Abstract
Oseltamivir-resistant H1N1 influenza viruses emerged in 2007 to 2008 and have subsequently circulated widely. However, prior to 2007 to 2008, viruses possessing the neuraminidase (NA) H274Y mutation, which confers oseltamivir resistance, generally had low growth capability. NA mutations that compensate for the deleterious effect of the NA H274Y mutation have since been identified. Given the importance of the functional balance between hemagglutinin (HA) and NA, we focused on amino acid changes in HA. Reverse genetic analysis showed that a mutation at residue 82, 141, or 189 of the HA protein promotes virus replication in the presence of the NA H274Y mutation. Our findings thus identify HA mutations that contributed to the replacement of the oseltamivir-sensitive viruses of 2007 to 2008.
INTRODUCTION
Influenza viruses cause annual epidemics and occasional pandemics in humans, resulting in high mortality primarily in the elderly and other high-risk populations (14, 33). Oseltamivir, a neuraminidase (NA) inhibitor that binds to the active site of the viral NA molecule, is frequently used to treat influenza. It was approved for clinical use in 1999, and prior to 2007 to 2008, the prevalence of oseltamivir-resistant viruses was <1% (22, 24, 34). However, in January 2008, a marked increase in oseltamivir-resistant isolates was reported by Norwegian authorities (13), and these strains soon became prevalent worldwide, accounting for approximately 15% of influenza activity globally between the last quarter of 2007 and the beginning of 2008 (34). During the 2008-2009 season, approximately 95% of H1N1 viruses analyzed from 30 countries were found to be oseltamivir resistant (34, 35). However, most of the circulating oseltamivir-resistant viruses were not associated with oseltamivir use (9, 19, 22), indicating that these resistant viruses dominated the oseltamivir-sensitive viruses without drug pressure.
Studies with laboratory and older seasonal H1N1 strains, such as A/WSN/33 (WSN), A/Texas/36/1991, and A/New Caledonia/20/1999 (NC/99), showed that the histidine (H)-to-tyrosine (Y) mutation at residue 274 (N2 numbering) of N1 NA (NA H274Y mutation) confers resistance to oseltamivir but attenuates virus growth in vivo and in vitro (1, 4, 6, 14, 17). Yet the growth kinetics of the oseltamivir-resistant viruses that circulated in 2007 and 2008 were similar to those of sensitive viruses (27). This finding was thought to be due to amino acid substitutions in NA (i.e., R222Q and V234M) that were introduced in 2004 and became prevalent in 2007 to 2008 (4). Indeed, a study using recombinant viruses that comprised the NC/99 NA gene and the A/Texas/36/1991 versions of the other genes showed that these secondary mutations in NA (R222Q and V234M) compensated for the defect in NA enzymatic activity, and thus in growth capability, caused by the H274Y mutation (4).
A functional balance between the surface glycoproteins of the influenza virus, hemagglutinin (HA) and NA, is important for efficient viral replication (18, 21, 23, 26, 31). HA attaches to sialyloligosaccharide receptors to mediate virus entry into the host cell, an event that is followed by a series of replication steps that result in the generation of viral progeny (10, 28). At the end of the virus replication cycle, NA removes sialic acid from the viral progeny to prevent their self-aggregation and also from the cell surface to facilitate virion release (8, 11, 20). Mutations that affect HA receptor binding can compensate for defects in NA function (2, 20). In this study, to elucidate the mechanism responsible for the prevalence of oseltamivir-resistant H1N1 viruses during the 2007-2008 season, we focused on HA changes in seasonal H1N1 influenza viruses from 2004 to 2009 (excluding pandemic A/H1N1 2009 viruses) and evaluated the contribution of HA mutations to the growth efficiency of oseltamivir-resistant H1N1 viruses carrying the NA H274Y mutation.
MATERIALS AND METHODS
Sequence analysis.
HA and NA sequences of H1N1 seasonal influenza viruses from 2004 to 2008 were retrieved from the Influenza Virus Resource database of the National Center for Biotechnology Information (3) (using the following query: type, influenza A virus; host, human; country, any; segment, HA/NA; subtype, H1N1; full length only; and collection date, from 2004 to March 2009). We used BioEdit software (12) to align sequences and identified seven HA1 amino acid changes that were maintained in oseltamivir-resistant viruses that circulated between 2007 and 2009 (Table 1). HA and NA were numbered according to the H1 and N2 numbering schemes, respectively. HA and NA phylogenetic analyses were performed by the neighbor-joining method with the coding regions of HA and NA nucleotide sequences containing only unambiguous sequences by using MEGA4 (30), and phylogenetic trees were drawn with TreeGraph 2.0.43-193 beta (29).
