Abstract
Purpose
We analyzed the prescriptions of alpha-blockers and phosphodiesterase 5 inhibitors (PDE5Is) in the urology department as well as in other departments of the general hospital.
Methods
We investigated the frequency of prescription of alpha-blockers and PDE5Is from 3 general hospitals from January 1, 2007 to December 31, 2009. For alpha-blockers, data were collected from patients to whom alpha-blockers were prescribed from among patients recorded as having benign prostatic hyperplasia according to the 5th Korean Standard Classification of Diseases. For PDE5Is, data were collected from patients to whom PDE5Is were prescribed by the urology department and by other departments. Alpha-blockers were classified into tamsulosin, alfuzosin, doxazosin, and terazosin, whereas PDE5Is were classified into sildenafil, tadalafil, vardenafil, udenafil, and mirodenafil.
Results
Alpha-blockers were prescribed to 11,436 patients in total over 3 years, and the total frequency of prescriptions was 68,565. Among other departments, the nephrology department had the highest frequency of prescription of 3,225 (4.7%), followed by the cardiology (3,101, 4.5%), neurology (2,576, 3.8%), endocrinology (2,400, 3.5%), pulmonology (1,102, 1.6%), and family medicine (915, 1.3%) departments in order. PDE5Is were prescribed to 2,854 patients in total over 3 years, and the total frequency of prescriptions was 10,558. The prescription frequency from the urology department was 4,900 (46.4%). Among other departments, the endocrinology department showed the highest prescription frequency of 3,488 (33.0%), followed by the neurology (542, 5.1%), cardiology (467, 4.4%), and family medicine (407, 3.9%) departments in order.
Conclusions
A high percentage of prescriptions of alpha-blockers and PDE5Is were from other departments. For more specialized medical care by urologists is required in the treatment of lower urinary tract symptoms and erectile dysfunction.
Keywords: Adrenergic alpha-1 Receptor Antagonists, Phosphodiesterase 5 Inhibitors, Prescriptions
INTRODUCTION
Adrenergic alpha-1 receptor antagonists (alpha blockers) and phosphodiesterase 5 inhibitors (PDE5Is) are the first-line treatment for lower urinary tract symptoms (LUTS) as well as erectile dysfunction (ED) [1]. For benign prostatic hyperplasia (BPH) accompanied by LUTS, the European Association of Urology encourages the pretreatment recommended assessment to include a medical history, symptom score, prostate-specific antigen (PSA) measurement, physical examination including a digital rectal examination, serum creatinine, urinalysis, flow rate, and post-voided residual urine (PVR) [2]. For ED, a basic workup should be performed, primarily including identification of the presence of hypertension, diabetes mellitus, myocardial disease, lipidemia, hypercholesterolemia, renal insufficiency, hypogonadism, neurologic disorders, and psychiatric disorders [3]. For the determination of the causes of ED after the basic workup, vascular studies, neurologic studies, endocrinologic studies, and specialized psychodiagnostic evaluation shall be performed for nocturnal penile tumescence and rigidity using Rigiscan, intracavernous vasoactive drug injection, and duplex ultrasound of the cavernous arteries. Both LUTS/BPH and ED can be assessed according to symptoms and treatment results by urological evaluation and questionnaires such as the International Prostate Symptom Score (IPSS), Overactive Bladder Symptom Scores, International Index of Erectile Function (IIEF), and the Sexual Health Inventory for Men for basic workup on a regular basis [4,5].
Thus, the pretreatment assessments of BPH/LUTS and ED are complicated and require prescriptions of alpha-blockers and PDE5Is, which are the primary therapeutic agents prescribed after the assessments are completed by use of the various urological diagnostic tools. A physician's lack of urologic knowledge can result in poor adherence. So far, there have been no reports in Korea on the actual prescription of alpha-blockers and PDE5Is by clinical departments other than the urology department. In the present study, therefore, the authors analyzed the prescriptions of alpha-blockers and PDE5Is in the treatment of BPH/LUTS and ED in outpatient medical examinations in the urology department as well as in other departments of the general hospital and considered the problems caused by the use of these agents by other departments.
MATERIALS AND METHODS
For this study, an investigation was conducted on the frequency of prescription of alpha-blockers and PDE5Is from 3 general hospitals from January 1, 2007 to December 31, 2009. For alpha-blockers, the data were collected from patients to whom alpha-blockers were prescribed from among patients recorded as having benign prostatic hyperplasia according to the 5th Korean Standard Classification of Diseases. For PDE5Is, the data were collected from patients to whom PDE5Is were prescribed by the urology department and by other departments. The period of data collection and analysis was from July 2010 to June 2011. Alpha-blockers were classified into tamsulosin, alfuzosin, doxazosin, and terazosin, whereas PDE5Is were classified into sildenafil, tadalafil, udenafil, vardenafil, and mirodenafil. The ages of the patients prescribed the above drugs for 3 years, the prescription frequency for the same patient, and the mean number of pills prescribed for a one-time dose were analyzed according to drug. The data collected included the prescription records of all 3 general hospitals for 3 years.
