in medium was determined by using E/T cell ratios of 0.25:1, 0.5:1, 1:1, and 5:1. The enumeration of CFU was performed by limiting dilution following 24 h of CD56+ NK cell exposure to infected monocytes or extracellular vegetative bacteria or spores. Values shown are the means ± SEM of results from 4 individual donors, with experiments performed in duplicate. *, P < 0.05; ***, P < 0.00 (P values indicate statistically significant differences in CFU between control samples and samples cultured with NK cells).
B. anthracis toxins do not impair NK cell cytotoxic/antibacterial function.
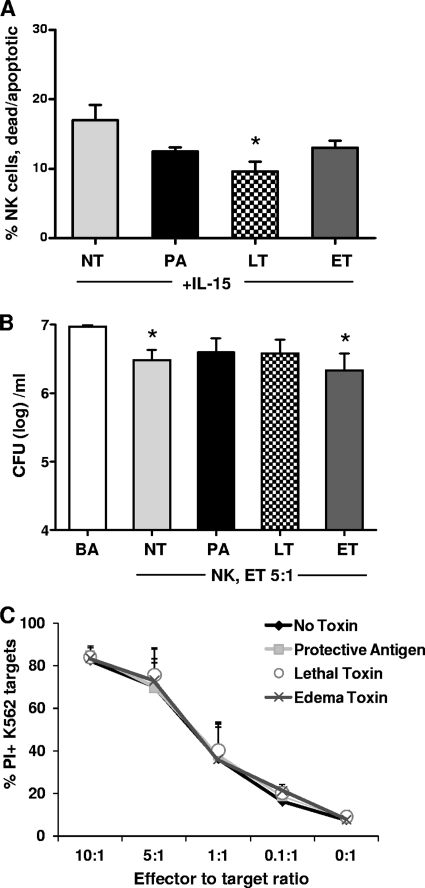
B. anthracis toxins, lethal toxin (LT) and edema toxin (ET), encoded by plasmid pX01, are major contributors to pathology during anthrax infection. Because previous studies have shown that these toxins can affect the functions of other immune cells (2, 5–7, 13), we sought to determine whether exposure to these toxins also had an effect on NK cells. To determine the general effects of toxins on NK cell viability, IL-15 (an important homeostasis and growth factor for NK cells) was added to purified NK cells treated with toxins or left untreated. After 24 h of exposure, the percentages of dead and apoptotic cells due to toxin treatment were compared to the spontaneous death/apoptosis in the NT group (Fig. 2A). Surprisingly, the toxin-treated cells were moderately more viable than the nontreated group, and this effect was significant with LT. As shown in Fig. 2, the antibacterial activity of NK cells against B. anthracis bacilli (Fig. 2B) and host cell targets (Fig. 2C) was not impaired due to exposure to anthrax toxins. Although NK cells treated with LT did not mediate a significant reduction of bacilli compared to the NT group (Fig. 2B), these effects were minimal and were similar to those observed following treatment with the PA component. In all measurements, the effects of LT and ET were evaluated to determine the potential for additive or synergistic effects, and none were noted (data not shown). Thus, the viability and CTL function of NK cells are not impaired due to 24 h of exposure to LT, ET, or both.
Fig 2.
Effects of B. anthracis LT and ET on NK cell antibacterial and cytotoxic function. Natural killer cells were isolated by use of a magnetic bead-conjugated antibody from PBMCs of healthy human donors and cultured with rIL-15 (15 ng/ml). (A) Flow cytometric analysis of NK cell viability, displayed as percent propidium iodide-positive annexin V-positive (dead/apoptotic) NK cells following 24 h of exposure to no toxin (NT), the protective antigen (PA) component, lethal toxin (LT), or edema toxin (ET). (B) CFU of B. anthracis (BA) bacilli following 24 h of in vitro coculture in media or with primary human NK cells (E/T ratio of 5:1) exposed to NT, PA, LT, or ET. (C) Cytotoxicity of NK cells treated with NT, PA, LT, or ET against the classical NK cell target K562 cells, displayed as percent PI-positive K562 cells. Values shown are the means ± SEM of results from 4 individual donors. *, P < 0.05 (P values indicate statistically significant differences due to treatment compared to NT [A] or B. anthracis [B]).
