Abstract
Vertical transmission has become the most common mode of transmission of hepatitis C virus (HCV) in children. The rate of perinatal transmission from an HCV-infected mother to her child ranges from 2% to 5% and the prevalence of HCV in children in developed countries ranges between 0.1% and 0.4%. Spontaneous viral clearance seems to be dependent on the genotype and has been reported between 2.4%-25%. For chronically infected patients, treatment with recombinant polyethylene glycol (PEG)-interferon α-2b and daily ribavirin has now been approved as standard treatment for children 2-17 years of age. In five large prospective studies, a total of 318 children and adolescents aged 3-17 years were treated either with subcutaneous PEG-interferon α-2b at a dose of 1-1.5 μg/kg or 60 μg/m² once a week in combination with oral ribavirin (15 mg/kg per day) or PEG-interferon α-2a with ribavirin. Subjects with genotype 1 and 4 received the medication for 48 wk and individuals with genotype 2 and 3 mainly for 24 wk. Overall sustained viral response (SVR) was achieved in 193/318 (60.7%) of treated patients. Stratified for genotype; 120/234 (51%) with genotype 1, 68/73 (93%) with genotype 2/3, and 6/11 (55%) with genotype 4 showed SVR. Relapse rate was between 7.7% and 17%. Overall, treatment was well tolerated; however, notable side effects were present in approximately 20%. According to recent experiences in the treatment of chronic hepatitis C in children and adolescents, a combination of PEG-interferon α with ribavirin has been found to be well tolerated and highly efficacious, particularly in individuals with genotype 2/3. Thus, this treatment can be recommended as standard of care until more effective treatment options will become available for genotype 1 patients.
Keywords: Chronic hepatitis C, Treatment, Children, Polyethylene glycol-interferon and ribavirin, Response rate
INTRODUCTION
Combination therapy of polyethylene glycol (PEG)-in-terferon α-2a or α-2b with ribavirin is standard of care for adults with chronic hepatitis C. Clear benefits in terms of sustained viral response (SVR) and side effect profile have been documented with PEG-interferon α compared with recombinant interferon α with and without ribavirin. An additional advantage of the pegylated form of interferon is the extended serum half-life, which allows a once-weekly administration regimen. Until recently, only recombinant interferon α-2b in combination with ribavirin had been approved by the Food and Drug Administration (FDA) and European Medicines Agency (EMA) for use in children and adolescents. Since December 2008 and September 2009, respectively, the FDA and EMA approved PEG-interferon α-2b in combination with ribavirin in the United States and Europe for children aged 3 years and older[1]. Although most experts believe treatment is beneficial, due to several factors associated with treating young patients with chronic hepatitis C, this topic remains controversial[2-4]. However, there is no doubt that chronic hepatitis C remains an epidemiologically important health care issue in children and adolescents. Associated costs in the United States are estimated between $17 and $40 million annually[5]. Effective treatment of chronic hepatitis C virus (HCV) at an early age would help to prevent the long-term sequelae of chronic infection, improve the prognosis of patients, and reduce health care expenditure.
The prevalence of HCV in children in developed countries ranges between 0.1% and 0.4% but may even exceed 10% in some regions of Saudi Arabia and Africa[6-8]. The rate of perinatal HCV transmission from an infected mother to her child ranges from 2% to 5%. Clinically most relevant are genotypes 1, 2 and 3; considerably less spread is genotype 4[2]. It is estimated that there are 1 million individuals aged less than 18 years infected with chronic hepatitis C worldwide[9].
Since the early 1990s, transmission of HCV infection has occurred predominantly by parenteral transfusion of blood products or by non-use of disposable syringes. However, transfusion-associated hepatitis C has now become extremely rare in countries with adequate hygienic facilities. Subjects who were particularly at risk such as premature infants, hemophiliacs, patients with thalassemia, and children with malignant diseases or organ transplantations have now reached adulthood and vertical transmission from HCV-infected mothers to their offspring has become the most common cause of chronic hepatitis C in children. Importantly, in the case of vertical infection, the chronicity rate is very high[10].
Children chronically infected with HCV may be at risk for social disintegration and impaired quality of life. A possible psychological burden may be present and some physical impairment has been described. To date, only two rather small studies have been published reporting significantly lower physical and psychosocial scores and worse cognitive functioning compared with non-infected controls[11,12].
