Abstract
There has been increasing concern regarding the role of prescription drug use in the causation of traffic crashes. The goal of this research is to describe the prevalence of prescription drug use among injured trauma patients and determine the association between classes of drugs and crash culpability, a surrogate measure of crash risk.
Methods:
Patient records, including chronic medication usage, for all drivers admitted to a trauma center following a traffic collision in 2008 (N=1,558) were linked with police crash reports to determine crash culpability. Multivariable analyses explored the association between medication use and crash culpability among non-drinking drivers. Adjusted odds ratios and 95% confidence intervals were compared among drivers who were and were not using central nervous system (CNS)-acting medications (single and multiple).
Results:
61.5% of all drivers were using any medications and usage increased with age, as did numbers of prescriptions per driver. Logistic regression analyses revealed that drivers who used CNS medications had an increased risk of culpability; those on more than one such medication had a crude (unadjusted) odds ratio of 2.16 for having caused the crash. Among drivers less than 45 years old, CNS medications did not significantly increase the risk of crash culpability. However, among drivers aged 45 or greater, the odds ratios for one, two, or 2+ CNS medications vs. none increased dramatically from 1.89 to 4.23 to 7.99, respectively.
Conclusions:
These results suggest that special attention should be given to older drivers (45+) using two or more CNS-acting agents.
INTRODUCTION
During the past decade there has been increasing concern regarding the possible role of prescription drug use in the causation of motor vehicle crashes (Morland, 2000). Although experimental studies have assessed the effects of medicinal drugs on driving ability using laboratory tests, driving simulators, or on-the-road driving tests, these do not adequately assess real-life conditions which represent not only driver behavior but also medical conditions and the road traffic environment. In a recent systematic review of epidemiological research on the subject, Orriols et al. (2009) reported that the methodologic approaches as well as the definition of drug exposure varied considerably across studies. In addition, the populations studied were different, ranging from fatalities to those with minor injuries. While the risk of crashes related to benzodiazepines has been clearly demonstrated, the findings for other medicinal drugs remain controversial. Many medicines (prescription or over-the-counter) affect the nervous system and have the potential for affecting driving ability (Ramaekers, 1998). Anticonvulsants, antidepressants/antipsychotics, narcotics analgesics, and skeletal muscle relaxants are of special interest since they are central nervous system (CNS) acting medications and known to be associated with possible responsibility for traffic crashes. For example, the CNS depressant-impaired driver may have difficulty maintaining lane position, drive too fast or slow for conditions, fail to obey traffic signals, and be more likely to be involved in crashes due to lack of sustained attention as well as slow reaction times (OECD, 2010).
Medication use in the general population is high. A recent survey on the non-institutionalized population of the continental U.S. found that, among adults age 18+ years, 81% used at least one medication in the preceding week, 50% took at least 1 prescription drug, and 7% took 5 or more (AAA, 2009). However, despite considerable research on the effects of alcohol and some illicit drugs on traffic crashes, the extent of drug-impaired driving due to prescription drugs has yet to be clearly defined.
The goal of this research is to describe the prevalence of prescription drug use in a population of injured trauma patients and to determine the association, if any, between specific classes of drugs and crash culpability which is often used as a surrogate measure of crash risk (Soderstrom et al., 2005; Kufera et al., 2006; Drummer et al., 2004a; Drummer et al., 2004b).
METHODS
The R Adams Cowley Shock Trauma Center (STC) serves as the clinical hub of Maryland’s system of emergency/trauma care. Triage criteria are defined by the Maryland Institute for Emergency Medical Services Systems, and follow national guidelines proposed by the CDC (CDC, 2009). Approximately 7,000 patients with serious/multiple trauma and/or neurotrauma are admitted each year; approximately 2,500 are motor vehicle occupants, of those approximately 75% are drivers.
