Abstract
Fructose-sweetened liquid consumption is associated with fatty liver and oxidative stress. In rodent models of fructose-mediated fatty liver, protein consumption is decreased. Additionally, decreased sulfur amino acid intake is known to cause oxidative stress. Studies were designed to test whether oxidative stress in fructose-sweetened liquid-induced fatty liver is caused by decreased ad libitum solid food intake with associated inadequate sulfur amino acid intake. C57BL6 mice were grouped as: control (ad libitum water), fructose (ad libitum 30% fructose-sweetened liquid), glucose (ad libitum 30% glucose-sweetened water) and pair-fed (ad libitum water and sulfur amino acid intake same as the fructose group). Hepatic and plasma thiol-disulfide antioxidant status were analyzed after five weeks. Fructose- and glucose-fed mice developed fatty liver. The mitochondrial antioxidant protein, thioredoxin-2, displayed decreased abundance in the liver of fructose and glucose-fed mice compared to controls. Glutathione/glutathione disulfide redox potential (EhGSSG) and abundance of the cytoplasmic antioxidant protein, peroxiredoxin-2, were similar among groups. We conclude that both fructose and glucose-sweetened liquid consumption results in fatty liver and upregulated thioredoxin-2 expression, consistent with mitochondrial oxidative stress; however, inadequate sulfur amino acid intake was not the cause of this oxidative stress.
Keywords: cystine, methionine, thioredoxin, redox potential, mitochondria, obesity
1. Introduction
Consumption of refined sugars has increased over the past decades [1,2] and fructose, in particular, has been implicated as a contributing factor in the development of metabolic diseases [3]. These diseases include conditions such as obesity, dyslipidemia, insulin resistance, diabetes, high blood pressure [4,5,6,7,8,9,10,11,12,13], and non-alcoholic fatty liver disease [14,15,16,17,18]. The etiology of fructose-mediated metabolic disturbances is not completely understood; however, it is likely due to a multifactorial disease process [4,5,9,19,20]. Fructose consumption and its metabolic alterations, including fatty liver, have been associated with oxidative stress [21,22,23,24,25,26,27,28,29,30,31,32,33], which may play role in the pathogenesis of these conditions.
In animal models, fructose-sweetened beverage consumption is associated with decreased food and protein intake [34,35,36]. Therefore, inadequate ingestion of macronutrients and energy from solid foods may be important in the metabolic alterations attributed to fructose-sweetened beverages [20,37,38,39,40,41,42,43]. In rodents, when fructose-sweetened liquid is provided ad libitum, liquid intake increases and solid food consumption decreases, while total energy intake is maintained at a level comparable to controls [34,44,45]. This resultant decrease in solid food results in decreased protein consumption and insufficient intake of non-essential and essential amino acids, which includes the sulfur amino acids, i.e., cysteine (Cys) and methionine.
All cells have thiol-dependent antioxidant systems that are critical in redox regulation of cellular processes, like gene transcription, and protection against oxidative stress [46]. Major thiol-containing redox couples (GSH/GSSG, thioredoxin (Trx) and peroxiredoxin (Prx)) contain Cys as a central thiol and oxidation of these residues provide useful markers of oxidative stress [47]. In humans, Cys deficiency can lead to plasma oxidative stress [48], and in rodents, dietary sulfur amino acid insufficiency causes plasma and tissue level oxidative stress [49,50], as shown by steady-state redox potentials (Eh) for GSH/GSSG and Cys/CySS redox couples. Because fructose-sweetened beverages decrease dietary sulfur amino acid intake and sulfur amino acid insufficiency causes oxidative stress, it is possible that decreased sulfur amino acid intake may contribute to oxidative stress observed in fructose-induced fatty liver. Therefore, the purpose of this study was to determine if oxidative stress associated with fructose-induced fatty liver was due to decreased sulfur amino acid intake. In the experimental design, pair-feeding of mice with the amount of solid food consumed by the fructose group resulted in substantial energy deficiency in the pair-fed group. Despite this difference in energy intake, the pair-fed group did not show hepatic oxidative stress either in terms of thiol/disulphide levels or mitochondrial thioredoxin-2 or cytoplasmic/nuclear peroredoxin-2 levels. Thus, the results show that fructose- or glucose-induced fatty liver is not an artefact due to oxidative stress caused by insufficient protein intake.
