Abstract
Fractures of the distal radius are among the most common injuries of the upper extremity, though treatment has traditionally focused on restoration of the radiocarpal joint and late sequelae may persist. X-ray imaging underestimates sigmoid notch involvement following distal radius fractures. No classification system exists for disruption patterns of the sigmoid notch of the radius associated with distal radius fractures. This study quantifies the anatomy of the sigmoid notch and identifies the landmarks of the articular surface and proximal boundaries of the distal radioulnar joint (DRUJ) capsule. Computed tomography scans of freshly frozen cadaveric hands were used - followed by dissection, and three-dimensional reconstruction of the distal radius and sigmoid notch. The sigmoid notch surface was divided into two surfaces and measured. The Anterior Posterior (AP) and Proximal Distal (PD) widths of the articulating surface were reviewed, along with the radius of curvature, version angle and depth. The study showed that the sigmoid notch is flatter than previously believed - and only the distal 69% of its surface is covered by cartilage. On average, it has about nine degrees of retroversion, and its average inclination is almost parallel to the anatomical axis of the radius. Clinical implications exist for evaluation of the DRUJ involvement in distal radius fractures or degenerative diseases and for future development and evaluation of hemiarthroplasty replacement of the distal radius.
Key words: distal radius fracture, sigmoid notch, distal radioulnar joint, hemiarthroplasty.
Introduction
Distal radius fractures are among the most common injuries of the upper extremity, but their impact to the sigmoid notch and Distal Radioulnar Joint (DRUJ) has not been clearly understood. Treatment of distal radius fractures has traditionally focused on restoration of the radiocarpal joint - and late sequelae may persist. In a study conducted by Frykman (1967), 25% of distal radius fracture patients had some complaints one year following the injury – involving pain, weakness and limited range of motion.1 Rozental et al. concluded that the distal radius fracture extension into the sigmoid notch was evident in 65% of the patients following a computed tomography (CT) scan, as opposed to 35% following a radiograph.2 Other studies evaluating the sigmoid notch with computed tomography following distal radius fractures also noted the inadequacy of plain radiographs to determine the extent of the fracture. Plain x-rays appear to underestimate sigmoid notch involvement following distal radius fractures and, in fact, have often poorly determined the adequate classification for distal radial fractures in general.3
While new information on the more thorough evaluation of distal radius fractures identified with three-dimensional computed tomography was reported by Harness et al., there is very little information available in the literature that assesses the bony and cartilage architecture of the sigmoid notch.4 And a classification system for disruption patterns of the sigmoid notch of the radius associated with distal radius fractures has not yet been established. The purpose of this study is to quantify the anatomy of the sigmoid notch, identify the landmarks of the articular surface, and identify the proximal boundaries of the distal radioulnar joint capsule.
Materials and Methods
Receiving approval from an Institutional Review Board, fifteen fresh frozen, unpaired mid-brachium hand specimens were used for this study - 9 male and 6 female, with ages ranging from 42 to 80 years. Computerized tomography (CT) scans were taken of the affected area and then followed by dissection and measurement, and a three-dimensional reconstruction and measurement of the distal radius and sigmoid notch (Figures 1, 2 and 3). The sigmoid notch is divided into two surfaces – the articulating surface, an average of 79.78 mm2 (69.13%); and the non-articulating surface, an average of 35.84 mm2 (30.87%). The AP and PD width of the articulating surface and the PD width of the sigmoid notch were reviewed, along with the radius of curvature, version angle and depth of the sigmoid notch.
Figure 1.
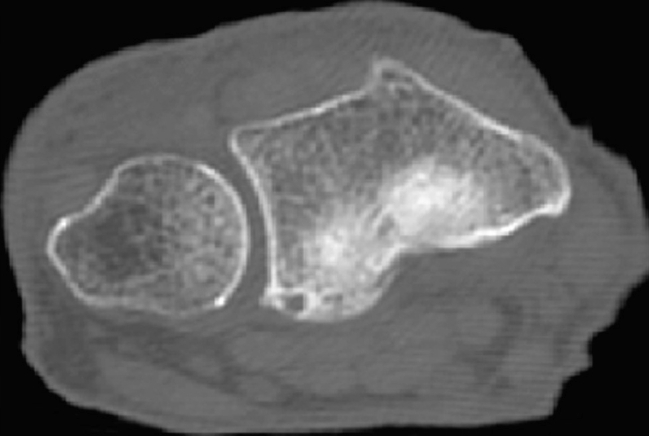
A computed tomography (CT) scan of the sigmoid notch
Figure 2.