All drivers admitted to the STC in 2008, in Baltimore, Maryland following a motor vehicle collision were identified. Data were obtained from the STC Trauma Research Registry, which collects patient demographics and information from various clinical systems Data on chronic medication utilization were obtained through the hospital medication reconciliation procedures, based on the National Patient Safety Goal on medication reconciliation (Joint Commission, 2006; Thompson et al., 2007). The process involves the reconciliation of patients’ medication therapy across the continuum of care. Upon admission, clinicians are responsible for obtaining detailed reports of the patient’s prior medication history, including strength, dosage, and dates of dispensation. Complete lists are generated within 24 hours of admission and are kept in the patient’s medical record. System alerts for possible medication interaction, duplicate therapy, and other warnings are generated to inform clinicians of possible errors and prevention of any significant risks to patients. This process was initiated on paper in 2007, and available electronically in 2008 for the first time.
Medication utilization was analyzed in terms of the numbers of medications as well as the therapeutic categories; drug dosages were not taken into consideration and illicit drug use was not identified. Medications were categorized into 12 therapeutic classes: anticoagulants, anticonvulsants, antidepressants/antipsychotics, antidiabetic agents, cardiovascular agents, gastrointestinal agents, narcotics/analgesics, non-steroidal anti-inflammatory drugs (NSAIDS), respiratory agents, skeletal muscle relaxants, thyroid agents, and vitamins/minerals. All medications were reviewed and classified by a clinical pharmacologist to determine which ones were CNS-acting. Drivers perceived by the police to have been drinking were removed from the analyses, since alcohol use is known to strongly influence crash culpability (Kufera et al., 2006).
Patient records were then linked, using probabilistic linkage techniques, with police crash reports in order to determine crash culpability. Determination of driver fault was obtained from police crash reports. While this method has acknowledged limitations, it has been widely used by traffic safety researchers and employed with great success in our earlier studies of alcohol and trauma patients (Soderstrom et al., 2005; Kufera et al., 2006).
Ages were grouped as <34, 35–44, and 45+; the numbers were not large enough to examine drivers 65+, but this will be possible when additional years of data are added in the future; currently there are only 35 drivers 65 and older in this study.
Multivariable analyses were used to explore the association between medication use and crash culpability. Adjusted odds ratios (AOR) and 95% confidence intervals (CI) were compared among drivers who were not using CNS-acting medications, and on CNS-acting medications (single and multiple).
RESULTS
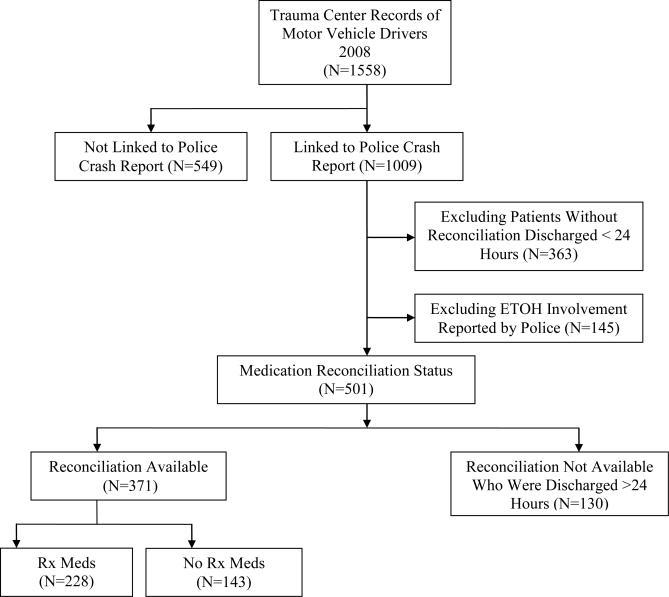
A total of 1,558 drivers were admitted to STC over the study period (Figure 1). Subsequent linkage with police crash reports was accomplished for 1,009 (64.8%) of these cases. For 145 (16.3%) of the linked cases the police indicated that they believed the driver had been drinking and these cases were removed from the analysis, resulting in a total of 864 drivers. Drivers with a stay less than 24 hours were excluded if their reconciliation was not known, leaving 501 drivers for analysis.
