Abstract
Background
Sunlight contains UV radiation that affects human health in both detrimental (skin cancers) and beneficial (vitamin D3) ways. An evaluation of the vitamin D status of adult Americans (22–40, 41–59, 60+ yr) show many have deficient or insufficient serum levels of 25-hydroxyvitamin D, indicating they are not getting enough from dietary sources or sunlight. Those findings are in conflict with calculated values from the American Academy of Dermatology who insist people make “ample” vitamin D3 (≥1,000 IU/day) from their “casual,” or everyday, outdoor UV exposures even if they use sunscreens with sun protection factor 15.
Objective
We investigated this situation using the everyday outdoor UV doses of indoor-working adult Americans (∼7,000) in the north (45°N) and south (35°N) to calculate how much vitamin D3 they produce each season with and without vacationing.
Results
Only during the summer can skin type II Caucasian adults (21–59 yr) meet their minimum (600 IU/day) vitamin D3 needs from everyday exposures, but only if they do not wear professional clothes or sunscreens (except beach vacations).
Method
To do vitamin D3 calculations properly, we used action spectrum and geometric conversion factors, not previously incorporated into other calculations.
Conclusions
Most adult Americans do not go outside enough to meet their minimum or optimum (≥1,200 IU/day) vitamin D3 needs all year. The darker skin types (III–VI) and the oldest people (>59 yr) are at the highest risk for not making enough vitamin D3 during the year from everyday outdoor exposures even with a 2–3 week summer vacation.
Key words: age, benefit, environment, health, race, risk, sunlight, sunscreen, vitamin D
Introduction
Sunlight can affect human health because it contains UV radiation (290–400 nm) that has both detrimental (skin cancers) and beneficial (vitamin D3) health effects. Vitamin D3 is formed in human skin when the UVB photons (290–315 nm) in sunlight break the B ring of the precursor molecule, 7-dehydrocholesterol or provitamin D3 forming previtamin D3, which thermally isomerizes (37°C) to vitamin D3 by a membrane enhanced mechanism.1,2
Vitamin D3 affects a variety of adult health problems besides osteoporosis and osteomalcia. It lowers blood pressure in hypertensive patients3,4 and the incidence and severity of cardiovascular disorders.5–8 Vitamin D decreases the incidence of type 2 diabetes,9,10 rheumatoid arthritis,11,12 and it prevents tooth loss13 and falls that can result in hip fractures of the elderly.14–16 The most hormonally active form of vitamin D, 1,25-dihydroxyvitamin D (1,25(OH)2D), can affect a variety of cancers because cancer cells produce 1,25(OH)2D from either 25(OH)D17 or vitamin D,18 which can kill them via apoptotic cell death. This hormonal conversion to 1,25(OH)2D inside the cancer cell may be responsible for reducing the mortality from different cancers:19 colon, breast, prostate, ovarian and melanoma.20–26 In support of those findings, is the reverse observation that about half the patients attending an outpatient, cancer-care clinic in Boston were vitamin D deficient during the summer.27 Production of 1,25(OH)2D in skin cells may be important for decreasing the incidence of melanoma28 because it causes growth inhibition and apoptosis in vitro and in vivo of melanoma cells.29–31 Ironically, regular, moderate sun exposures increase the survival of melanoma patients.20 In fact, more deaths occur from internal cancers and disorders associated with low UV exposures (50,000–63,000/yr), which are often related to lower serum levels of 25-hydroxyvitamin D (25(OH) D), than from high UV exposures that are often related to skin cancers, especially melanoma (about 10,000/yr).32,33
For most people, their major source of vitamin D comes from exposing their skin to sunlight,34 which creates a public health dilemma because the UV radiation in sunlight also causes skin cancers. Skin cancers have been increasing at the alarming rate of about 4% (±1%) each year, so that health organizations have been warning the public to avoid sun exposure between 10 A.M. and 4 P.M. and have been advising them to wear protective clothing, sunglasses and sunscreens with sun protection factor (SPF) ≥15 while outdoors.35 However, the vitamin D status, measured in serum as 25(OH)D (where the ‘D’ represents D2 or D3), shows many American adults have insufficient levels (<75 nmol/L or <30 ng/ml) 17 for most of the year, especially during and after winter.36–41 These observations disagree with a recent publication by the American Academy of Dermatology that claims Americans are getting adequate “casual,” or everyday, UV exposures even if they diligently wear SPF 15 sunscreen, to make ample (≥1,000 IU/day) vitamin D3.42
However, we found many American children (<20 yr) are not getting enough everyday outdoor UV exposures43 to meet either their minimum (600 IU/day) or optimum (>1,200 IU/day) vitamin D3 needs for most of the year, except some Caucasian children during the summer, but only if they do not wear sunscreens except on beach vacations.44 African American children are not even making the minimum amount of vitamin D all year due to the increased sunscreening effect of the melanin in their skin.45
Here we investigated the indoor-working adult American's (≥22 yr) situation by calculating the amount of vitamin D3 they make from their everyday exposure to sunlight. We used UV doses calculated46 from an Environmental Protection Agency two-year survey of 9,386 Americans,47 over 7,000 of which were adults, located all over the contiguous United States (US). We first adjusted their erythemally-weighted UV doses to previtamin D3-weighted UV doses using action spectrum conversion factors (ASCF),48 and then adjusted those previtamin D3-weighted UV doses relative to the horizontal plane to UV doses relevant to the human body using geometric conversion factors (GCF).49 We calculated both male and female indoor-working adult Americans' (22–40, 41–59, 60+ yr) vitamin D3 production in international units (IU) produced by Fitzpatrick skin types II, III, IV and V50 during each season of the year in the north (45°N) and south (35°N). We also take the decreasing capacity to make vitamin D3 with increasing age into account51 and calculate the average amount people make everyday during the summer with or without a 1–3-week mixed vacation.