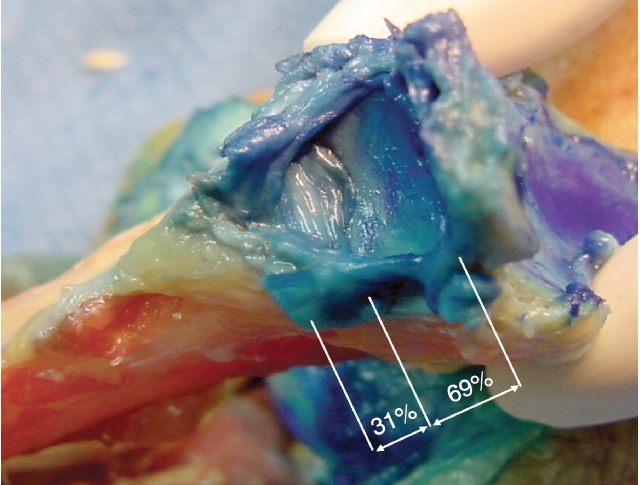
The width of the articulating and non-articulating surfaces of the Sigmoid Notch.
Figure 3.
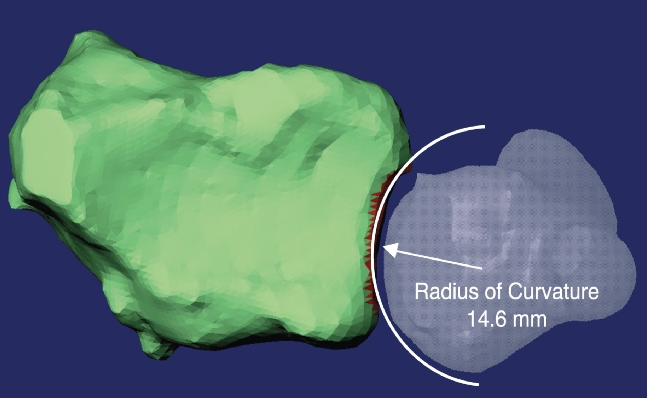
The 3-D analysis of sigmoid notch radius of curvature.
Results
The inclination of the sigmoid notch toward the radial axis was visible at 1.64 degrees with ranges between −14.46 degrees to +11.34 degrees. The AP width of the distal radius was 12.9 mm, the PD width of the articulating surface was 5.1 mm and the PD width of the sigmoid notch was 8.1 mm. The radius of curvature of the sigmoid notch was 14.6 mm, and the version angle was 9.8 degrees (Figures 4, 5). The maximum depth of the sigmoid notch was 1.67 mm (Figure 5).
Figure 4.
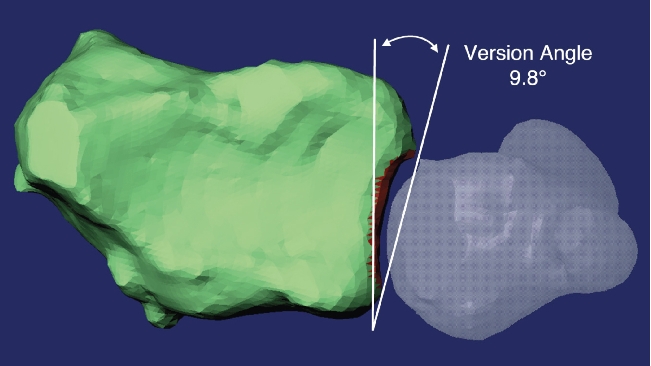
The 3-D analysis of sigmoid notch version angle.
Figure 5.
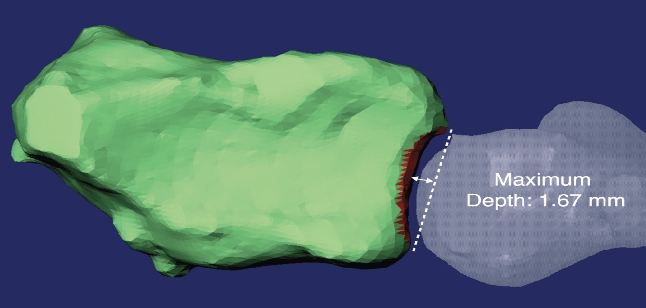
The 3-D analysis of sigmoid notch maximum depth.
