Abstract
A number of risk indices have been formulated in an attempt to predict risk of a major hemorrhage in an individual on warfarin therapy. No single index to date is able to reliably predict this risk in an individual patient. Although most warfarin related hemorrhages are gastrointestinal or intracranial in origin this case represents a particularly rare entity of a major hemorrhage presenting as an encysted empyema. To the best of our knowledge this has never before been described.
Keywords: empyema, hematology, lung, thoracotomy.
Introduction
An 83 year old gentleman presented to the emergency department of a local hospital with a history of hemoptysis – two weeks duration – fatigue, loss of weight, shortness of breath and high grade fever. The patient, although taking warfarin for atrial fibrillation, discontinued this once hemopotysis was noted, with no effect. Further medical history of note included a history of hypertension on treatment, mild mitral regurgitation and previous right hemicolectomy for caecal carcinoma. Sputum sent for microscopy, culture and sensitivity by the general practitioner, four days prior to admission to a local Hospital, grew Klebsiella pneumoniae and Moraxella catarrhalis. In the light of the patient’s condition, the general practitioner trialed the patient on a course of Amoxicillin/Clavulanic acid and roxithromycin, based on the sensitivity report but with minimal effect.
On presentation, mild dyspnoea with movement was noted, peripheries were warm and well perfused with an elevated blood pressure and an irregularly irregular pulse rate below 100 beats per minute was observed. Breath sounds were diminished in the right lower zone with coarse inspiratory crepitations and increased tactile fremitus in the right posterior zones. The patient’s INR (international normalized ratio) on admission was 1.9.
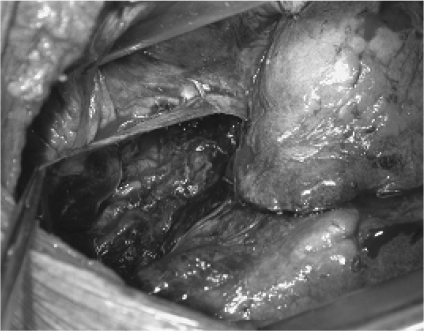
Chest x-ray done on admission revealed consolidation of the right middle and lower lobes with an air fluid level in the right mid zone, and blunting of the right hemidiaphragm (Fig 1). Findings were suspicious of empyema and it was decided to obtain computerized tomography (CT) of the thorax.
Fig 1. Chest radiograph showing consolidation of the right middle and lower lobes and air fluid level in the right midzone.
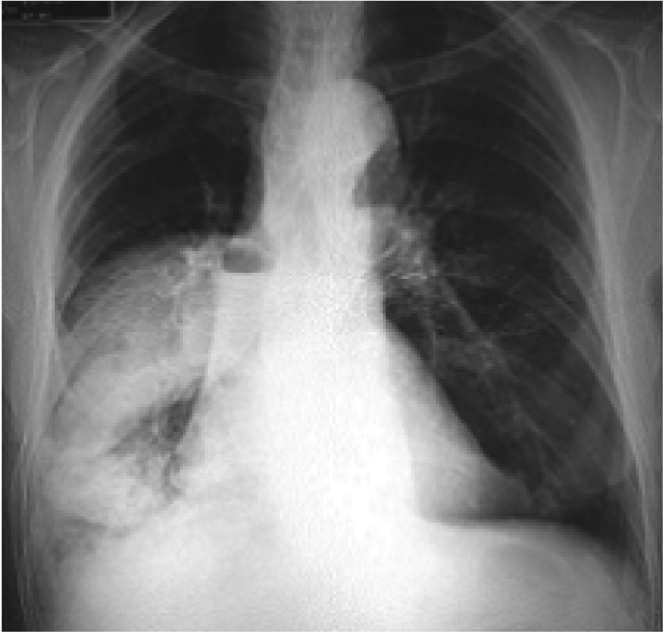
CT confirmed consolidation in the lateral and posterior basal segments of the right lower lobe and right middle lobe. A rounded opacity projected over the right mid-zone, lentiform in shape and compatible with being pleural in origin. An air fluid level at its medial aspect was typical of gas in the pleural space (Fig 2). These findings were suggestive of pneumonia complicated by empyema. The patient was started on intravenous Cefuroxime and transfer to the Department Cardiothoracic Surgery, Wellington was organized for further management.