2. Materials and Methods
2.1. Animals and Feeding Protocol
This protocol was approved by the Institutional Animal Care and Use Committee at Emory University and performed according to NIH guidelines. The study outlined below was repeated in two separate experiments to confirm findings. Results were similar for both experiments and combined for presentation.
Five week-old C57BL6 male mice (N = 39) were purchased from Charles River Laboratory. Anhydrous dextrose and D-fructose were purchased from Harlan Teklad. Mice were housed in individual cages in a pathogen-free barrier facility. During an initial acclimatization period of 1 week, all mice received water ad libitum and solid food ad libitum (LabDiet-5001, AIN 93M, PMI Nutrition International). Methionine (Met) and Cys content of the diet were 0.67% and 0.31%, respectively. At 6 weeks of age, mice were allocated to four groups: control (ad libitum water and ad libitum solid food; n = 10), fructose (ad libitum 30% fructose-sweetened water (w/v) and ad libitum solid food; n = 11), glucose (ad libitum 30% dextrose-sweetened water (w/v) and ad libitum solid food; n = 10) and a pair fed group (ad libitum water, pair fed to fructose for solid food intake of F; n = 8). The pair-fed animals were started on dietary intervention one day after starting the fructose-fed mice and the mean daily individual food consumption of the fructose group was fed to individual pair-fed mice. Mice were examined daily for signs of dehydration and distress. Body weight and water and food consumption, were measured every other day. After 5 weeks, at sacrifice, animals were anesthetized with 80 mg/kg ketamine and 6 mg/kg xylazine i.p. Blood was collected from a cheek and 50 µL of plasma was processed for Cys, CySS, GSH and GSSG analyses by high performance liquid chromatography (HPLC) as previously outlined [49,50]. Portions of liver (approximately 5 mg) were immediately added to preservation solution for redox measurements [49,50]. Additional samples were snap frozen in liquid nitrogen or placed in OCT compound for cryosectioning and Oil Red O staining and stored at −80 °C. Because of a laboratory error, samples for Oil Red O staining were not available for the glucose-treated group. Because glucose-induced fatty liver is established in the literature [29,51] and confirmed by the triglyceride measurements obtained in the present studies, the experiment was not repeated to obtain this additional control.
2.2. Analytical Methods
Plasma and hepatic Cys, CySS, GSH and GSSG concentrations were measured using HPLC. Methods were adopted from Jones et al. and Nkabyo et al. [49,52,53]. Protein concentration of liver samples was measured using the Bradford assay. EhCyss and EhGSSG were calculated using the Nernst Equation. Percent of oxidized thiol (% CySS and % GSSG) was calculated with respect to thiol concentration (oxidized + reduced + mixed disulfide Cys-GSH). Plasma Met concentration was measured as an additional indicator of plasma sulfur amino acid levels using liquid chromatography mass spectrometry (LC-FTMS) with electrospray ionization in positive ion mode essentially as described by Johnson et al. [54]. Plasma samples with visible hemolysis were excluded. Plasma extracts were separated using anion exchange chromatography and detected using LTQ-FT mass spectrometer (Thermo Fisher Scientific, San Jose, CA). Met (m/z 149.0510) was quantified relative to a stable isotopic internal standard. Hepatic triglycerides (TG) were assayed using a TG quantification kit (BioVision, CA; cat# K622-100). Liver samples (approximately 100 mg) were collected into 1 mL of 5× Triton-X solution, homogenized and processed per manufacturer’s instructions. For TG quantification, absorbance at 570 nm was calibrated to reference standards and data were expressed as nmol/100 mg of liver tissue.
2.3. Western Blot Analyses
Hepatic protein abundance of thioredoxin-2 (Trx2) and peroxiredoxin-2 (Prx2) was analysed by Western blot. Liver (approximately 5 mg) was washed with ice cold PBS and immediately placed in 300 µL lysis buffer (1% NP-40, 0.5% Triton X-100, 50 mM Tris, 2 mM EDTA, 500 mM NaCl, protease inhibitor; pH 7.6), sonicated, vortexed, and centrifuged. Supernatant was used for protein quantification and Western blot analysis.
