Abstract
Ralph Steinman, an editor at the Journal of Experimental Medicine since 1978, shared the 2011 Nobel Prize in Physiology or Medicine for his discovery of dendritic cells (DCs) and their role in immunity. Ralph never knew. He died of pancreatic cancer on September 30, 3 days before the Nobel announcement. Unaware of his death at the time of their announcement, the Nobel Committee made the unprecedented decision that his award would stand. Ralph was the consummate physician-scientist to the end. After his diagnosis, he actively participated in his 4.5 years of treatments, creating experimental therapies using his own DCs in conjunction with the therapies devised by his physicians, all the while traveling, lecturing, and most of all pursuing new investigations in his laboratory. For 38 years—from his discovery of DCs to his Nobel Prize—Ralph pioneered the criteria and methods used to identify, isolate, grow, and study DCs. He and his colleagues demonstrated that DCs are initiators of immunity and regulators of tolerance. In his most recent studies, Ralph was harnessing the specialized features of DCs to design improved vaccines. The following synopsis describes some of his seminal discoveries.
Until Ralph Steinman discovered DCs, the innate and adaptive systems had been considered separate entities for nearly a century. Innate immunity involved Elie Metchnikoff’s phagocytes, particularly macrophages that internalize and kill microbes. Paul Ehrlich’s adaptive immunity involved lymphocytes that produce the antibodies that are so often used for clinical benefit. A new dimension to Ehrlich’s work was first described in the 1940s by Merrill Chase, a researcher at the Rockefeller Institute who showed that lymphocytes, rather than antibodies, bring about adaptive immunity. It is now known that this cell-mediated immunity involves T lymphocytes in many different helper, cytotoxic, and suppressor forms, and that they are all controlled by DCs. Ralph’s discovery thus provided the missing link between innate and adaptive immunity. DCs are essential for understanding how the immune system works during health and how diseases develop. They are unavoidable targets for identifying new preventions and therapies.
Discovery
During his medical training, Ralph was challenged to learn how an antigen provokes an immune response. He recognized that MacFarlane Burnet’s clonal selection theory could not account for how the body responds to substances—both foreign and self—by generating a diverse repertoire of immune cells, each with a single, distinct antibody as its receptor (Burnet, 1957). Because clonal selection could not be initiated by adding foreign proteins to lymphocytes, it was thought that mysterious “accessory” cells were also required to induce immunity. One idea was that accessory cells were macrophages.
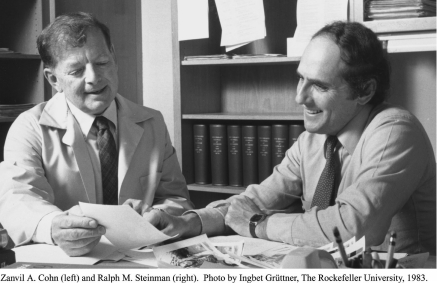
The story of DCs began in 1970, when Ralph joined the Rockefeller University as a postdoctoral fellow in the laboratory of Zanvil (Zan) Cohn, the founder of modern macrophage biology. This was an ideal place to directly test whether macrophages would trap intact antigens and present them to lymphocytes. The laboratory was founded by the premier microbiologist René Dubos, who recognized the need to study the host during infection. He had been the ideal mentor for James Hirsch and Zan, two physicians devoted to infectious disease, who pursued elegant careers with phagocytes. Dubos, Hirsch, and Cohn were all editors of this journal.
Ralph’s initial research focused on endocytosis of proteins in macrophages. But when he was unable to find reservoirs of intact antigen on peritoneal macrophages, he turned to the spleen to see if this organ might harbor cells responsible for generating immunity (Steinman and Cohn, 1972).
Ralph and Zan discovered DCs in 1973. Looking through a phase contrast microscope, they encountered a population of cells from the spleen that had never been seen before and did not look like macrophages. The cells were elongated with unusual stellate, or treelike, processes that were constantly forming and retracting. Ralph named them dendritic cells (from the Greek word dendreon for tree; Steinman and Cohn, 1973, 1974).