Results
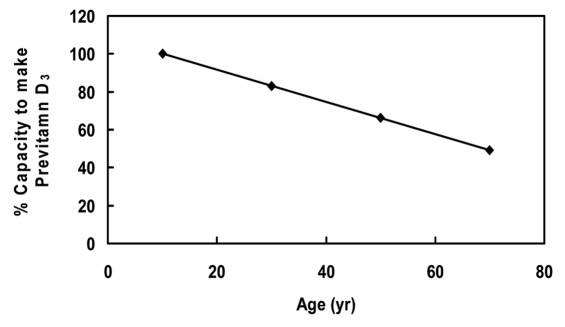
Figure 1 shows a decreasing capacity to make vitamin D3 with increasing age. We normalized the data from MacLaughlin and Holick (1985) 51 using the American children (0–20 yr) because they have the highest capacity to make vitamin D3 (100% or 1.0). Compared to American children (<22 yr), the youngest adult Americans (22–40 yr) have 83% (or 0.83) and the middle-aged adults (41–59 yr) have 66% (or 0.66), while the senior adults (60+ yr) only have 49% (or 0.49) their capacity to make vitamin D3. We used these fractions in the vitamin D3 calculations for the different age groups of adults presented in Figures 2–5.
Figure 1.
The percent drop in the ability to make vitamin D3 in human skin with age. We normalized values to 100% using the children's values (0–20 yr). The data plotted is the average of vitamin D3 formed in the epidermis and dermis from 0–20 yr (100%), 22–40 yr (83%), 41–59 yr (66%) and 60+ yr (49%); calculated from the data in Figure 1 of MacLaughlin and Holick (1985). Note that some seniors over 70 yr make less than 25% of the vitamin D that children <21 yr can make.67
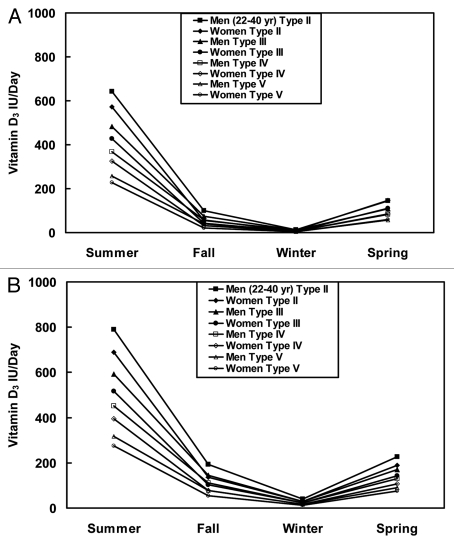
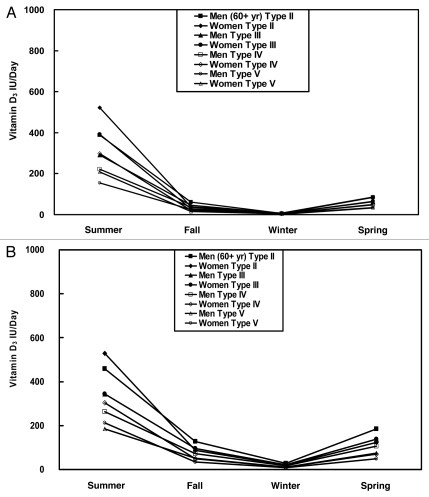
Figure 2.
The average amount of vitamin D3 (IU/day) indoor-working adult men and women of reproductive age (22–40 yr) with skin types II–V make from everyday outdoor UV exposures each season in the (A) Northern (45°N) and (B) Southern (35°N) US.
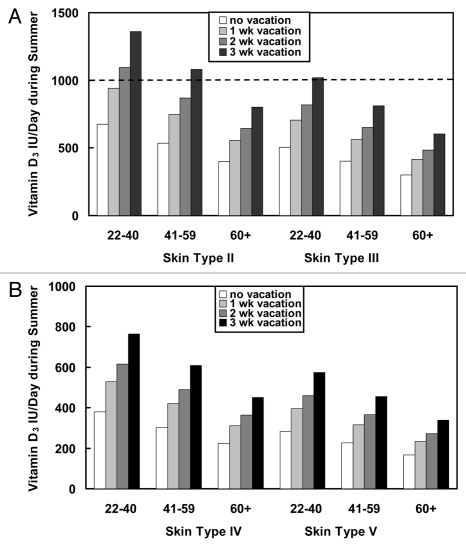
Figure 5.
The average amount of vitamin D3 made by indoor-working adults every day during the summer without taking a summer vacation compared to the amount made by indoor-working adults of different ages and skin types if they take a 1-, 2- or 3-week “mixed” summer vacation at latitude ∼40°N in the continental US. The dashed lines indicate the recommended IU/day of vitamin D for people under (600 IU/day) and people over 70 yr (800 IU/day). A mixed summer vacation is the average of four types of vacations: beach, country, sightseeing and home; (A) skin types II and III and (B) skin types IV and V.
Figure 2 shows the average amounts of vitamin D3 (IU/day) made by indoor-working adult Americans of reproductive/child-rearing ages (22–40 yr) with Fitzpatrick skin types II–V during each season of the year, excluding vacations and sunscreen use (see in ref. 44) in the north (45°N, Fig. 2A) and south (35°N, Fig. 2B). Caucasians with skin type II (also includes type I) can make the minimum amount of vitamin D3 (∼600 IU/day) during the summer so that they are not deficient, but only if they wear “sporty” clothing and do not wear sunscreens except on beach vacations. Almost no one else, except some outdoor workers, in the young adult age group can make enough vitamin D3 to meet his or her needs all year.