LT suppresses NK cell activation of IFN-γ.
Here we evaluated the potential for toxins to interfere with the activation of NK cell proliferation and effector molecule expression in response to positive stimuli. In these experiments, human IL-15 was again used as a positive stimulus to activate proliferation and effector molecule expression. The same measurements were simultaneously performed by using human T cells from the same donor, as LT and ET were previously shown to suppress murine T cell activation (5). T cells were activated with magnetic bead-conjugated antibodies to CD3 and CD28. As shown by representative donor data in Fig. 3A, T cells were strongly activated to proliferate (Ki67 cell cycle marker) and expressed increased levels of granulysin and IFN-γ in response to T cell receptor (TCR) engagement. Exposure to LT reduced the T cell expression levels of both granulysin and IFN-γ upon activation, while proliferation was not affected (Fig. 3A). ET did not have suppressive effects on the T cell parameters measured here, while treatment with LT plus ET produced effects similar to those of LT (data not shown). Consistent with the responses observed for T cells, NK cells proliferated following activation with IL-15, and this response was not impaired by LT (Fig. 3B) or ET (data not shown). In contrast to T cells, the NK cell expression of granulysin was not significantly impaired by LT, although moderate suppression was observed for some donors (Fig. 3B and C). LT exposure suppressed IFN-γ expression by activated NK cells of several donors and reached statistical significance with the inclusion of 6 individual donors (Fig. 3B and D). Overall, our results show that similarly to T cells, LT suppresses the capacity for NK cells to secrete IFN-γ upon activation. The expression of the antibacterial granulysin protein by activated NK cells, at least in response to IL-15, however, is not impaired by toxin exposure.
Fig 3.
B. anthracis LT suppresses activation of NK cell IFN-γ and T cell granulysin. Purified NK cells or PBMCs were rested (medium) or exposed to PA (negative control), LT, or ET and activated with IL-15 (15 ng/ml) or antibodies to CD3 and CD28. (A and B) Flow cytometric results of CD3+ CD56− (T cell; n = 4) (A) and CD56+ CD3− (NK cell; n = 6) (B) events from a representative donor. The results displayed are the effects of LT on the activation of T cell or NK cell proliferation (Ki67 proliferation marker) and the expression of intracellular granulysin and IFN-γ activated by IL-15 or CD3/CD28. (C and D) Summarized flow cytometry results for the expression of granulysin and IFN-γ by NK cells affected by exposure to LT or ET. Summarized values shown in panels C and D are the means ± SEM of results from 6 individual donors. *, P < 0.05 (P values indicate statistically significant differences due to treatment compared to the NT treatment).
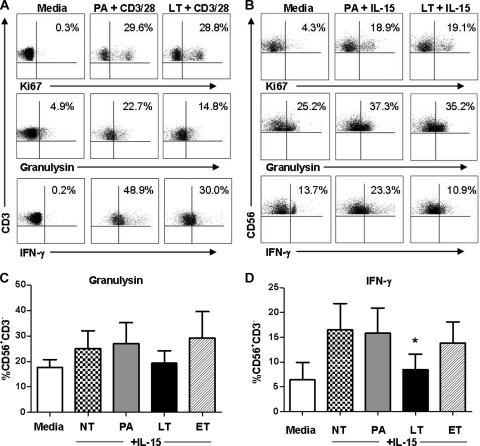
Murine NK cells also have antibacterial activity against B. anthracis.
The antibacterial activity of murine NK cells against B. anthracis has not been described. To determine the potential to study the role of NK cells in a murine model of B. anthracis infection, we used DX5+ cells isolated from splenocytes of healthy mice and repeated the antibacterial activity experiments that we performed with human NK cells. As illustrated in Fig. 4, murine NK cells were able to mediate the killing of intracellular and extracellular B. anthracis within 24 h at a 5:1 E/T ratio.
Fig 4.
