Abstract
Objective
To determine risk factors for cardiac complications following total joint replacement (TJR) surgery.
Methods
We performed a case–control study of patients who had undergone a primary or revision total knee or total hip replacement surgery. Cases consisted of those who received a TJR and experienced a cardiac complication during the surgical admission period (myocardial infarction [MI], congestive heart failure [CHF], unstable angina, arrhythmia, symptomatic hypotension, or pulmonary embolus). Controls consisted of those who received a TJR and did not experience a cardiac complication during the surgical admission period. Controls were matched to the cases for age at surgery, year of surgery, and surgeon. Case and control status and identification of potential risk factors were ascertained by review of medical records. Conditional logistic regression analysis was used to identify independent predictors of cardiac complications.
Results
The sample included 209 cases and 209 controls. Factors associated with a higher risk of cardiac complications included a history of arrhythmia (adjusted odds ratio [OR] 2.6 [95% confidence interval (95% CI) 1.5–4.3]), a history of coronary artery disease, MI, CHF, or valvular heart disease (OR 1.6 [95% CI 0.9–2.6]), revision surgery (OR 2.2 [95% CI 1.2–3.9]), and bilateral surgery (adjusted OR 3.5 [95% CI 1.6–8.0]). Even though controls were matched for age (within age brackets), age was still associated with a higher risk of cardiac complications (OR 1.7 [95% CI 0.9–3.4]).
Conclusion
This case–control study identified 2 new risk factors for cardiac complications following TJR: bilateral and revision surgery. The study also confirmed previously documented risk factors, including older age at surgery and a history of arrhythmia and of other cardiac problems. These findings should help clinicians anticipate and prevent cardiac complications following TJR surgery.
Morbidity and mortality due to cardiovascular disease are prevalent and costly for patients undergoing noncardiac surgery. The current American College of Cardiology and American Heart Association guidelines recommend the use of clinical predictors, surgical predictors, and assessments of functional capacity to evaluate patients undergoing noncardiac surgery (1).
A multifactorial index examining potential clinical predictors of cardiac risk was originally proposed in 1977 and has since undergone further refinement (2–7). Surgical predictors of outcome include the intrinsic risk of the surgical procedure, with vascular surgery categorized as high risk, most orthopedic surgery as intermediate risk, and endoscopic procedures as low risk (1). Previous studies did not distinguish higher risk from lower risk orthopedic procedures. In the particular case of total joint arthroplasty, there is little information on the risks of primary versus revision or bilateral procedures. Functional capacity in patients undergoing joint replacement surgery is predictably poor (usually, <4 METS, or metabolic equivalents, a standardized measure of energy expenditure), making it a suboptimal predictor of cardiac complications. Thus, while the literature on cardiac complications associated with noncardiac procedures is rich, specific literature on cardiac complications following total joint replacement (TJR) surgery is sparse.
The acute mortality rate among inpatients after elective joint replacement surgery ranges from 0.3% to 0.95% (8), with a 1-year mortality rate of ~2% (9). Acute mortality rates following surgery for hip fracture are significantly higher (10). A population-based study of patients undergoing elective, primary total knee replacement surgery documented a 0.8% risk of myocardial infarction (MI) within 90 days of surgery (11). TJR surgery is now being offered to older patients, and an increasing proportion of the procedures are complex, such as revision surgery and bilateral joint replacement surgery. Older patients undergoing noncardiac surgery have been noted to be at increased risk of developing postoperative arrhythmias (12–15).
While orthopedic procedures are not intrinsically high-risk, joint replacement surgery is performed frequently. In 2004, more than 700,000 total hip and total knee replacement surgeries were performed in US hospitals, with more than 60% performed in patients who were ages 65 years and older (16). Thus, even if the risk of cardiovascular complications is low in this group, the total number of patients who are at risk is very high, and efforts to reduce cardiovascular risk are warranted. The purpose of this study was to evaluate factors that contribute to cardiovascular risk in a select population of patients undergoing TJR surgery. Our hypothesis was that traditional risk factors (such as a history of cardiac-related conditions) put patients at risk of cardiac events, as do more complex, lengthy procedures, such as bilateral and revision TJR surgeries.