Purification
It took nearly 5 years to get pure populations of DCs and to compare their functions with those of other cell types. DCs were rare (<1% of mouse spleen cells), and their only unique markers were their unusual shape and movement. Fortunately, George Palade, Phil Siekevitz, David Sabatini, Günter Blobel, and Christian de Duve—who were in the process of inventing modern cell biology—were neighbors of the Cohn laboratory in Rockefeller’s Bronk Building. The de Duve laboratory’s expertise in density gradient centrifugation for subcellular fractionation was key to Ralph’s purification methods. The elegant and ingenious steps Ralph worked out started with centrifuging spleen cells on a bovine serum albumin gradient, on which semipurified DCs rose to the top. He then placed this fraction on glass for one hour, delicately washed away all but the DCs and some macrophages, and cultured these cells overnight to let the DCs detach from the culture dish and float into suspension. The lingering few macrophages were removed by adding antibody-coated sheep red blood cells and centrifuging them out (Steinman et al., 1979). This procedure was laborious, and the DC yield was poor. As a result, few laboratories attempted to reproduce it or to work with DCs for many years. After an antibody was developed to CD11c, an antigen expressed by DCs, activated monocytes, and NK cells, purification became routine (Metlay et al., 1990).
Mixed leukocyte reaction
Functional studies on DCs began once Ralph had pure DC populations. He noted that DCs expressed high levels of MHC proteins. Therefore, along with Maggi Witmer-Pack, he evaluated their capacity to stimulate the mixed leukocyte reaction (MLR). This T cell reaction had been used for 15 years to detect differences in MHC antigens between potential donors and recipients of organ transplants. At the time, it was termed mixed lymphocyte reaction because it was thought that B cells from the potential transplant donor triggered the division of T cells of the potential transplant recipient. Ralph showed that the newly identified DCs were 100 times more potent than bulk spleen cells at inciting the MLR, and that antigen-bearing B cells and macrophages contributed little to initiating the reaction. The DCs were converting transplantation antigens into “immunogens” capable of eliciting cell and organ rejection. In 1978, Ralph predicted that DCs would “prove to be a critical accessory cell required in the generation of many immune responses” (Steinman and Witmer, 1978). However, this interpretation was not accepted by most immunologists because of the unusual features of the MLR in comparison to other immune responses. For example, the antigens responsible for initiating the MLR were not well defined, and vigorous in vitro responses apparently required no priming.
Antigen presentation
The next few years were very productive, and DCs were quickly shown to effectively present antigens to T cells. Michel Nussenzweig, the first student to work on DCs, showed that DCs capture antigens and present them to cytolytic T lymphocytes. Michel modified syngeneic thymocytes with trinitrophenyl and showed that DCs could capture, process, and present the antigen to produce MHC-restricted cytolytic T lymphocytes (Nussenzweig et al., 1980). Michel also developed 33D1, the first DC-specific monoclonal antibody (Nussenzweig et al., 1982). Although 20 years passed before the antigen recognized by 33D1 was characterized at the molecular level (Dudziak et al., 2007), 33D1 was important because it revealed the first molecular distinction between DCs and all other immune cell types. Michel and Ralph used this monoclonal antibody to selectively deplete DCs, but not monocytes, from spleen suspensions to show that the DC was the primary stimulator of the MLR in bulk spleen (Steinman et al., 1983).
Another student, Wes van Voorhis, identified DCs in human blood (Van Voorhis et al., 1982) and developed a monoclonal antibody that killed monocytes, but not DCs. These experiments were important because they provided evidence that DCs also existed in humans and set the stage for later immunization experiments (Inaba et al., 1983).