For all Western blots, 20 µg of protein was loaded in each well, separated using 15% SDS polyacrylamide gel electrophoresis and transferred to nitrocellulose membranes. After blocking, the membranes were incubated with primary antibodies specific to Trx-2 [55], Prx2 (Abcam16748), COX-IV (Abcam16056 as a mitochondrial control protein) or β-actin (Sigma-Aldrich A5441) for 1 h followed by the secondary antibody (IRDyeTM-800-conjugated anti-rabbit or anti-mouse antibody (Rockland Immuno chemicals, Gilbertsville, PA)) for 1 h. Protein bands were visualized by the Odyssey system (LiCor, Lincoln, NE) and quantified by densitometry.
2.4. Thiobarbituric Acid Reactive Substances Assay
A small amount of frozen liver tissue was placed in a 1.5 mL tube containing 200 μL of RIPA buffer. The samples were then sonicated for approximately 10 s to homogenize the tissue. Insoluble debris was pelleted via centrifugation and 100 μL of supernantant was added to 200 μL of 10% trichloroacetic acid. The samples were incubated on ice for 15 min and the precipitated protein was pelleted by centrifugation. 200 μL of supernatant was added to 200 μL of 0.67% (w/v) 2-thiobarbituric acid and incubated for 15 min at 100 °C. Samples were cooled to room temperature and absorbance at 532 nm was read on a microplate reader.
2.5. Oil Red O Staining
Liver tissue preserved in OCT compound was cryosectioned into 10 µM sections, mounted onto microscope slides and stored at −10 °C until staining. Slides were allowed to acclimate to room temperature for approximately 10-15 min prior to staining. Tissue was then fixed in 10% neutral buffered formalin for 5 min and briefly washed in water. The slides were then rinsed in 60% isopropanol and placed into freshly prepared Oil Red O working solution. Slides were allowed to stain for 15 min at room temperature. After staining, slides were rinsed with 60% isopropanol and the nuclei were lightly stained with hematoxylin stain (approx. 5 dips). Lastly, the slides were washed 3 times in water and coverslips were applied using aqueous mounting media. The slides were then visualized on a light microscope at 100× magnification.
2.6. Statistical Analysis
Data are expressed as mean ± SEM. Statistical analysis was performed using SPSS 16.0 (IBM, Chicago, IL). ANOVA with Tukey’s post-hoc test was used to compare the groups. p ≤ 0.05 was considered statistically significant.
3. Results
3.1. Fatty Liver
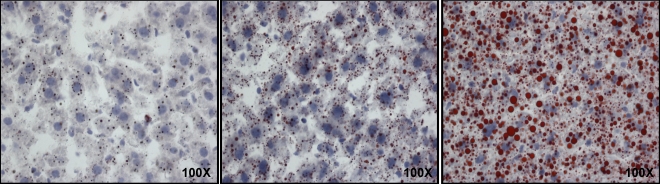
Fructose and glucose fed mice developed fatty liver as evidenced by significantly higher hepatic TG content (75 ± 4 nmol/100 mg and 70 ± 5 nmol/100 mg, respectively) compared to control and pair-fed mice (44 ± 1 nmol/100 mg and 41 ± 2 nmol/100 mg), respectively (each p < 0.05). To confirm the development of hepatic steatosis, frozen liver sections were stained with Oil Red O to visualize lipid accumulation (Figure 1). Results from fructose-fed mice confirmed fatty liver; samples from glucose-treated mice were not available, but glucose-induced fatty liver has been previously established [29,51] and confirmed in the present study by the TG measurements. Together, these data show that both fructose and glucose cause fatty liver.
Figure 1.
Oil Red O staining of frozen liver sections from control, pair-fed and fructose-fed mice. These sections are visualized at 100× magnification. The red staining corresponds to lipids and the blue stain corresponds to nuclei, respectively.
3.2. Animal Characteristics
Body weight and food consumption data are detailed in Table 1.