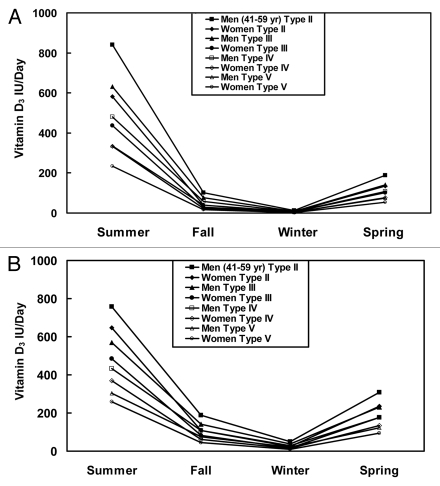
Figure 3 shows the average amounts of vitamin D3 (IU/day) made by middle-aged (41–59 yr) indoor-working Americans with Fitzpatrick skin types II–V during each season of the year, excluding vacations and sunscreen use, in the north (45°N; Fig. 3A) and south (35°N, Fig. 3B). Again, only Caucasians with skin type II (and type I) can make enough vitamin D3 to meet their needs during the summer, but only if they wear “sporty” clothing and do not wear sunscreens except on beach vacations. Almost no one else, except some outdoor workers, can make enough vitamin D3 to meet his or her needs all year.
Figure 3.
The average amount of vitamin D3 (IU/day) indoor-working adult men and women of middle age (41–59 yr) with skin types II–V make from everyday outdoor UV exposures each season in the (A) Northern (45°N) and (B) Southern (35°N) US.
Figure 4 shows the average amounts of vitamin D3 (IU/day) made by senior (60+ yr) indoor-working or retired Americans with Fitzpatrick skin types II–V during each season of the year, excluding vacations and sunscreen use, in the north (45°N; Fig. 4A) and south (35°N; Fig. 4B). Almost no one in the senior group can make the minimum amount of vitamin D3 (600–800 IU/day) all year so that they are not deficient. No senior can meet their vitamin D need all year from everyday exposures even with a 3-week vacation (see Fig. 5), unless they either work or stay outdoors for most of the day, to have sufficient blood levels of 25(OH)D (>50 nmol/L or >20 ng/ml).
Figure 4.
The average amount of vitamin D3 (IU/day) indoor-working adult men and women seniors (60+ yr) with skin types II–V make from everyday outdoor UV exposures each season in the (A) Northern (45°N) and (B) Southern (35°N) US. Note that senior's ≥70 yr might only make about half the amount shown in the figure.
Figure 5 shows the average amount of vitamin D3 indoor-working adults over 21 yr can make each day during the summer without and with a 1-, 2- or 3-week summer vacation. These vacation estimates include the use of the equivalent of SPF 4 sunscreen only during a beach vacation and are averages of four different types of vacations: beach, sightseeing, country and home.46 Only some skin type II Caucasians (22–40 yr) will meet their minimum vitamin D needs (∼600 IU/day) during the summer, and some can possibly meet their optimum vitamin D needs (≥1,200 IU/day) if they take a 2-week vacation. The older Caucasians (60+) and skin type III will need at least a 3-week vacation. However, no other indoor-working adult will meet their minimum vitamin D needs (600–800 IU/day), let alone their optimum needs (≥1,200 IU/day), all year even with a 3-week vacation at 40°N.
Discussion
According to current findings, people need ∼2,000 IU/day to maintain blood levels of 25(OH)D above 75 nmol/L or 30 ng/ml.52,53 Our calculations revealed that only some “outdoorsy” indoor-working Caucasians of skin type II (22–59 yr) may make optimal amounts of vitamin D3 (≥1,200 IU/day) during the summer, but only if they expose more than 30% of their body every day to sunlight, take a 2–3 week vacation at latitudes ≤40°N, and do not wear sunscreens except on beach vacations. The summer values shown in the figures are very optimistic because most adults work indoors (>90%) and, consequently, wear more clothing during their workweek, exposing only ∼10–15% of their body to UV. Thus, most indoor-working adults that wear professional clothing will actually make about half the values shown in the figures during the summer and will not meet their minimum vitamin D needs. As people age, their ability to make vitamin D3 from the same UV exposure decreases (Fig. 1) so that only the most active “outdoorsy” Caucasian adults over 60 yr can make the minimum amount of vitamin D (800 IU/day) they need during the summer to prevent deficiency (>50 nmol/L; Figs. 2–4). Caucasians over 60 yr with skin type II, and all other skin types over 21 yr do not meet their minimum vitamin D3 needs from everyday outdoor exposures all year and would need to be supplemented,54 except some people during the summer if they wear sporty clothing to work and also take a 2–3 week vacation (see Fig. 5).
Overall our findings agree with reports of vitamin D deficiency (<50 nmol/L; <20 ng/ml) and insufficiency (<75 nmol/L; <30 ng/ml) among adults in the US.36–41 Vitamin D deficiency and insufficiency increases with increasing latitude, age and skin color, so that almost all adult African Americans are deficient in vitamin D during and after winter and about half have insufficient levels during the summer. Unless an adult works outdoors for most of the day, especially the darker skin types, they cannot get enough UV exposure to make the minimum amount of vitamin D (∼600 IU/day) so that they are not deficient, and they cannot possibly make optimal amounts of vitamin D to be sufficient (≥1,200 IU/day) without supplementation unless they work outdoors (∼5% US population).
The average time indoor-working adults stay outdoors during the summer months in the US is 93.5 ± 2.5 min/day in the south at ∼35°N and 102.5 ± 5.5 min/day in the north at ∼45°N.46 If that increasing time trend from south-to-north continues during the summer, we would expect people living around 55°N to stay outdoors for about 111.5 ± 9 min/day or less than 2 hr/day. However, Thieden et al. (2009) found Danish workers at ∼56°N stay outdoors for almost 3 hr/day during the summer and have 25(OH)D blood levels ∼82 nmol/L, similar to outdoor workers.56 Their study mixed outdoor worker's (gardeners) times with indoor worker's times, which increased the overall time outdoors. In addition, they only measured the UV exposures and 25(OH)D blood levels of 25 people, but they failed to disclose how many of those people worked outdoors. In contrast, a very large European study (>12,000 people) found about 60% of the English workers at 52°N had blood levels of 25(OH)D below 75 nmol/L during the summer months.57 Their findings agree with our estimates that about half the “optimistic” (clothing) amount of vitamin D3 Caucasian Americans make at 40°N (≤800 IU/day) can be made at 52°N (≤400 IU/day) based on erythemally-weighted doses measured at the same latitude in the Netherlands.58 People at 52°N receive about half the annual erythemally-weighted UV dose that Americans get at ∼40°N, and consequently would make about half the amount of vitamin D3 Americans make during any season of the year.