PATIENTS AND METHODS
Study design
We performed a nested case–control study of risk factors for cardiovascular complications following total hip or total knee replacement surgeries.
Selection of patients
Patient population
Patients were eligible to be either cases or controls if they had undergone elective total hip or total knee replacement surgery, whether primary or revision, between November 1, 2001 and March 31, 2004 at the New England Baptist Hospital in Boston. A total of 5,376 patients underwent elective primary or revision total hip or knee replacement during this period.
Identification of potential cases and controls
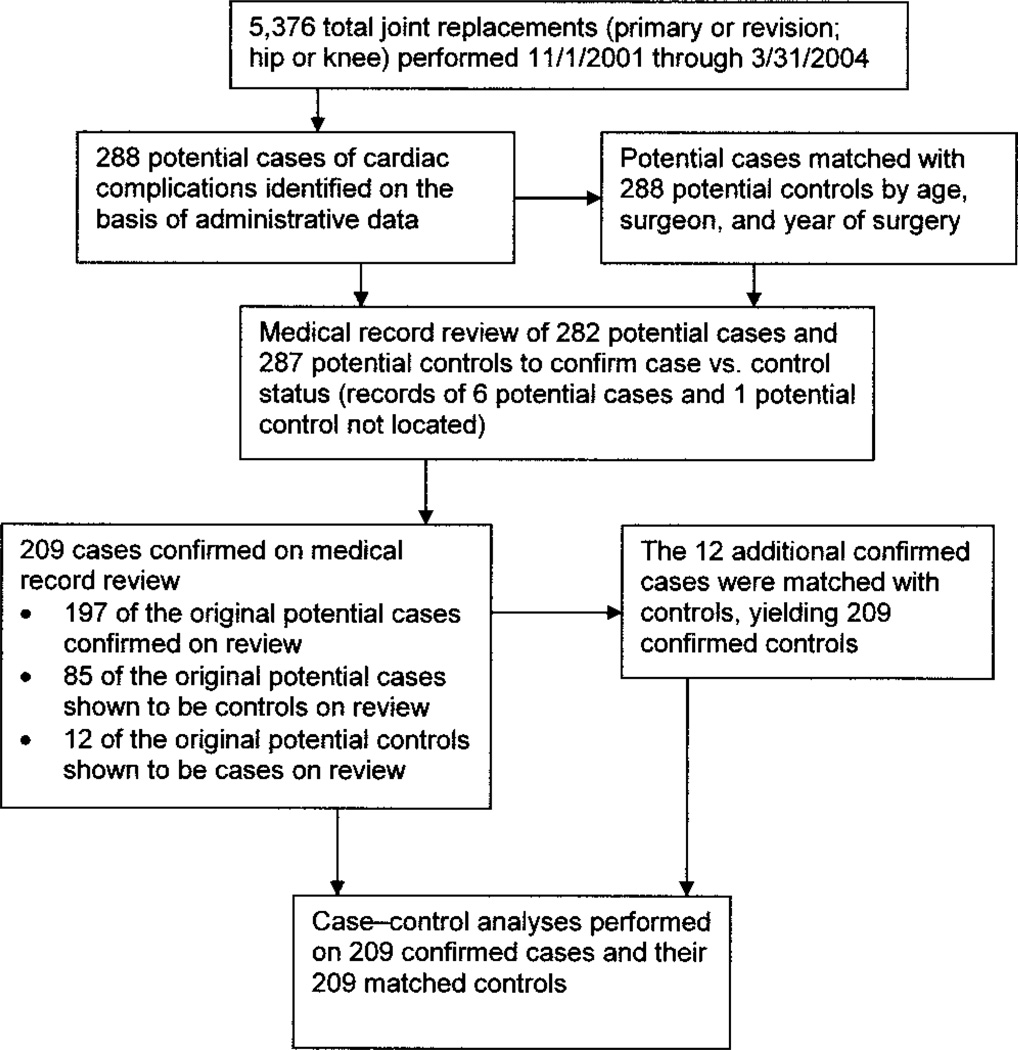
We used a 2-stage strategy to identify cases and controls. The process is depicted in Figure 1. First, we used administrative data to identify potential cases, which were patients who appeared to be at high risk of having experienced cardiac complications. Potential cases had administrative codes indicating that they had been referred to the telemetry unit or the intensive care unit, and had International Classification of Diseases, Ninth Revision (ICD-9) diagnosis codes indicating arrhythmia, MI, unstable angina, congestive heart failure (CHF), or pulmonary embolus. In addition, these patients had a procedure code indicating that the surgery was for a primary or revision total knee or total hip replacement (codes 81.51, 81.53, 81.54, 81.55).