Figure 1.
Flow Chart of Study Participant Inclusion Process
Among the 501 drivers, medication reconciliation was carried out for 371 (74.0%). As shown in Table 1, 228/371 (61.5%) of drivers were using any medications. The proportion of drivers using prescription drugs increased with age (Table 1); medication use was highest among the oldest group; however, 37.2%% of drivers aged less than 34 also reported drug use. Women had a significantly higher rate of prescription drug use as compared to men; also, medication use varied considerably by race, with the highest usage among white drivers.
Table 1.
Characteristics of Drivers by Prescription Medication Use (N=371)
| On Prescrip Meds (n= 228) N (%) | No Prescrip Meds (n = 143) N (%) | P-value | ||
|---|---|---|---|---|
| Demographic | ||||
| Age | <=34 | 61 (37.2) | 103 (62.8) | <0.0001 |
| 35 – 44 | 42 (66.7) | 21 (33.3) | ||
| >=45 | 125 (86.8) | 18 (13.2) | ||
| Gender | Female | 115 (70.1) | 49 (29.9) | 0.0023 |
| Male | 113 (54.6) | 94 (45.4) | ||
| Race* | Caucasian | 179 (67.5) | 86 (32.5) | <0.0001 |
| African American | 43 (51.2) | 41 (48.8) | ||
| Others | 4 (21.0) | 15 (79.0) | ||
| Crash | ||||
| Crash Type | Single Vehicle | 75 (59.1) | 52 (40.9) | 0.64 |
| Multiple | 137 (63.4) | 79 (36.6) | ||
| Other/Unknown | 16 (57.1) | 12 (42.9) | ||
| Seatbelt Use | Yes | 180 (61.4) | 113 (38.6) | 0.61 |
| No | 30 (57.7) | 22 (42.3) | ||
| Other/Unknown | 18 (69.2) | 8 (30.8) | ||
| Daytime | Yes | 152 (71.0) | 62 (29.0) | |
| No | 76 (48.4) | 81 (51.6) | <0.0001 | |
| Fault (Culpability) | Yes | 142 (60.1) | 94 (39.9) | 0.57 |
| No | 75 (62.5) | 45 (37.5) | ||
| Unknown | 11 (73.3) | 4 (26.7) | ||
With respect to crash characteristics, no differences were noted for type of crash, seatbelt use, or at-fault status for those who did and did not report prescription medication usage. However, those with daytime crashes had significantly higher rates of medication usage as compared to drivers whose collisions occurred at night (71% vs. 48%, p<.001) The number of prescriptions per driver also increased with age (Table 2). Among drivers aged 45 and greater, only 13.2% were on no medications; 24.3% were taking five or more medications.
Table 2.
Number of Prescription Medications Per Injured Driver (N=371)
| Number of Rx | Age group (Years) | ||||
|---|---|---|---|---|---|
| <=34 | 35 – 44 | 45 + | Total | P-value | |
| 0 | 103 (62.8) | 21 (33.3) | 19 (13.2) | 143 | <0.0001 |
| 1 | 38 (23.2) | 13 (20.6) | 28 (19.4) | 79 | |
| 2 | 11 (6.7) | 11 (17.5) | 26 (18.1) | 48 | |
| 3 | 8 (4.9) | 10 (15.9) | 23 (16.0) | 41 | |
| 4 | 3 (1.9) | 4 (6.4) | 13 (9.0) | 20 | |
| >=5 | 1 (0.6) | 4 (6.4) | 35 (24.3) | 40 | |
| Total | 164(100) | 63 (100) | 144 (100) | 371 | |
The distribution of medications used by drivers by therapeutic class and age is shown in Table 3. The data in the table are person-specific, i.e. if a person used multiple drugs within one class, that category was only counted once per person; however, since drivers also used multiple drugs across classes, the totals add to more than 100%. Medications are grouped into three categories: CNS drugs, non-CNS-acting drugs, and others. Of all drivers studied, the most common medications were antidepressants/antipsychotics, (24.5%), cardiovascular agents (24.8%), narcotics analgesics (15.1%), and NSAIDS 12.4%). For the youngest drivers, the most prevalent drugs included antidepressants/antipsychotics (14.0%), and narcotics analgesics (10.4%). For drivers aged at least 45 years and older, the highest prevalence was for cardiovascular agents (50.7%), antidepressants/antipsychotics (33.3%), and NSAIDS (26.4%).