Ralph and Kayo Inaba demonstrated a role for DCs in stimulating naive B cells to produce antibodies capable of binding sheep red blood cells and protein antigens. They showed that once helper T cells had been activated by DCs, the T cells could interact efficiently with antigen-presenting B cells to drive B cell clonal expansion and antibody production (Inaba and Steinman, 1984, 1985; Inaba et al., 1984). They noted that antigen-reactive T cells clustered on the surfaces of the very small number of DCs, typically 1% or less of the total cells, in their experimental systems. Analyzing these T cell–DC clusters, they showed that DCs provide the “microenvironment” for T cell activation and generation of cellular immunity (Inaba et al., 1987).
In all of these systems, small numbers of DCs would elicit a T cell response, whereas much larger numbers of other cell types failed to do so. These experiments led to the realization that there are two stages to every immune response. The first is an afferent stage during which DCs stimulate the growth and differentiation of rare quiescent precursors of antigen-specific helper and cytolytic T cells. The second stage is an efferent limb during which T cells that have been activated by DCs divide in response to encounter with antigens that have been processed and presented by other cells, including B cells and macrophages. This second stage yields large numbers of effector T cells that participate in many immunological reactions (Steinman and Nussenzweig, 1980; Steinman, 1991). Together, these afferent and efferent limbs solve the conundrum of how rare antigen-specific lymphocytes are selected and mobilized to bring about vigorous specific responses.
Maturation
To gain information about DCs in nonlymphoid tissues, Ralph turned to the epidermal Langerhans cells, which were also known to express high levels of MHC class II proteins. With Gerold Schuler, Niki Romani, and Kayo, Ralph found that Langerhans cells needed to differentiate, or mature, to become typical immune stimulatory cells (Schuler and Steinman, 1985; Inaba et al., 1986; Romani et al., 1989). Although Langerhans cells were later shown to have a separate cellular origin from that of DCs (Merad et al., 2002), they served as a model to understand DC function. Ralph and his colleagues discovered that maturing cells exhibited different functional attributes during different periods of time. The first function, antigen capture and presentation, is exhibited by immature DCs. The second function, accessory or co-stimulatory activity, is mediated by mature DCs. Although all DCs process and present antigens, the maturation of DCs determines the type and quality of the immune response that will result from recognition of DC-presented antigens by T cells. There was also evidence that the environment in which DCs mature exerts a major influence on the form of adaptive immunity they promote. Thus, maturation of DCs serves as the critical link between innate and adaptive T cell–dependent immunity.
Growing DCs
Early research on DCs was limited by the need to isolate these scarce cells from primary tissues. During the early 1990s, Ralph and colleagues identified methods for stimulating bone marrow cells to grow and differentiate in vitro into cells that displayed many of the phenotypic characteristics of DCs (Inaba et al., 1992a,b, 1993a; Romani et al., 1994). By 2000, other investigators had discovered that Flt-3L, a hematopoietin that causes a dramatic 10–15-fold expansion of DCs in mice and in humans, can be used to grow authentic DCs in vitro. Once methods to generate large numbers of DCs became available, scientists could more easily study their immunizing properties. This development triggered a major expansion in research and greatly accelerated the pace of discovery.
Pursuing the concept that DCs are “nature’s adjuvant,” Ralph’s group incubated maturing DCs with antigens in vitro and injected these cells into mice and, eventually, humans. The DCs stimulated T cell growth, and the expanded T cells recognized the specific antigens presented on the MHC products of the injected DCs (Inaba et al., 1990). These included microbial antigens in mice (Inaba et al., 1993b) and model antigens in humans (Dhodapkar et al., 1999). Prior to these discoveries, research on antigen presentation had emphasized tissue culture systems and used previously activated lymphocytes or cloned lymphocyte lines. With DCs, Ralph took the problem into immunologically intact mice and humans. By showing that DCs initiated immunity specific for the antigens they had captured, he justified using these cells to develop immunotherapeutic strategies.
Ralph Steinman. Photo by Robert Reichert, The Rockefeller University, 1992.