Figure 1.
Flowchart showing the identification of 209 cases of cardiac complications following total joint replacement (TJR) surgery, as well as 209 controls without cardiac complications following TJR surgery who were matched with the cases for age at surgery, surgeon, and year of surgery. TJRs (primary or revision surgery; hip or knee replacement) were performed between November 1, 2001 and March 31, 2004.
Controls for these 288 potential cases were selected from the pool of 5,376 patients who underwent elective primary or revision total hip or knee replacement surgery during the study period. Controls were matched to the cases according to surgeon (lowest-volume surgeons were grouped together), age at the time of surgery (<50, 50–69, 70–79, ≥80 years), and year of admission. Potential cases were not eligible to be chosen as controls. Cases without a matched control were then matched according to the categories of surgeon and age at surgery only. Cases remaining without a matched control were then matched according to the category of surgeon only.
Identification of definite cases and controls with the use of medical records
We performed a detailed medical record review of the potential cases and their controls to confirm their status as cases and controls. Of the 288 potential cases, 282 had records from the inpatient admission available for chart abstraction, whereas records were available for 287 controls. The medical records of these 569 patients were abstracted by a physical therapist (JG) who had extensive experience caring for patients following TJR and who was trained specifically in the chart review technique. Outcomes and potential risk factors were defined unambiguously directly on the medical record abstraction form. The abstractor discussed any uncertainties with a cardiac nurse practitioner (DS), and any further concerns were reviewed with 1 of 2 board certified cardiologists (FCB or GS).
The medical record review documented the presence of cardiac complications, as well as the presence of specific potential risk factors. A patient was deemed to have a cardiac complication during the admission if the medical record provided evidence of any of the following: MI, unstable angina, CHF, atrial or ventricular arrhythmia, or pulmonary embolus. The arrhythmias required documentation with a rhythm strip or a full electrocardiogram (EKG) tracing. Unstable angina required confirmation by the attending physician. MI required confirmation by findings on EKG or on assessment of cardiac enzyme levels. CHF required confirmation by radiography or the presence of an audible S3 gallop. Pulmonary embolus required confirmation by V̇/Q̇ scanning, high-resolution computed tomography scanning, or angiography.
Risk factors, including preexisting medical conditions, were recorded as present if they were documented by a physician or by a nursing note in the medical record. The source of this information was a standard intake form administered by nursing personnel in the preadmission test center that required uniform ascertainment of medical history and of patient-recorded risk factors, such as smoking status.
After the detailed medical record review, 85 potential cases originally suspected of having a cardiac complication based upon administrative data were found not to satisfy the criteria for cardiac complications. These patients were therefore regarded as noncases and were included in the pool of potential controls. Similarly, 12 patients who were initially presumed to be controls based on administrative data were found to have had cardiac complications. These patients were therefore reclassified as cases. A total of 209 patients were found by medical record review to have cardiac complications. These patients were retained as study cases. All other chart-reviewed patients were placed into a control pool, and resampling was performed based on the same system for matching controls that was used in phase I as described above. The final sample consisted of 418 patients: 209 cases and 209 controls.
Assessment of potential risk factors
In addition to determining case status, the medical record review was also used to determine the presence or absence of potential risk factors for cardiac complications. Several categories of risk factors were ascertained: medical history, physical examination findings, EKG results, and surgical procedure.