Table 3.
Distribution of Chronic Medications by Therapeutic Classes and Age Group (N=371)*
| Therapeutic class | Age Groups | |||||||
|---|---|---|---|---|---|---|---|---|
| <=34 (n=164) | 35–44 (n=63) | 45+ (n=144) | All (N=371) | |||||
| N | % | N | % | N | % | N | % | |
| CNS | ||||||||
| Antidepressants/Antipsychotics | 23 | 14.0 | 20 | 31.8 | 48 | 33.3 | 92 | 24.5 |
| Narcotics Analgesics | 17 | 10.4 | 10 | 15.9 | 29 | 20.1 | 56 | 15.1 |
| Anticonvulsants | 5 | 3.1 | 5 | 7.9 | 10 | 6.9 | 20 | 5.4 |
| Skeletal muscle relaxer | 4 | 2.4 | 2 | 3.2 | 6 | 4.2 | 12 | 3.2 |
| Non-CNS | ||||||||
| Cardiovascular Agents | 5 | 3.1 | 14 | 22.2 | 73 | 50.7 | 92 | 24.8 |
| Gastrointestinal Agents | 2 | 1.2 | 4 | 6.4 | 29 | 20.1 | 35 | 9.4 |
| Respiratory Agents | 4 | 2.4 | 8 | 12.7 | 18 | 12.5 | 30 | 8.1 |
| Anti-Diabetic Agents | 2 | 1.2 | 1 | 1.6 | 16 | 11.1 | 19 | 5.1 |
| Thyroid Hormones Agents | 0 | 0.0 | 3 | 4.8 | 11 | 7.6 | 14 | 3.8 |
| NSAIDs | 6 | 3.7 | 2 | 3.2 | 38 | 26.4 | 46 | 12.4 |
| Anticoagulants | 1 | 0.6 | 2 | 3.2 | 8 | 5.6 | 11 | 3.0 |
| Others | ||||||||
| Vitamins and Minerals | 10 | 6.1 | 1 | 1.6 | 13 | 9.0 | 24 | 6.5 |
Table 4 shows the number of CNS-acting medications used by drivers according to age groups. The highest usage for any CNS drugs is in the age group 45 years and over, with 68 of the 144 drivers (47.2%) in this age group taking CNS-acting drugs. With the exception of drivers under age 35, more than one-half of all drivers taking any CNS medications were taking two or more CNS-acting medications.
Table 4.
Distribution (%) of CNS-Acting Prescriptions by Age Group (N=134)
| Age group | Total | |||
|---|---|---|---|---|
| <=34 | 35 – 44 | >=45 | ||
| Number of CNS-acting drugs | ||||
| 1 | 20 (52.6) | 12 (42.9) | 27 (39.7) | 59 |
| 2 | 7 (18.4) | 9 (32.1) | 21 (30.9) | 37 |
| 3 | 9 (23.7) | 3 (10.7) | 11 (16.2) | 23 |
| >=4 | 2 (5.3) | 4 (14.3) | 9 (13.2) | 15 |
| Total | 38(100.0) | 28 (100.0) | 68(100.0) | 134 |
Logistic regression analyses revealed that drivers who used CNS medications had an increased risk of culpability; those on more than one such medication had a crude (unadjusted) odds ratio of 2.16 for having caused the crash (Table 5). While there was no univariate association between culpability and age, interaction effects were noted between CNS drug use and age with the effect of CNS drugs being much greater in the 45 years and older group (Table 6). Because of this finding we explored interaction terms between age and CNS medication use, as shown in Table 6. Race and gender did not improve the fit and were not included in the final model. Among drivers less than 45 years of age, CNS medications did not significantly increase the risk of crash culpability. However, they did significantly increase the risk among older drivers. Among drivers aged 45 or greater, the odds ratios for one, two, or 2+ CNS medications vs none increased dramatically from 1.89 to 4.23 to 7.99, respectively.