The epidemiology results and our calculated amounts of vitamin D3/day produced by Americans (>21 yr) significantly differ from what the American Academy of Dermatology claims.42 They claim people can make “ample” vitamin D3 (≥1,000 IU/day) from “casual” sun exposure, even if they diligently wear SPF 15 sunscreen. However, they did not convert the erythemally-weighted UV doses to previtamin D3-weighted UV doses and they did not convert horizontal plane doses to full-cylinder or actual body doses; they also did not take age into account. In contrast to their claims, we find the majority of indoor-working adult Americans are not going outside enough all year to get adequate everyday sun exposure to make the minimum amounts of vitamin D3 (600–800 IU/day) they need. Only some “out-doorsy” indoor-working Caucasians can make optimal vitamin D3 (≥1,200 IU/day) during the summer and some other skin types if they wear sporty clothing to work, take a 2–3 week vacation at latitudes ≤40°N (see Fig. 5), and do not wear sunscreens except on beach vacations. The only other people who can make enough vitamin D are some of the outdoor-working adult Americans (∼5% of the population). The most serious situation occurs with seniors (60+ yr) who cannot even make the minimum amount of vitamin D3 (600–800 IU/day) all year even with a 3-week vacation. Furthermore, if anyone wears sunscreens with SPF ≥15, they will make virtually no vitamin D3 (see in ref. 44).
We also find that almost all indoor-working adult Americans are not getting adequate everyday UV exposures all year to make optimal amounts of vitamin D3 (≥1,200 IU/day).53,59–61 Some people with skin type II and some men with skin types III and IV can make the optimal amounts of vitamin D3 during the summer if they also take a 2–3 wk vacation (Fig. 5). However, if they wear sunscreen of SPF ≥15, they will make virtually no vitamin D3 all year including during the summer (see in ref. 44). Thus, as found in the NHANES III study, Caucasian adult Americans with Fitzpatrick skin type II, and especially the darker skin types III, IV and V/VI, are not getting adequate everyday UV exposures for most of the year to make the minimum amounts of vitamin D3 to prevent deficiency. The situation would be much worse if they diligently wore sunscreens with SPF ≥15. The African-Americans have a similar situation from melanin protection, which may explain the disparity in health found between whites and blacks.62 Furthermore, neither diet nor supplements correct this situation.63–65 In fact, 83% of Australian dermatologists, who advise people to take vitamin D supplements rather than get more UV exposure, have insufficient blood levels of 25(OH) D.66 Because the UV doses of indoor-working people around the world are similar to ours at similar latitudes (25–50°N),58 vitamin D deficiency (<50 nmol/L or 20 ng/ml) and insufficiency (<75 nmol/L or 30 ng/ml) is also found around the world, especially at higher latitudes (>50°N) and in countries that do not fortify foods.63 As a result, vitamin D deficiency is a worldwide problem with serious health consequences,67 which occurs from too little sun exposure.
However, too much sun exposure can result in skin cancer, which is also a potentially serious health consequence. Paradoxically, while intermittent UVB sunburns increases indoor workers incidence of melanoma, regular, moderate UVB exposures keeps outdoor workers incidence of melanoma at the same level68,69 although they get 3–10 times more UV exposure as indoor workers get.58 Furthermore, regular moderate outdoor UV exposures increase the survival of melanoma patients.20 Thus, complete avoidance of or protection from all peak hour (10 A.M.–4 P.M.) UVB exposures and the diligent use of SPF ≥15 sunscreens may not only increase the incidence of a variety of adult diseases and the mortality from some internal cancers, but may also paradoxically be increasing the incidence of and mortality from melanoma.28 However, fair-skinned people who are prone to burning should wear sunscreens during beach vacations or if they are outside for a while in the strong midday summer sun (11 A.M.–3 P.M.) to prevent sunburn and the initiation of melanoma. Because the overall population probably should not increase their UV exposure and consequently their risk of getting skin cancers, and because most people do not take supplements on a regular basis, the best approach for maintaining healthy blood levels of 25(OH)D may be to supplement foods and drinks.
Materials and Methods
We give the details of these calculations in Godar et al.44 so that only the changes needed for the adult calculations are included below. We obtained the outdoor solar doses every season of the year for indoor-working adults (∼95% population) from reference 46.
The equation for calculating the amount of vitamin D3 produced by people from an average daily, erythemally-weighted UV exposure during each season of the year is: Vitamin D3 (IU)/day = VDD × (4,861 IU/SED for skin type II) × STF × FBE × AF. Where VDD is the “Vitamin D Dose” or the person's standard erythemally-weighted, average seasonal solar UV dose in SED/day at either 45°N or 35°N multiplied by its corresponding ASCF48 to convert it to a standard vitamin D3 dose (SVD), and then multiplied by its corresponding GCF.49 The later step converts it from a horizontal plane dose to a person's body dose. The ASCF for each season in the northern (45°N) and Southern (35°N) US are 1.034 and 1.104 for summer, 0.879 and 1.029 for fall, 0.565 and 0.842 for winter, and 0.9 and 1.049 for spring, respectively.48 The GCF conversion factors in the northern (45°N) US are 0.434 for clear skies during the summer and spring, and 0.508 for clear skies during the winter and fall. The GCF conversion factors in the Southern (35°N) US are 0.417 for clear skies during the summer and spring and 0.484 for clear skies during the winter and fall.49 Note here that although the typical effect of cloud cover is a slight increase (<3%) in the average GCF, it can reduce UVB radiation drastically (up to ∼50%).58 FBE is the fraction body exposed (described below), and AF is the age factor (described below and see Fig. 1).