For the medical history, the medical record abstractor obtained information about a history of hypertension, arrhythmia, MI, CHF, coronary artery bypass graft surgery, coronary stenting, hyperlipidemia, diabetes (including whether insulin-dependent or not), chronic lung disease, alcohol use, and tobacco use. The anesthesia note listed the American Society of Anesthesiology (ASA) physical status category. We also obtained data on preoperative medication use, including beta-blockers and other cardiac agents.
For the physical examination findings, the patient’s height and weight were recorded, which permitted the calculation of the body mass index (weight [in kg]/height [in m2]). We recorded certain findings of the cardiac examination, such as an S3 gallop, but these were documented infrequently and were therefore not analyzed.
For the EKG results, the preoperative EKG findings were shown on a computerized report that listed abnormalities of rate, rhythm, and QRS complex. We divided the many possible EKG abnormalities into rhythm abnormalities and abnormalities suggestive of myocardial damage (e.g., Q waves, reduced voltage).
For the surgical procedure, the medical record confirmed whether the procedure was a hip or knee replacement, whether it was a primary or revision procedure, and whether it was a unilateral or bilateral procedure.
The medical record data were quite complete. For example, only 5 patients were missing data on arrhythmia, 1 on MI, none on CHF, 3 on family history of coronary artery disease (CAD), and none on bilateral or revision procedures.
Statistical analysis
The goal of the analysis was to identify factors associated with cardiac complications during the admission. We aggregated several of the preoperative potential predictors to yield composite categories, providing more-stable estimates. For example, we created a category for “any cardiac history” to include patients who had a history of any of the following: MI, CHF, valvular disease, or arrhythmia. (These variables are intercorrelated, and hence, examining them individually is inefficient.) Because of the paired nature of the data, differences between cases and controls were evaluated with McNemar’s chi-square test in univariate analyses and with conditional logistical regression in multivariate analyses.
We performed a sensitivity analysis in which only the pairs of cases and controls that were not rematched after the medical record review were included. This analysis included 190 pairs of cases and controls and yielded results similar to those of the principal analysis; hence, these results are not reported herein.
RESULTS
Of the 209 pairs of cases and controls, 184 pairs (88%) were successfully matched for all 3 factors (age at surgery, surgeon, and year of surgery). Another 5% were matched only for surgeon and age at surgery, and 7% were matched only for surgeon.
The mean ± SD age of the 418 patients was 71.4 ± 10.1 years; 55% of them were female, and 96% were Caucasian. Twenty different surgeons operated on these patients, with the number of patients per surgeon ranging from 2 to 65. Eighty percent of procedures were primary arthroplasties, and 20% were revisions. Eleven percent were bilateral procedures, and the remainder were unilateral. Overall, 49% were hip replacement surgeries and 51% were knee replacement surgeries.
Each of the 209 cases experienced a cardiac event during the hospitalization. The individual problems among these cases included arrhythmia in 70%, hypotension in 24%, unstable angina in 8%, MI in 2%, CHF in 11%, death in 1%, and miscellaneous cardiac complications in 3%.
Results of bivariate analysis
Features of the cases and controls are shown in Table 1. There was no difference in the risk of cardiac complications according to sex, body mass index, alcohol intake, diabetes, and hypertension, hip versus knee surgery, or type of anesthesia. Factors associated with complications included age >75 years, rhythm abnormality on preoperative EKG, revision surgery, and bilateral surgery. Bone grafting was also associated with case status, but was not included in the analysis because it correlated closely with revision surgery. Similarly, higher ASA class was related to surgical complications, but this variable was not included in the analysis because it incorporates several component variables, such as history of cardiac problems. The use of COX-2 inhibitors and nonsteroidal antiinflammatory drugs did not differ between cases and controls. Approximately one-fourth of the cases and controls took COX-2 inhibitors prior to surgery, and approximately one-fourth of each group took nonsteroidal antiinflammatory drugs (Table 1). Aspirin use (data not shown) also did not differ between cases and controls. The distributions of potential risk factors among cases and controls and the crude odds ratios (ORs) with 95% confidence intervals (95% CIs) are shown in Table 1.
Table 1.