Table 1.
HA amino acid substitutions that occurred between 2004 and 2007 and were maintained in the oseltamivir-resistant viruses that caused epidemics in the 2007-2009 seasons
| Amino acid position | HA amino acid |
|
|---|---|---|
| 2004 to 2006 | 2007 to March 2009 | |
| 35 | D | N |
| 82 | T | K |
| 94 | Y | H |
| 141 | K | E |
| 189 | R | K |
| 209 | R | K |
| 274 | E | K |
Virus.
A human-derived oseltamivir-resistant influenza A/H1N1 virus isolated during the epidemic of the 2007-2008 season, namely, A/Tottori/52/2008 (To/08), was passaged twice in Madin-Darby canine kidney (MDCK) cells maintained in minimal essential medium (MEM) supplemented with 4% bovine serum albumin and 0.03% tosylsulfonyl phenylalanyl chloromethyl ketone (TPCK)-treated trypsin. The virus was grown at 35°C with 5% CO2 for 48 h. The cell culture supernatant was collected and stored at −80°C until use.
Cloning of viral genes.
Viral RNA of the To/08 strain was extracted with a QIAamp viral RNA minikit (Qiagen, Germantown, MD). Reverse transcriptase PCR (RT-PCR) was performed by using a one-step RT-PCR system (SuperScript III One-Step RT-PCR system with Platinum Taq High Fidelity polymerase; Invitrogen, Carlsbad, CA) and primer pairs containing a BsmBI restriction site (15, 16). The amplified products for full-length HA (GenBank accession number CY075490) and NA (GenBank accession number CY075491) were inserted into the pCR2.1-TOPO cloning vector (Invitrogen). Three clones were sequenced to obtain the consensus sequences of the HA and NA genes.
Mutagenesis of viral HA and NA segments and subcloning into the pHH21 plasmid.
pCR2.1 plasmids encoding To/08 HAs possessing the D35N, T82K, Y94H, K141E, R189K, R209K, or E274K mutation were generated by using a QuikChange site-directed mutagenesis kit (Stratagene, Cedar Creek, TX). To make an oseltamivir-sensitive To/08 NA, a TAT-to-CAC nucleotide mutation that creates a tyrosine-to-histidine substitution was introduced at amino acid position 274 of the To/08 NA encoded in pCR2.1. After the mutations were confirmed by sequencing, the pCR2.1 plasmids were digested with BsmBI at 55°C, and DNA fragments were subcloned into a pHH21 vector containing the human RNA polymerase I promoter and the mouse RNA polymerase I terminator (25) to produce pPolI-To/08-HA-wild, pPolI-To/08-HA-D35N, pPolI-To/08-HA-T82K, pPolI-To/08-HA-Y94H, pPolI-To/08-HA-K141E, pPolI-To/08-HA-R189K, pPolI-To/08-HA-R209K, pPolI-To/08-HA-E274K, pPolI-To/08-HA-186-193, pPolI-To/08-NA-274Y, and pPolI-To/08-NA-274H.
Recombinant virus generation.
Recombinant viruses were generated by using reverse genetics as previously described (25). Each pPolI-To/08-HA plasmid with pPolI-To/08-NA-274Y or -274H, together with six pHH21 plasmids bearing the non-HA and -NA genes of WSN (H1N1) (pPolI-WSN-PB2, pPolI-WSN-PB1, pPolI-WSN-PA, pPolI-WSN-NP, pPolI-WSN-MP, and pPolI-WSN-NS) and four WSN protein expression plasmids (pCAGGS-PB2, pCAGGS-PB1, pCAGGS-PA, and pCAGGS-NP), were transfected into 293T cells with Trans-IT LT-1 (PanVera, Madison, WI). The supernatant was harvested 48 h after transfection and then inoculated onto MDCK cells and incubated for 48 h in the presence of TPCK-treated trypsin (Worthington, Lakewood, NJ) (final concentration, 3.0 μg/ml). The viruses generated were stored at −80°C until use.
Growth kinetics of recombinant viruses.