In vitro antibacterial activity of murine NK cells against B. anthracis. NK cells were isolated from single-cell suspensions of spleens from Swiss Webster mice by magnetic bead-based isolation using an antibody to DX5. CFU of extracellular and intracellular B. anthracis was assessed in vitro following the addition of murine DX5+ NK cells to infected monocytes (A) or extracellular bacteria (B) at an E/T ratio of 5:1. The results indicate the means and standard deviations (SD) from 6 mice pooled into 3 groups. Values are means ± SEM of these determinations. Enumeration of CFU was performed by limiting dilution following 24 h of NK cell exposure to infected monocytes or extracellular vegetative bacteria or spores. Values shown are the means ± SEM of results from 6 animals. *, P < 0.05; ***, P < 0.001 (P values indicate statistically significant differences in CFU between control samples and samples cultured with NK cells).
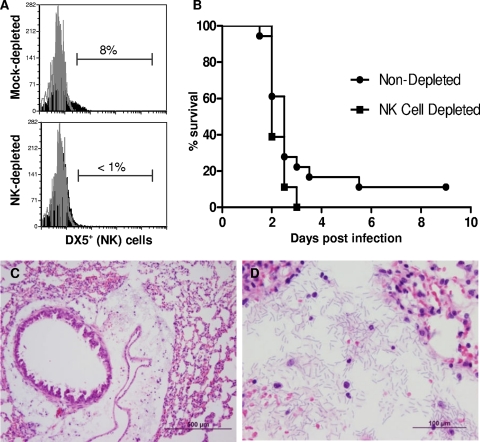
Depletion of NK cells does not impact survival or disease pathology of Swiss Webster mice following inhalational anthrax infection.
Female Swiss Webster mice were dosed with 50 μg of anti-asialo GM1 to deplete NK cells 72 h prior to, and 48 h after, infection with 5 LD50 of B. anthracis Ames spores. In the depleted group, DX5+ cells could not be detected in the spleen of animals compared to the nondepleted group (Fig. 5A). Survival data for NK cell-depleted and nondepleted female Swiss Webster mice following intranasal challenge yielded no significant differences between the two groups (Fig. 5B). The mean time to death for the NK cell-depleted group was 2 days postchallenge, versus the nondepleted control group, with a mean time to death of 2.5 days postchallenge. This experiment was performed a total of 3 times (twice by the intranasal route and once by aerosol distillation), with similar results.
Fig 5.
In vivo depletion of NK cells does not alter survival of animals infected with B. anthracis. Female Swiss Webster mice were inoculated with 50 μg of control rabbit immunoglobulin serum or anti-asialo GM1 to deplete NK cells 72 h prior to, and 48 h after, infection with B. anthracis Ames spores. (A and B) Flow cytometric analysis for the NK marker DX5, confirming the splenic depletion of NK cells in representative animals (n = 2 per treatment group in each of 3 independent experiments) (A), and mean time to death in the NK cell-depleted and mock-depleted control animals postchallenge, representative of one of three independent experiments (B). (C and D) Peribronchiolar and perivascular edema with acute inflammation and bacilli in the lung of a mouse infected with B. anthracis (C) and higher magnification of panel C showing edema, inflammatory cells, and bacilli present in the lung of this mouse (D).
After confirming the presence of B. anthracis in the lungs and blood, we evaluated the pathological consequences of infection in the lungs. The lungs were removed from both NK cell-depleted and nondepleted mice infected with B. anthracis Ames spores at 18 and 36 h and processed for H&E staining. In general, lesions consistent with anthrax infection (edema, inflammation, and the presence of bacteria) were present in both NK cell-depleted and nondepleted mice (Fig. 5C and D). The lesions were more frequent and severe at 36 h and not significantly different between the two groups of mice. Thus, the depletion of NK cells does not alter survival or pathology in this model of inhalational anthrax.
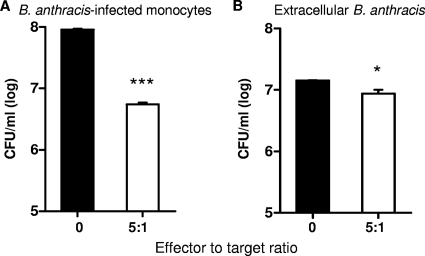
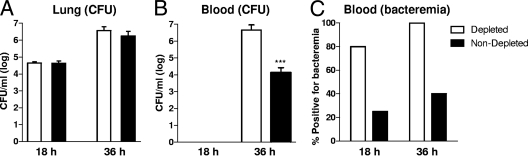
Depletion of NK cells increases bacteremia in the murine model of inhalational anthrax.
