Abstract
Objective
This prospective study aimed to evaluate dimensions of sacral rhomboid (quadrangular area at lower back) as predictors of Contracted pelvis (CP).
Methods
In 300 uncomplicated primigravidae after 37 weeks gestation, transverse and vertical diagonal (TD and VD) of sacral rhomboid were recorded. Post- delivery, patients fell into two groups: Normal Deliveries (group 1) and CP (group 2, i.e., LSCS for contracted pelvis, instrumental delivery for Non Progress of Labor (NPOL) or birth mishaps). Analysis was done with SPSS version 10.5 and cross tabulation.
Results
Rhomboid dimensions were smaller in CP group (P value 0.003 and 0.012. On univariate analysis, 10th percentile cutoff of TD was the most significant risk factor with Odds ratio of 7.5 (95% CI 3.5–16.2). VD and height below 10th percentile had Odds ratio of 2.7 (95% CI 1.2–6.1) and 2.99 (95% CI 1.2–7.3), respectively. Both dimensions of sacral rhomboid below 10th percentile increased risk of CP by 13 times (OR 13, 95% CI 3.5–48.6) and detected 2 out of 3 at risk women.
Conclusion
Smaller dimensions of sacral rhomboid are promising screening parameter for contracted pelvis which can be used in community to pick up high risk primigravidae.
Keywords: Sacral rhomboid, Contracted pelvis, Primigravidae, Indian, Predict
Introduction
Pelvic disproportion complicates 2–15% of pregnancies [1–3] and is associated with significant maternal and fetal complications, [2, 4]. The antenatal prediction of this condition and timely management is essential for decreasing its contribution to obstetric mishaps [4]. As most women in developing countries are unable to avail high level of health care, it is essential to develop reliable screening parameters that can be used by all health personnel at primary level. Maternal height is presently the only parameter incorporated in antenatal charts for identification of women at risk of pelvic disproportion. Other anthropometric variables viz. maternal weight, shoe size and external pelvic measurements have also been evaluated with conflicting results [5, 6].
In the nineteenth century, Adolf Gustav Michaelis described a rhomboid on the lower back overlying the sacrum (Fig. 1). The posterior iliac spines bound it on either side, L5 vertebra superiorly and upper end of natal cleft inferiorly. Michaelis noticed that its shape and size differed in women with and without contracted pelvis [7, 8]. However, it was abandoned without complete evaluation until the year 2000 when two African studies reported its use in identifying women with cephalopelvic disproportion [1, 9].
Fig. 1.
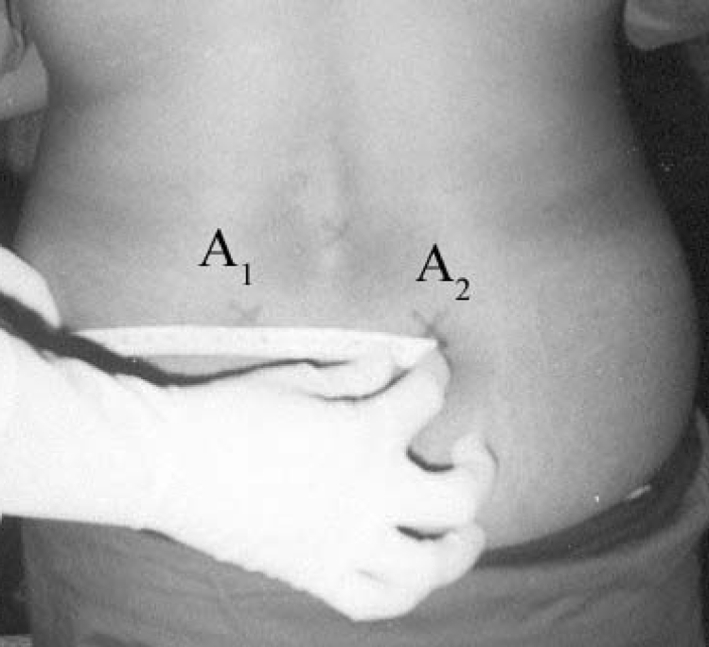
Measurement of transverse diagonal of rhomboid
The present study was conducted with the aim to evaluate the dimensions of the sacral rhomboid as predictors of contracted pelvis and to compare its efficacy to other measures like maternal height, weight and external pelvic parameters.