Virus growth was evaluated by infecting MDCK cells with each virus at a multiplicity of infection of 10−3. Culture supernatants were collected 24, 48, and 72 h after infection. Triplicate wells were tested for each virus, and virus titers were evaluated by use of plaque assays. Tenfold dilutions of samples from each time point were prepared and inoculated onto MDCK cells. After incubation for 1 h at 35°C, cells were washed and overlaid with agarose-containing maintenance medium in the presence of TPCK-treated trypsin (final concentration, 3 μg/ml). Plates were incubated at 35°C in 5% CO2 for 3 days, and PFU per ml were determined.
RESULTS AND DISCUSSION
Evolution of seasonal H1N1 virus HA and NA genes from 2004 to 2008.
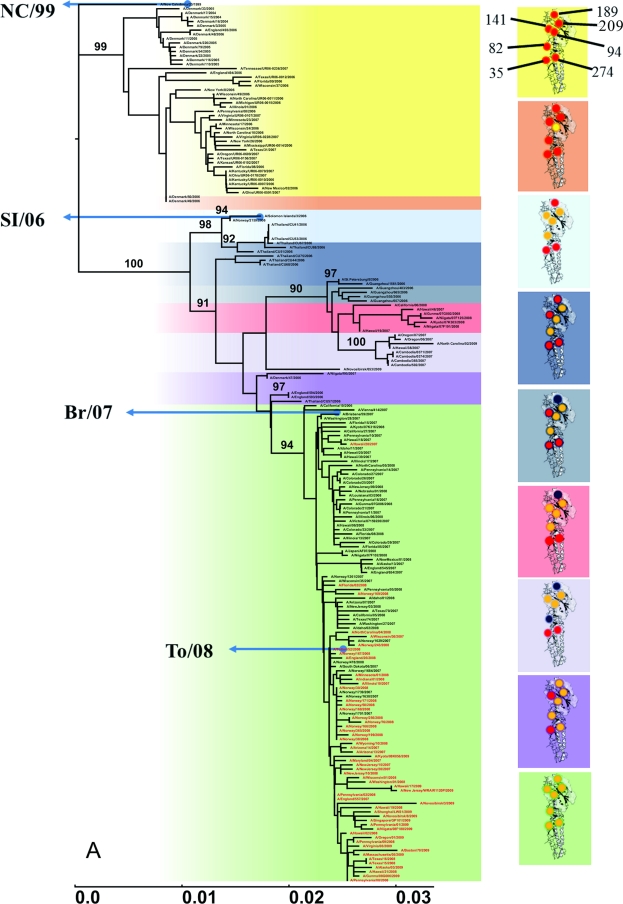
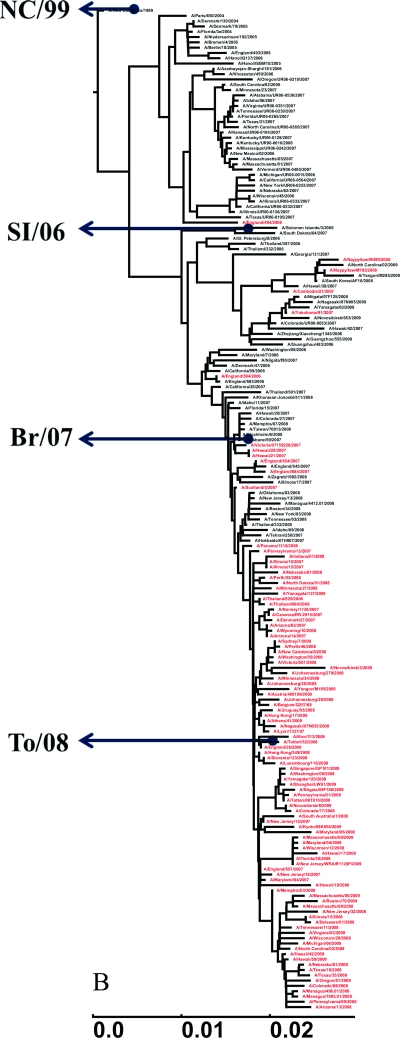
To determine whether the epidemic of oseltamivir-resistant viruses with the NA 274Y mutation was associated with specific mutations in HA, we analyzed the HA (bases 1 to 1689) and NA (bases 1 to 1410) nucleotide sequences of representative seasonal H1N1 strains isolated between 2004 and March 2009, including three vaccine strains that were recommended between 2004 and 2008: A/New Caledonia/20/1999 (NC/99), A/Solomon Island/3/2006 (SI/06), and A/Brisbane/52/2007 (Br/07) (36). Oseltamivir-resistant isolates carrying NA 274Y were found sporadically in 2007 and became more prevalent in 2008, when Br/07 was used as a vaccine strain (Fig. 1A and B). Phylogenetic analysis revealed that HA and NA showed similar clustering patterns, indicating coevolution of these two proteins. However, from this analysis, we did not find any amino acid changes, in either HA or NA, that were associated with the emergence of viruses possessing the NA 274Y mutation.