Sample data were analyzed with descriptive analysis, using Open Office.org Calc (Open Office.org ver. 3.2.0, Oracle Co., Redwood Shores, CA, USA), and with the chi-square test using MedCalc (MedCalc ver. 11.2.1.0, MedCalc Software, Mariakerke, Belgium). For the statistical analysis, P-values less than 0.05 were considered statistically significant.
RESULTS
Alpha-Blockers
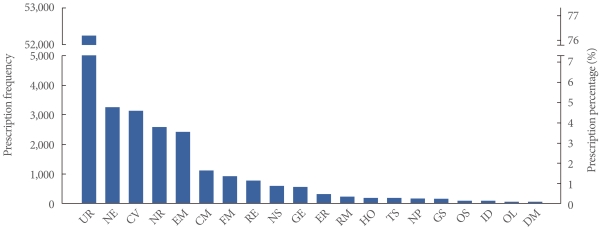
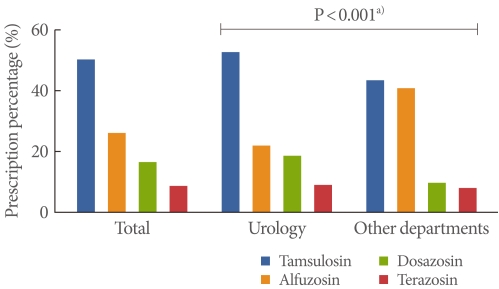
Alpha-blockers were prescribed to 11,436 patients in total over 3 years, and the total frequency of prescriptions was 68,565. The mean frequency of prescription in the same patient was 5.54 (range, 1 to 63) times, and the mean age of the patients was 64.12±11.12 years old. The prescription frequency from the urology department was 52,220 times (76.2%). The nephrology department showed the next highest frequency of prescription of 3,225 (4.7%), followed by the cardiology department (3,101, 4.5%), the neurology department (2,576, 3.8%), the endocrinology department (2,400, 3.5%), the pulmonology department (1,102, 1.6%), and the family medicine department (915, 1.3%) in order (Fig. 1). The prescription frequency by drug was as follows: tamsulosin, 34,212 (49.9%); alfuzosin, 17,714 (25.8%); doxazosin, 10,980 (16.0%); and terazosin, 5,659 (8.3%). The prescription frequency from the urology department was as follows: tamsulosin, 27,195 (52.1%); alfuzosin, 11,124 (21.3%); doxazosin, 9,450 (18.1%); and terazosin, 4,451 (8.5%). Drugs prescribed from the other departments showed the same order of frequency as did the urology department as follows: tamsulosin, 7,017 (42.9%); alfuzosin, 6,590 (40.3%); doxazosin, 1,530 (9.4%); and terazosin, 1,208 (7.4%). The prescription frequency between the urology department and the other departments showed statistically significant differences, however (P<0.001) (Fig. 2).
Fig. 1.
Comparison of prescription of alpha-blockers for 3 years. UR, urology; NE, nephrology; CV, cardiology; NR, neurology; EM, endocrinology; CM, pulmonology; FM, family medicine; RE, rehabilitation medicine; NS, neurosurgery; GE, gastroenterology; ER, emergency medicine; RM, rheumatology; HO, hemato-oncology; TS, chest surgery; NP, neuropsychiatrics; GS, general surgery; OS, orthopaedic surgery; ID, infectious disease; OL, otolaryngology; DM, dermatology.
Fig. 2.
The percentage of prescription of alpha-blockers from the urology department and from the other departments. a)Pearson's chi-square test.