Endocytosis
Ralph had assumed that splenic and skin DCs were fully ready to initiate immunity because of their high content of MHC II molecules. But when former Cohn laboratory member Ira Mellman and colleagues at Yale brought their expertise in cellular molecular biology to the DC field, they found that the MHC II proteins were mostly sequestered within the endocytic system of developing monocyte-derived DCs in vitro (Trombetta et al., 2003). They proposed that this adaptation allows DCs to efficiently capture, process, and present antigens by preventing the complete catabolism of protein antigens (Inaba et al., 2000). By allowing peptide–MHC II complexes to form inside the endocytic system, DCs optimized their subsequent display at the cell surface (Turley et al., 2000). The regulation and composition of the endocytic system points to a hallmark difference between DCs and macrophages. Whereas macrophages are specialized for continual antigen scavenging and destruction, DCs process antigen in a manner that generates the peptides that bind to different types of antigen-presenting molecules.
Ralph’s studies with Michel on endocytic receptors expressed by DCs introduced yet another field of study: how to increase the immunogenicity of proteins by exploiting specific pathways for antigen uptake. The research began with biomedical student William Swiggard, who isolated DEC-205 (also called CD205; Swiggard et al., 1995). Wanping Jiang, a postdoctoral fellow in Michel’s laboratory, cloned the gene and showed that it encoded an endocytic receptor, the first such receptor identified on DCs in situ (Jiang et al., 1995). By incorporating antigens into monoclonal antibodies specific for DEC-205 and administering these antibodies to living animals, Daniel Hawiger, a student in Michel’s laboratory, first showed that targeting antigens to DCs increased the efficiency of presentation by 100-fold (Hawiger et al., 2001). Although the potency of DCs after antigen capture had been emphasized in the past, Ralph and Michel’s work on antigen handling revealed that this function of DCs can be dramatically improved in intact animals.
Immune tolerance
Beginning in 2000, in close collaboration with Michel and Hawiger, Ralph uncovered roles for DCs in controlling immune tolerance (Hawiger et al., 2001; Steinman and Nussenzweig, 2002). To analyze tolerance, Ralph took an approach first suggested by their discovery that immature DCs induce antigen-specific tolerance in humans (Dhodapkar et al., 2001). Ralph studied two forms of antigen. One consisted of peptides and proteins incorporated into antibodies that recognize DEC-205, which is expressed on DCs in lymphoid tissues (Hawiger et al., 2001). The other consisted of antigen within dying cells (Iyoda et al., 2002; Liu et al., 2002). When antigens were attached to anti–DEC-205, and thus targeted directly to immature DCs in vivo, in the absence of inflammatory stimuli that promote DC maturation, the antigens were processed and recognized by T cells but the T cells were tolerized in response. In contrast, delivery of a maturation stimulus together with the same targeted antigen produced long-lived immunity involving both helper and cytolytic T cells (Hawiger et al., 2001; Liu et al., 2005).
In addition to the classical pathway of clonal deletion, the regulatory T cell, particularly the variety programmed by the protein Foxp3, is a powerful mechanism of tolerance. In this issue of the journal, a paper by a postdoctoral fellow in Ralph’s laboratory (Sela et al.) describes a way to use DCs to generate antigen-specific T reg cells capable of preventing graft versus host disease in mice.
Whereas inducing tolerance in fully developed lymphocytes formerly required high doses of nontargeted antigens and met with limited success, the targeted delivery of antigen to DCs more efficiently and specifically silenced the immune system.
DC-based vaccines
From the beginning, Ralph planned to take DCs into medicine. His deep insights into the biology of DCs and his interest in the control of immunity led him to explore two novel approaches to stimulate innate immunity.
One strategy was an active immunization against advanced cancer. Madhav Dhodapkar, Ralph, and others developed ways to remove DCs from a patient, charge them with specific antigens, and deliver them back into the patient (Chang et al., 2005). This approach, resulting in expanded and sustained T cell responses, recently approved by the US Food and Drug Administration, is now being used by many other laboratories.