Crude and adjusted ORs for the association between potential risk factors and cardiac complications of total joint replacement*
| Factor | No. (%) of cases (n = 209) |
No. (%) of controls (n = 209) |
Crude OR (95% CI) |
Adjusted OR (95% CI) |
|---|---|---|---|---|
| Age >75 years | 88 (42) | 72 (34) | 1.9 (1.1–3.5) | 1.7 (0.9–3.4) |
| Male | 100 (48) | 88 (42) | 1.3 (0.9–2.1) | – |
| Body mass index >30 | 67 (34) | 70 (36) | 0.9 (0.6–1.4) | – |
| History of arrhythmia | 70 (33) | 31 (15) | 2.6 (1.6–4.2) | 2.6 (1.5–4.3) |
| Abnormal rhythm on preoperative EKG | 35 (18) | 17 (9) | 2.3 (1.2–4.3) | – |
| History of CAD, MI, CHF, and/or valvular disease | 71 (34) | 39 (19) | 2.2 (1.4–3.4) | 1.6 (0.9–2.6) |
| Hypertension | 127 (61) | 115 (55) | 1.3 (0.9–1.9) | – |
| Diabetes | 21 (11) | 20 (10) | 1.1 (0.6–2.0) | – |
| Use of COX-2 inhibitor | 51 (26) | 46 (23) | 1.1 (0.7–1.8) | – |
| Use of traditional NSAIDs | 45 (23) | 53 (26) | 0.9 (0.6–1.4) | – |
| Revision surgery | 55 (26) | 28 (13) | 2.2 (1.3–3.7) | 2.2 (1.2–3.9) |
| Bilateral joint replacements | 32 (15) | 13 (6) | 3.1 (1.6–6.6) | 3.5 (1.5–8.0) |
| General anesthesia | 182 (89) | 186 (91) | 0.8 (0.4–1.6) | – |
ORs = odds ratios; 95% CI = 95% confidence interval; EKG = electrocardiogram; CAD = coronary artery disease; MI = myocardial infarction; CHF = congestive heart failure; COX-2 = cyclooxygenase 2; NSAIDs = nonsteroidal antiinflammatory drugs.
Results of multivariate analysis
The adjusted ORs from the multivariate conditional logistic regression analysis are also shown in Table 1. These analyses demonstrated that age >75 years (OR 1.7 [95% CI 0.9–3.4]), history of arrhythmia (OR 2.6 [95% CI 1.5–4.3]), history of CAD, MI, CHF, and/or valvular disease (OR 1.6 [95% CI 0.9–2.6]), revision surgery (OR 2.2 [95% CI 1.2–3.9]), and bilateral surgery (OR 3.5 [95% CI 1.5–8.0]) were independent predictors of postoperative cardiac complications. In analyses that included preoperative use of beta-blockers instead of the history of cardiac-related conditions, the ORs for the other factors in the model were similar. None changed by more than 15%, and the beta-blocker OR was 2.1 (95% CI 1.3–3.4).
DISCUSSION
The results of this study confirm that several traditional risk factors for cardiac complications of noncardiac surgery also apply to the population of patients undergoing total joint arthroplasty. The study also identifies new surgical predictors of increased cardiac risk, specifically, revision surgery and bilateral surgery. Age has been traditionally identified as a risk factor; thus, we matched for age in broad categories (<50, 50–69, 70–79, ≥80 years). Nevertheless, age emerged as a risk factor in the model, reflecting an effect of age even within these age brackets. We include age in our models to ensure that the estimates of effects of other variables were age-adjusted. Moreover, a history of cardiac-related conditions, including arrhythmia, CAD, MI, CHF, or valvular disease, was associated with a significantly increased risk of adverse cardiovascular events postoperatively.
These findings are consistent with those of previous studies. In an aging population that remains active and functional, more elderly patients are undergoing TJR surgery. Most studies have shown that the risk of cardiac complications increases for persons over the age of 70 years (2–5,10). Previous studies have demonstrated that CAD, especially during the first 6 months after an MI, physical signs of CHF, or objective findings of left ventricular dysfunction identify patients with increased postoperative cardiovascular risk (2–6). This study found that as a group, patients with a history of either MI at any time, CHF, CAD, or valvular heart disease are at ~1.5 times excess risk of experiencing cardiac complications. Patients with a history of arrhythmia are also at higher risk. We emphasize that, in general, orthopedic surgery appears to be of lower risk than other types of surgery, such as abdominal and vascular surgery (6).