Initial body weights were similar for all groups. At the end of dietary treatment, the fructose and glucose-fed groups had a 10% and 25% weight gain respectively, compared to control. The pair-fed group lost weight during the course of the study because the design resulted in a relatively severe calorie restriction. However, these mice remained active and did not show any signs of distress. Consumption of fructose or glucose supplemented water resulted in a 38% and 54% decrease in solid food (and thus sulfur amino acid intake) consumption respectively, compared to control. Dietary liquid consumption was different across all the groups. Fructose-fed and glucose-fed mice had 42% and 98% higher, while the pair-fed mice had 56% lower liquid intake respectively compared to controls. Total energy intake (solid food + liquid) in fructose-fed (18 ± 1 kcal/day) and glucose-fed (19 ± 1 kcal/day) mice was similar to control mice (16 ± 1 kcal/day) (Table 1). As liquid consumption in the fructose and glucose groups increased, solid food intake decreased and total energy intake was similar compared to controls. Glucose-fed mice consumed about 30% more energy (11.4 ± 1 kcal/day) from liquid than fructose-fed mice (8.1 ± 1 kcal/day). Energy intake for mice in the pair-fed group (10 ± 0 kcal/day) was 52-62% of other groups.
Table 1.
Animal weights and dietary intake #.
| Parameters | Control | Fructose | Glucose | Pair fed | p† |
|---|---|---|---|---|---|
| n = 10 | n = 11 | n = 10 | n = 8 | ||
| Initial weight (g) | 20.1 ± 0.1 a | 20 ± 0.3 a | 19.9 ± 0.3 a | 19.6 ± 0.3 a | 0.7 |
| Final weight (g) | 25.5 ± 0.3 a | 28.1 ± 0.6 b | 31.8 ± 0.6 c | 17.1 ± 0.2 d | <0.001 |
| Solid food intake (gm/day) | 3.9 ± 0.2 a | 2.4 ± 0.3 b | 1.8 ± 0.2 b | 2.4 ± 0 b | <0.001 |
| Liquid intake (mL/day) | 4.8 ± 0.3 a | 6.8 ± 0.2 b | 9.5 ± 0.2 c | 2.1 ± 0.1 d | <0.001 |
| Cysteine intake (mg/day) | 12.2 ± 0.7 a | 7.5 ± 0.9 b | 5.7 ± 0.5 b | 7.5 ± 0 b | <0.001 |
| Methionine intake (mg/day) | 26.4 ± 1.5 a | 16.3 ± 20 b | 12.2 ± 1.2 b | 16.3 ± 0 b | <0.001 |
| Total caloric intake (kcal/day) | 16.0 ± 1.0 a | 18.0 ± 1.0 a | 19.0 ± 1.0 a | 10.0 ± 0 b | <0.001 |
a,b,c,d Different superscripted letters indicate statistically significant (p < 0.05) difference between groups; # Data expressed as mean ± SEM; † ANOVA.
3.3. Plasma Sulfur Amino Acids
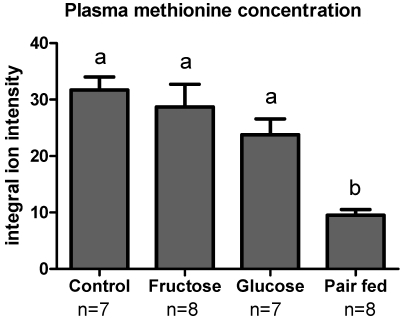
Plasma methionine levels were measured using LC-FTMS. The ion intensity of methionine in both fructose-fed and glucose-fed mice was similar to controls even though sulfur amino acid intake was lower (Figure 2). Pair-fed animals displayed methionine levels that were significantly lower than the other groups. Additionally, plasma Cys (Table 2) showed a trend similar to methionine and was also lower in pair-fed animals compared to other groups.
Figure 2.
Plasma methionine concentration as measured by LC-FTMS. The data is expressed as integral ion intensity relative to internal standard. Pair-fed mice had significantly decreasedplasma methionine concentration compared to other groups. Different superscripted letters (a,b) indicate statistically significant differences among respective groups.
Table 2.