Fig 1.
Phylogenetic analyses of HA and NA of seasonal H1N1 viruses by using the neighbor-joining method with 1,000 bootstrap replications. Oseltamivir-resistant isolates carrying NA 274Y are shown in red. (A) HA phylogenetic tree of selected seasonal H1N1 isolates from 2004 to 2009 (excluding 2009 pandemic H1N1 viruses). Branches are colored to reflect amino acid changes. Only bootstrap values of >90% are shown for each corresponding group. The scale bar indicates the number of nucleotide substitutions per site. The following vaccine strains are included in the tree as a reference: 2004-2007 season (NC/99), 2007-2008 season (SI/06), and 2008-2010 season (Br/07) vaccines. The To/08 virus used in this study is included in the oseltamivir-resistant 2007-2008 isolates (green box). The seven amino acid substitutions that occurred in the HA head and were maintained in subsequent viruses during HA evolution between 2004 and 2008 include D35N, T82K, Y94H, K141E, R189K, R209K, and E274K. HA amino acids of 2004-2005 isolates are represented by red spheres and changed to other amino acids (shown in yellow) in subsequent viruses. Occasional amino acid substitutions that are not listed in Table 1 appeared temporarily at two of these positions (blue spheres). (B) NA phylogenetic tree of prepandemic seasonal H1N1 strains from 2004 to 2009. To/08 NA is included in the oseltamivir-resistant 2007-2008 isolates.
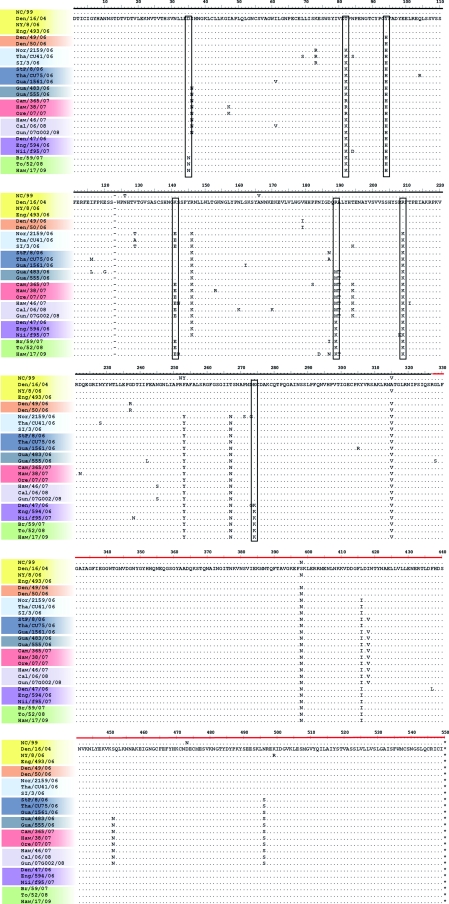
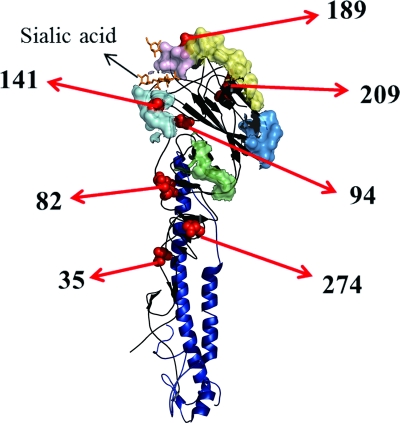
Next, we focused on HA changes that occurred prior to the emergence of the oseltamivir-resistant viruses. Sequence alignment showed that the HA molecules of seasonal H1N1 influenza viruses underwent several amino acid substitutions in the HA1 domain from 2004 to 2008: aspartic acid to asparagine at residue 35 (D35N), threonine to lysine at residue 82 (T82K), tyrosine to histidine at residue 94 (Y94H), lysine to glutamic acid at residue 141 (K141E), arginine to lysine at residue 189 (R189K), arginine to lysine at residue 209 (R209K), and glutamic acid to lysine at residue 274 (E274K) (Table 1; Fig. 2). These residues were mapped on the HA molecule (Fig. 3). Among them, residues 141 and 189 were located at the Ca2 and Sb antigenic sites (5), respectively. Although none of these substitutions occurred among the conserved residues in the HA receptor binding site (10), residues 94, 141, 189, and 209 are located near this site.