The other vaccine strategy harnesses the major features of DCs—location, presentation, maturation, and formation of subsets—in situ. It involves engineering disease-relevant antigens into monoclonal antibodies and targeting them to particular DC-specific receptors. This approach, based on the work of Hawiger et al. (2001), is currently being applied to malaria, tuberculosis, Leishmania, cancer, and AIDS. The resulting T cell–mediated immune response to targeted antigens, relative to nontargeted antigens, is greater in efficacy, higher in magnitude, and associated with protection (Boscardin et al., 2006; Trumpfheller et al., 2006, 2008; Nchinda et al., 2008).
A critical and separate issue in targeting vaccine proteins is to incorporate a stimulus or adjuvant to incite DC maturation. A paper in this issue, by Caskey et al. of the Rockefeller Hospital, together with Rafick Sékaly and his colleagues in Port St. Lucie, shows that in healthy humans the adjuvant double-stranded RNA (poly ICLC) stimulated a broad innate immune response mimicking that induced by a live viral vaccine.
Ralph was that rare scientist who lived through a period in which his endeavors came to fruition. He experienced a revolution in immunology and both performed and witnessed work that explained how DCs provide the physiological means to initiate clonal expansion, bring about tolerance, differentiate lymphocytes into disease-fighting cells, and develop memory, each in an antigen-specific manner. Ralph was excited when he found novel cells in 1973, and he died convinced that these cells had become a novel force in medicine.
Acknowledgments
Michel Nussenzweig, Svetlana Mojsov, and Maggi Witmer-Pack made valuable contributions to this manuscript.
References
- Boscardin S.B., Hafalla J.C., Masilamani R.F., Kamphorst A.O., Zebroski H.A., Rai U., Morrot A., Zavala F., Steinman R.M., Nussenzweig R.S., Nussenzweig M.C. 2006. Antigen targeting to dendritic cells elicits long-lived T cell help for antibody responses. J. Exp. Med. 203:599–606 10.1084/jem.20051639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnet F.M. 1957. A modification of Jerne’s theory of antibody production using the concept of clonal selection. Aust. J. Sci. 20:67–69 [DOI] [PubMed] [Google Scholar]
- Caskey M., Lefebvre F., Filali-Mouhim A., Cameron M.J., Goulet J.-P., Haddad E.K., Breton G., Trumpfheller C., Pollak S., Shimeliovich I., et al. 2011. Synthetic double-stranded RNA induces innate immune responses similar to a live viral vaccine in humans. J. Exp. Med. 208:2357–2366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang D.H., Osman K., Connolly J., Kukreja A., Krasovsky J., Pack M., Hutchinson A., Geller M., Liu N., Annable R., et al. 2005. Sustained expansion of NKT cells and antigen-specific T cells after injection of α-galactosyl-ceramide loaded mature dendritic cells in cancer patients. J. Exp. Med. 201:1503–1517 10.1084/jem.20042592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhodapkar M.V., Steinman R.M., Sapp M., Desai H., Fossella C., Krasovsky J., Donahoe S.M., Dunbar P.R., Cerundolo V., Nixon D.F., Bhardwaj N. 1999. Rapid generation of broad T-cell immunity in humans after a single injection of mature dendritic cells. J. Clin. Invest. 104:173–180 10.1172/JCI6909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhodapkar M.V., Steinman R.M., Krasovsky J., Münz C., Bhardwaj N. 2001. Antigen-specific inhibition of effector T cell function in humans after injection of immature dendritic cells. J. Exp. Med. 193:233–238 10.1084/jem.193.2.233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dudziak D., Kamphorst A.O., Heidkamp G.F., Buchholz V.R., Trumpfheller C., Yamazaki S., Cheong C., Liu K., Lee H.W., Park C.G., et al. 2007. Differential antigen processing by dendritic cell subsets in vivo. Science. 315:107–111 10.1126/science.1136080 [DOI] [PubMed] [Google Scholar]