To determine the potential for NK cells to alter the bacterial burden, we first evaluated the number of B. anthracis bacteria within the lung and blood at 18 and 36 h postinfection. Following intranasal infection with 5 LD50 (5.6 × 104 CFU) of Ames spores, the lungs and blood were evaluated at 18 and 36 h postinfection for bacterial burden. As shown in Fig. 6B and C, at 18 h postinfection, the lungs of control and NK cell-depleted animals contained measurable amounts of B. anthracis organisms, while bacteria were not detected in the blood. By 36 h, the lungs and blood from both treatment groups had measurable B. anthracis bacteria. In animals lacking NK cells, the lungs contained a nonsignificant increase in average bacterial numbers (3.7 × 106 CFU/ml) compared to bacterial numbers (1.8 × 106 CFU/ml) in nondepleted animals. In contrast, a dramatic increase in B. anthracis numbers was observed for the NK cell-depleted animals compared to the control animals (Fig. 6B and C). Thus, the absence of NK cells results in a significant increase in bacteremia by 36 h.
Fig 6.
Depletion of NK cells increases bacteremia in a murine model of inhalational anthrax. Female Swiss Webster mice were inoculated with 50 μg of control rabbit immunoglobulin or anti-asialo GM1 to deplete NK cells 72 h prior to, and 48 h after, infection with B. anthracis Ames spores. Mock- and NK cell-depleted Swiss Webster mice (5 animals per group per time point) were sacrificed at 18 and 36 h following intranasal infection with B. anthracis (Ames) spores. The enumeration of CFU from disrupted tissue was performed by limiting-dilution plating onto blood agar. (A and B) Bacterial CFU in the lungs (A) and in blood (B) at 18 and 36 h postinfection. (C) Assessment for the presence of blood bacteria following 48 h of growth in selective liquid medium, shown as the percentage of bacteremic animals at 18 and 36 h postinfection. ***, P < 0.001 (P values indicate statistically significant differences in CFU between mock- and NK cell-depleted animals).
DISCUSSION
Disease progression during inhalational anthrax is extremely rapid and occurs prior to the development of an acquired immune response by the infected individual. The identification of avenues for the augmentation of the innate immune system to complement antibiotic treatments may then lead to the development of effective clinical interventions. NK cells are important effector cells in the innate immune repertoire and have antibacterial activity that could contribute to host immunity early in infection. A role for NK cells has been identified for the host defense against several bacterial pathogens, including Mycobacterium tuberculosis, Listeria monocytogenes, Escherichia coli, and Salmonella enterica serovar Typhimurium (1, 4, 14, 16, 17, 24). The clinical potential for NK cell-based immune modulation is highlighted by results from a recent study where the targeted activation of NK cells was shown to generate protective innate immunity to pneumonic Francisella tularensis infection (26). The development of this type of strategy to augment innate immune mechanisms could reduce postexposure morbidity and mortality from inhalational anthrax. In this study, we assessed the potential effector function of NK cells in the immune response to B. anthracis infection in vitro and sought to identify the significance of NK cells in vivo in a murine model of inhalational anthrax infection.