The amount of vitamin D3 adults make from outdoor UV exposures will depend on how much skin they expose to the sun while they are outside or their Fraction Body Exposed (FBE), so that one needs to multiply the FBE by the amount made from a whole body exposure (4,861 IU/SED).44 We get the best estimates of how much body area adult Americans expose during each season of the year using the “rule of nines,” originally developed to estimate burn areas.70 To make these estimates, we assumed most adults would expose their face (3.5%), the front half of their neck (1%) and the front and back of both their hands (5%) during all seasons of the year, including winter (FBE is 9.5%; long-sleeved shirts/blouses and long pants/skirts). In addition to those body areas, we assumed most adults would also expose their lower arms (6%) during the spring and fall (FBE is 15.5%). In addition to those body areas, we assumed most adults would also expose half of their upper arms (4%; short-sleeved shirts or tee shirts) and all of their lower legs (14%; knee-length shorts/skirts) during the entire summer (FBE is 33.5%). However, adults have to work during the summer, so that they tend to expose only about 9.5–15.5% of their body (face, neck, hands and sometimes their lower arms) during their workweek. Thus, the amounts made during the summer are closer to half the values shown in the figures. For the children and adult body percentages exposed during each season see Table 1 of reference 44. The FBE is the percent body area exposed divided by 100%.
The final part of the calculation involves the ability of an adult to make vitamin D3 with age because it decreases with increasing age due to epidermal thinning.51 Because children (<22 yr) have the highest ability to make vitamin D3, they have an age factor (AF) of unity compared to older adults; all other values are relative to theirs (Fig. 1): 0–20 yr (100% or 1.0), 22–40 yr (83% or 0.83), 41–59 yr (66% or 0.66) and 60+ yr (49% or 0.49). Note that adults over 70 yr can make as little as 25% of what children can make,67 so that our calculations are on the “optimistic” side for the eldest adults (60+ yr).
One can do the sunscreen calculations by simply dividing the amount of vitamin D3 made without sunscreen (equation above) by the SPF factor.71 These numbers only apply to people who diligently wear sunscreens correctly, i.e., they generously apply them prior to going outdoors, covering their entire body and they reapply them every 2 hours.
To convert IU of vitamin D to ng/ml blood levels of 25(OH) D multiply by 0.01,60 and to convert 25-(OH)D ng/ml to 25(OH) D nmol/L multiply by 2.599,71 or multiply IU of vitamin D by 0.0385 to get 25-(OH)D nmol/L directly.
Basically, 100 IU of ingested vitamin D3 raises blood levels of 25(OH)D by 0.6–1 ng/ml.52,53
Abbreviations
- AF
age factor
- ASCF
action spectrum conversion factors
- FBE
fraction body exposure
- GCF
geometric conversion factors
- 25(OH)D
25-hydroxyvitamin D
- 1,25(OH)2D
1,25-dihydroxyvitamin D
- IU
international units
- MED
minimum erythemal dose
- SED
standard erythemal dose
- SPF
sun protection factor
- STF
skin type factor
- SVD
standard vitamin D dose
- US
United States
- UVB
290–315 nm
- UVR
290–400 nm
- VDD
vitamin D3 dose
Disclosure of Potential Conflicts of Interest
D.E.G. and S.J.P. have nothing to disclose. W.B.G. gets funding from the UV foundation (McLean, VA), the Sunlight Research Forum (Veldhoven), Bio-Tech-Pharmacal (Fayetteville, AR), the Vitamin D Council (San Luis Obispo, CA), and the Danish Sunbed Federation. M.F.H. gets funding from the UV Foundation (McClean, VA).
References
- 1.Holick MF, MacLaughlin JA, Clark MB, Holick SA, Potts JT, Jr, Anderson RR, et al. Photosynthesis of pre-vitamin D3 in human skin and the physiological consequences. Science. 1980;210:203–205. doi: 10.1126/science.6251551. [DOI] [PubMed] [Google Scholar]
- 2.MacLaughlin JA, Anderson RR, Holick MF. Spectral character of sunlight modulates photosynthesis of previtamin D3 and its photoisomers in human skin. Science. 1982;216:1001–1003. doi: 10.1126/science.6281884. [DOI] [PubMed] [Google Scholar]
- 3.Krause R, Buhring M, Hopfenmuller W, Holick MF, Sharma AM. Ultraviolet B and blood pressure. Lancet. 1998;352:709–710. doi: 10.1016/S0140-6736(05)60827-6. [DOI] [PubMed] [Google Scholar]
- 4.Pfeifer M, Begerow B, Minne HW. Vitamin D and muscle function. Osteoporos Int. 2002;13:187–194. doi: 10.1007/s001980200012. [DOI] [PubMed] [Google Scholar]
- 5.Parker J, Hashmi O, Dutton D, Mavrodaris A, Stranges S, Kandala NB, et al. Levels of vitamin D and cardiometabolic disorders: systematic review and metaanalysis. Maturitas. 2009;65:225–236. doi: 10.1016/j.maturitas.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 6.Wang L, Manson JE, Song Y, Sesso HD. Systematic review: Vitamin D and calcium supplementation in prevention of cardiovascular events. Ann Intern Med. 2010;152:3153–3163. doi: 10.7326/0003-4819-152-5-201003020-00010. [DOI] [PubMed] [Google Scholar]