Table 5.
The Associations Between Multiple CNS Meds Use and Culpable Crash Risk Among Drivers who Did Not drink Determined by Police Report (N=371)
| Culpable crash risk | ||
|---|---|---|
| Unadjusted OR | 95% CI | |
| Main predictor | ||
| No CNS med (n=237) | 1 | – |
| On one CNS meds (n=59) | 1.23 | 0.68 – 2.23 |
| On more than one CNS meds (n=75) | 2.16 | 1.20 – 3.89 |
| Other predictors | ||
| Age | ||
| <=34 | 1 | – |
| 35 – 44 | 0.58 | 0.32 – 1.06 |
| >=45 | 0.75 | 0.47 – 1.20 |
| Gender | ||
| Female | 1 | – |
| Male | 1.35 | 0.88 – 2.06 |
| Race | ||
| Others | 1 | – |
| Caucasian | 1.06 | 0.40 – 2.79 |
| African American | 0.90 | 0.32 – 2.52 |
Table 6.
Odds Ratio of Culpability by CNS Drug Use Stratified by Age Group (N = 371)
| Risk of Crash Culpability | ||
|---|---|---|
| OR | 95% CI | |
| Age<=34 | ||
| 1 vs. no CNS meds | 1.13 | 0.40–3.14 |
| 2 vs. no CNS meds | 1.25 | 0.42–3.76 |
| 2 vs 1 CNS meds | 1.11 | 0.27–4.55 |
| Age35 – 44 | ||
| 1 vs. no CNS meds | 1.05 | 0.28–3.97 |
| 2 vs. no CNS meds | 0.75 | 0.23–2.46 |
| 2 vs 1 CNS meds | 0.71 | 0.16–3.23 |
| Age 45 + | ||
| 1 vs. no CNS meds | 1.89 | 0.77–4.65 |
| 2 vs. no CNS meds | 7.99 | 2.83–22.57 |
| 2 vs 1 CNS meds | 4.23 | 1.25–14.31 |
CONCLUSIONS/SUMMARY
Among drivers admitted to STC, 61.5% reported the use of prescription drugs; many used multiple prescriptions. These findings, based on validated drug usage in a population of drivers hospitalized following motor vehicle crashes, show a high rate of medication usage which increases with age. Although the type of medication varies with age, a large proportion of drivers in all age groups use CNS-acting medications, and many use two or more such drugs. Only those drivers taking 2 or more CNS-acting drugs were more likely to be culpable for their crash, an indication of increasing crash risk. In addition, many of the commonly used drugs have potential effects on the CNS, and should be considered as possibly affecting driving abilities. When two or more such drugs are reported, the odds ratio for having caused the crash was almost 8 times that for drivers on fewer or no drugs, among the oldest drivers (45+).
The use of medications in the community is high and the American Automobile Association conducted a survey of community dwelling drivers aged 55+ (AAA, 2009). That study found that 61.5% were noted to use one or more prescription medications that were potentially driver impairing and 10.2% were found to use five or more prescription drugs that could affect driving. In addition, 36.1% of all drivers were taking CNS drugs known to impair driving. Despite this fact, awareness of the risks of driving was low and warnings about these medications were rarely provided by health care workers. Simply describing the prevalence of medication use does not suggest that the drugs are involved in causing crashes. This project’s culpability analyses indicate that 2 or more CNS-acting drugs do increase the likelihood of the driver being culpable for the crash.