In this study, the use of beta-blockers predicted an increased risk of cardiac complications, because all patients who were taking beta-blockers had underlying cardiovascular disease (CAD, MI, CHF, valvular disease, or arrhythmia). The use of beta-blockers can essentially be substituted for a history of CAD, MI, CHF, or valvular disease. Beta-blocker therapy has traditionally been shown to decrease the cardiovascular risk associated with noncardiac surgery (17–19).
A key new finding from this study is that patients who undergo revision or bilateral joint replacement surgery are at significantly higher increased risk than patients who undergo unilateral, primary procedures. Revision joint replacement and bilateral surgery are much more prolonged operations than primary unilateral joint replacement. These findings suggest an increased risk with more prolonged surgery.
This study is limited by its medical record–based design, which precludes evaluation of risk factors that were not captured in the medical records. For example, while preoperative functional status and mental health status might plausibly be related to cardiac complications, these variables were not captured routinely and therefore could not be evaluated. The major strength of the study is the large sample size of patients undergoing elective total hip and total knee replacement surgeries at the institution. In particular, the volume of revision and bilateral procedures enabled us to identify the increased risk associated with revision and bilateral surgery. We did not present data on operative variables, such as time of procedure or tourniquet time (for total knee replacements), because these data were missing for a number of the patients and because the goal of the analysis was to examine variables that could be ascertained preoperatively.
In summary, this case–control study confirmed the traditional factors that lead to increased cardiovascular complications of TJR surgery. These risk factors include age, underlying heart disease, and a history of arrhythmia (or, as a substitute for history of heart disease or arrhythmia, a history of beta-blocker use). This study identified a new high-risk group, namely, patients undergoing revision or bilateral TJR surgery. These patients will incur a 2–3.5-fold increased risk as compared with a group of matched control patients. Clinicians can use this information to better estimate the risk of cardiovascular complications following TJR surgery and, ultimately, to prevent and better manage these complications.
Acknowledgments
Supported by the New England Baptist Hospital and by the NIH (grants K24-AR-02123 and P60-AR-47782).
Footnotes
AUTHOR CONTRIBUTIONS
Drs. Katz, Wright, and Losina had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study design. Basilico, Sweeney, Losina, Wright, Katz.
Acquisition of data. Basilico, Sweeney, Gaydos, Skoniecki.
Analysis and interpretation of data. Basilico, Sweeney, Losina, Gaydos, Skoniecki, Wright, Katz.
Manuscript preparation. Basilico, Sweeney, Losina, Gaydos, Skoniecki, Wright, Katz.
Statistical analysis. Losina, Wright.
REFERENCES
- 1.Eagle KA, Berger PB, Calkins H, Chaitman BR, Ewy GA, Fleischmann KE, et al. ACC/AHA guideline update for perioperative cardiovascular evaluation for noncardiac surgery—executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1996 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery) [published erratum appears in J Am Coll Cardiol 2006;47:2356] J Am Coll Cardiol. 2002;39:542–553. doi: 10.1016/s0735-1097(01)01788-0. [DOI] [PubMed] [Google Scholar]
- 2.Goldman L, Caldera DL, Nussbaum SR, Southwick FS, Krogstad D, Murray B, et al. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med. 1977;297:845–850. doi: 10.1056/NEJM197710202971601. [DOI] [PubMed] [Google Scholar]
