Abstract
Background and Objectives
The incidence of inflammatory heart diseases is not yet as high as those of other cardiovascular diseases; however, inflammatory heart diseases do have relatively high mortality rate. Therefore, update information on the economic burden of inflammatory heart diseases are necessary in order to appropriate policy making on these diseases.
Materials and Methods
This study used a number of resources to obtain data, national health insurance statistics, the Korean Health Panel, and the causes of death report by the Korean National Statistical Office. The total costs of inflammatory heart diseases were estimated as the sum of direct medical care costs, direct non-medical care and indirect costs.
Results
The total direct cost of inflammatory heart disease was higher in Korean men than that of Korean women and cost due to inpatient was higher than that of outpatients cost. The costs to cover premature death were highest among all of the components used to determine the total costs for inflammatory heart disease, representing 66.3% of these costs in Korea.
Conclusion
Inflammatory heart disease has a relatively high mortality rate, and the costs that are associated with premature deaths consume the greatest proportion of the costs associated with this disease. In spite of some limitations of study, this could be a reliable evidence of economic burden of inflammatory heart disease.
Keywords: Inflammation, Cost of illness, Endocarditis
Introduction
Inflammatory heart diseases are caused by heart inflammation or muscle failure that may result from a diverse number of reasons.1) Pericarditis, endocarditis, myocarditis, and cardiomyopathy are classified as inflammatory heart diseases. Inflammatory heart diseases do not yet make up a large proportion of the total heart diseases. Mortality due to cardiovascular disease is mainly a result of having coronary heart disease in addition to a cerebrovascular disease. The Korean mortality rate of all cardiovascular diseases in 2004 was 169.9 people per 100,000, and that of inflammatory heart disease was 2.0 people per 100,000. However, the mortality rate of inflammatory heart disease was 11.4 per 100,000 people in the United States of America (USA), 9.7 in France, 5.5 in China, and 5.1 in Japan, all of which are higher than that reported in Korea. Thus, there is a high probability that the death rate in Korea will increase in the future.2),3)
The severity of inflammatory heart disease seems high compared to the mortality rate. For example, myocarditis is a potentially life-threatening disease, the acute form of which is treatable but can progress to chronic myocarditis or dilated cardiomyopathy (DCM) in cases of severe inflammation that may then result in congestive heart failure. Myocarditis also causes sudden death among young adults.4-6)
Therefore, the economic burden of inflammatory heart disease is thought to be quite high, although no exact measures have been made. According to the 2004 World health organization (WHO) report, Korea's Disability Adjusted Life Years (DALY) on cardiovascular disease was estimated to be 1,277 (per 100,000 population), while the DALY on inflammatory heart disease was estimated to be 28 (per 100,000 population).2) However, Korea does not have estimates on any of the groups of cardiovascular disease. As a result, we used various sources of data in this study to determine the economic burdens of inflammatory heart disease so that the costs could be expressed as in currency value.
Materials and Methods
In this study, we measured the economic costs of inflammatory heart disease using a prevalence rate approach. We did not separate the existing inflammatory heart disease patients from the newly affected patients of 2008 in our study. We calculated the medical costs paid by Korean society as a result of these patients.
We used the precedent study by Jung and Ko7) as a guide to measure socioeconomic costs, based on both direct and indirect costs.8) The direct costs for medical treatment included medical non-medical care costs. Direct medical care costs included inpatient and outpatient expenses that are paid by the insurer, medical treatment costs that are paid by the patients, non-covered care costs such as meals, high-end ward and special care costs, and prescribed pharmaceutical costs. As for the direct non-medical costs, transportation fees needed to get to the hospital, admission fees and the cost of having a caregiver were all considered. Indirect costs factor in lost productivity, which refers to the opportunity costs resulting from hospital visits, the costs of admission, and the costs of premature death.
We can also account for the costs of over-the-counter drugs and out-of-pocket expenses (e.g., child care and home aids). However, we excluded the costs of over-the-counter drugs and out-of-pocket expenses due to objectivity reasons because not much data exists with regard to these are out-of-pocket expenses.