It is unclear whether crashes occur as a result of medication usage or the underlying disease for which the medication was taken, a concern that is highlighted in recent literature reviews (Cushman et al., 1990; Dischinger et al., 2000; Hours et al., 2008; Jones et al., 2009; Longo et al., 2000a; Longo et al., 2000b; McGwin et al,. 2000; Movig et al., 2004; Mura et al., 2003; Orriols et al., 2009; Parmentier et al., 2005; Petridou et al,. 2000; Sims et al,. 1998; Stutts et al., 2003; Zhang et al., 2000).
There is a need for large studies investigating the individual and combined role of medications in the risk of road traffic crashes. In addition, the differential effect of older generations of medications versus newer ones must be compared. The impact of dose changes on crash risk, at the beginning or end of treatment, also needs investigation. Some non-psychoactive medications may alter driving abilities due to their physiological functions or central side effects. Recently, a systematic review evaluated the quality of epidemiological research into effects of prescription medications on traffic safety (Orriols et al., 2009). The review included 22 studies and found the definition of drug exposure varied and potential confounding due to interaction between the effects of prescription medications and disease-related symptoms was often not controlled. Another recent paper by the same investigators found evidence for increased risk for a traffic crash among users of prescribed medications identified as having a high-risk of driving impairment according to the French medication classification system (Orriols et al., 2010). The risk of being responsible for a crash increased from 1.14 [1.06–1.22] for users of one high-risk medicine to 1.88 [1.58–2.25] for users of more than 3 high-risk medications.
Five of those studies used a similar methodology to the current paper, to assess crash responsibility among drivers with either fatal or non-fatal injuries. (Longo et al., 2000a; Longo et al., 2000b; Drummer et al., 2004a; McGwin et al., 2000; Benzodiazepine/Driving Collaborative Group, 1993; Jick et al., 1981). This methodology, which relies heavily on police determination of crash responsibility, has been widely used by traffic safety researchers, and has been employed with great success in our earlier studies of alcohol use and driving among trauma patients (Soderstrom et al., 2005; Kufera et al., 2006). The underlying hypothesis of this approach is that, if prescription drug use contributes to crash causation, it will be over-represented in drivers who were culpable.
There are several limitations to this analysis which need to be addressed in future studies. First, drug use was documented according to the physician as well as from patient and/or family sources, but laboratory findings of actual drug levels were not used to corroborate this. Also, no information was obtained on drug dosage changes in dosage at the beginning or end of treatment; misuse of prescription medications was not addressed either. Cases where alcohol use was reported by police were excluded, making it impossible to analyze the interaction of alcohol and prescription medication. Alcohol is a significant predictor of crash risk, which is difficult to separate from potential drug affects. However, alcohol can interact with many CNS-acting drugs and potentiate their effects.
Another limitation is that because complete data on medication reconciliation has only been available for one year, we did not have sufficient numbers to separately examine risks in older persons (65 and over) who have higher usage of prescription drugs.
As the driving population continues to age, medication usage and its effects on driving will become more visible as a major public health problem. Based on these findings, among drivers injured in motor vehicle crashes, more attention should be focused on older drivers (45+) using two or more CNS-acting agents.
Acknowledgments
The authors would like to acknowledge the significant contributions of Ms. Ying Tang, and Ms. Cindy Burch, who assisted with the programming of the analysis.
REFERENCES
- AAA Foundation for Traffic Safety Older Adults’ Knowledge About Medications that can Impact Driving. Aug, 2009. AAAFoundation.org.