- Hawiger D., Inaba K., Dorsett Y., Guo M., Mahnke K., Rivera M., Ravetch J.V., Steinman R.M., Nussenzweig M.C. 2001. Dendritic cells induce peripheral T cell unresponsiveness under steady state conditions in vivo. J. Exp. Med. 194:769–780 10.1084/jem.194.6.769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inaba K., Steinman R.M. 1984. Resting and sensitized T lymphocytes exhibit distinct stimulatory (antigen-presenting cell) requirements for growth and lymphokine release. J. Exp. Med. 160:1717–1735 10.1084/jem.160.6.1717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inaba K., Steinman R.M. 1985. Protein-specific helper T-lymphocyte formation initiated by dendritic cells. Science. 229:475–479 10.1126/science.3160115 [DOI] [PubMed] [Google Scholar]
- Inaba K., Steinman R.M., Van Voorhis W.C., Muramatsu S. 1983. Dendritic cells are critical accessory cells for thymus-dependent antibody responses in mouse and in man. Proc. Natl. Acad. Sci. USA. 80:6041–6045 10.1073/pnas.80.19.6041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inaba K., Witmer M.D., Steinman R.M. 1984. Clustering of dendritic cells, helper T lymphocytes, and histocompatible B cells during primary antibody responses in vitro. J. Exp. Med. 160:858–876 10.1084/jem.160.3.858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inaba K., Schuler G., Witmer M.D., Valinksy J., Atassi B., Steinman R.M. 1986. Immunologic properties of purified epidermal Langerhans cells. Distinct requirements for stimulation of unprimed and sensitized T lymphocytes. J. Exp. Med. 164:605–613 10.1084/jem.164.2.605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inaba K., Young J.W., Steinman R.M. 1987. Direct activation of CD8+ cytotoxic T lymphocytes by dendritic cells. J. Exp. Med. 166:182–194 10.1084/jem.166.1.182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inaba K., Metlay J.P., Crowley M.T., Steinman R.M. 1990. Dendritic cells pulsed with protein antigens in vitro can prime antigen-specific, MHC-restricted T cells in situ. J. Exp. Med. 172:631–640 10.1084/jem.172.2.631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inaba K., Steinman R.M., Pack M.W., Aya H., Inaba M., Sudo T., Wolpe S., Schuler G. 1992a. Identification of proliferating dendritic cell precursors in mouse blood. J. Exp. Med. 175:1157–1167 10.1084/jem.175.5.1157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inaba K., Inaba M., Romani N., Aya H., Deguchi M., Ikehara S., Muramatsu S., Steinman R.M. 1992b. Generation of large numbers of dendritic cells from mouse bone marrow cultures supplemented with granulocyte/macrophage colony-stimulating factor. J. Exp. Med. 176:1693–1702 10.1084/jem.176.6.1693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inaba K., Inaba M., Deguchi M., Hagi K., Yasumizu R., Ikehara S., Muramatsu S., Steinman R.M. 1993a. Granulocytes, macrophages, and dendritic cells arise from a common major histocompatibility complex class II-negative progenitor in mouse bone marrow. Proc. Natl. Acad. Sci. USA. 90:3038–3042 10.1073/pnas.90.7.3038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inaba K., Inaba M., Naito M., Steinman R.M. 1993b. Dendritic cell progenitors phagocytose particulates, including bacillus Calmette-Guerin organisms, and sensitize mice to mycobacterial antigens in vivo. J. Exp. Med. 178:479–488 10.1084/jem.178.2.479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inaba K., Turley S., Iyoda T., Yamaide F., Shimoyama S., Reis e Sousa C., Germain R.N., Mellman I., Steinman R.M. 2000. The formation of immunogenic MHC class II- peptide ligands in lysosomal compartments of dendritic cells is regulated by inflammatory stimuli. J. Exp. Med. 191:927–936 10.1084/jem.191.6.927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iyoda T., Shimoyama S., Liu K., Omatsu Y., Akiyama Y., Maeda Y., Takahara K., Steinman R.M., Inaba K. 2002. The CD8+ dendritic cell subset selectively endocytoses dying cells in culture and in vivo. J. Exp. Med. 195:1289–1302 10.1084/jem.20020161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang W., Swiggard W.J., Heufler C., Peng M., Mirza A., Steinman R.M., Nussenzweig M.C. 1995. The receptor DEC-205 expressed by dendritic cells and thymic epithelial cells is involved in antigen processing. Nature. 