- 3.Desky AS, Abrams HB, Forbath N, Scott JG, Hilliard JR. Cardiac assessment for patients undergoing noncardiac surgery: a multifactorial clinical risk index. Arch Intern Med. 1986;146:2131–2134. [PubMed] [Google Scholar]
- 4.Goldman L. Multifactorial index of cardiac risk in noncardiac surgery: ten year status report. J Cardiothorac Anesth. 1987;1:237–244. doi: 10.1016/s0888-6296(87)80011-x. [DOI] [PubMed] [Google Scholar]
- 5.Mangano DT, Goldman L. Preoperative assessment of patients with known or suspected coronary disease. N Engl J Med. 1995;333:1750–1756. doi: 10.1056/NEJM199512283332607. [DOI] [PubMed] [Google Scholar]
- 6.Lee TH, Marcantonio ER, Mangione CM, Thomas EJ, Polanczyk CA, Cook EF, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 1999;100:1043–1049. doi: 10.1161/01.cir.100.10.1043. [DOI] [PubMed] [Google Scholar]
- 7.Cohn SL, Goldman L. Preoperative risk evaluation and perioperative management of patients with coronary artery disease. Med Clin North Am. 2003;87:111–136. doi: 10.1016/s0025-7125(02)00143-8. [DOI] [PubMed] [Google Scholar]
- 8.Mahomed NN, Barrett JA, Katz JN, Phillips CB, Losina E, Lew RA, et al. Rates and outcomes of primary and revision total hip replacement in the United States Medicare population. J Bone Joint Surg Am. 2003;85:27–32. doi: 10.2106/00004623-200301000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Barrett J, Losina E, Baron JA, Mahomed NN, Wright J, Katz JN. Survival following total hip replacement. J Bone Joint Surg Am. 2005;87:1965–1971. doi: 10.2106/JBJS.D.02440. [DOI] [PubMed] [Google Scholar]
- 10.Bhattacharyya T, Iorio R, Healy W. Rate of and risk factors for acute inpatient mortality after orthopaedic surgery. J Bone Joint Surg Am. 2002;84:562–572. doi: 10.2106/00004623-200204000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Katz JN, Barrett J, Mahomed NN, Baron JA, Wright RJ, Losina E. Association between hospital and surgeon procedure volume and the outcomes of total knee replacement. J Bone Joint Surg Am. 2004;86:1909–1916. doi: 10.2106/00004623-200409000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Kahn RL, Hargett MJ, Urquhart B, Sharrock NE, Peterson MG. Supraventricular tachyarrhythmias during total joint arthroplasty. Clin Orthop Relat Res. 1993;296:265–269. [PubMed] [Google Scholar]
- 13.Polanczyk CA, Goldman L, Marcantonio ER, Orav EJ, Lee TH. Supraventricular arrhythmia in patients having noncardiac surgery: clinical correlates and effect on length of stay. Ann Intern Med. 1998;129:279–285. doi: 10.7326/0003-4819-129-4-199808150-00003. [DOI] [PubMed] [Google Scholar]
- 14.Christians KK, Wu B, Quebbeman EJ, Brasel KJ. Postoperative atrial fibrillation in noncardiothoracic surgical patients. Am J Surg. 2001;182:713–715. doi: 10.1016/s0002-9610(01)00799-1. [DOI] [PubMed] [Google Scholar]
- 15.Nazon D, Abergel G, Hatem CM. Critical care in orthopedic and spine surgery. Crit Care Clin. 2003;19:33–53. doi: 10.1016/s0749-0704(02)00052-0. [DOI] [PubMed] [Google Scholar]
- 16.Agency for Healthcare Research and Quality. Healthcare cost and utilization project. 2004 http://hcupnet.ahrq.gov/
- 17.Lindenauer PK, Pekow P, Wang K, Mamidi DK, Gutierrez B, Benjamin EM. Perioperative beta-blocker therapy and mortality after major noncardiac surgery. N Engl J Med. 2005;353:349–361. doi: 10.1056/NEJMoa041895. [DOI] [PubMed] [Google Scholar]
- 18.McGory ML, Maggard MA, Ko CY. A meta-analysis of perioperative beta blockade: what is the actual risk reduction? Surgery. 2005;138:171–179. doi: 10.1016/j.surg.2005.03.022. [DOI] [PubMed] [Google Scholar]
- 19.Mangano DT, Layug EL, Wallace A, Tateo I for the Multicenter Study of Perioperative Ischemia Research Group. Effect of atenolol on mortality and cardiovascular morbidity after noncardiac surgery [published erratum appears in N Engl J Med 1997;336:1039] N Engl J Med. 1996;335:1713–1720. doi: 10.1056/NEJM199612053352301. [DOI] [PubMed] [Google Scholar]