In this study, we defined inflammatory heart disease according to the International Classification of Disease 10th version (ICD-10) codes I30-I32 (pericarditis), I33 (acute and subacute endocarditis), I38 (endocarditis, valve unspecified), I40 (acute myocarditis) and I42 (cardiomyopathy).2),9) The classifications followed the global burden of disease study of WHO.2) We used the claim records from the Korean National Health Insurance Corporation (NHIC) to collect related data on inflammatory heart disease medical usage in order to calculate the total cost and the average cost per patient. We defined patients with inflammatory heart disease as individuals who were diagnosed by a physician or those for whom the hospital had submitted a 2008 claim to the NHIC that had stated inflammatory heart disease as the primary disease.
The direct costs include the total expenses of both inpatients and outpatients throughout the year paid to treat the specified diseases, which in our study were the diseases defined as the major claim codes I30-33, I38, I40, and I42. Non-covered service expenses were calculated using the NHIC data, which includes the survey data of non-covered care costs for every patient in 2008 and is based on the non-covered cost rate of the total expense. The cost rate of inpatients was 29.3% and that of outpatients was 40.2%.10-12)As for estimating the pharmaceutical costs, the average rate of pharmaceutical cost among insurance benefit in cardiovascular diseases (ischemic heart disease, cerebrovascular disease, rheumatic heart disease, hypertensive disease) was applied.13) The total cost of annual transportation related to the treatment of inflammatory heart diseases was estimated by multiplying the number of visits (outpatient, emergency room, and inpatient) by the cost of transportation.
The average cost for visiting a hospital was estimated at ₩7,597 per one-way trip for inpatients and ₩777 per one-way trip for outpatients, based on the results of the 2008 Korean Medical Expenditure Survey. The equations used to calculate these values are listed below.14)
Transportation costs of inpatients=the number of total inpatient visits×average one-way trip cost×2 (round trip)
Transportation costs of outpatients=the number of total outpatient visits×average one-way trip cost×2 (round trip)
We informally calculated the average cost of having a caregiver since there were no officially published figures. In Korea, the care of inpatients is almost exclusively performed by a female family member between the ages of 20 to 60 of age. As a result, the total number of days a patient was admitted was multiplied by the average daily wage of Korean females be-tween the ages of 20 and 60 years.15) Indirect costs were determined by calculating the premature death costs and the costs that result from productivity loss due to hospitalization or clinic visits. In regard to the productivity loss of inpatients, we used the average working hours per month and the average wage per month based on an informed 2008 survey to adjust for age, working conditions and type of employment 2008. We did not calculate productivity loss for patients who were not of working age, which in our study were defined as children and teenagers (1-19 years old) and older adults (over 70 years of age).15)
In order to calculate the costs associated with productivity lost in outpatients, we used the average patient visit time, which was calculated by multiplying the average time spent during outpatient visits by the number of days the outpatient would visit the hospital. The average patient visit time was estimated to be 1/3 of days, which was assumed to include time spent travelling to the appointment, and was assumed to consume one-third of a patient's daily working hours.
To estimate the loss of expenditure caused by premature death, we determined the number of deaths that were due to inflammatory heart disease using the cause of death statistics,16) and we also converted the future incomes of the dead patients to their current values by adjusting for age. As we previously mentioned, we also factored in the average number of working hours and wages per month.
Results
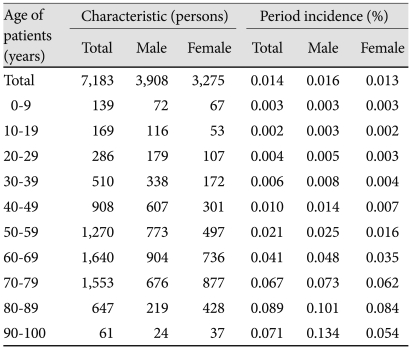
Table 1 presents the distribution of inflammatory heart disease in Korea. The incidence rate of inflammatory heart disease in 2008 was 0.016% in male patients and 0.013% in female patients. There were no gender-related differences in the incidence rate of adolescents less than 20 years of age. However, the incidence rate of males was observed to be higher than that of females when the age group was restricted to the upper twenties. The total number of visits that outpatients had visited was 73,529, in which men were admitted 42,000 days and women 31,529 days. As for inpatients, men were admitted for a total of 3,927 days and women were admitted for a total of 3,330 days, thus showing that men were admitted more often than women.
Table 1.