375:151–155 10.1038/375151a0 [DOI] [PubMed] [Google Scholar]
- Liu K., Iyoda T., Saternus M., Kimura Y., Inaba K., Steinman R.M. 2002. Immune tolerance after delivery of dying cells to dendritic cells in situ. J. Exp. Med. 196:1091–1097 10.1084/jem.20021215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu K., Idoyaga J., Charalambous A., Fujii S., Bonito A., Mordoh J., Wainstok R., Bai X.F., Liu Y., Steinman R.M. 2005. Innate NKT lymphocytes confer superior adaptive immunity via tumor-capturing dendritic cells. J. Exp. Med. 202:1507–1516 10.1084/jem.20050956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merad M., Manz M.G., Karsunky H., Wagers A., Peters W., Charo I., Weissman I.L., Cyster J.G., Engleman E.G. 2002. Langerhans cells renew in the skin throughout life under steady-state conditions. Nat. Immunol. 3:1135–1141 10.1038/ni852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metlay J.P., Witmer-Pack M.D., Agger R., Crowley M.T., Lawless D., Steinman R.M. 1990. The distinct leukocyte integrins of mouse spleen dendritic cells as identified with new hamster monoclonal antibodies. J. Exp. Med. 171:1753–1771 10.1084/jem.171.5.1753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nchinda G., Kuroiwa J., Oks M., Trumpfheller C., Park C.G., Huang Y., Hannaman D., Schlesinger S.J., Mizenina O., Nussenzweig M.C., et al. 2008. The efficacy of DNA vaccination is enhanced in mice by targeting the encoded protein to dendritic cells. J. Clin. Invest. 118:1427–1436 10.1172/JCI34224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nussenzweig M.C., Steinman R.M., Gutchinov B., Cohn Z.A. 1980. Dendritic cells are accessory cells for the development of anti-trinitrophenyl cytotoxic T lymphocytes. J. Exp. Med. 152:1070–1084 10.1084/jem.152.4.1070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nussenzweig M.C., Steinman R.M., Witmer M.D., Gutchinov B. 1982. A monoclonal antibody specific for mouse dendritic cells. Proc. Natl. Acad. Sci. USA. 79:161–165 10.1073/pnas.79.1.161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romani N., Koide S., Crowley M., Witmer-Pack M., Livingstone A.M., Fathman C.G., Inaba K., Steinman R.M. 1989. Presentation of exogenous protein antigens by dendritic cells to T cell clones. Intact protein is presented best by immature, epidermal Langerhans cells. J. Exp. Med. 169:1169–1178 10.1084/jem.169.3.1169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romani N., Gruner S., Brang D., Kämpgen E., Lenz A., Trockenbacher B., Konwalinka G., Fritsch P.O., Steinman R.M., Schuler G. 1994. Proliferating dendritic cell progenitors in human blood. J. Exp. Med. 180:83–93 10.1084/jem.180.1.83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuler G., Steinman R.M. 1985. Murine epidermal Langerhans cells mature into potent immunostimulatory dendritic cells in vitro. J. Exp. Med. 161:526–546 10.1084/jem.161.3.526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sela U., Olds P., Park A., Sclesinger S.J., Steinman R.M. 2011. Dendritic cells induce antigen-specific regulatory T cells that prevent graft versus host disease and persist in mice. J. Exp. Med. 208:2489–2496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinman R.M. 1991. The dendritic cell system and its role in immunogenicity. Annu. Rev. Immunol. 9:271–296 10.1146/annurev.iy.09.040191.001415 [DOI] [PubMed] [Google Scholar]