Material and Methods
This was a prospective study conducted at University College of Medical Sciences and Guru Teg Bahadur Hospital, New Delhi, approved by the ethical committee of the institution. It included 300 primigravidas at or beyond 37 week of pregnancy attending the antenatal clinic. Women were excluded if they had pelvic or leg deformities, twin pregnancies, non vertex presentation, complicating medical and surgical illness and delivered fetuses <2 kg or >4 kg.
The following points were marked on the woman’s back after obtaining written informed consent (See Figs. 1, 2)
The two posterior iliac spines (A1, A2) as protuberances on the dimples overlying gluteal region.
Uppermost point of natal cleft which represented lower border of sacrum (C).
Spine of lumbar 5 vertebra, this corresponding to upper border of sacrum (B).
Vertical diagonal (VD) of sacral rhomboid was measured between point B and C. Transverse diagonal (TD) was measured from point A1 and A2 (Figs. 1, 2).
Fig. 2.
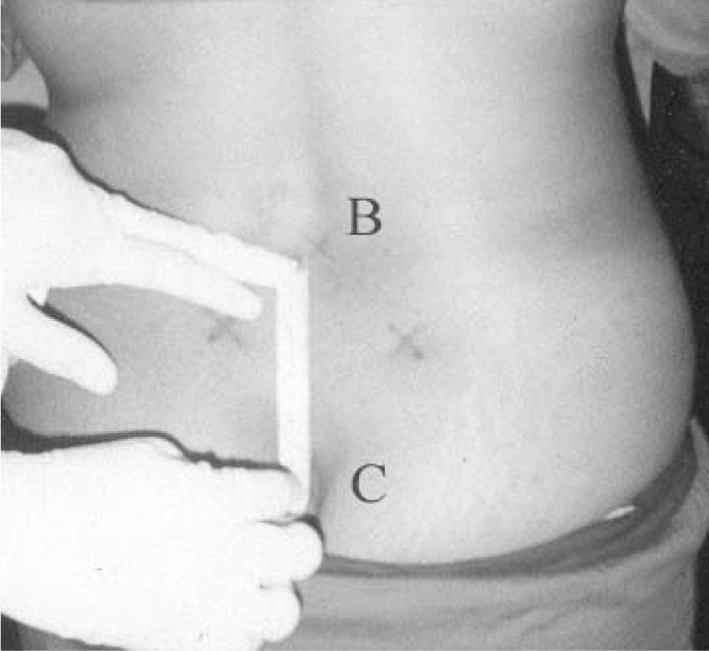
Measurement of vertical diagonal of rhomboid
A single observer recorded these measurements using a flexible graduated measuring tape.
In all these subjects’ height (cm), weight (kg) and external pelvic parameters (cm) viz. intercrestal, intertrochantric and anteroposterior diameter of inlet were also recorded along with neonatal birth weight (gm).
These measurements were recorded separate from the antenatal record and had no bearing on the subsequent labor management of these subjects. Following delivery, the women were allotted into two groups.
Group 1: Controls (no CP): included 264 women having uncomplicated vertex births.
Group 2: Cases (CP): included 36 women with pelvic disproportion, i.e., 1. Caesarean section for disproportion detected on pelvic assessment or for non-descent/non rotation of fetal head; 2. Vacuum or forceps delivery for non-descent/non rotation of fetal head or; 3. Vaginal delivery complicated by obstruction, birth trauma or unexplained intrapartum asphyxia. The 10th percentile cutoffs of maternal parameters were taken as the risk factors for contracted pelvis. For neonatal weight 90th percentile was taken as cutoff. Using SPSS version 10.5 and cross tabulation, univariate analysis was done to assess predictive ability of these factors.
Results
Out of the 300 women, 36 (12%) were detected to have contracted pelvis/pelvic disproportion and formed group 2. In this group 22 underwent Caesarean section, 13 had operative vaginal deliveries and 1 delivery was complicated by intracranial hemorrhage in baby. These women were older than women in group 1. Maternal weight was not significantly different in the two groups (Table 1).
Table 1.