NATURAL COURSE
Spontaneous viral clearance in vertically infected children seems to be dependent on genotype and was found to range from 2.4%-25%[13,14]. It may be higher in parenterally infected individuals and was reported to reach 35%-45% by adolescence[15,16]. Children infected with genotype 3 have a higher spontaneous clearance rate than those infected with genotype 1. Beyond the age of 4 years, spontaneous viral clearance seems to become rather unlikely[13]. Patients who do not clear the virus within the first years of life will develop chronic hepatitis C. Overall, the cumulative probability of progression to chronicity is approximately 80%[17,18]. Most children are clinically asymptomatic or show only mild unspecific symptoms. In roughly 10% of patients, hepatomegaly may be present[17]. During the chronic course, alanine aminotransferase (ALT) levels may be normal or intermittently elevated. Only few patients show persistent markedly elevated ALT levels. Inflammatory activity in liver tissue is usually mild and the risk of severe complications is low. However, despite the favourable prognosis during the first and second decade of life, approximately 4%-6% of children will develop evidence of advanced liver fibrosis or cirrhosis[19,20]. A recently published study in pediatric patients with chronic hepatitis C cured of malignancy reported liver cirrhosis in 5% after three decades of observation[21]. Progression of fibrosis depends on age and additional risk factors such as obesity and alcohol consumption. Thus, progression usually starts beyond the second life decade and there is evidence that it seems to proceed more rapidly in patients with genotype 3[22]. Large liver transplantation units have reported on children who needed liver transplantation due to progressive HCV infection[23].
TREATMENT OPTIONS
Many years ago, treatment started in adults with the use of interferons, yielding SVR rates in the 10%-15% range. According to the use of different treatment regimens and small numbers of treated children, it was difficult to compare the response rates in children to those in adults. Overall, SVR seemed to be better in children. Nineteen studies using recombinant α-interferon were published between 1992 and 2003[24]. A meta-analysis of trials with interferon-α monotherapy revealed a wide range (0%-76%, mean 27%) of SVR. Subjects infected with genotype 2 and 3 clearly responded better than patients harbouring genotype 1. Based on an increasing number of randomized controlled trials in adults, ribavirin was added to interferon-α in treatment trials for children. Between 2000 and 2005, six studies were published all demonstrating an SVR from 27% to 64%[25]. The stratification according to genotypes showed a very good response (> 80%) in patients with genotype 2 and 3 and an SVR of approximately 36%-53% in those with genotype 1. Results of an extensive trial in children published by Gonzalez-Peralta led to the approval of recombinant interferon α-2b in combination with ribavirin[26].
However, when PEG-interferon in combination with ribavirin became the standard of care for adults with chronic hepatitis C, trials in children promptly started. Some advantages were present such as a reduced injection frequency to once per week, better SVR, and better interferon tolerance. Interestingly, the sole controlled randomized trial, comparing a pegylated interferon α (PEG-interferon α-2a) with and without additional ribavirin, was only published in 2011. It clearly demonstrated that in the pediatric age group, the addition of ribavirin was necessary to obtain significantly better treatment results[27]. Specifically, in genotype 1 patients, SVR rate was 17% with PEG-interferon monotherapy compared with 47% in individuals with combination treatment. The difference was also striking in subjects infected with genotype 2 and 3 (36% vs 80%).
Up to now, results of seven trials using PEG-interferon α in combination with ribavirin have been reported[27-32]. SVR rates in patients with genotype 1 from 5 trials with more than 30 patients ranged from 44% to 59%. Achieving SVR in children with genotype 2 and 3 was very successful and yielded rates of more than 90%. The relapse rate was between 7.7% and 17%. Four trials used PEG-interferon α-2b and two used PEG-interferon α-2a in combination with ribavirin. An additional report presented the retrospective data in 33 treated Japanese children and young adults[33]. SVR rate in these patients was approximately 82%. Unfortunately, no information regarding genotypes was provided. Table 1 and Figure 1 summarize the characteristics of the five prospective studies. Peg-interferon α-2b and ribavirin were approved for patients aged 3 to 17 years of age by the FDA in December 2008 and the EMA in September 2009.
Table 1.