- Benzodiazepine/Driving Collaborative Group Are benzodiazepines a risk factor for road accidents. Drug Alcohol Depend. 1993;33(1):19–22. doi: 10.1016/0376-8716(93)90029-p. [DOI] [PubMed] [Google Scholar]
- CDC Guidelines for Field Triage of Injured Patients. MMWR. 2009 Jan;58(RR-1) [PubMed] [Google Scholar]
- Cushman LA, Good RG, States JD. Psychiatric disorders and motor vehicle accidents. Psychological Reports. 1990;67(2):483–489. doi: 10.2466/pr0.1990.67.2.483. [DOI] [PubMed] [Google Scholar]
- Dischinger PC, Ho SM, Kufera JA. Medical conditions and car crashes. Annu Proc Assoc Adv Automot Med. 2000;44:335–346. [PMC free article] [PubMed] [Google Scholar]
- Drummer OH, Gerostamoulos J, Batziris H, et al. The involvement of drugs in drivers of motor vehicles killed in Australian road traffic crashes. Accid Anal Prev. 2004a Mar;36(2):239–248. doi: 10.1016/s0001-4575(02)00153-7. [DOI] [PubMed] [Google Scholar]
- Drummer OH. Postmortem toxicology of drugs of abuse. Forensic Sci Int. 2004b Jun 10;142(2–3):101–113. doi: 10.1016/j.forsciint.2004.02.013. [DOI] [PubMed] [Google Scholar]
- Hours M, Fort E, Charnay P, Bernard M, Martin JL, Boisson D. Diseases, consumption of medicines and responsibility for a road crash: A case-control study. Accid Anal Prev. 2008;(5):1789–1796. doi: 10.1016/j.aap.2008.06.017. [DOI] [PubMed] [Google Scholar]
- Jick H, Hunter JR, Dinan BJ, Madsen S, Stergachis A. Sedating drugs and autaomobile accidents leading to hospitalization. Am J Public Health. 1981;71(12):1399–1400. doi: 10.2105/ajph.71.12.1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joint Commission on Accreditation of Healthcare Organizations Using medication reconciliation to prevent errors. Jt Comm J Qual Patient Saf. 2006;32(4):230–232. doi: 10.1016/s1553-7250(06)32030-2. [DOI] [PubMed] [Google Scholar]
- Jones AW, Kugelberg FC, Holmgren A, Ahlner J. Five-year update on the occurrence of alcohol and other drugs in blood samples from drivers killed in road-traffic crashes in Sweden. Forensic Sci Int. 2009;186(1–3):56–62. doi: 10.1016/j.forsciint.2009.01.014. [DOI] [PubMed] [Google Scholar]
- Kufera JA, Soderstrom CA, Dischinger PC, Ho SM, Shepard A. Crash culpability and the role of driver blood alcohol levels. Annu Proc Assoc Adv Automot Med. 2006;50:91–106. [PMC free article] [PubMed] [Google Scholar]
- Longo MC, Hunter CE, Lokan RJ, White JM, White MA. The prevalence of alcohol, cannabinoids, benzodiazepines and stimulants amongst injured drivers and their role in driver culpability: Part i: The prevalence of drug use in drive the drug-positive group. Accid Anal Prev. 2000a;32(5):613–622. doi: 10.1016/s0001-4575(99)00111-6. [DOI] [PubMed] [Google Scholar]
- Longo MC, Hunter CE, Lokan RJ, White JM, White MA. The prevalence of alcohol, cannabinoids, benzodiazepines and stimulants amongst injured drivers and their role in driver culpability: Part ii: The relationship between drug prevalence and drug concentration, and driver culpability. Accid Anal Prev. 2000b;32(5):623–632. doi: 10.1016/s0001-4575(99)00110-4. [DOI] [PubMed] [Google Scholar]
- McGwin G, Jr, Sims RV, Pulley L, Roseman JM. Relations among chronic medical conditions, medications, and automobile crashes in the elderly: a population-based case-control study. Am J Epidemiol. 2000;152(5):424–431. doi: 10.1093/aje/152.5.424. [DOI] [PubMed] [Google Scholar]