Fig 2.
HA amino acid alignment for seasonal H1N1 viruses isolated between 2004 and 2009 (excluding pandemic A/H1N1/2009). A gap was inserted to correspond to H1 numbering. Colors indicate the strains that belong to the groups with the corresponding colors in the HA phylogenetic tree (Fig. 1A). Black frames indicate the amino acid substitutions from 2004 to March 2009 that were studied; NC/99 is included for reference (residues 146, 253, and 267 were excluded because the former two were the same in the other strains as in NC/99 and the last residue has been conserved since 2006). Black and red horizontal lines indicate the HA1 and HA2 domains, respectively.
Fig 3.
Structure of HA monomer showing antigenic sites and amino acid residues at which substitutions occurred between 2004 and 2008. The drawing shows the HA monomer of the 1918 H1N1 virus, modified from the Protein Data Bank structure 2WRG (5) by using PyMOL (The PyMOL Molecular Graphics System, version 1.3; Schrödinger, LLC [www.pymol.org]). The head and stem are indicated by black and dark blue ribbons, respectively. Antigenic sites are indicated as colored surfaces, as follows: Sa, light yellow; Sb, light purple; Ca1, blue; Ca2, cyan; and Cb, light green. Residues at which amino acid changes occurred are shown as red spheres (residues 35, 82, 94, 141, 189, 209, and 274). Sialic acid is shown with orange sticks.
Effect of HA amino acid substitutions on oseltamivir-resistant virus growth.
To determine if any of the above-described HA mutations are required for growth by viruses with the NA H274Y mutation, we examined the HA and NA proteins of A/Tottori/52/2008 (To/08), one of the early oseltamivir-resistant strains that later became dominant. We generated plasmids encoding mutant To/08 HAs that each possessed one of the amino acids found in oseltamivir-sensitive viruses isolated between 2004 and 2006, as listed in Table 1 (35D, 82T, 94Y, 141K, 189R, 209R, and 274E). We then generated recombinant viruses possessing the mutant To/08 HA and To/08 NA segments together with the remaining six segments from WSN. All viral growth was tested in MDCK cells, although these cells may not reflect viral fitness in vivo. For comparison, we also made HA mutant viruses possessing a mutant To/08 NA with the residue 274H, which makes NA oseltamivir sensitive. In addition, we made a virus possessing the wild-type To/08 HA and wild-type oseltamivir-resistant To/08 NA genes along with the remaining genes from WSN as a control. We then compared the growth efficiencies of a virus carrying wild-type To/08 HA and oseltamivir-resistant NA 274Y (Wt-res) and a virus with wild-type To/08 HA and oseltamivir-sensitive NA 274H (Wt-sen). Although the titers at 24 and 72 h postinfection (hpi) differed, the titers were similar at 48 hpi (Fig. 4A), as previously described (4). This result suggests that the HA molecule from the 2007-2008 season functions well with either oseltamivir-resistant or -sensitive NA to support efficient virus growth.
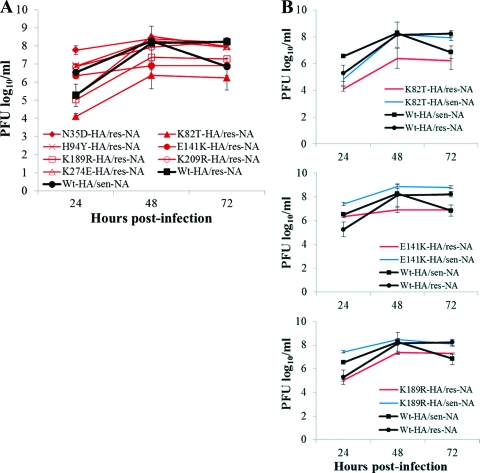
Fig 4.