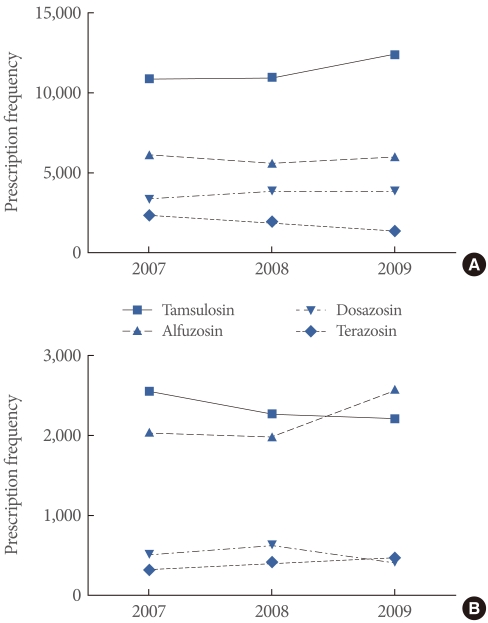
Over the 3 years studied, the prescriptions of tamsulosin from all hospitals were 10,864 (2007), 10,959 (2008), and 12,389 (2009), and there were no significant differences (Fig. 3A). Over the 3 years studied, the prescriptions of tamsulosin versus alfuzosin from departments other than the urology department were 2,546 vs. 2,042 (2007), 2,263 vs. 1,977 (2008), and 2,208 vs. 2,571 (2009) (Fig. 3B).
Fig. 3.
Yearly variations in the prescription of alpha-blockers (A) From all departments; (B) From departments other than the urology department.
Phosphodiesterase 5 Inhibitors
PDE5Is were prescribed to 2,854 patients in total over 3 years, and the total frequency of prescriptions was 10,558. The mean age of the patients was 58.36±0.10 years, and the mean frequency of prescription in the same patient was 3.70 (range, 1 to 36) times with the mean number of pills prescribed for a one-time dose being 7.54±0.17. The prescription frequency from the urology department was 4,900 (46.4%). Among other departments, the endocrinology department showed the highest prescription frequency of 3,488 (33.0%), followed by the neurology department (542, 5.1%), the cardiology department (467, 4.4%), and the family medicine department (407, 3.9%) in order (Fig. 4). The prescription frequency by drug was as follows: sildenafil, 4,345 (41.2%); tadalafil, 2,518 (23.8%); udenafil, 2,301 (21.8%); vardenafil, 984 (9.3%); and mirodenafil, 410 (3.9%). The prescription frequency from the urology department was as follows: sildenafil, 1,758 (35.9%); tadalafil, 1,403 (28.6%); udenafil, 763 (15.6%); vardenafil, 707 (14.4%); and mirodenafil, 269 (5.5%). The frequency of prescription of drugs by the other departments was as follows: sildenafil, 2,587 (45.7%); udenafil, 1,538 (27.2%); tadalafil, 1,115 (19.7%); vardenafil, 277 (4.9%); and mirodenafil, 141(2.5%). The prescription frequency between the urology department and the other departments showed statistically significant differences (P<0.001) (Fig. 5).
Fig. 4.
Comparison of prescription of phosphodiesterase 5 inhibitors for 3 years. UR, urology; EM, endocrinology; NR, neurology; CV, cardiology; GE, gastroenterology; NE, nephrology; RM, rheumatology; NP, neuropsychiatrics; TS, chest surgery; PD, pediatrics; NS, neurosurgery; OG, obsterics-gynecology; RE, rehabilitation medicine; GS, general surgery; CM, pulmonology; OS, orthopaedic surgery; DM, dermatology; OT, ophthalmology; ER, emergency medicine; ID, infectious disease; RT, therapeutic radiology; SP, pediatric surgery.
Fig. 5.
The percentage of prescription of phosphodiesterase 5 inhibitors from the urology department and from the other departments. a)Pearson's chi-square test.
In the 3 years studied, prescriptions of tadalafil from all hospitals surpassed those of udenafil in 2009 (1,126 vs. 738), whereas no substantial differences in the prescription of sildenafil were shown (1,423 in 2007, 1,473 in 2008, and 1,449 in 2009) (Fig. 6A). Concerning the prescription of PDE5Is from departments other than the urology department over the 3 years studied, udenafil was prescribed at a higher percentage compared with tadalafil each year, unlike the result for all hospitals combined (Fig. 6B).
Fig. 6.
Yearly variations in the prescription of phosphodiesterase 5 inhibitors (A) From all departments; (B) From departments other than the urology department.
DISCUSSION
Medical adherence (the degree to which a patient follows the recommendations of health professionals) is a salient outcome of the process of care. Poor adherence is affected by patient-related, physician-related, and health system/team building-related factors [6]. In particular, physician-related factors are grounded on a good physician-patient relationship and play an important role in increasing medical adherence [7]. The ways in which physicians contribute to patients' poor adherence include failing to explain the benefits and side effects of a medication adequately, not giving consideration to the patient's lifestyle or the cost of the medications, and having poor therapeutic relationships with patients [8-10]. According to a meta-analysis conducted by Zolnierek and Dimatteo [11] that analyzed 127 pieces of literature, communication and medical adherence had a higher correlation depending on whether the physician was a specialist or not (r=2.2, P=0.022). To this end, it is considered that the relationship, communication, and detailed explanation by the physician play important roles in increasing medical adherence in the treatment of chronic disease.