- Morland J. Driving under the influence of non-alcoholic drugs. Forensic Sci Rev. 2000;12(1/2):79–104. [PubMed] [Google Scholar]
- Movig KLL, Mathijssen MPM, Nagel PHA, Egmond T van, de Gier JJ, Leufkens HGM, Egberts ACG. Psychoactive substance use and the risk of motor vehicle accidents. Accid Anal Prev. 2004;36:631–636. doi: 10.1016/S0001-4575(03)00084-8. [DOI] [PubMed] [Google Scholar]
- Mura P, Kintz P, Ludes B, Gaulie JM, Marquet P, Martin-Dupont S. Comparison of the prevalence of alcohol, cannabis and other drugs between 900 injured drivers and 900 control subjects: Results of a French collaborative study. Forensic Sci Int. 2003;133(1–2):79–85. doi: 10.1016/s0379-0738(03)00052-5. [DOI] [PubMed] [Google Scholar]
- OECD . Drugs and Driving: Detection and Deterrence. OECD Publishing; 2010. [Google Scholar]
- Orriols L, Salmi L-R, Philip P, Moore N, Delorme B, Castro A, Lagarde E. The impact of medicinal drugs on traffic safety a systematic review of epidemiological studies. Pharmacoepidemiology and Drug Safety. 2009;18:647–658. doi: 10.1002/pds.1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orriols L, Delorme B, Gadegbeku B, Tricotel A, contrand B, Laumon B, Salmi L-R, Lagarde E. Prescription medicines and the risk of road traffic crashes: a French registry-based study. PLoS Medicine. 2010;7:1–10. doi: 10.1371/journal.pmed.1000366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parmentier G, Chastang JF, Nabi H, Chiron M, Lafont S, Lagarde E. Road mobility and the risk of road traffic accident as a driver. the impact of medical conditions and life events. Acc Anal Pre. 2005;37(6):1121–1134. doi: 10.1016/j.aap.2005.06.012. [DOI] [PubMed] [Google Scholar]
- Petridou E, Moustaki M. Human factors in the causation of road traffic crashes. Eur J Epi. 2000;16(9):819–826. doi: 10.1023/a:1007649804201. [DOI] [PubMed] [Google Scholar]
- Ramaekers JG. Behavioural toxicity of medicinal drugs. Practical consequences, incidence, management and avoidance. Drug Safety. 1998;18:189–208. doi: 10.2165/00002018-199818030-00004. [DOI] [PubMed] [Google Scholar]
- Sims RV, Owsley C, Allman RM, Ball K, Smoot TM. A preliminary assessment of the medical and functional factors associated with vehicle crashes by older adults. J Amer Ger Soc. 1998;46(5):556–561. doi: 10.1111/j.1532-5415.1998.tb01070.x. [DOI] [PubMed] [Google Scholar]
- Stutts JC, Wilkins JW, Scott Osberg J, Vaughn BV. Driver risk factors for sleep-related crashes. Accid Anal Prev. 2003;35(3):321–331. doi: 10.1016/s0001-4575(02)00007-6. [DOI] [PubMed] [Google Scholar]
- Soderstrom CA, Dischinger PC, Kufera JA, Ho SM, Shepard A. Crash culpability relative to age and sex for injured drivers using alcohol, marijuana or cocaine. Annu Proc Assoc Adv Automot Med. 2005;49:327–341. [PMC free article] [PubMed] [Google Scholar]
- Thompson KK. Medication reconciliation: challenges and opportunities. Am J Health Syst Pharm. 2007 Sep 15;64(18):1912. doi: 10.2146/ajhp060622. [DOI] [PubMed] [Google Scholar]
- Zhang J, Lindsay J, Clarke K, Robbins G, Mao Y. Factors affecting the severity of motor vehicle traffic crashes involving elderly drivers in Ontario. Accid Anal Prev. 2000;32(1):117–125. doi: 10.1016/s0001-4575(99)00039-1. [DOI] [PubMed] [Google Scholar]