Incidences of inflammatory heart disease in males, females, and total patients (2008)
Direct costs
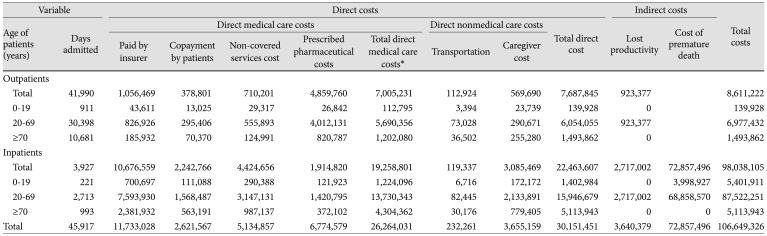
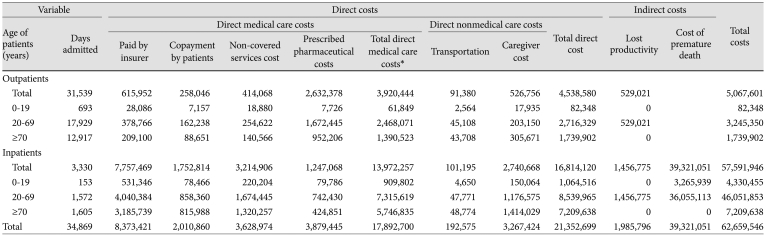
The total direct costs of inflammatory heart disease were higher in men than in women. The total direct medical care costs of male outpatients were ₩7,005,231,000, and those of male inpatients were ₩19,258,801,000. The total direct costs of female outpatients were ₩3,920,444,000 and those of female inpatients were ₩13,972,257,000. When categorized according to age, infant and adolescent outpatients and inpatients had the lowest cost, regardless of sex, while adults had the highest cost (Table 2 and 3).
Table 2.
Direct and indirect economic burdens of inflammatory heart diseases in male patients
Expressed as thousand won. *Sum of costs paid by insurer+copayment by patients+non-covered services cost+prescribed pharmaceutical costs
Table 3.
Direct and indirect economic burdens of inflammatory heart diseases in female patients
Expressed as thousand won. *Sum of costs paid by insurer+copayment by patients+non-covered services cost+prescribed pharmaceutical costs
Direct medical care costs
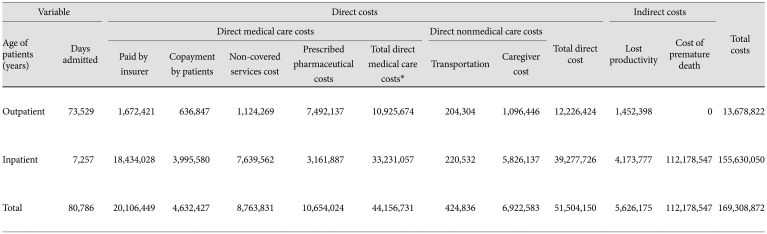
Total direct medical care costs were calculated to be ₩44,156,731,000 (Table 4). Of this amount, 45.5% was paid by the insurer, 10.5% was paid in the form of patient copayments, 19.8% was non-covered care cost and 24.1% was prescribed pharmaceutical costs. In the both cases of outpatients and inpatients, the total direct medical care costs of male were higher than those of females. But women over the age of 70, where the costs of outpatients were ₩1,390,523,000 and those of inpatients were ₩5,746,835,000, higher than those calculated for both male outpatients and inpatients (₩1,202,080,000 and ₩4,304,362,000, respectively) (Table 2 and 3). Among the costs of outpatients, the prescribed pharmaceutical costs occupied more than half of total medical cost (68.6%), but in the case of inpatients, the payment by insurer ranked the first among cost components (55.5%).
Table 4.
Direct and indirect economic burdens of inflammatory heart diseases
*Sum of costs paid by insurer+copayment by patients+noncovered services cost+prescribed pharmaceuticals
Direct nonmedical costs
The transportation fees used for hospital visits of outpatients were approximately ₩204,304,000, while those of inpatients were approximately ₩220,532,000. The outpatient cost of having a caregiver was ₩1,096,446,000, and that of inpatients was ₩5,826,137,000. The total direct nonmedical costs were ₩7,347,419,000, 14.3% of the total direct costs (Table 4).