In the field of urology, Collins et al. [12] reported on the differences in practice patterns of 444 primary care physicians (PCPs) and 394 urologists in the United States in the diagnosis and treatment in 1997 in compliance with the 1994 version of the Agency for Health Care Policy and Research BPH guidelines. Among PCPs and urologists, respectively, approximately 18% and 63% had routinely conducted the American Urological Association symptom scoring, respectively, whereas 1% and 40% had conducted uroflowmetry and 3% and 39% had performed routine PVR identification with use of ultrasonography. These differences were statistically significant. In that study, the authors analyzed the practice patterns of PCPs who had been trained in the diagnosis and treatment of BPH according to the guidelines; therefore, no direct comparison can be made with the diagnostic tools being used by physicians of other departments in Korea when they prescribe alpha-blockers. Nevertheless, it is possible to see that PCPs in the United States also show lower percentages statistically in the use of recommended diagnostic tools compared with urologists. In 2004, Seftel et al. [13] also conducted a comparative study on the practice patterns of 351 PCPs and 437 urologists in the United States for patients with BPH/LUTS and sexual dysfunction. Among PCPs, only 41% had used the IPSS for the evaluation of LUTS, whereas 97% of urologists had used it for the same purpose. Conversely, 26% of PCPs had used BPH medication, whereas 21% of urologists had used it. The authors concluded that more systematic education is required for PCPs on the diagnosis and treatment of patients with BPH. According to recently reported research, the IPSS is being used as an initial diagnostic test for BPH by 98% of Korean urologists in general hospitals and by 73.3% in private urologic clinics in comparison with uroflowmetry, which was used by 90.0% and by 50.0%, respectively [14]. This result was similar to the results for urologists from the research of Seftel et al. [13], which makes it possible to infer that diagnosis and treatment by clinicians other than urologists may be insufficient.
Rutchik et al. [15] reported on the practice patterns of family practitioners for ED. They reported that 84% of family practitioners carried out history taking as well as physical examination and approximately 60% of them performed hormone and chemical laboratory tests, but only 2 to 3% of them performed Rigiscan or penile Doppler ultrasound. In 2006, Young et al. [16] reported the interesting results of their analysis of the sildenafil-prescribing patterns of urologists and physicians of family medicine as well as internal medicine by use of data from the National Center for Health Statistics in the United States. Urologists documented erectile or psychosexual dysfunction significantly more often than did family medicine, internal medicine, and other physicians (P=0.003). Those results, which presented the actual prescription of medication in a cross-sectional manner for patients with ED in the United States, showed that urologists prescribed with the highest frequency. In present study, the result showed that 46.4% of physicians in the urology department had prescribed PDE5Is, whereas 33% of the endocrinology department had prescribed PDE5Is. In the case of primary physicians, it is considered that PDE5Is would be prescribed in other departments at a higher frequency than the PDE5Is prescription ratio of a medical center. Nonetheless, this result requires identification of the cause of ED by performing a medical and psychosexual history with the use of validated instruments such as the IIEF at the basic diagnostic workup with subsequent physical examination and laboratory tests [17]. Because Korean linguistic validation has been completed of questionnaires such as the IIEF and IIEF-5, such instruments can be effective tools for history taking [18,19].
Our study is an observational study that investigated the prescription frequencies of alpha-blockers and PDE5Is of each clinical department from 3 different general medical centers. Although it was not possible to take into consideration the performance of the first medical examination and urological consultation in the subjected data, it was identified that alpha-blockers and PDE5Is were prescribed often by departments other than the urology department. This is the first domestic report of these data. Also, studies of practical patterns of the family medicine department or the actual primary physicians are lacking. Thus, the implications of the present results are various.