Sustained viral response in five representative prospective trials using polyethylene glycol-interferon alpha-2b and polyethylene glycol-interferon alpha-2a in combination with ribavirin and stratified for different clinical and laboratory parameters and genotypes, published between 2005 and 2011
| Wirth 20051 | Jara 20081 | Wirth 20101 | Total PEG-interferon a-2b trials | Schwarz 20112 | Sokal 20102 | Total all trials | |
| Dosage | 1.5 μg/kg per week | 1.0 μg/kg per week | 60 μg/m² per week | 180 μg/1.73 m²per week | 100 μg/m² per week | ||
| Total (%) | 36/61 (59) | 15/30 (50) | 70/107 (65.4) | 121/198 (61.1) | 29/55 (53) | 43/65 (66.1) | 193/318 (60.7) |
| Genotype (%) | |||||||
| 1 | 22/46 (48) | 12/26 (46) | 38/72 (53) | 72/144 (50) | 21/45 (47) | 27/47 (59) | 120/236 (51) |
| 2/3 | 13/13 (100) | 3/3 (100) | 28/30 (93) | 44/46 (96) | 8/10 (80) | 16/17 (94) | 68/73 (93) |
| 4 | 1/2 | 0/1 | 4/5 (80) | 5/8 (62) | Included in G1 | ||
| ALT-levels (%) | |||||||
| Elevated | 12/25 (48) | 27/44 (61) | 19/33 (58) | 58/102 (57) | |||
| Normal | 24/36 (67) | 42/63 (67) | 24/30 (80) | 90/129 (70) | |||
| Mode of infection (%) | |||||||
| Parenteral | 19/27 (70) | 7/9 (78) | 5/5 (100) | 31/41(76) | |||
| Genotype 1 | 13/21 (62) | 1/1 | |||||
| Vertical | 12/25 (48) | 8/21 (38) | 46/75 (61) | 66/121 (55) | |||
| Genotype 1 | 7/20 (35) | 26/52 (50) | 33/72 (46) | ||||
| Break through | 9.8% | 6/41 (15) | |||||
| Relapse | 7.7% | 8% | 6/35 (17) | ||||
ALT: Alanine aminotransferase; PEG: Polyethylene glycol.
PEG-interferon α-2b;
PEG-interferon α-2a.
Figure 1.
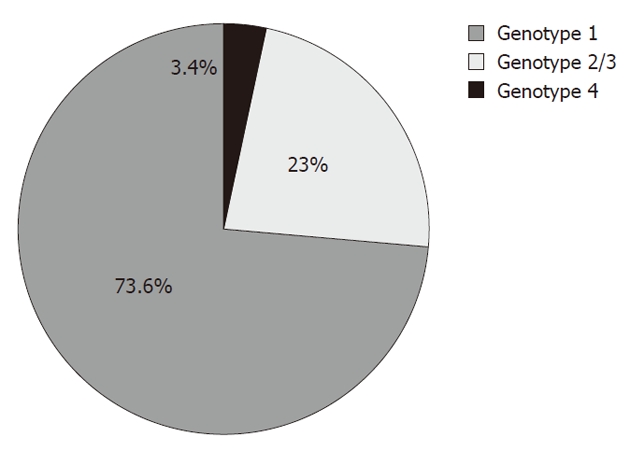
Distribution of genotypes in the five representative prospective trials using polyethylene glycol-interferon α-2b and polyethylene glycol-interferon α-2a in combination with ribavirin, published between 2005 and 2011.
Baseline viral load
Two studies stratified the results in genotype 1 patients according to the viral load before treatment. In the first study, the cut-off level was 600 000 IU/mL: 32% of children with genotype 1 and high viral load (> 600 000 IU/mL) and 73% with low viral load (< 600 000 IU/mL) achieved SVR[32]. In the second trial, the cut-off value was 500 000 IU/mL: 45% of children with genotype 1 and > 500 000 IU/mL and 62% with < 500 000 IU/mL achieved SVR[30].
Figure 2 summarizes the SVR in relevant pediatric trials using PEG-interferon in combination with ribavirin.
Figure 2.
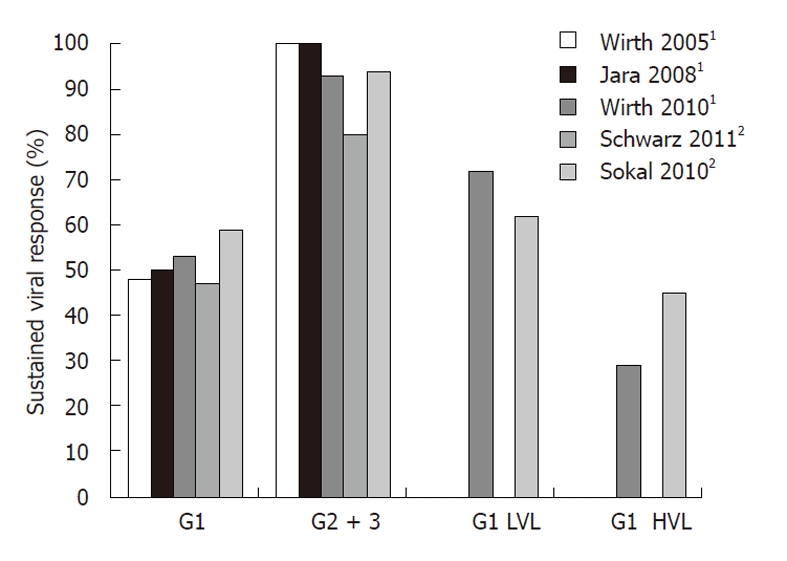
Sustained viral response in five large prospective trials with polyethylene glycol-interferon α-2b1/α-2a2 and ribavirin stratified for genotype and viral load[27,28,30-32]. G: Genotype; HVL: High viral load, > 600 000 U/mL, (Wirth et al[32]), > 500 000 U/mL (Sokal et al[30]); LVL: Low viral load, < 600 000 U/mL (Wirth et al[32]), < 500 000 U/mL (Sokal et al[30]).