- 7.Weishaar RE, Simpson RU. Involvement of vitamin D with cardiovascular function. II. Direct and indirect effects. Am J Physiol. 1987;253:675–683. doi: 10.1152/ajpendo.1987.253.6.E675. [DOI] [PubMed] [Google Scholar]
- 8.Zitterman A, Schleithoff SS, Koerfer R. Putting cardiovascular disease and vitamin D insufficiency into perspective. Br J Nutr. 2005;94:483–492. doi: 10.1079/bjn20051544. [DOI] [PubMed] [Google Scholar]
- 9.Chiu KC, Chu A, Go VL, Saad MF. Hypovitaminosis D is associated with insulin resistance and beta cell dysfunction. Am J Clin Nutr. 2004;79:820–825. doi: 10.1093/ajcn/79.5.820. [DOI] [PubMed] [Google Scholar]
- 10.Lindqvist PG, Olsson H, Landin-Olsson M. Are active sun exposure habits related to lowering risk of type 2 diabetes mellitus in women, a prospective cohort study? Diabetes Res Clin Pract. 2010;90:109–114. doi: 10.1016/j.diabres.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 11.Merlino LA, Curtis J, Mikuls TR, Cerhan JR, Criswell LA, Saag KG. Vitamin D intake is inversely associated with rheumatoid arthritis. Arthritis Rheum. 2004;50:723–777. doi: 10.1002/art.11434. [DOI] [PubMed] [Google Scholar]
- 12.Pelajo CF, Lopez-Benitez JM, Laurie C, Miller LC. Vitamin D and Autoimmune Rheumatologic Disorders. Autoimmunity Reviews. 2010;9:507–510. doi: 10.1016/j.autrev.2010.02.011. [DOI] [PubMed] [Google Scholar]
- 13.Krall EA, Wehler C, Garcia RI, Harris SS, Dawson-Hughes B. Calcium and vitamin D supplements reduce tooth loss in the elderly. Am J Med. 2001;111:452–456. doi: 10.1016/s0002-9343(01)00899-3. [DOI] [PubMed] [Google Scholar]
- 14.Bischoff HA, Stahelin HN, Dick W, Akos R, Knecht M, Salis C, et al. Effects of vitamin D and calcium supplementation on falls: a randomized trial. J Bone Min Res. 2003;18:343–351. doi: 10.1359/jbmr.2003.18.2.343. [DOI] [PubMed] [Google Scholar]
- 15.Broe KE, Chen TC, Weinberg J, Bischoff-Ferrari HA, Holick MF, Kiel DP. A higher dose of vitamin D reduces the risk of falls in nursing home residents: a randomized, multiple-dose study. J Am Geriatr Soc. 2007;55:234–239. doi: 10.1111/j.1532-5415.2007.01048.x. [DOI] [PubMed] [Google Scholar]
- 16.Lips P, Graafmanns WC, Ooms ME, Bezemer PD, Bouter LM. Vitamin D supplementation and fracture incidence in elderly persons. A randomized trial. Ann Int Med. 1996;15:400–406. doi: 10.7326/0003-4819-124-4-199602150-00003. [DOI] [PubMed] [Google Scholar]
- 17.Holick MF. Vitamin D deficiency. N Engl J Med. 2004;357:266–281. doi: 10.1056/NEJMra070553. 2007. [DOI] [PubMed] [Google Scholar]
- 18.Reichrath J, Rech M, Moeini M, Meese E, Tilgen W, Seifert M. In vitro comparison of the vitamin D endocrine system in 1,25(OH)2D3-responsive and -resistant melanoma cells. Cancer Biol Ther. 2007;6:48–55. doi: 10.4161/cbt.6.1.3493. [DOI] [PubMed] [Google Scholar]
- 19.Lappe JM, Travers-Gustafson D, Davies KM, Recker RR, Heaney RP. Vitamin D and calcium supplementation reduces cancer risk: results of a randomized trial. Am J Clin Nutr. 2007;85:1586–1591. doi: 10.1093/ajcn/85.6.1586. [DOI] [PubMed] [Google Scholar]
- 20.Berwick M, Armstrong BK, Ben-Porat L, Fine J, Kricker A, Eberle C, Barnhill R. Sun exposure and mortality from melanoma. JNCI. 2005;97:195–199. doi: 10.1093/jnci/dji019. [DOI] [PubMed] [Google Scholar]
- 21.Berwick M, Kesler D. Ultraviolet radiation exposure, vitamin D and cancer. Photochem Photobiol. 2005;81:1261–1266. doi: 10.1562/2005-02-18-IR-445. [DOI] [PubMed] [Google Scholar]
- 22.Freedman DM, Dosemeci M, McGlynn K. Sunlight and mortality from breast, ovarian, colon, prostate and non-melanoma skin cancer: a composite death certificate based case-control study. Occup Environ Med. 2002;59:257–262. doi: 10.1136/oem.59.4.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Garland CF, Comstock GW, Garland FC, Helsing KJ, Shaw EK, Gorham ED. Serum 25-hydroxyvitamin D and colon cancer: eight-year prospective study. Lancet. 1989;2:1176–1178. doi: 10.1016/s0140-6736(89)91789-3. [DOI] [PubMed] [Google Scholar]
- 24.Millen AE, Tucker MA, Hartge P, Halpern A, Elder DE, Guerry D, 4th, et al. Diet and melanoma in a case-control study. Cancer Epidemiol Biomarkers Prev. 2004;13:1042–1051. [PubMed] [Google Scholar]
- 25.Moon SJ, Fryer AA, Strange RC. Ultraviolet radiation: effects on risks of prostate cancer and other internal cancers. Mut Res. 2005;571:207–219. doi: 10.1016/j.mrfmmm.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 26.Yin L, Grandi N, Raum E, Haug U, Arndt V, Brenner H. Meta-analysis: serum vitamin D and breast cancer risk. Eur J Cancer. 2010;46:2196–2205. doi: 10.1016/j.ejca.2010.03.037. [DOI] [PubMed] [Google Scholar]
- 27.Tangpricha V, Colon NA, Kaul H, Wang SL, Decastro, Blanchard RA, et al. Prevalence of vitamin D deficiency in patients attending an outpatient cancer care clinic in Boston. Endocr Pract. 2004;10:292–293. doi: 10.4158/EP.10.3.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Godar DE, Landry R, Lucas AD. Increased UVA exposures and decreased cutaneous Vitamin D3 levels may be responsible for the increasing incidence of melanoma. Med Hypotheses. 2009;72:434–443. doi: 10.1016/j.mehy.2008.09.056. [DOI] [PubMed] [Google Scholar]