Indirect costs
The productivity loss due to outpatient hospital visits was ₩923,377,000 for men and ₩529,021,000 for women, which was determined using the average salary per day. In cases of hospitalization, the costs for men were ₩2,717,002,000 and those for women were ₩1,456,775,000. The costs resulting from premature death were ₩72,857,496,000 for men and ₩39,321,051,000 for women, which when combined come to a total of ₩112,178,547,000. As a result, the total indirect costs due to both productivity loss and premature death were ₩164,599,010,000 (Table 4).
Discussion
This study made use of NHIC claims records to measure the medical usage and the social economic burden that results from inflammatory heart disease in Korea. According to the results, the 2008 economic burden of inflammatory heart disease was approximately 169.4 billion won, including both the direct and indirect costs. This result is bigger than the cost of bladder cancer, which is 104.5 billion won, based on a study by Kim et al.17) Comparing the present study with the one by Kim et al. one difference is that their study also considered complementary and alternative medicine costs when measuring the economic burden.
In this study, as mentioned in the results, of the ₩44,156, 731,000 total direct medical care costs, the amount paid by the insurer accounted for the largest percentage, 45.5% (₩20,106,449,000). The sum of the direct costs and the indirect costs was higher in men than in women. But the group of aged 70 and more, the direct medical cost in female group was higher than those of male group. Because the incidence of inflammatory heart disease is higher in male even the aged group, the longer life expectancy of female may attribute the higher economic burden of old female group.
Considering the levels of contribution for each category of burden of disease, the costs for premature death were highest at 66.3%, followed by the amount paid by the insurer at 11.8%, prescribed pharmaceutical costs at 6.3%, the costs of non-covered services at 5.2%, the costs of having a caregiver at 4.1%, the costs associated with the loss of productivity at 3.3%, copayments that are paid by the patients at 2.7%, and the costs of transportation fees at 0.3%. Indirect cost, especially the cost due to premature death occupies more than half of total economic burden of inflammatory heart disease in this study. Therefore it is justifiable to invest drastically to prevent the disability and mortality due to inflammatory heart disease. For example, future research and investment on treatment to minimize the mortality will be needed.
This study has some limitations. First, the range of inflammatory heart diseases could have been defined differently. We selected and thereby limited the disease codes to I30-33, I38, I40, and I42 according to the ICD-10 according to the definition of global burden of disease study of WHO. This includes the cardiomyopathy, myocarditis, non-tuberculosis pericarditis and endocarditis.2),9) But the definition of inflammatory heart disease could be debated. For example, the hypertrophic cardiomyopathy among cardiomyopathy could be genetic disease.18) Also acute endocarditis could result from infectious agent rather than self-inflammation. Therefore the trend of cost in endocarditis could differ by the reason. But in this study, we followed the classification of WHO to increase the comparability of other burden of disease study. The estimate of burden of disease could be changed with definition. For example, if atherosclerosis was included according to World Heart Federation, then the economic burden of inflammatory heart disease would have been even higher.19)
Secondly, according to the study by Ariza et al.20) which focuses on the economic consequences of diabetes and cardiovascular disease in the USA, cardiovascular disease is a major complication of diabetes. The cost of diabetes-related care accounts for a considerable portion of the health care expenditure in the USA. This means there is a possibility that inflammatory heart disease from complication and primarily developed diabetes could have been measured together or omitted. We need to continue to address this problem in future studies.
Despite these limitations, this study calculated the economic burden of inflammatory heart disease in Korea using the claim records of NHIC which is a national representative. This could be an evidence of economic burden of inflammatory heart disease in Korea and could attribute an evidence base policy making for manage inflammatory heart diseases.