Baseline aminotransferases
It is remarkable that the level of aminotransferases or histological findings by liver biopsy do not significantly correlate with SVR. However, interestingly, there was a trend towards a slightly better SVR in patients with normal aminotransferases.
Mode of infection
There is no significant correlation between SVR and the mode of infection. Nevertheless, it seems that individuals with parenteral infection may have a slightly higher probability to obtain SVR. However, the overall response rate in vertically infected subjects was 55% and in genotype 1 patients 46%, which is comparable to the SVR in adults who are mainly parenterally infected (Table 1).
Standard of care
According to approval, in principle, treatment with interferon α-2b and ribavirin administering injections thrice per week can be performed. However, the majority of experts will prefer once weekly dosing using PEG-interferon. To date in America and Europe, only PEG-interferon α-2b (60 μg/m² per week) in combination with ribavirin (15 mg/kg per day) is approved by the FDA and EMA[1]. Patients with genotypes 1 and 4 should be treated for 48 wk, with treatment discontinued at 4-6 mo if there has been no viral response. Patients with genotypes 2 and 3 should be treated for 24 wk irrespective of pre-treatment viral load. In routine clinical practice, there is no need to perform liver biopsy before initiating treatment. In addition, pre-treatment levels of aminotransferases and mode of infection are not predictive for SVR. A five-year follow-up study of children with SVR treated with interferon α and ribavirin showed permanent viral elimination in 98% (Kelly D, personal communication).
Re-treatment
Response rates in patients retreated with a standard of care protocol are dependent on the primary treatment regimen. Individuals with previous interferon α mono-therapy or recombinant α-interferon in combination with ribavirin may achieve a higher response rate. There are no studies specifically addressing re-treatment except for the trial by Gerner et al[34], which has been performed with a natural interferon α in combination with ribavirin. Previously published reports have only included small numbers of children with failed response, demonstrating a re-treatment response rate of 40%-50% in those with previous interferon α monotherapy. Gerner et al[34] reported SVR in only 2/18 patients. Thus, re-treatment, particularly in individuals who have been primarily treated with PEG-interferon and ribavirin, remains prognostically difficult and cannot be recommended until new combination treatment options including directly acting antivirals such as protease inhibitors become available.
ADVERSE EVENTS
The majority of treated children and adolescents will tolerate PEG-interferon and ribavirin well. Nevertheless, almost all patients will experience at least one side effect. The clinical significance of adverse events is summarized in Table 2. Most adverse events are mild to moderate, such as flu-like symptoms including fever, anorexia, fatigue, dry skin and moderate hair loss. In some patients, dose reduction of PEG-interferon may be necessary due to decreased white blood cell counts. Severe anemia is very rare; hence, the need for dose reduction of ribavirin is extremely infrequent. The rates of discontinuation of treatment due to adverse events were low in all trials published. Severe psychiatric side effects were rare in pre-pubertal individuals, but may be of significance in affected individuals. Appearance of thyroid autoantibodies and thyroid dysfunction during long-term treatment (> 24 wk) has to be considered and carefully monitored. Up to 20% of treated patients, particularly with genotype 1, may have abnormal thyroid stimulating hormone levels or other signs of thyroid dysfunction[31,35]. Another notable side effect is transient growth impairment. Inhibited growth can be observed in 50%-70% with decrease of growth velocity below the 3rd percentile. Shortly after the end of treatment, catch-up growth usually starts with an increased growth velocity followed by achievement of previous growth velocity levels, which can be observed during the follow-up period. Nevertheless, if possible, treatment during pubertal growth spurt should be avoided[36]. In addition, weight loss is very common during the treatment phase; however, most patients experience compensatory weight gain after treatment ends[32]. Regarding quality of life, and behavioral, emotional and cognitive outcomes during and after treatment, no significant impairment has been detected in the PEDS-C trial[37]. More follow-up studies are in progress to evaluate long-term sequelae.
Table 2.
Most frequent adverse events during polyethylene glycol-interferon treatment in combination with ribavirin and its appraisal of clinical significance
| Interferon α-treatment: |
| Leukopenia, thrombocytopenia: Frequent, not really significant; if necessary dose reduction |
| Flu-like symptoms: In all treated patients, not significant |
| Alopecia: Not significant |
| Autoimmune thyroiditis: At least 15 %, significant, mostly reversible |
| Acute psychosis, depression: Very seldom before puberty (< 1 %), rare in adolescents, significant in cases with manifestation; should be under investigation in future trials |
| Growth delay: Clinically not significant, catch-up growth, but under investigation with relative high priority |
| Anorexia, weight loss: Mostly not significant with exceptions, normalisation after therapy stop |
| Ribavirin: |
| Anemia: Mostly clinically not significant with exceptions, reversible |
Most side effects’ intensity is decreasing after some weeks of treatment.