Fig 2. Computerized tomography showing rounded opacity over the right mid-zone, pleural in origin.
Rigid bronchoscopy together with right posterolateral thoracotomy were undertaken at Wellington Public hospital. Rigid bronchoscopy revealed an ulcer in the right main bronchus near the carina, most likely the cause of the hemoptysis. Bronchoscopic lavage was performed on this lesion and a specimen sent for cytology (no malignant cells noted).
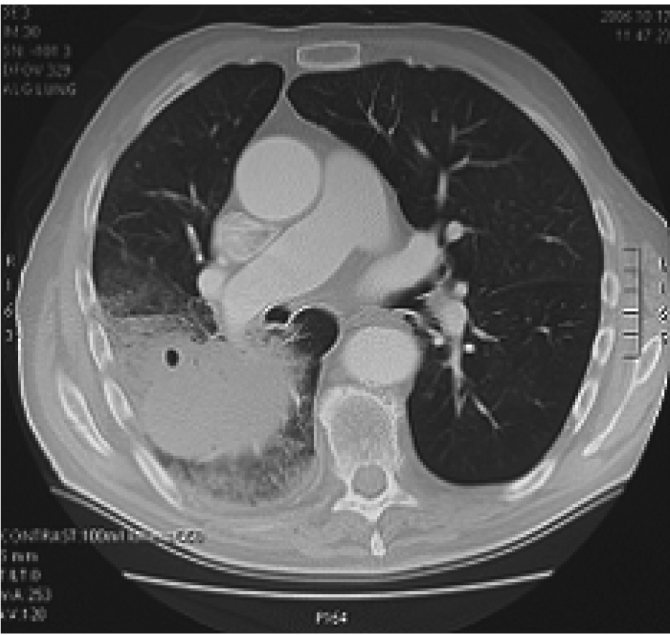
Right thoracotomy revealed a large hematoma in the fissure between the middle and lower lobes, contained beneath the visceral pleura of the lower lobe (Fig 3). Extension of ecchymosis was noted all over the surface of the lower lobe. However, no further collections were seen anywhere else on the lower lobe. A smaller collection was also noted on the inferior surface of the right middle lobe.
Fig 3. Right middle and lower lobes exposed by posterlateral thoracotomy, revealing encysted collection and ecchymosis.

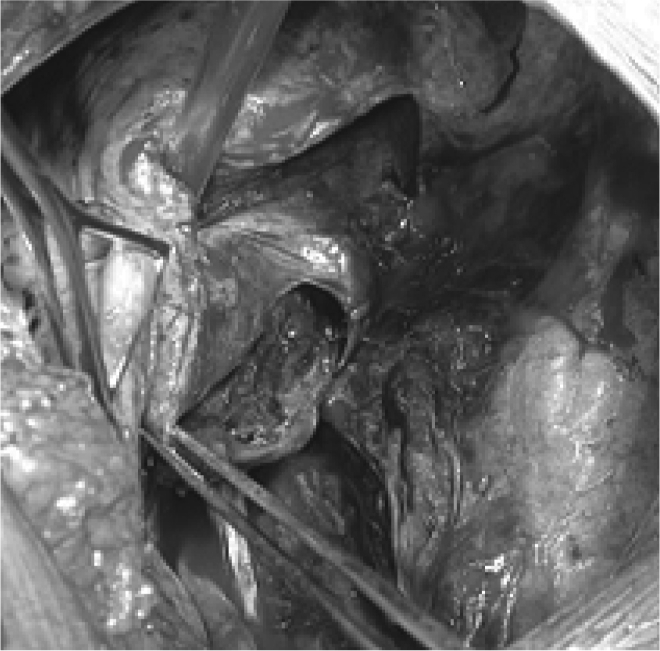
Both collections were evacuated completely and no further ongoing bleeding recorded (Fig 4, Fig 5). The visceral pleura of the lower lobe were left open whereas air leaks on the middle lobe were sutured. Basal and apical drains were inserted and the chest was closed in layers. The patient was extubated and transferred to the recovery room.