Comparison of maternal parameters in two groups
| Maternal parameters | GROUP 2 (n: 264) | GROUP 2 (n: 36) | P value |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Age in years | 22.5 ± 2.49 | 23.5 ± 2.77 | 0.011* |
| Height (cm) | 154 ± 5.97 | 150.5 ± 7.25 | 0.003* |
| Weight (kg) | 57.8 ± 7.63 | 59.7 ± 7.76 | 0.168 |
| Anteroposterior diameter (cm) | 20.8 ± 1.55 | 21.25 ± 1.89 | 0.118 |
| Intercrestal distance (cm) | 25.4 ± 1.74 | 25.3 ± 1.82 | 0.65 |
| Intertrochanteric distance (cm) | 29.9 ± 1.84 | 29.8 ± 1.95 | 0.86 |
| Transverse diagonal (cm) | 10.54 ± 0.71 | 10.04 ± 0.91 | 0.003* |
| Vertical diagonal (cm) | 11.85 ± 1.027 | 11.39 ± 1.1 | 0.012* |
| Birth weight (gm) | 2810 ± 340 | 3012 ± 417.6 | 0.001* |
* Significant P values
Mean Maternal height was significantly less in group 2 (P value 0.003). 31 women in total were identified with height below 10th percentile (<146.5 cm) out of which 8 (25%) were inferred to have CP. Odds ratio indicated a 2.99 times (95% CI 1.22–7.32) increased risk of disproportion at this cutoff (Tables 1, 2).
Table 2.
Univariate analysis of 10th percentile cutoffs of maternal parameters
| Parameter | No. of women | Group 1 | Group 2 | Odds ratio | Confidence interval 95% | χ2 Value | |
|---|---|---|---|---|---|---|---|
| Height | |||||||
| <146.5 cm | 31 | 23 | 8 | 2.994 | 1.22 | 7.32 | 6.24 |
| ≥146.5 cm | 269 | 241 | 28 | ||||
| Antero posterior | |||||||
| <19 cm | 37 | 33 | 4 | 0.875 | 0.29 | 2.63 | NS |
| ≥19 cm | 263 | 231 | 32 | ||||
| Inter crestal | |||||||
| <23 cm | 32 | 27 | 5 | 1.42 | 0.51 | 3.94 | NS |
| ≥23 cm | 268 | 237 | 31 | ||||
| Inter trochanteric | |||||||
| <28 cm | 54 | 45 | 9 | 1.62 | 0.72 | 3.68 | NS |
| ≥28 cm | 246 | 219 | 27 | ||||
| Transverse diagonal | |||||||
| <9.5 cm | 45 | 28 | 17 | 7.54 | 3.52 | 16.17 | 33.31 |
| ≥9.5 cm | 255 | 236 | 19 | ||||
| Vertical diagonal | |||||||
| <10.5 cm | 43 | 33 | 10 | 2.69 | 1.19 | 6.08 | 6.022 |
| ≥10.5 cm | 257 | 231 | 26 | ||||
| Birth weight | |||||||
| >3250 gm | 28 | 18 | 19 | 9.99 | 4.67 | 21.3 | 45.72 |
| ≥3250 gm | 272 | 246 | 26 | ||||
NS not significant
Mean Transverse diagonal of sacral rhomboid (TD) was 0.5 cm less in the group 2, and was statistically significant (P value 0.003). When the 10th percentile (<9.5 cm) was taken as cut off, 45 women were identified to be at risk and 17 (37%) actually had CP. Odds ratio indicated that TD < 9.5 cm alone increased the risk by 7.5 times (95% CI 3.52–16.17) (Tables 1, 2).
Mean Vertical diagonal of sacral rhomboid (VD) was also 0.5 cm less in group 2, this being statistically significant (P value 0.012). 43 women fell below the 10th percentile cut off (<10.5 cm) and 10 (25%) finally had CP. Odds ratio indicated a 2.7 times increased risk of disproportion with VD < 10.5 cm (95% CI 1.19–6.09) (Tables 1, 2).
Mean anteroposterior, intercrestal and intertrochanteric distances were not significantly different between group 1 and 2 (Table 1). 10th percentile cut off for these parameters indicated no risk (Table 2).
Combination Models: Combination models of the significant parameters were constructed to enhance the predictive accuracy (Table 3)
Table 3.