- Steinman R.M., Cohn Z.A. 1972. The interaction of soluble horseradish peroxidase with mouse peritoneal macrophages in vitro. J. Cell Biol. 55:186–204 10.1083/jcb.55.1.186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinman R.M., Cohn Z.A. 1973. Identification of a novel cell type in peripheral lymphoid organs of mice. I. Morphology, quantitation, tissue distribution. J. Exp. Med. 137:1142–1162 10.1084/jem.137.5.1142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinman R.M., Cohn Z.A. 1974. Identification of a novel cell type in peripheral lymphoid organs of mice. II. Functional properties in vitro. J. Exp. Med. 139:380–397 10.1084/jem.139.2.380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinman R.M., Nussenzweig M.C. 1980. Dendritic cells: features and functions. Immunol. Rev. 53:127–147 10.1111/j.1600-065X.1980.tb01042.x [DOI] [PubMed] [Google Scholar]
- Steinman R.M., Nussenzweig M.C. 2002. Avoiding horror autotoxicus: the importance of dendritic cells in peripheral T cell tolerance. Proc. Natl. Acad. Sci. USA. 99:351–358 10.1073/pnas.231606698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinman R.M., Witmer M.D. 1978. Lymphoid dendritic cells are potent stimulators of the primary mixed leukocyte reaction in mice. Proc. Natl. Acad. Sci. USA. 75:5132–5136 10.1073/pnas.75.10.5132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinman R.M., Kaplan G., Witmer M.D., Cohn Z.A. 1979. Identification of a novel cell type in peripheral lymphoid organs of mice. V. Purification of spleen dendritic cells, new surface markers, and maintenance in vitro. J. Exp. Med. 149:1–16 10.1084/jem.149.1.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinman R.M., Gutchinov B., Witmer M.D., Nussenzweig M.C. 1983. Dendritic cells are the principal stimulators of the primary mixed leukocyte reaction in mice. J. Exp. Med. 157:613–627 10.1084/jem.157.2.613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swiggard W.J., Mirza A., Nussenzweig M.C., Steinman R.M. 1995. DEC-205, a 205-kDa protein abundant on mouse dendritic cells and thymic epithelium that is detected by the monoclonal antibody NLDC-145: purification, characterization, and N-terminal amino acid sequence. Cell. Immunol. 165:302–311 10.1006/cimm.1995.1218 [DOI] [PubMed] [Google Scholar]
- Trombetta E.S., Ebersold M., Garrett W., Pypaert M., Mellman I. 2003. Activation of lysosomal function during dendritic cell maturation. Science. 299:1400–1403 10.1126/science.1080106 [DOI] [PubMed] [Google Scholar]
- Trumpfheller C., Finke J.S., Lopez C.B., Moran T.M., Moltedo B., Soares H., Huang Y., Schlesinger S.J., Park C.G., Nussenzweig M.C., et al. 2006. Intensified and protective CD4+ T cell immunity at a mucosal surface after a single dose of anti-dendritic cell HIV gag fusion antibody vaccine. J. Exp. Med. 203:607–617 10.1084/jem.20052005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trumpfheller C., Caskey M., Nchinda G., Longhi M.P., Mizenina O., Huang Y., Schlesinger S.J., Colonna M., Steinman R.M. 2008. The microbial mimic poly IC induces durable and protective CD4+ T cell immunity together with a dendritic cell targeted vaccine. Proc. Natl. Acad. Sci. USA. 105:2574–2579 10.1073/pnas.0711976105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turley S.J., Inaba K., Garrett W.S., Ebersold M., Unternaehrer J., Steinman R.M., Mellman I. 2000. Transport of peptide-MHC class II complexes in developing dendritic cells. Science. 288:522–527 10.1126/science.288.5465.522 [DOI] [PubMed] [Google Scholar]
- Van Voorhis W.C., Hair L.S., Steinman R.M., Kaplan G. 1982. Human dendritic cells. Enrichment and characterization from peripheral blood. J. Exp. Med. 155:1172–1187 10.1084/jem.155.4.1172 [DOI] [PMC free article] [PubMed] [Google Scholar]