Fig 4. Evacuated right lower lobe collection and visceral pleura open.
Fig 5. Evacuated right middle lobe collection with visceral pleura open.
The haematoma was cultured. However, there was no growth after 72 hours of incubation.
Post-operative recovery was unremarkable. The intercostal drains were removed on third post-operative day and the patient was discharged the day after. At the time of discharge, he was afebrile, his white cell count had returned to normal limits and the surgical wounds were healing well with no signs of infection/inflammation. Considering the fact that the patient was old and the episode of haemoptysis and intra-thoracic haematoma, the warfarin therapy was discontinued and he was started on regular aspirin. Follow up was arranged with the referring physicians.
He was followed up six months after discharge at the local hospital. A chest X-ray done then showed complete resolution of his condition, according to the report.
Discussion
This case represents a unique presentation of warfarin associated hemorrhage, to the best of our knowledge never having been described before. Nonetheless it should be borne in mind as part of the differential diagnosis when evaluating a patient with empyema on anticoagulation.
Although serial INR monitoring will detect a number of patients who are over anticoagulated before they have a significant bleed, serial INR is not entirely protective against major bleeding while on warfarin therapy (1). There would appear to be only a brief warning period of slightly elevated INR indicating an increased risk of haemorrhage (1). Although, an INR > 6.0 has been shown to have significant short term risk for major haemorrhage (1), (2).
Prediction of major bleeding in individual patients has proven difficult and factors including extent of anticoagulation and individual risk factors for major bleeding need to be taken into consideration (4),(5),(6). Despite various indices having been formulated in an attempt to quantify this risk, no single index has proved entirely effective in individual patients.
The annual incidence of warfarin administration related fatality has often been reported at approximately 1%. One study suggests that this may be overestimated owing to the advances made in monitoring over the last 10-15 years (3).
Age would appear to be the main factor affecting risk of bleeding, specifically advanced age over 75 years (3). Factors including increased sensitivity to the effect of anticoagulation, concomitant usage of drugs that increase bleeding risk and associated co-morbidity which decreases compliance are generally cited as possible causes for this.
Conclusion
This case highlights one of the differential diagnoses in a patient on oral anticoagulants (e.g. warfarin) presenting with pleural effusion.
References
- 1.Kucher N, Connolly S, Beckman JA, Cheng LH, Tsilimingras KV, Fanikos J, et al. International normalized ratio increase before warfarin-associated hemorrhage: brief and subtle. Arch Intern Med. 2004;164:2176–9. doi: 10.1001/archinte.164.19.2176. [DOI] [PubMed] [Google Scholar]
- 2.Hylek EM, Chang YC, Skates SJ, Hughes RA, Singer DE. Prospective study of the outcomes of ambulatory patients with excessive warfarin anticoagulation. Arch Intern Med. 2000;160:1612–7. doi: 10.1001/archinte.160.11.1612. [DOI] [PubMed] [Google Scholar]
- 3.Fitzmaurice David A, Blann Andrew D, Lip Gregory Y H. ABC of antithrombotic therapy. Bleeding risks of antithrombotic therapy. BMJ. 2002;325:828–31. doi: 10.1136/bmj.325.7368.828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beyth RJ, Quinn LM, Landefeld CS. Prospective evaluation of an index for predicting the risk of major bleeding in outpatients treated with warfarin. Am J Med. 1998;105:91–9. doi: 10.1016/s0002-9343(98)00198-3. [DOI] [PubMed] [Google Scholar]
- 5.Kuijer PM, Hutten BA, Prins MH, Büller HR. Prediction of the risk of bleeding during anticoagulant treatment for venous thromboembolism. Arch Intern Med. 1999;159:457–60. doi: 10.1001/archinte.159.5.457. [DOI] [PubMed] [Google Scholar]
- 6.Wells PS, Forgie MA, Simms M, Greene A, Touchie D, Lewis G, et al. The outpatient bleeding risk index: validation of a tool for predicting bleeding rates in patients treated for deep venous thrombosis and pulmonary embolism. Arch Intern Med. 2003;163:917–20. doi: 10.1001/archinte.163.8.917. [DOI] [PubMed] [Google Scholar]