Growth of recombinant viruses with an HA amino acid substitution and oseltamivir-resistant or -sensitive NA. (A) MDCK cells were incubated with recombinant viruses at a multiplicity of infection of 10−3. Growth was evaluated at 24, 48, and 72 h. Black squares indicate a virus with wild-type To/08 HA and oseltamivir-resistant NA 274Y (Wt-HA/res-NA), whereas black spheres indicate a virus with wild-type To/08 HA and oseltamivir-sensitive NA 274H (Wt-HA/sen-NA). Red lines are for viruses with a To/08 HA mutation. Viruses are designated according to the HA mutation and NA phenotype; for example, HA-N35D/res-NA indicates a virus possessing To/08 HA with the N35D mutation and NA with the 274Y mutation. (B) Growth of viruses with oseltamivir-resistant (res-NA) To/08 NA 274Y (red lines) or oseltamivir-sensitive (sen-NA) To/08 NA 274H (blue lines) and carrying the K81T, E141K, or K189R HA mutation. The virus with wild-type To/08 HA and NA 274Y (Wt-HA/res-NA) and that with wild-type To/08 HA and NA 274H (Wt-HA/sen-NA) (marked with black squares and black spheres, respectively), shown in panel A, are also included for comparison. When HA K82T, E141K, and K189R mutations were paired with oseltamivir-sensitive NA (274H), growth was restored. Data are expressed as means and standard deviations (SD) for three replicate plates.
To determine whether the HA amino acid substitutions that occurred between 2004 and 2007 compensate for the growth of viruses possessing the NA H274Y mutation, we compared the growth kinetics of seven To/08 mutants that each possessed one of the HA amino acid substitutions found in the earlier strains (i.e., N35D, K82T, H94Y, E141K, K189R, K209R, or K274E). We found that three mutants with the oseltamivir-resistant NA 274Y (res-NA), namely, K82T-HA/res-NA, E141K-HA/res-NA, and K189R-HA/res-NA, replicated at 10- to 100-fold lower rates than those of virus with wild-type HA (Wt-HA/res-NA) (Fig. 4A). Bloom et al. (4) showed that two NA mutations (R222Q and V234M) compensate for the deleterious oseltamivir resistance-conferring NA H274Y mutation, thus supporting the efficient growth of oseltamivir-resistant viruses. The oseltamivir-resistant To/08 NA used in this study possessed the R222Q and V234M amino acid substitutions, yet viruses possessing To/08 NA did not replicate well when paired with mutated HAs that corresponded to those found in the 2004-2006 isolates (i.e., HA-K82T, HA-E141K, or HA-K189R). However, the growth efficiency of the viruses that possessed HA 82T, 141K, or 189R was restored to a level similar to that of Wt-HA/res-NA and Wt-HA/sen-NA when these viruses were paired with an oseltamivir-sensitive NA (Fig. 4B, blue lines). We did not observe appreciable differences in plaque size among the viruses. These results suggest that the T82K, K141E, or R189K mutation is critical to viruses with oseltamivir-resistant NA 274Y for achieving a growth level similar to that of viruses carrying oseltamivir-sensitive NA 274H.
Although the previous report (4) suggested that the NA mutations R222Q and V234M could compensate for the defect caused by the NA H274Y mutation, we showed that in addition to these NA mutations, the HA T82K, K141E, and R189K mutations, which accumulated prior to the emergence of oseltamivir-resistant viruses in 2007, also promote efficient growth of oseltamivir-resistant viruses. Therefore, the NA substitutions previously identified by Bloom et al. (4) and the HA substitutions identified here, both of which accumulated prior to the emergence of oseltamivir-resistant viruses in 2007, are essential for the efficient growth of oseltamivir-resistant viruses possessing the NA H274Y mutation. HA residues 141 and 189 are located at the Ca2 and Sb antigenic sites, respectively, and residue 189 is also located near the HA receptor binding site, suggesting the need for further study to determine whether the changes at these residues alter HA antigenicity, binding affinity, or both (5, 7, 32, 37). Residue 82 is not on or near the HA antigenic or receptor binding site; therefore, further study is required to understand the mechanism by which mutations at residue 82 support the efficient growth of viruses possessing the oseltamivir resistance-conferring N1 275Y substitution.
Antiviral drugs are an important defense when humans face influenza epidemics and pandemics. Our studies further our understanding of the emergence of drug-resistant viruses. Current epidemic viruses continue to evolve under selective pressure; therefore, the continuous monitoring of epidemic viruses is essential to reduce the risk of emergence of epidemics caused by drug-resistant viruses.
ACKNOWLEDGMENTS
We thank Ryo Suzuki for excellent technical assistance and Susan Watson for editing the manuscript.