Our results provide the first demonstration that human NK cells have antibacterial activity against B. anthracis bacilli. The reduction in numbers of B. anthracis cells within infected monocytes that we observed is consistent with other reports of antibacterial NK cell activity against bacterial pathogens that target the monocyte/macrophage cell lineage (4, 29). NK cells mediate antibacterial effects on infected host cells by direct cytolytic activity or through the indirect action of secreted mediators (e.g., IFN-γ). NK cells are activated for cytotoxicity through separate and overlapping mechanisms that augment cytotoxic gene expression and activate degranulation against infected host cells (28). The ligation of natural cytotoxicity or activating receptors on NK cells by complementary ligands on the host cell triggers attack against target cells (21, 28). An interesting observation of our studies, however, is that NK cells also have significant antibacterial activity against extracellular B. anthracis. The potency of the antibacterial activity against extracellular bacteria was less than that observed against infected monocytes; however, we still observed up to a 50% reduction of bacterial CFU in cell culture medium at a 5:1 E/T ratio. The mechanisms whereby NK cells would be activated to mediate the direct damage of free bacteria are poorly understood. Natural cytotoxicity receptors (NCRs) are known to bind several viral as well as host cell proteins. An important member of the NCR family, NKp44, was shown previously to directly bind ligands on the surfaces of Mycobacterium tuberculosis and Pseudomonas aeruginosa (11). Potentially, undefined B. anthracis ligands could also be recognized by a member of the NCR family of receptors expressed by NK cells. The identification of the molecules and receptors that mediate these interactions between NK cells and B. anthracis or B. anthracis-infected monocytes/macrophages may have relevance to the design of effective immune modulation strategies.
Consistent with previous reports of anthrax toxin effects on murine cells (5, 15, 20), we observed the suppression of human T cell and NK cell expression of IFN-γ due to LT exposure. This is important, as IFN-γ activates the host macrophage for enhanced intracellular clearance. We also provide the first report, to our knowledge, that LT inhibits the activation of granulysin in human T cells. We have previously reported that granulysin, stored in the cytotoxic granules of NK cells and cytotoxic T cells, has bactericidal activity against B. anthracis (10). Granulysin can directly damage bacterial membranes and can mediate both intracellular and extracellular bactericidal effects (25). In contrast to T cells, a significant effect of LT on NK cell granulysin expression was not observed in our study, although a significant effect may be realized upon the inclusion of a larger donor pool, given the nonsignificant decrease that we observed.
With the exception of IFN-γ, our studies show that anthrax toxins appear to have minimal effects on several other measures of NK cell effector function, including proliferation, viability, direct antibacterial activity, or cytotoxicity. LT and ET have well-described immunosuppressive effects on several leukocyte populations, including T cells, B cells, NKT cells, and professional antigen-presenting cells (2, 5, 13). LT has been shown to increase apoptosis and interfere with mitogen-activated protein kinase (MAPK) signaling, resulting in decreased bactericidal activity (reactive oxygen species [ROS]) and cytokine production. In addition, LT can also cause a decrease in leukocyte proliferation and cellular activation as well as decreased B cell antibody production (5). In support of our findings, Joshi and colleagues recently reported a lack of LT effects on murine NK cells despite observing LT-mediated suppression of the NKG2D activation receptor on natural killer T (NKT) cells (20). The anthrax ET can act alone or synergistically with LT to amplify effects by also causing an increase in cyclic AMP (cAMP) levels, such as that which occurs correspondent with decreased phagocytosis by toxin-exposed macrophages (2, 6). We did not observe any effects of ET on NK cell proliferation or function despite the use of both toxins at concentrations previously shown to impair leukocyte activation (5, 15, 20). Thus, NK cells may be less susceptible to the immunosuppressive effects of anthrax toxins and could potentially be targeted to clinically augment innate immune function.
Based on our observations of potent antibacterial responses of human NK cells against B. anthracis, we further explored the potential of these responses in vivo using a mouse model. The rabbit is the most relevant model for the study of inhalational anthrax pathogenesis and for the testing of vaccines and therapeutics. Due to the availability of reagents, however, the mouse is the model most often used for studying host defense against B. anthracis. Using NK cells isolated from healthy mouse spleen, we observed that, similarly to human cells, murine NK cells also have potent bactericidal activity against extracellular and intracellular B. anthracis. The depletion of NK cells in a well-established murine model of inhalational anthrax, however, did not alter the course of infection or pathology. This was not unexpected, as the depletion of a single leukocyte subset in an immunocompetent mouse frequently does not significantly alter the survival outcome in infection models.