NEW DEVELOPMENTS
There is no doubt that treatment response in patients with genotype 1 is not entirely satisfactory and improved treatment regimens are desirable. A number of directly acting antiviral agents, designed to target viral encoded proteins essential to the HCV life cycle, are currently under development. Phase III trials in adults have been completed for two protease inhibitors (telaprevir and boceprevir) and have shown a significantly increased viral elimination rate in combination with PEG-interferon and ribavirin[38-40]. Brand new data indicate that in a considerable number of patients with rapid response, exposure to PEG-interferon and ribavirin may be shortened and response-guided therapy will become the treatment of choice[41]. Approval of telaprevir and boceprevir has been sanctioned by the FDA and EMA in 2011, and pediatric trials will follow in the near future. In adults, genotype 1 non-responders have also demonstrated SVR rates ranging between 59% and 66%, depending on the duration of boceprevir treatment, compared to 20% with standard of care[42]. Given that efficacy data could be extrapolated from adults to children, an approved triple therapy regimen should be expected for non-responders. Nevertheless, they should definitely be included in future pediatric trials[36].
CONCLUSION
In children and adolescents, PEG-interferon treatment in combination with ribavirin for 48 wk produces a sustained viral response rate in approximately 50% of adequately treated individuals. Thus, this option can be offered to all patients irrespective of the level of aminotransferases or mode of infection. There is evidence that subjects with low viral load may respond better than patients with high viral load. In patients infected with genotype 2 or 3, a 90% or even better SVR rate can be achieved. Thus, treatment for 24 wk should be administered in all patients with genotype 2 and 3. According to the approval of the drugs, treatment start is possible beyond three years of age. However, because spontaneous viral elimination may occur within the first 4-5 years of life in vertically infected individuals, watchful waiting for up to five years of age is a justified alternative to an early treatment start. Additionally, different individual and family variables may influence the appropriate time to initiate therapy. An experienced pediatric gastroenterologist should supervise the management of treating these patients. Mid-childhood age before pubertal growth spurt is preferable. Table 3 summarizes pros and cons to indicate or possibly to defer treatment. Adverse events are usually well tolerated, but severe side effects may occur in a small number of patients making dose adjustment necessary. Overall, the encouraging results, particularly in patients with relatively low viral load and/or favourable genotypes and in line with an appropriate consideration of early stopping rules, endorse application of treatment in eligible patients. Re-treatment in non-responding genotype 1 patients should be deferred until a combination of standard care with direct acting antivirals has become available.
Table 3.
Indication for hepatitis C virus treatment in children-pros and cons
| In favour of treatment | Deferral might be considered |
| High response rate, sustained viral response means cure of the disease | Before 3-4 years of age because of possible spontaneous viral elimination |
| Prevention of disease progression and social burden | Psychiatric disorder |
| Better tolerability and less side effects in younger patients (particularly before puberty) | Low response rate in subjects with genotype 1 and high viral load |
| More favourable factors for response in children (e.g., low viral load) | Pubertal growth spurt |
| Parents facilitate compliance | More effective treatments in future in genotype 1 non-responders |
Footnotes
Peer reviewer: Emanuel K Manesis, MD, Professor of Medicine, Athens University School of Medicine, Liver Unit, Euroclinic, 19 Mavromateon Street, Athens 1034, Greece