Acknowledgments
This research was supported by a fund (code R1006511) by Research of Korea Centers for Disease Control and Prevention.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Fairweather D, Rose NR. Inflammatory heart disease: a role for cytokines. Lupus. 2005;14:646–651. doi: 10.1191/0961203305lu2192oa. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Geneva: World Health Organization; [cited 2009 Feb 20]. The global burden of disease: 2004 update [Internet] Available from: http://www.who.int/healthinfo/global_burden_disease/estimates_regional/en/index.html. [Google Scholar]
- 3.Hufnagel G, Pankuweit S, Richter A, Schönian U, Maisch B. The European Study of Epidemiology and Treatment of Cardiac Inflammatory Diseases (ESETCID)-first epidemiological results. Herz. 2000;25:279–285. doi: 10.1007/s000590050021. [DOI] [PubMed] [Google Scholar]
- 4.Dec GW. Introduction to clinical myocarditis. In: Cooper LT, editor. Myocarditis: from bench to bedside. New Jersey: Human Press; 2003. pp. 257–281. [Google Scholar]
- 5.Drory Y, Turetz Y, Hiss Y, et al. Sudden unexpected death in persons less than 40 years of age. Am J Cardiol. 1991;68:1388–1392. doi: 10.1016/0002-9149(91)90251-f. [DOI] [PubMed] [Google Scholar]
- 6.Blauwet LA, Cooper LT. Myocarditis. Prog Cardiovasc Dis. 2010;52:274–288. doi: 10.1016/j.pcad.2009.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jung YH, Ko SJ. Estimating socioeconomic costs of five major diseases. Public Finance Revi. 2004;18:77–104. [Google Scholar]
- 8.Kim SY, Yoon SJ, Jo MW, Kim EJ, Kim HJ, Oh IH. Economic burden of allergic rhinitis in Korea. Am J Rhinol Allergy. 2010;24:e110–e113. doi: 10.2500/ajra.2010.24.3513. [DOI] [PubMed] [Google Scholar]
- 9.Mathers CD, Vos T, Lopez AD, Salomon J, Ezzati M. National Burden of Disease Studies: a Practical Guide. 2nd ed. Geneva: World Health Organization; 2001. [Google Scholar]
- 10.National Health Insurance Corporation. National Health Insurance Statistical Yearbook. Seoul: National Health Insurance Corp; 2007. pp. 488–489. [Google Scholar]
- 11.Park BH, Lee TJ, Lim WY. Incidence and magnitude of out-of-pocket payment and factors influencing them in Industrial Accident Compensation Insurance. Korean J Health Policy Adm. 2010;20:103–124. [Google Scholar]
- 12.Kim JH, Jung JC, Lee HY, Choi SJ, Lee JK. Survey on the Benefit Coverage Rate of National Health Insurance in 2005. Seoul: National Health Insurance Corp; 2006. Results of survey on medical care cost by patient; pp. 131–138. [Google Scholar]
- 13.Yoon SJ, Kim EJ, Kim HJ, Oh Ih, Seo HY. A study on measuring the economic burden of cardio-cerebrovasucular disease in Korea. Seoul: Korea Centers for Disease Control and Prevention; 2011. [Google Scholar]
- 14.Korea Institute for Health and Social Affairs and National Health Insurance Corporation. Korea Health Panel [Internet] Seoul: Korea Institute for Health and Social Affairs and National Health Insurance corporation; [Cited 2011 Jan 4]. Available from: http://www.khp.re.kr. [Google Scholar]
- 15.Ministry of Labor[Internet] Ministry of Labor; [cited 2011 Jan 4]. Survey Report on Wage Structure in 2008. Available from: http://www.laborstatmolab.go.kr. [Google Scholar]
- 16.National Statistical Office. The Cause of Death Statistics of 2008. Seoul: 2009. [Google Scholar]
- 17.Kim J, Hahm MI, Park EC, et al. Economic burden of cancer in South Korea for the year 2005. J Prev Med Public Health. 2009;42:190–198. doi: 10.3961/jpmph.2009.42.3.190. [DOI] [PubMed] [Google Scholar]
- 18.Maron BJ. Hypertrophic cardiomyopathy: a systematic review. JAMA. 2002;287:1308–1320. doi: 10.1001/jama.287.10.1308. [DOI] [PubMed] [Google Scholar]
- 19.World Heart Federation: different heart diseases [Internet] Geneva: World Heart Federation; [cited 2011 Jan 4]. Available from: http://www.worldheart.org. [Google Scholar]
- 20.Ariza MA, Vimalananda VG, Rosenzweig JL. The economic consequences of diabetes and cardiovascular disease in the United States. Rev Endocr Metab Disord. 2010;11:1–10. doi: 10.1007/s11154-010-9128-2. [DOI] [PubMed] [Google Scholar]