The primary route of infection during inhalational anthrax is the lungs. However, we did not observe differences in lung CFU or lung pathology due to NK cell depletion at 18 or 36 h postinfection. We did, however, see a dramatic and significant difference in the number of bacterial CFU in the blood of animals at 36 h postinfection. Animals lacking NK cells had a significantly higher bacterial load in the bloodstream than did animals with a fully intact immune system. NK cell numbers in the lung are likely to be very limited in early infection at the time when rapid uptake and trafficking of spores are occurring. In contrast, NK cells are most abundant in the blood and would have plentiful opportunities to interact with circulating vegetative bacteria. Taken together, these findings suggest that NK cells play a complementary, rather than obligatory, role in innate immunity to B. anthracis in the murine model.
In summary, NK cells have antibacterial activity against B. anthracis bacilli or infected monocytes that may contribute to innate host defense. Anthrax LT suppresses the human NK cell expression of IFN-γ, while many other NK effector functions are not significantly affected by either LT or ET. Depletion studies with a murine model of inhalational anthrax suggest a role for NK cells in the control of bacteremia. The augmentation of NK cell function should then be explored as a potential avenue for therapeutic intervention during B. anthracis infection.
ACKNOWLEDGMENTS
This research was supported by an NIH NIAID contract (NO1-AI-30065), the Department of Microbiology and Immunology (UTMB), the James W. McLaughlin Fellowship Fund (UTMB), and the NIH/NIAID Prematriculation Reinforcement Enrichment Program (grant 1R25GM069285).
We also thank Mark Griffin from the Department of Microbiology and Immunology at UTMB for providing assistance in the core laboratory for flow cytometry studies.
Footnotes
Published ahead of print 17 October 2011
REFERENCES
- 1. Ashkar AA, Reid S, Verdu EF, Zhang K, Coombes BK. 2009. Interleukin-15 and NK1.1+ cells provide innate protection against acute Salmonella enterica serovar Typhimurium infection in the gut and in systemic tissues. Infect. Immun. 77: 214–222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Baldari CT, Tonello F, Paccani SR, Montecucco C. 2006. Anthrax toxins: a paradigm of bacterial immune suppression. Trends Immunol. 27: 434–440 [DOI] [PubMed] [Google Scholar]
- 3. Bell DM, Kozarsky PE, Stephens DS. 2002. Clinical issues in the prophylaxis, diagnosis, and treatment of anthrax. Emerg. Infect. Dis. 8: 222–225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Brill KJ, et al. 2001. Human natural killer cells mediate killing of intracellular Mycobacterium tuberculosis H37Rv via granule-independent mechanisms. Infect. Immun. 69: 1755–1765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Comer JE, Chopra AK, Peterson JW, Konig R. 2005. Direct inhibition of T-lymphocyte activation by anthrax toxins in vivo. Infect. Immun. 73: 8275–8281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Comer JE, et al. 2006. Murine macrophage transcriptional and functional responses to Bacillus anthracis edema toxin. Microb. Pathog. 41: 96–110 [DOI] [PubMed] [Google Scholar]
- 7. Crawford MA, Aylott CV, Bourdeau RW, Bokoch GM. 2006. Bacillus anthracis toxins inhibit human neutrophil NADPH oxidase activity. J. Immunol. 176: 7557–7565 [DOI] [PubMed] [Google Scholar]
- 8. Cybulski RJ, Jr, Sanz P, O'Brien AD. 2009. Anthrax vaccination strategies. Mol. Aspects Med. 30: 490–502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Endsley JJ, Endsley MA, Estes DM. 2006. Bovine natural killer cells acquire cytotoxic/effector activity following activation with IL-12/15 and reduce Mycobacterium bovis BCG in infected macrophages. J. Leukoc. Biol. 79: 71–79 [DOI] [PubMed] [Google Scholar]