S- Editor Zhang SJ L- Editor Logan S E- Editor Zhang DN
References
- 1.Ghany MG, Strader DB, Thomas DL, Seeff LB. Diagnosis, management, and treatment of hepatitis C: an update. Hepatology. 2009;49:1335–1374. doi: 10.1002/hep.22759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mohan N, González-Peralta RP, Fujisawa T, Chang MH, Heller S, Jara P, Kelly D, Mieli-Vergani G, Shah U, Murray KF. Chronic hepatitis C virus infection in children. J Pediatr Gastroenterol Nutr. 2010;50:123–131. doi: 10.1097/MPG.0b013e3181c61995. [DOI] [PubMed] [Google Scholar]
- 3.Jara P, Hierro L. Treatment of hepatitis C in children. Expert Rev Gastroenterol Hepatol. 2010;4:51–61. doi: 10.1586/egh.09.76. [DOI] [PubMed] [Google Scholar]
- 4.Yeung LT, Roberts EA. Current issues in the management of paediatric viral hepatitis. Liver Int. 2010;30:5–18. doi: 10.1111/j.1478-3231.2009.02145.x. [DOI] [PubMed] [Google Scholar]
- 5.Jhaveri R, Grant W, Kauf TL, McHutchison J. The burden of hepatitis C virus infection in children: estimated direct medical costs over a 10-year period. J Pediatr. 2006;148:353–358. doi: 10.1016/j.jpeds.2005.10.031. [DOI] [PubMed] [Google Scholar]
- 6.al-Faleh FZ, Ayoola EA, al-Jeffry M, al-Rashed R, al-Mofarreh M, Arif M, Ramia S, al-Karawi M, al-Shabrawy M. Prevalence of antibody to hepatitis C virus among Saudi Arabian children: a community-based study. Hepatology. 1991;14:215–218. [PubMed] [Google Scholar]
- 7.Gerner P, Wirth S, Wintermeyer P, Walz A, Jenke A. Prevalence of hepatitis C virus infection in children admitted to an urban hospital. J Infect. 2006;52:305–308. doi: 10.1016/j.jinf.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 8.el-Nanawy AA, el Azzouni OF, Soliman AT, Amer AE, Demian RS, el-Sayed HM. Prevalence of hepatitis-C antibody seropositivity in healthy Egyptian children and four high risk groups. J Trop Pediatr. 1995;41:341–343. doi: 10.1093/tropej/41.6.341. [DOI] [PubMed] [Google Scholar]
- 9.Yeung LT, King SM, Roberts EA. Mother-to-infant transmission of hepatitis C virus. Hepatology. 2001;34:223–229. doi: 10.1053/jhep.2001.25885. [DOI] [PubMed] [Google Scholar]
- 10.Tovo PA, Pembrey LJ, Newell ML. Persistence rate and progression of vertically acquired hepatitis C infection. European Paediatric Hepatitis C Virus Infection. J Infect Dis. 2000;181:419–424. doi: 10.1086/315264. [DOI] [PubMed] [Google Scholar]
- 11.Nydegger A, Srivastava A, Wake M, Smith AL, Hardikar W. Health-related quality of life in children with hepatitis C acquired in the first year of life. J Gastroenterol Hepatol. 2008;23:226–230. doi: 10.1111/j.1440-1746.2007.04859.x. [DOI] [PubMed] [Google Scholar]
- 12.Rodrigue JR, Balistreri W, Haber B, Jonas MM, Mohan P, Molleston JP, Murray KF, Narkewicz MR, Rosenthal P, Smith LJ, et al. Impact of hepatitis C virus infection on children and their caregivers: quality of life, cognitive, and emotional outcomes. J Pediatr Gastroenterol Nutr. 2009;48:341–347. doi: 10.1097/MPG.0b013e318185998f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bortolotti F, Verucchi G, Cammà C, Cabibbo G, Zancan L, Indolfi G, Giacchino R, Marcellini M, Marazzi MG, Barbera C, et al. Long-term course of chronic hepatitis C in children: from viral clearance to end-stage liver disease. Gastroenterology. 2008;134:1900–1907. doi: 10.1053/j.gastro.2008.02.082. [DOI] [PubMed] [Google Scholar]
- 14.Iorio R, Giannattasio A, Sepe A, Terracciano LM, Vecchione R, Vegnente A. Chronic hepatitis C in childhood: an 18-year experience. Clin Infect Dis. 2005;41:1431–1437. doi: 10.1086/497141. [DOI] [PubMed] [Google Scholar]
- 15.Vogt M, Lang T, Frösner G, Klingler C, Sendl AF, Zeller A, Wiebecke B, Langer B, Meisner H, Hess J. Prevalence and clinical outcome of hepatitis C infection in children who underwent cardiac surgery before the implementation of blood-donor screening. N Engl J Med. 1999;341:866–870. doi: 10.1056/NEJM199909163411202. [DOI] [PubMed] [Google Scholar]
- 16.Posthouwer D, Fischer K, van Erpecum KJ, Mauser-Bunschoten EP. The natural history of childhood-acquired hepatitis C infection in patients with inherited bleeding disorders. Transfusion. 2006;46:1360–1366. doi: 10.1111/j.1537-2995.2006.00903.x. [DOI] [PubMed] [Google Scholar]