Conclusions
Measurements of the AP width and radius of curvature of the sigmoid notch were compatible with the previous studies. The version angle and maximum depth of the sigmoid notch was defined.
The proximal border of the Distal Radioulnar Joint (DRUJ) and the articular surface were also defined. The study showed that the sigmoid notch is flatter than previously believed and is not entirely covered by cartilage. Only the distal 69% of its surface is covered by cartilage. It has about 9 degrees of retroversion, and its average inclination is almost parallel to the anatomical axis of the radius. Clinical implications exist for evaluation of the DRUJ involvement in distal radius fractures or degenerative diseases, as well as for future development and evaluation of hemiarthroplasty replacement of the distal radius.
Discussion
Shallow and concave, the sigmoid notch of the distal radius articulates with the convex asymmetric shaped ulnar head. Additional anatomical studies of the DRUJ, one of the least understood joints in the body, and its characteristics has generated over the years a greater understanding of the interconnected role of the sigmoid notch in distal radial fractures - affecting both the imaging tools used in assessing such injuries as well as the treatment.5–12 Though, more study is needed.
Imaging techniques available in evaluating the DRUJ include plain radiograph, computed tomography (CT), CT scans with digital reconstruction, magnetic resonance imaging (MRI), wrist arthrography, bone scans and wrist arthroscopy (Figure 6). With advanced imaging techniques such as CT scans, an effective evaluation of DRUJ subluxation, fractures and sigmoid notch abnormalities may be performed. Digital reconstruction of CT scans is especially useful to construct an image of the DRUJ.12,13
Figure 6.
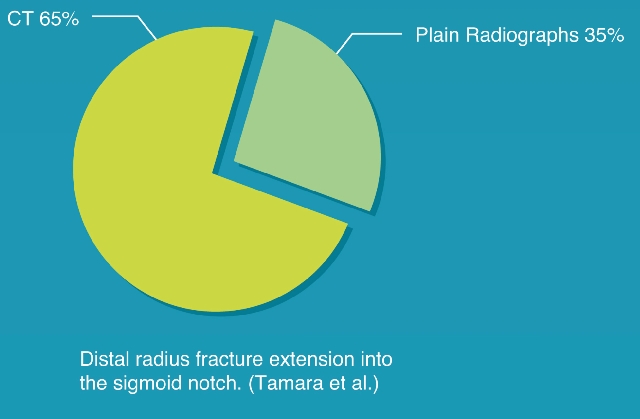
Distral radius fracture extension into the sigmoid notch.
In previous studies, inclination of the sigmoid notch toward the ulna axis was 21 degrees (Ekenstam and Hagert, anatomical study) and 8 degrees (Sagerman et al., radiographic study - 1995).14–16 In this three-dimensional analysis of a reconstructed computed tomography image of the distal radius and sigmoid notch, it was revealed that inclination of the sigmoid notch toward the radial axis was 1.64 degrees.
A study conducted by De Smet and Fabry found that the orientation of the sigmoid notch of the distal radius is related to the ulnar length and that angulation of the sigmoid notch determines the shape of the notch.9 Tolat et al. demonstrated in a study involving 50 cadaver wrists, 4 primary notch shapes in the transverse plane. Indicating that the DRUJ is part of an interconnected forearm unit that both allows for significant mobility and structural support necessary for the transmission of force across the wrist and elbow, they further showed that an important geometric joint characteristic of the DRUJ is the radius of curvature between two articulating surfaces. The radius of curvature of the ulnar head differs from the radius of curvature of the sigmoid notch, resulting in pronation/supination with both a rotational and gliding component - a transverse and anteroposterior plane.12,17
More studies investigating the dynamic three-dimensional measurement of the contact areas and congruence of the DRUJ articulating surfaces in pronation, supination and neutral would be beneficial, as well as studies with combined cadaver and radiographic data.