In conclusion, alpha-blockers and PDE5Is are the most widely used drugs in the urology department, requiring specialized knowledge for their prescription. However, in this study, it was found that these drugs were being prescribed at a high frequency by other departments. Given the fact that a high ratio of the prescriptions were from other departments, it appears that far more specialized medical care by urologists is required in the treatment of LUTS/BPH and ED.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Wang C. Phosphodiesterase-5 inhibitors and benign prostatic hyperplasia. Curr Opin Urol. 2010;20:49–54. doi: 10.1097/MOU.0b013e328333ac68. [DOI] [PubMed] [Google Scholar]
- 2.Madersbacher S, Alivizatos G, Nordling J, Sanz CR, Emberton M, de la Rosette JJ. EAU 2004 guidelines on assessment, therapy and follow-up of men with lower urinary tract symptoms suggestive of benign prostatic obstruction (BPH guidelines) Eur Urol. 2004;46:547–554. doi: 10.1016/j.eururo.2004.07.016. [DOI] [PubMed] [Google Scholar]
- 3.Wespes E, Amar E, Hatzichristou D, Hatzimouratidis K, Montorsi F, Pryor J, et al. EAU Guidelines on erectile dysfunction: an update. Eur Urol. 2006;49:806–815. doi: 10.1016/j.eururo.2006.01.028. [DOI] [PubMed] [Google Scholar]
- 4.Porru D, Jallous H, Cavalli V, Sallusto F, Rovereto B. Prognostic value of a combination of IPSS, flow rate and residual urine volume compared to pressure-flow studies in the preoperative evaluation of symptomatic BPH. Eur Urol. 2002;41:246–249. doi: 10.1016/s0302-2838(02)00021-0. [DOI] [PubMed] [Google Scholar]
- 5.Rosen RC, Cappelleri JC, Smith MD, Lipsky J, Peña BM. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11:319–326. doi: 10.1038/sj.ijir.3900472. [DOI] [PubMed] [Google Scholar]
- 6.Brown MT, Bussell JK. Medication adherence: WHO cares? Mayo Clin Proc. 2011;86:304–314. doi: 10.4065/mcp.2010.0575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 8.Black HR. Will better-tolerated antihypertensive agents improve blood pressure control? JNC VI revisited. Am J Hypertens. 1999;12(12 Pt 3):225S–230S. doi: 10.1016/s0895-7061(99)00102-8. [DOI] [PubMed] [Google Scholar]
- 9.Elliott WJ, Maddy R, Toto R, Bakris G. Hypertension in patients with diabetes. Overcoming barriers to effective control. Postgrad Med. 2000;107:29–32. 35–36, 38. doi: 10.3810/pgm.2000.03.940. [DOI] [PubMed] [Google Scholar]
- 10.Golin CE, Liu H, Hays RD, Miller LG, Beck CK, Ickovics J, et al. A prospective study of predictors of adherence to combination antiretroviral medication. J Gen Intern Med. 2002;17:756–765. doi: 10.1046/j.1525-1497.2002.11214.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zolnierek KB, Dimatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47:826–834. doi: 10.1097/MLR.0b013e31819a5acc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Collins MM, Barry MJ, Bin L, Roberts RG, Oesterling JE, Fowler FJ. Diagnosis and treatment of benign prostatic hyperplasia. Practice patterns of primary care physicians. J Gen Intern Med. 1997;12:224–229. doi: 10.1046/j.1525-1497.1997.012004224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seftel AD, Rosen RC, Rosenberg MT, Sadovsky R. Benign prostatic hyperplasia evaluation, treatment and association with sexual dysfunction: practice patterns according to physician specialty. Int J Clin Pract. 2008;62:614–622. doi: 10.1111/j.1742-1241.2008.01699.x. [DOI] [PubMed] [Google Scholar]
- 14.Oh CY, Lee SH, Yoo SJ, Chung BH. Korean urologist's view of practice patterns in diagnosis and management of benign prostatic hyperplasia: a nationwide survey. Yonsei Med J. 2010;51:248–252. doi: 10.3349/ymj.2010.51.2.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rutchik SD, Baudiere M, Wade M, Sullivan G, Rayford W, Goodman J. Practice patterns in the diagnosis and treatment of erectile dysfunction among family practice physicians. Urology. 2001;57:146–150. doi: 10.1016/s0090-4295(00)00880-3. [DOI] [PubMed] [Google Scholar]
- 16.Young SE, Mainous AG, 3rd, Diaz VA, Everett CJ. Practice patterns in sildenafil prescribing. Fam Med. 2006;38:110–115. [PubMed] [Google Scholar]
- 17.Hatzimouratidis K, Amar E, Eardley I, Giuliano F, Hatzichristou D, Montorsi F, et al. Guidelines on male sexual dysfunction: erectile dysfunction and premature ejaculation. Eur Urol. 2010;57:804–814. doi: 10.1016/j.eururo.2010.02.020. [DOI] [PubMed] [Google Scholar]
- 18.Chung TG, Lee TK, Chung S, Lee MS, Kim YS, Ahn TY. The Korean Version of the International Index of Erectile Function (IIEF): Reliability and Validation Study. Korean J Urol. 1999;40:1334–1343. [Google Scholar]
- 19.Ahn TY, Lee DS, Kang WC, Hong JH, Kim YS. Validation of an abridged Korean Version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Korean J Urol. 2001;42:535–540. [Google Scholar]