Univariate analysis of combination models
| Combination models | No. of women | Group 1 | Group 2 | Odds ratio | Confidence interval 95% | χ2 Value | |
|---|---|---|---|---|---|---|---|
| HTTDa | 14 | 7 | 7 | 8.86 | 2.9 | 27.05 | 20.08 |
| * | 286 | 257 | 29 | ||||
| HTVDb | 9 | 4 | 5 | 10.48 | 2.67 | 41.11 | 16.67 |
| * | 291 | 260 | 31 | ||||
| TDVDc | 10 | 4 | 6 | 13.00 | 3.47 | 48.68 | 22.57 |
| * | 290 | 260 | 30 | ||||
aHeight(HT) <146.5 cm and transverse diagonal of sacral rhomboid (TD) <9.5 cm
bHeight(HT) <146.5 cm and vertical diagonal of sacral rhomboid (VD) <10.5 cm
cTransverse diagonal of sacral rhomboid (TD) <9.5 cm and vertical diagonal of sacral rhomboid (VD) <10.5 cm
* Combinations other than above
Model-I: (TD + VD)
10 women had both transverse diagonal and vertical diagonal below 10th percentile (TD < 9.5 cm and VD < 10.5 cm). Out of these 6 (60%) were found to have CP. This combination increased the risk of disproportion by 13 times (OR 13.00, 95% CI 3.47–48.68).
Model-II: (TD + ht.)
Fourteen Women had Transverse diagonal <9.5 cm and height <146.5 cm and 7 out of these finally had CP. They were 8.86 times more at risk (OR 8.86, 95% CI 2.9–27.05).
Model-III: (VD + ht.)
Out of 9 women who had Vertical diagonal <10.5 cm together with height <146.5 cm, 5 were detected to have CP, i.e., this model posed a risk of 10.5 times (OR 10.48, 95% CI 2.67–41.11).
Neonates in group 2 were significantly heavier than in group 1, the mean weight in this group being more than 3 kg.
Discussion
The incidence of pelvic disproportion/(Contracted Pelvis) in this study was 12%. Considering the tertiary center setting and primiparity of recruited women, this is comparable to incidences reported by various observers [1–3, 10]. Disproportion was found to be more common in older women although the reports in literature in this regard are conflicting [1–3, 9–11]. The ACOG bulletin has also reported age more than 35 years to be a risk factor for second stage dystocia [12]. The women were shorter in disproportion group. When 10th percentile values (<146.5 cm) were used risk of CPD was 3 times and up to 26% women with CPD could be detected using this parameter alone (sensitivity 25.8%). These findings are consistent with the observations of various workers who have found short stature to be a significant risk factor for dystocia. When used as a screening tool, it has a sensitivity of 20–30%, specificity of 90–93% and relative risk of 2–3 times [1, 9, 11, 13]. Maternal weight was not found to be different in the two groups in the present study. Although earlier workers have reported similarly, [11, 13] a recent study found that women with higher BMIs and pregnancy weight gain are more at risk for disproportion [15]. The mean transverse diagonal of sacral rhomboid was found to be significantly smaller in the disproportion group. The 10th percentile cutoff (<9.5 cm) had sensitivity of 38% in identifying the women at risk of CPD and the risk increased 7.5 times. These findings are consistent with those reported by Hubert Lislele et al. who found sensitivity of 43%, specificity of 91% and relative risk of 7 with 10th percentile cut offs of this parameter [1, 9]. The mean vertical diagonal of the sacral rhomboid was also significantly smaller in the CPD group. 10th percentile cut off (<10.5 cm) had sensitivity of 23% and relative risk of 8.7 times. This finding is contrary to that of Hubert Lislele et al. who did not find this parameter significant [1, 9]. This can probably be attributed to the racial differences in pelvic architecture between African and Indian women. The external pelvic measurements viz. anteroposterior, intercrestal and intertrochanteric diameter in the present study were not found to be of use in predicting CPD. Although intertrochanteric diameter was found to be a significant risk factor in studies in African populationl, the other parameters have been reported to have low sensitivities by other observers [1, 7, 8, 9, 11–15]. Heavier babies were more common in the disproportion group this being an obvious finding as fetal size is an integral component of CPD. When combination models using maternal height, transverse and vertical diagonals of sacral rhomboid were evaluated, the detection rates increased to 50–60% and the risk increased manifold. As actual number of women in group 2 is small, these combination models had very few subjects and their validity needs confirmation by larger studies.