- 29.Danielsson C, Fehsel K, Polly P, Carlberg C. Differential apoptotic response of human melanoma cells to 1α, 25-dihydroxyvitamin D3 and its analogues. Cell Death Different. 1998;5:946–951. doi: 10.1038/sj.cdd.4400437. [DOI] [PubMed] [Google Scholar]
- 30.Eisman JA, Barkla DH, Tutton PJ. Suppression of in vivo growth of human cancer solid tumor xenografts by 1,25-dihydroxyvitamin D3. Cancer Res. 1987;47:21–25. [PubMed] [Google Scholar]
- 31.Reichrath J, Rech M, Moeini M, Meese E, Tilgen W, Seifert M. In vitro comparison of the vitamin D endocrine system in 1,25(OH)2D3-responsive and -resistant melanoma cells. Cancer Biol Ther. 2007;6:48–55. doi: 10.4161/cbt.6.1.3493. [DOI] [PubMed] [Google Scholar]
- 32.Grant WB. An estimate of premature cancer mortality in the US due to inadequate doses of solar ultraviolet-B radiation. Cancer. 2002;94:1867–1875. doi: 10.1002/cncr.10427. [DOI] [PubMed] [Google Scholar]
- 33.Grant WB. In defense of the sun: An estimate of changes in mortality rates in the United States if mean serum 25-hydroxyvitamin D levels were raised to 45 ng/mL by solar ultraviolet-B irradiance. Dermato-Endocrinol. 2009;1:207–214. doi: 10.4161/derm.1.4.9841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Glerup H, Mikkelsen K, Poulsen L, Has E, Overbeck S, Thomsen J, et al. Commonly recommended daily intake of vitamin D is not sufficient if sunlight exposure is limited. J Intern Med. 2000;247:260–268. doi: 10.1046/j.1365-2796.2000.00595.x. [DOI] [PubMed] [Google Scholar]
- 35. Web sites: http://www.aad.org/00PSA1.html; http://www.skincancer.org/skincancer-facts.php; http://www.cancer.org; http://acpm.org; http://www.skincancer.org; http://www.cdc.gov/cancer/nscpep/skin.htm; http://cancernet.nci.nih.gov/wyntk_pubs/skin.htm; http://www.umm.edu/skincancer/causes.htm; http://www.lustra.net/cgi-bin/multiple_choice.cgi; http://www.epa.gov/sunwise/kids.html.
- 36.Ginde AA, Liu MC, Camargo CA., Jr Demographic differences and trends of vitamin D insufficiency in the US population 1988–2004. Arch Intern Med. 2009;169:626–632. doi: 10.1001/archinternmed.2008.604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Looker AC, Dawson-Hughes B, Calvo MS, Gunter EW, Sahyoun NR. Serum 25-hydroxyvitamin D status of adolescents and adults in two seasonal subpopulations from NHANES III. Bone. 2002;30:771–777. doi: 10.1016/s8756-3282(02)00692-0. [DOI] [PubMed] [Google Scholar]
- 38.Looker AC, Pfeiffer CM, Lacher DA, Schleicher RL, Picciano MF, Yetley EA. Serum 25-hydroxyvitamin D status of the US population: 1988–1994 compared with 2000–2004. Am J Clin Nutr. 2008;88:1519–1527. doi: 10.3945/ajcn.2008.26182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nesby-O'Dell S, Scanlon KS, Cogswell ME, Gillespie C, Hollis BW, Looker AC, et al. Hypovitaminosis D prevalence and determinants among African American and white females of reproductive age: third National Health and Nutrition Examination Survey 1988–1994. Am J Clin Nutr. 2002;76:187–192. doi: 10.1093/ajcn/76.1.187. [DOI] [PubMed] [Google Scholar]
- 40.Stryd RP, Gilbertson TJ, Brunden MN. A seasonal variation of 25-hydroxyvitamin D3 serum levels in normal humans. J Clin Endocrinol Metabol. 1979;48:771–775. doi: 10.1210/jcem-48-5-771. [DOI] [PubMed] [Google Scholar]
- 41.Tangpricha V, Pearce EN, Chen TC, Holick MF. Vitamin D insufficiency among free-living healthy young adults. Am J Med. 2002;112:659–662. doi: 10.1016/s0002-9343(02)01091-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lim HW, Gilchrest BA, Cooper KD, Bischoff-Ferrari HA, Rigel DR, Cyr WH, et al. Sunlight, tanning booths and vitamin D. J Am Acad Dermatol. 2005;52:868–876. doi: 10.1016/j.jaad.2005.03.015. [DOI] [PubMed] [Google Scholar]
- 43.Godar DE. UV Doses of American Children and Adolescents. Photochem Photobiol. 2001;74:787–793. doi: 10.1562/0031-8655(2001)074<0787:UDOACA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 44.Godar DE, Pope SJ, Grant WB, Holick MF. Solar UV Doses of Young Americans and Vitamin D3 Production. Environmental Health Perspectives. doi: 10.1289/ehp.1003195. Submitted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Clemens TL, Adams JS, Henderson SL, Holick MF. Increased skin pigment reduces the capacity to synthesize vitamin D3. Lancet. 1982;1:74–76. doi: 10.1016/s0140-6736(82)90214-8. [DOI] [PubMed] [Google Scholar]
- 46.Godar DE, Wengraitis SP, Shreffler J, Sliney DH. UV doses of Americans. Photochem Photobiol. 2001;73:621–629. doi: 10.1562/0031-8655(2001)073<0621:udoa>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 47.Klepeis NE, Nelson WC, Ott WR, Robinson JP, Tsang AM, Switzer P, et al. The National Human Activity Pattern Survey (NHAPS): a resource for assessing exposure to environmental pollutants. J Expo Anal Environ Epidemiol. 2001;11:231–252. doi: 10.1038/sj.jea.7500165. [DOI] [PubMed] [Google Scholar]