- 17.European Paediatric Hepatitis C Virus Network. Three broad modalities in the natural history of vertically acquired hepatitis C virus infection. Clin Infect Dis. 2005;41:45–51. doi: 10.1086/430601. [DOI] [PubMed] [Google Scholar]
- 18.Resti M, Jara P, Hierro L, Azzari C, Giacchino R, Zuin G, Zancan L, Pedditzi S, Bortolotti F. Clinical features and progression of perinatally acquired hepatitis C virus infection. J Med Virol. 2003;70:373–377. doi: 10.1002/jmv.10405. [DOI] [PubMed] [Google Scholar]
- 19.Goodman ZD, Makhlouf HR, Liu L, Balistreri W, Gonzalez-Peralta RP, Haber B, Jonas MM, Mohan P, Molleston JP, Murray KF, et al. Pathology of chronic hepatitis C in children: liver biopsy findings in the Peds-C Trial. Hepatology. 2008;47:836–843. doi: 10.1002/hep.22094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guido M, Bortolotti F, Leandro G, Jara P, Hierro L, Larrauri J, Barbera C, Giacchino R, Zancan L, Balli F, et al. Fibrosis in chronic hepatitis C acquired in infancy: is it only a matter of time? Am J Gastroenterol. 2003;98:660–663. doi: 10.1111/j.1572-0241.2003.07293.x. [DOI] [PubMed] [Google Scholar]
- 21.Cesaro S, Bortolotti F, Petris MG, Brugiolo A, Guido M, Carli M. An updated follow-up of chronic hepatitis C after three decades of observation in pediatric patients cured of malignancy. Pediatr Blood Cancer. 2010;55:108–112. doi: 10.1002/pbc.22438. [DOI] [PubMed] [Google Scholar]
- 22.Bochud PY, Cai T, Overbeck K, Bochud M, Dufour JF, Müllhaupt B, Borovicka J, Heim M, Moradpour D, Cerny A, et al. Genotype 3 is associated with accelerated fibrosis progression in chronic hepatitis C. J Hepatol. 2009;51:655–666. doi: 10.1016/j.jhep.2009.05.016. [DOI] [PubMed] [Google Scholar]
- 23.Barshes NR, Udell IW, Lee TC, O’Mahony CA, Karpen SJ, Carter BA, Goss JA. The natural history of hepatitis C virus in pediatric liver transplant recipients. Liver Transpl. 2006;12:1119–1123. doi: 10.1002/lt.20793. [DOI] [PubMed] [Google Scholar]
- 24.Bortolotti F, Giacchino R, Vajro P, Barbera C, Crivellaro C, Alberti A, Nebbia G, Zancan L, De Moliner L, Bertolini A. Recombinant interferon-alfa therapy in children with chronic hepatitis C. Hepatology. 1995;22:1623–1627. [PubMed] [Google Scholar]
- 25.Christensson B, Wiebe T, Akesson A, Widell A. Interferon-alpha and ribavirin treatment of hepatitis C in children with malignancy in remission. Clin Infect Dis. 2000;30:585–586. doi: 10.1086/313709. [DOI] [PubMed] [Google Scholar]
- 26.González-Peralta RP, Kelly DA, Haber B, Molleston J, Murray KF, Jonas MM, Shelton M, Mieli-Vergani G, Lurie Y, Martin S, et al. Interferon alfa-2b in combination with ribavirin for the treatment of chronic hepatitis C in children: efficacy, safety, and pharmacokinetics. Hepatology. 2005;42:1010–1018. doi: 10.1002/hep.20884. [DOI] [PubMed] [Google Scholar]
- 27.Schwarz KB, Gonzalez-Peralta RP, Murray KF, Molleston JP, Haber BA, Jonas MM, Rosenthal P, Mohan P, Balistreri WF, Narkewicz MR, et al. The combination of ribavirin and peginterferon is superior to peginterferon and placebo for children and adolescents with chronic hepatitis C. Gastroenterology. 2011;140:450–458.e1. doi: 10.1053/j.gastro.2010.10.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jara P, Hierro L, de la Vega A, Díaz C, Camarena C, Frauca E, Miños-Bartolo G, Díez-Dorado R, de Guevara CL, Larrauri J, et al. Efficacy and safety of peginterferon-alpha2b and ribavirin combination therapy in children with chronic hepatitis C infection. Pediatr Infect Dis J. 2008;27:142–148. doi: 10.1097/INF.0b013e318159836c. [DOI] [PubMed] [Google Scholar]
- 29.Baker RD, Dee D, Baker SS. Response to pegylated interferon alpha-2b and ribavirin in children with chronic hepatitis C. J Clin Gastroenterol. 2007;41:111–114. doi: 10.1097/MCG.0b013e31802dd2f6. [DOI] [PubMed] [Google Scholar]