- 10. Endsley JJ, et al. 2009. Comparative antimicrobial activity of granulysin against bacterial biothreat agents. Open Microbiol. J. 3: 92–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Esin S, et al. 2008. Direct binding of human NK cell natural cytotoxicity receptor NKp44 to the surfaces of mycobacteria and other bacteria. Infect. Immun. 76: 1719–1727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ferlazzo G, et al. 2004. The abundant NK cells in human secondary lymphoid tissues require activation to express killer cell Ig-like receptors and become cytolytic. J. Immunol. 172: 1455–1462 [DOI] [PubMed] [Google Scholar]
- 13. Fukao T. 2004. Immune system paralysis by anthrax lethal toxin: the roles of innate and adaptive immunity. Lancet Infect. Dis. 4: 166–170 [DOI] [PubMed] [Google Scholar]
- 14. Garcia-Penarrubia P, Koster FT, Kelley RO, McDowell TD, Bankhurst AD. 1989. Antibacterial activity of human natural killer cells. J. Exp. Med. 169: 99–113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Glomski IJ, et al. 2007. Murine splenocytes produce inflammatory cytokines in a MyD88-dependent response to Bacillus anthracis spores. Cell. Microbiol. 9: 502–513 [DOI] [PubMed] [Google Scholar]
- 16. Godshall CJ, Scott MJ, Burch PT, Peyton JC, Cheadle WG. 2003. Natural killer cells participate in bacterial clearance during septic peritonitis through interactions with macrophages. Shock 19: 144–149 [DOI] [PubMed] [Google Scholar]
- 17. Harshan KV, Gangadharam PR. 1991. In vivo depletion of natural killer cell activity leads to enhanced multiplication of Mycobacterium avium complex in mice. Infect. Immun. 59: 2818–2821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hogg AE, Bowick GC, Herzog NK, Cloyd MW, Endsley JJ. 2009. Induction of granulysin in CD8+ T cells by IL-21 and IL-15 is suppressed by human immunodeficiency virus-1. J. Leukoc. Biol. 86: 1191–1203 [DOI] [PubMed] [Google Scholar]
- 19. Hu H, Emerson J, Aronson AI. 2007. Factors involved in the germination and inactivation of Bacillus anthracis spores in murine primary macrophages. FEMS Microbiol. Lett. 272: 245–250 [DOI] [PubMed] [Google Scholar]
- 20. Joshi SK, et al. 2009. Bacillus anthracis lethal toxin disrupts TCR signaling in CD1d-restricted NKT cells leading to functional anergy. PLoS Pathog. 5: e1000588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Moretta A, Marcenaro E, Parolini S, Ferlazzo G, Moretta L. 2008. NK cells at the interface between innate and adaptive immunity. Cell Death Differ. 15: 226–233 [DOI] [PubMed] [Google Scholar]
- 22. Peterson JW, et al. 2007. Human monoclonal antibody AVP-21D9 to protective antigen reduces dissemination of the Bacillus anthracis Ames strain from the lungs in a rabbit model. Infect. Immun. 75: 3414–3424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Peterson JW, et al. 2006. Human monoclonal anti-protective antigen antibody completely protects rabbits and is synergistic with ciprofloxacin in protecting mice and guinea pigs against inhalation anthrax. Infect. Immun. 74: 1016–1024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Shegarfi H, et al. 2009. The role of natural killer cells in resistance to the intracellular bacterium Listeria monocytogenes in rats. Scand. J. Immunol. 70: 238–244 [DOI] [PubMed] [Google Scholar]
- 25. Stenger S, et al. 1998. An antimicrobial activity of cytolytic T cells mediated by granulysin. Science 282: 121–125 [DOI] [PubMed] [Google Scholar]
- 26. Troyer RM, Propst KL, Fairman J, Bosio CM, Dow SW. 2009. Mucosal immunotherapy for protection from pneumonic infection with Francisella tularensis. Vaccine 27: 4424–4433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Vahlne G, Becker S, Brodin P, Johansson MH. 2008. IFN-gamma production and degranulation are differentially regulated in response to stimulation in murine natural killer cells. Scand. J. Immunol. 67: 1–11 [DOI] [PubMed] [Google Scholar]
- 28. Vivier E, Nunes JA, Vely F. 2004. Natural killer cell signaling pathways. Science 306: 1517–1519 [DOI] [PubMed] [Google Scholar]
- 29. Yoneda T, Ellner JJ. 1998. CD4(+) T cell and natural killer cell-dependent killing of Mycobacterium tuberculosis by human monocytes. Am. J. Respir. Crit. Care Med. 158: 395–403 [DOI] [PubMed] [Google Scholar]