- 48.Pope SJ, Holick MF, Mackin S, Godar DE. Action spectrum conversion factors that change erythemally weighted to previtamin D3-weighted UV doses. Photochem Photobiol. 2008;84:1277–1283. doi: 10.1111/j.1751-1097.2008.00373.x. [DOI] [PubMed] [Google Scholar]
- 49.Pope SJ, Godar DE. Solar UV geometric conversion factors: horizontal plane to cylinder model. Solar UV geometric conversion factors: horizontal plane to cylinder model. Photochem Photobiol. 2010;86:457–466. doi: 10.1111/j.1751-1097.2009.00679.x. [DOI] [PubMed] [Google Scholar]
- 50.Fitzpatrick TB. The validity and practicality of Sunreactive skin types I through VI. Arch Dermatol. 1988;124:869–871. doi: 10.1001/archderm.124.6.869. [DOI] [PubMed] [Google Scholar]
- 51.MacLaughlin JA, Holick MF. Aging decreases the capacity of human skin to make vitamin D3. J Clin Invest. 1985;76:1536–1538. doi: 10.1172/JCI112134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Heaney RP, Davies KM, Chen TC, Holick MF, Barger-Lux MJ. Human serum 25-hydroxycholecalciferol response to extended oral dosing with cholecalciferol. Am J Clin Nutr. 2003;77:204–210. doi: 10.1093/ajcn/77.1.204. [DOI] [PubMed] [Google Scholar]
- 53.Holick MF, Biancuzzo RM, Chen TC, Klein EK, Young A, Bibuld D, et al. Vitamin D2 is as effective as vitamin D3 in maintaining circulating concentrations of 25-hydroxyvitamin D. J Clin Endocrinol Metab. 2008;93:677–681. doi: 10.1210/jc.2007-2308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Norman AW, Bouillon R. Vitamin D nutritional policy needs a vision for the future. Exp Biol Med. 2010;235:1034–1045. doi: 10.1258/ebm.2010.010014. [DOI] [PubMed] [Google Scholar]
- 55.Thieden E, Philipsen PA, Heydenreich J, Wulf HC. Vitamin D level in summer and winter related to measured UVR exposure and behavior. Photochem Photobiol. 2009;85:1480–1484. doi: 10.1111/j.1751-1097.2009.00612.x. [DOI] [PubMed] [Google Scholar]
- 56.Devgun MS, Paterson CR, Johnson BE, Cohen C. Vitamin D nutrition in relation to season and occupation. Am J Clin Nutr. 1981;34:1501–1504. doi: 10.1093/ajcn/34.8.1501. [DOI] [PubMed] [Google Scholar]
- 57.Hyppönen E, Power C. Hypovitaminosis D in British adults at age 45 y: nationwide cohort study of dietary and lifestyle predictors. Am J Clin Nutr. 2007;85:860–868. doi: 10.1093/ajcn/85.3.860. [DOI] [PubMed] [Google Scholar]
- 58.Godar DE. UV Doses Worldwide. Photochem Photobiol. 2005;81:736–749. doi: 10.1562/2004-09-07-ir-308r.1. [DOI] [PubMed] [Google Scholar]
- 59.Grant WB, Holick MF. Benefits and requirements of vitamin D for optimal health: a review. Altern Med Rev. 2005;10:94–111. [PubMed] [Google Scholar]
- 60.Maalouf J, Nabulsi M, Vieth R, Kimball S, El-Rassi R, Mahfoud Z, et al. Short- and long-term safety of weekly high-dose vitamin D3 supplementation in school children. J Clin Endocrinol Metab. 2008;93:2693–2701. doi: 10.1210/jc.2007-2530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Weaver CM, Fleet JC. Vitamin D requirements: current and future. Am J Clin Nutr. 2004;80:1735–1739. doi: 10.1093/ajcn/80.6.1735S. [DOI] [PubMed] [Google Scholar]
- 62.Bibuld D. Health disparities and vitamin D. Clinic Rev Bone Miner Metab. 2009;7:63–76. [Google Scholar]
- 63.Calvo MS, Whiting SJ, Barton CN. Vitamin D intake: a global perspective of current status. J Nutr. 2005;135:310–316. doi: 10.1093/jn/135.2.310. [DOI] [PubMed] [Google Scholar]
- 64.Moore CE, Murphy MM, Keast DR, Holick MF. Vitamin D intake in the United States. J Am Diet Assoc. 2004;104:980–983. doi: 10.1016/j.jada.2004.03.028. [DOI] [PubMed] [Google Scholar]
- 65.Moore CE, Murphy MM, Holick MF. Vitamin D intakes by children and adults in the United States differ among ethnic groups. J Nutr. 2005;135:2478–2485. doi: 10.1093/jn/135.10.2478. [DOI] [PubMed] [Google Scholar]
- 66.Czarnecki D, Meehan CJ, Bruce F. The vitamin D status of Australian dermatologists. Clin Exp Dermatol. 2009;34:624–625. doi: 10.1111/j.1365-2230.2008.03002.x. [DOI] [PubMed] [Google Scholar]
- 67.Holick MF, Chen TC. Vitamin D deficiency: a worldwide problem with health consequences. Am J Clin Nutr. 2008;87:1080–1086. doi: 10.1093/ajcn/87.4.1080S. [DOI] [PubMed] [Google Scholar]
- 68.Chang YM, Barrett JH, Bishop DT, Armstrong BK, Bataille V, Bergman W, et al. Sun exposure and melanoma risk at different latitudes: a pooled analysis of 5,700 cases and 7,216 controls. Int J Epidemiol. 2009;38:814–830. doi: 10.1093/ije/dyp166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gandini S, Sera F, Cattaruza MS, Pasquini P, Picconi O, Boyle P, Melchi CF. Meta-analysis of risk factors for cutaneous melanoma: II. Sun exposure. Eur J Cancer. 2005;41:45–60. doi: 10.1016/j.ejca.2004.10.016. [DOI] [PubMed] [Google Scholar]
- 70.Lund CC, Browder NC. The estimation of areas of burns. Surgery Gynecol Obstetrics. 1944;79:352–358. [Google Scholar]
- 71.Matsuoka LY, Wortsman J, Hanifan N, Holick MF. Chronic sunscreen use decreases circulating concentrations of 25-hydroxyvitamin D. A preliminary study. Arch Dermatol. 1988;124:1802–1804. [PubMed] [Google Scholar]