This work was supported in part by Takeda Science Foundation, Precursory Research for Embryonic Science and Technology (PRESTO), Grants-in-Aid for Specially Promoted Research and for Scientific Research, by a contract research fund of the Program of Founding Research Centers for Emerging and Reemerging Infectious Diseases, ERATO (Japan Science and Technology Agency), by Special Coordination Funds for Promoting Science and Technology from the Ministry of Education, Culture, Sports, Science, and Technology of Japan, and by U.S. National Institute of Allergy and Infectious Diseases and Public Health Service research grants.
Footnotes
Published ahead of print 19 October 2011
REFERENCES
- 1. Abed Y, Gayette N, Boivin G. 2004. A reverse genetic study of resistance to neuraminidase inhibitors in an influenza A/H1N1 virus. Antivir. Ther. 9:577–581 [PubMed] [Google Scholar]
- 2. Banks J, et al. 2000. Changes in the haemagglutinin and the neuraminidase genes prior to the emergence of highly pathogenic H7N1 avian influenza viruses in Italy. Arch. Virol. 146:963–973 [DOI] [PubMed] [Google Scholar]
- 3. Bao Y, et al. 2008. The influenza virus resource at the National Center for Biotechnology Information. J. Virol. 82:596–601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bloom JD, Gong LI, Baltimore D. 2010. Permissive secondary mutations enable the evolution of influenza oseltamivir resistance. Science 328:1272–1275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brownlee GG, Fodor E. 2001. The predicted antigenicity of the haemagglutinin of the 1918 Spanish influenza pandemic suggests an avian origin. Philos. Trans. R. Soc. Lond. B Biol. Sci. 356:1871–1876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Carr J, et al. 2001. Influenza virus carrying neuraminidase with reduced sensitivity to oseltamivir carboxylate has altered properties in vitro and is compromised for infectivity and replicative ability in vivo. Antiviral Res. 54:79–88 [DOI] [PubMed] [Google Scholar]
- 7. Caton AJ, Brownlee GG, Yewdell JW, Gerhard W. 1982. The antigenic structure of the influenza virus A/PR/8/34 hemagglutinin (H1 subtype). Cell 31:417–427 [DOI] [PubMed] [Google Scholar]
- 8. Colman PM, Hoyne PA, Lawrence MC. 1993. Sequence and structure alignment of paramyxovirus hemagglutinin-neuraminidase with influenza virus neuraminidase. J. Virol. 67:2972–2980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dharan NJ, et al. 2009. Infections with oseltamivir-resistant influenza A (H1N1) virus in the United States. JAMA 30:1034–1041 [DOI] [PubMed] [Google Scholar]
- 10. Gamblin SJ, et al. 2004. The structure and receptor binding properties of the 1918 influenza hemagglutinin. Science 303:1838–1842 [DOI] [PubMed] [Google Scholar]
- 11. Gottschalk A. 1957. Neuraminidase: the specific enzyme of influenza virus and Vibrio cholerae. Biochim. Biophys. Acta 23:645–646 [DOI] [PubMed] [Google Scholar]
- 12. Hall TA. 1999. BioEdit: a user-friendly biological sequence alignment editor and analysis program for Windows 95/98/NT. Nucleic Acids Symp. Ser. 41:95–98 [Google Scholar]
- 13. Hauge SH, Dudman S, Borgen K, Lackenby A, Hungnes O. 2009. Oseltamivir-resistant influenza viruses A (H1N1), Norway, 2007-08. Emerg. Infect. Dis. 15:155–162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hayden FG. 1997. Prevention and treatment of influenza in immunocompromised patients. Am. J. Med. 102:55–60 [DOI] [PubMed] [Google Scholar]
- 15. Hoffman E. 1997. Ph.D. thesis Justus-Liebig-University, Giessen, Germany [Google Scholar]
- 16. Hoffmann E, Stech J, Guan Y, Webster RG, Perez DR. 2001. Universal primer set for the full-length amplification of all influenza A viruses. Arch. Virol. 146:2275–2289 [DOI] [PubMed] [Google Scholar]
- 17. Ives JAL, et al. 2002. The H274Y mutation in the influenza A/H1N1 neuraminidase active site following oseltamivir phosphate treatment leave virus severely compromised both in vitro and in vivo. Antiviral Res. 55:307–317 [DOI] [PubMed] [Google Scholar]
- 18. Kobasa D, et al. 1999. Amino acid residues contributing to substrate specificity of influenza A virus neuraminidase. J. Virol. 73:6743–6751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kramarz P. 2009. Use of oseltamivir in 12 European countries between 2002-2007—lack of association with the appearance of oseltamivir-resistant influenza A (H1N1) viruses. Euro Surveill. 14:19112 http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=19112 [DOI] [PubMed] [Google Scholar]