- 30.Sokal EM, Bourgois A, Stéphenne X, Silveira T, Porta G, Gardovska D, Fischler B, Kelly D. Peginterferon alfa-2a plus ribavirin for chronic hepatitis C virus infection in children and adolescents. J Hepatol. 2010;52:827–831. doi: 10.1016/j.jhep.2010.01.028. [DOI] [PubMed] [Google Scholar]
- 31.Wirth S, Pieper-Boustani H, Lang T, Ballauff A, Kullmer U, Gerner P, Wintermeyer P, Jenke A. Peginterferon alfa-2b plus ribavirin treatment in children and adolescents with chronic hepatitis C. Hepatology. 2005;41:1013–1018. doi: 10.1002/hep.20661. [DOI] [PubMed] [Google Scholar]
- 32.Wirth S, Ribes-Koninckx C, Calzado MA, Bortolotti F, Zancan L, Jara P, Shelton M, Kerkar N, Galoppo M, Pedreira A, et al. High sustained virologic response rates in children with chronic hepatitis C receiving peginterferon alfa-2b plus ribavirin. J Hepatol. 2010;52:501–507. doi: 10.1016/j.jhep.2010.01.016. [DOI] [PubMed] [Google Scholar]
- 33.Tajiri H, Inui A, Kiyohara Y, Suzuki M, Kagimoto S, Etani Y, Shimizu T, Fujisawa T. Peginterferon alpha-2b and ribavirin for the treatment of chronic hepatitis C in Japanese pediatric and young adult patients: a survey of the Japan Society of Pediatric Hepatology. Eur J Gastroenterol Hepatol. 2009;21:1256–1260. doi: 10.1097/MEG.0b013e32832a4e97. [DOI] [PubMed] [Google Scholar]
- 34.Gerner P, Hilbich J, Wenzl TG, Behrens R, Walther F, Kliemann G, Enninger A, Wirth S. Re-treatment of children with chronic hepatitis C who did not respond to interferon-alpha treatment. J Pediatr Gastroenterol Nutr. 2010;51:187–190. doi: 10.1097/MPG.0b013e3181d9c7f6. [DOI] [PubMed] [Google Scholar]
- 35.Wirth S, Lang T, Gehring S, Gerner P. Recombinant alfa-interferon plus ribavirin therapy in children and adolescents with chronic hepatitis C. Hepatology. 2002;36:1280–1284. doi: 10.1053/jhep.2002.36495. [DOI] [PubMed] [Google Scholar]
- 36.Wirth S, Kelly D, Sokal E, Socha P, Mieli-Vergani G, Dhawan A, Lacaille F, Saint Raymond A, Olivier S, Taminiau J. Guidance for clinical trials for children and adolescents with chronic hepatitis C. J Pediatr Gastroenterol Nutr. 2011;52:233–237. doi: 10.1097/MPG.0b013e3181f6f09c. [DOI] [PubMed] [Google Scholar]
- 37.Rodrigue JR, Balistreri W, Haber B, Jonas MM, Mohan P, Molleston JP, Murray KF, Narkewicz MR, Rosenthal P, Smith LJ, et al. Peginterferon with or without ribavirin has minimal effect on quality of life, behavioral/emotional, and cognitive outcomes in children. Hepatology. 2011;53:1468–1475. doi: 10.1002/hep.24248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McHutchison JG, Everson GT, Gordon SC, Jacobson IM, Sulkowski M, Kauffman R, McNair L, Alam J, Muir AJ. Telaprevir with peginterferon and ribavirin for chronic HCV genotype 1 infection. N Engl J Med. 2009;360:1827–1838. doi: 10.1056/NEJMoa0806104. [DOI] [PubMed] [Google Scholar]
- 39.Kwo PY, Lawitz EJ, McCone J, Schiff ER, Vierling JM, Pound D, Davis MN, Galati JS, Gordon SC, Ravendhran N, et al. Efficacy of boceprevir, an NS3 protease inhibitor, in combination with peginterferon alfa-2b and ribavirin in treatment-naive patients with genotype 1 hepatitis C infection (SPRINT-1): an open-label, randomised, multicentre phase 2 trial. Lancet. 2010;376:705–716. doi: 10.1016/S0140-6736(10)60934-8. [DOI] [PubMed] [Google Scholar]
- 40.Poordad F, McCone J, Bacon BR, Bruno S, Manns MP, Sulkowski MS, Jacobson IM, Reddy KR, Goodman ZD, Boparai N, et al. Boceprevir for untreated chronic HCV genotype 1 infection. N Engl J Med. 2011;364:1195–1206. doi: 10.1056/NEJMoa1010494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jacobson IM, McHutchison JG, Dusheiko G, Di Bisceglie AM, Reddy KR, Bzowej NH, Marcellin P, Muir AJ, Ferenci P, Flisiak R, et al. Telaprevir for previously untreated chronic hepatitis C virus infection. N Engl J Med. 2011;364:2405–2416. doi: 10.1056/NEJMoa1012912. [DOI] [PubMed] [Google Scholar]
- 42.Bacon BR, Gordon SC, Lawitz E, Marcellin P, Vierling JM, Zeuzem S, Poordad F, Goodman ZD, Sings HL, Boparai N, et al. Boceprevir for previously treated chronic HCV genotype 1 infection. N Engl J Med. 2011;364:1207–1217. doi: 10.1056/NEJMoa1009482. [DOI] [PMC free article] [PubMed] [Google Scholar]