But we can safely conclude that sacral rhomboid dimensions are promising new parameters that warrant a place in antenatal screening charts alongside maternal height for timely identification of women at risk of CPD. Larger studies across various ethnic groups need to be conducted to find the cutoffs for a particular population. In developing world, this can have a long-term impact in reducing maternal and neonatal morbidity and mortality.
Acknowledgments
We genuinely acknowledge the assistance received from our statistical interpreter Dr. T. P. Krishna, National Institute of Nutrition, Hyderabad.
References
- 1.Hubert BL, Mischel B, Kalala CT, et al. Maternal height and external pelvimetry to predict cephalopelvic disproportion in nulliparous African women: a cohort study. Br J Obstet Gynaecol. 2000;107:947–952. doi: 10.1111/j.1471-0528.2000.tb10394.x. [DOI] [PubMed] [Google Scholar]
- 2.Melah GS, El-Nafaty AU, Massa AA, et al. Obstructed labour: a public health problem in Gombe, Gombe State, Nigeria. J Obstet Gynaecol. 2003;23:369–373. doi: 10.1080/01443610310001119510. [DOI] [PubMed] [Google Scholar]
- 3.Brabin L, Verhoeff F, Brabin BJ. Maternal height, birthweight and cephalo pelvic disproportion in urban Nigeria and rural Malawi. Acta Obstet Gynecol Scand. 2002;81:502–507. doi: 10.1034/j.1600-0412.2002.810605.x. [DOI] [PubMed] [Google Scholar]
- 4.Dafallah SE, Ambago J, El-Agib F. Obstructed labor in a teaching hospital in Sudan. Saudi Med J. 2003;24:1102–1104. [PubMed] [Google Scholar]
- 5.World Health Organisation Maternal Anthropometry and Pregnancy Outcomes. A WHO collaborative study. WHO Bull. 1995;73:1–69. [PMC free article] [PubMed] [Google Scholar]
- 6.Sue F, Judy M, Allison P, et al. Maternal height and shoe size as predictors of pelvic disproportion: an assessment. Br J Obstet Gynaecol. 1985;92:1239–1245. doi: 10.1111/j.1471-0528.1985.tb04869.x. [DOI] [PubMed] [Google Scholar]
- 7.Spert H. Gustav Adolf Michaelis and Michaelis’ Rhomboid. In: Obstetric and Gynaecologic Milestones Illustrated. New York: Parthenon Publishing Group. 1996; 162–5.
- 8.Longo LD. Classic pages in obstetrics and gynaecology. Das enge Becken nach eigenen Beobachtungen and Untersuchungen. Gustav Adolf Michaelis. Leipzig, Georg Wigand, 1851. Am J Obstet Gynaecol. 1977;129:695–696. [PubMed] [Google Scholar]
- 9.Hubert BL, Kalal CT, Sylvain M. Association between external pelvimetry and vertex delivery complications in African women. Acta Obstet Gynaecol Scand. 2000;79:673–678. [PubMed] [Google Scholar]
- 10.Vivien DT. Antenatal screening: its use in assessing obstetric risk factors in Zimbabwe. J Epidemiol Community Health. 1994;48:297–305. doi: 10.1136/jech.48.3.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Helen AB. Anthropometric measures as a predictor of cephalopelvic disproportion. Trop Doct. 1997;27:135–138. doi: 10.1177/004947559702700305. [DOI] [PubMed] [Google Scholar]
- 12.ACOG Practice Bulletin Number 49, December 2003: Dystocia and Augmentation of Labor. Obstet Gynecol. 2003;102:1445–54. [DOI] [PubMed]
- 13.Bruno D, Roger VC, Thierry L. The value of maternal height as risk factor of dystocia: a meta-analysis. Trop Med Int Health. 1996;1:510–521. doi: 10.1046/j.1365-3156.1996.d01-83.x. [DOI] [PubMed] [Google Scholar]
- 14.Jensen H, Agger AO, Rasmussen KL. The influence of prepregnancy body mass index on labor complications. Acta Obstet Gynecol Scand. 1999;78:799–802. doi: 10.1080/j.1600-0412.1999.780911.x. [DOI] [PubMed] [Google Scholar]
- 15.Young TK, Woodmansee B. Factors those are associated with cesarean delivery in a large private practice: the importance of prepregnancy body mass index and weight gain. Am J Obstet Gynecol. 2002;187:312–318. doi: 10.1067/mob.2002.126200. [DOI] [PubMed] [Google Scholar]