- 20. Liu C, Eichelberger MC, Compans RW, Air GM. 1995. Influenza type A virus neuraminidase does not play a role in viral entry, replication, assembly, or budding. J. Virol. 69:1099–1106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Matrosovich M, Zhou N, Kawaoka Y, Webster R. 1999. The surface glycoproteins of H5 influenza viruses isolated from humans, chickens, and wild aquatic birds have distinguishable properties. J. Virol. 73:1146–1155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Meijer A, et al. 2009. Oseltamivir-resistant influenza A (H1N1) virus, Europe, 2007-08 season. Emerg. Infect. Dis. 15:552–560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mitnaul LJ, et al. 2000. Balanced hemagglutinin and neuraminidase activities are critical for efficient replication of influenza A virus. J. Virol. 74:6015–6020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Monto AS, et al. 2006. Detection of influenza viruses resistant to neuraminidase inhibitors in global surveillance during the first 3 years of their use. Antimicrob. Agents Chemother. 50:2395–2402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Neumann G, et al. 1999. Generation of influenza A viruses entirely from cloned cDNAs. Proc. Natl. Acad. Sci. U. S. A. 96:9345–9350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ohuchi M, Ohuchi R, Feldmann A, Klenk HD. 1997. Regulation of receptor binding affinity of influenza virus hemagglutinin by its carbohydrate moiety. J. Virol. 71:8377–8384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rameix-Welti M, Enouf V, Cuvelier F, Jeannin P, van der Werf S. 2008. Enzymatic properties of the neuraminidase of seasonal influenza H1N1 viruses provide insights for the emergence of natural resistance to oseltamivir. PLoS Pathog. 4:e1000103 doi:10.1371/journal.ppat.1000103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Skehel JJ, Wiley DC. 2000. Receptor binding and membrane fusion in virus entry: the influenza hemagglutinin. Annu. Rev. Biochem. 69:531–569 [DOI] [PubMed] [Google Scholar]
- 29. Stöver BC, Müller K. 2010. Treegraph 2: combining and visualizing evidence from different phylogenetic analyses. BMC Bioinformatics 11:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Tamura K, Dudley J, Nei M, Kumar S. 2007. MEGA4: Molecular Evolutionary Genetics Analysis (MEGA) software version 4.0. Mol. Biol. Evol. 24:1596–1599 [DOI] [PubMed] [Google Scholar]
- 31. Wagner R, Matrosovich M, Klenk HD. 2002. Functional balance between haemagglutinin and neuraminidase in influenza virus infections. Rev. Med. Virol. 12:159–166 [DOI] [PubMed] [Google Scholar]
- 32. Wang W, et al. 2010. Glycosylation at 158N of the hemagglutinin protein and receptor binding specificity synergistically affect the antigenicity and immunogenicity of a live attenuated H5N1 A/Vietnam/1203/2004 vaccine virus in ferrets. J. Virol. 84:6570–6577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Whitley RJ, Monto AS. 2006. Prevention and treatment of influenza in high-risk groups: children, pregnant women, immunocompromised hosts, and nursing home residents. J. Infect. Dis. 194:S133–S138 [DOI] [PubMed] [Google Scholar]
- 34. WHO 2008. Influenza A(H1N1) virus resistance to oseltamivir. Last quarter 2007 to first quarter 2008. WHO, Geneva, Switzerland: http://www.who.int/csr/disease/influenza/oseltamivir_summary/en/index.html Accessed 8 August 2011 [Google Scholar]
- 35. WHO 21 March 2009. Influenza A(H1N1) virus resistance to oseltamivir. WHO, Geneva, Switzerland: http://www.who.int/csr/disease/influenza/h1n1_table/en/ Accessed 8 August 2011 [Google Scholar]
- 36. WHO 2010. Recommended viruses for influenza vaccines for use in the 2010–2011 northern hemisphere influenza season. WHO, Geneva, Switzerland: http://www.who.int/influenza/vaccines/virus/recommendations/201002_Recommendation.pdf Accessed 8 August 2011 [Google Scholar]
- 37. Yang Z, et al. 2007. Immunization by avian H5 influenza hemagglutinin mutants with altered receptor binding specificity. Science 317:825–828 [DOI] [PMC free article] [PubMed] [Google Scholar]