References
- 1.Frykman G. Fracture of the distal radius including sequelae – shoulder-hand-finger syndrome, disturbance in the distal radioulnar joint and impairment of nerve function. A clinical and experimental study. Acta Orthop Scand. 1967;108:3–3. doi: 10.3109/ort.1967.38.suppl-108.01. [DOI] [PubMed] [Google Scholar]
- 2.Rozental TD, Bozentka DJ, Katz MA, et al. Evaluation of the sigmoid notch with computed tomography following intra-articular distal radius fracture. J Hand Surg. 2001;26:244–51. doi: 10.1053/jhsu.2001.22930. [DOI] [PubMed] [Google Scholar]
- 3.Johnston GH, Friedman L, Kriegler JC. Computerized tomographic evaluation of acute distal radial fractures. J Hand Surg. 1992;17:738–44. doi: 10.1016/0363-5023(92)90326-k. [DOI] [PubMed] [Google Scholar]
- 4.Harness NG, Ring D, Zurakowski D, et al. The influence of three-dimensional computed tomography reconstructions on the characterization and treatment of distal radial fractures. J Bone Joint Surg. 2006;88:1315–23. doi: 10.2106/JBJS.E.00686. [DOI] [PubMed] [Google Scholar]
- 5.Cole DW, Elsaidi GA, Kuzma KR, et al. Distal radioulnar joint instability in distal radius fractures: the role of sigmoid notch and triangular fibrocartilage complex revisited. Injury. 2006;37:252–8. doi: 10.1016/j.injury.2005.08.019. [DOI] [PubMed] [Google Scholar]
- 6.Hagert CG. Distal radius fracture and the distal radioulnar joint - anatomical considerations. Handchir Mikrochir Plast Chir. 1994;26:22–6. [PubMed] [Google Scholar]
- 7.Hagert CG. The distal radioulnar joint in relation to the whole forearm. Clin Orthop Relat Res. 1992;275:56–54. [PubMed] [Google Scholar]
- 8.Linscheid RL. Biomechanics of the distal radioulnar joint. Clin Orthop Relat Res. 1992;275:46–55. [PubMed] [Google Scholar]
- 9.De Smet L, Fabry G. Orientation of the sigmoid notch of the distal radius: determination of different types of the distal radioulnar joint. Acta Ortoph Belg. 1993;59:269–72. [PubMed] [Google Scholar]
- 10.Katz MA, Beredjiklian PK, Bozentka DJ, Steinberg DR. Computed tomography scanning of intra-articular distal radius fractures: does it influence treatment? J Hand Surg. 2001;26:415–21. doi: 10.1053/jhsu.2001.22930a. [DOI] [PubMed] [Google Scholar]
- 11.Wallwork N, Bain G. Sigmoid notch osteoplasty for chronic volar instability of the distal radioulnar joint: a case report. J Hand Surg. 2001;26:454–9. doi: 10.1053/jhsu.2001.24968. [DOI] [PubMed] [Google Scholar]
- 12.Fornalski S, Lee T, Gupta R. Chronic instability of the distal radioulnar joint: a review. The University of Pensylvania Orthopaedic Journal (UPOJ) 2000;13:1–9. [Google Scholar]
- 13.Green DP, Hotchkiss RN, Pederson WC. Green’s Operative Hand Surgery book. Churchill Livingstone; New York: 1999. Green’s operative hand surgery. [Google Scholar]
- 14.af Ekenstam F, Hagert CG. Anatomical studies on the geometry and stability of the distal radio ulnar joint. Scand J Plast Reconstr Surg. 1985;19:17–25. doi: 10.3109/02844318509052861. [DOI] [PubMed] [Google Scholar]
- 15.af Ekenstam F. Anatomy of the distal radioulnar joint. Clin Orthop Relat Res. 1992;275:14–8. [PubMed] [Google Scholar]
- 16.Sagerman SD, Zogby RG, Palmer AK, et al. Relative articularinclination of the distal radioulnar joint: a radiographic study. J Hand Surg. 1995;20:597–601. doi: 10.1016/S0363-5023(05)80275-8. [DOI] [PubMed] [Google Scholar]
- 17.Tolat AR, Stanley JK, Trail IA. A cadaveric study of the anatomy and stability of the distal radioulnar joint in the coronal and transverse planes. J Hand Surg. 1996;21:587–94. doi: 10.1016/s0266-7681(96)80136-7. [DOI] [PubMed] [Google Scholar]