High Performance Liquid Chromatography data of plasma and liver thiols #.
| Antioxidant thiols | Control | Fructose | Glucose | Pair fed | p† |
|---|---|---|---|---|---|
| n = 10 | n = 11 | n = 10 | n = 8 | ||
| Plasma | |||||
| Cys (µM) | 18.2 ± 2.0 a | 17.1 ± 1.0 a | 13.2 ± 2.0 a,b | 9.1 ± 1.0 b | 0.002 |
| CySS (µM) | 40.4 ± 2.0 | 40.9 ± 3.0 | 43.7 ± 3.0 | 33.4 ± 2.0 | 0.06 |
| GSH (µM) | 26.4 ± 5.0 a | 17.2 ± 2.0 | 20.7 ± 2.0 | 10.5 ± 2.0 b | 0.005 |
| GSSG (µM) | 1.6 ± 0.3 | 1.3 ± 0.3.0 | 1.3 ± 0.2 | 0.7 ± 0.2 | 0.2 |
| Total Cys (µM) | 114.1 ± 4.0 a | 109.4 ± 8.0 a | 113.8 ± 3.0 a | 81.0 ± 5.0 b | 0.004 |
| Total GSH (µM) | 44.8 ± 7.0 a | 30.4 ± 3.0 a,b | 36.5 ± 4.0 a | 17.0 ± 2.0 b | 0.001 |
| Liver | |||||
| Cys (µM) | 9.9 ± 2.0 | 7.2 ± 2.0 | 17.1 ± 9.0 | 11.8 ± 2.0 | 0.5 |
| CySS (µM) | 38.3 ± 7.0 a | 34.6 ± 6.0 a,b | 41.7 ± 8.0 a | 10.9 ± 2.0 b | 0.01 |
| GSH (µM) | 1884 ± 149.0 a | 1642 ± 137.0 a | 1432 ± 177 a,b | 982 ± 63 b | 0.002 |
| GSSG (µM) | 81.9 ± 13.0 a | 52.3 ± 5.0 a,b | 40.8 ± 7.0 b | 40.5 ± 4.0 b | 0.004 |
| Total Cys (µM) | 126.1 ± 15.0 a | 104.5 ± 14.0 a,b | 116.6 ± 18.0 a | 57.4 ± 5.0 b | 0.01 |
| Total GSH (µM) | 2087.2 ± 144 a | 1774.5 ± 142 a | 1530 ± 202 a,b | 1087 ± 66 b | 0.001 |
a,b Different superscripted letters indicate statistically significant (p < 0.05) difference between groups; # Data expressed as mean ± SEM; † ANOVA.
3.4. Plasma Oxidative Stress Indices
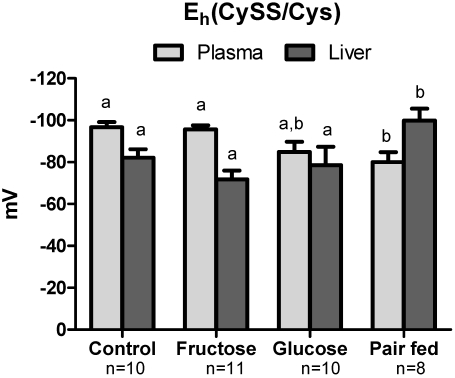
Even with the decreased sulfur amino acid intake due to fructose and glucose, plasma Cys, total Cys (Cys + CySS + Cys-GSH) and total GSH concentration (GSH + GSSG + Cys-GSH) were similar to control mice (Table 2). In contrast, GSH level was lower in fructose-fed and glucose-fed mice compared to control. Interestingly, the fructose and pair-fed groups had the same sulfur amino acid intake, but the pair-fed animals had lower plasma Cys, total Cys, GSH and total GSH. Pair-fed animals also had an increased % CySS (Figure 3) indicating greater systemic oxidative stress. GSH/GSSG ratio, Cys/CySS ratio and % GSSG were not different across groups (data not shown). Plasma EhCySS was more oxidized (more positive Eh) in pair-fed mice compared to control and fructose groups (Figure 4). EhGSSG values did not show significant differences between groups.
3.5. Hepatic Oxidative Stress
Similar to data from the plasma, hepatic Cys and GSH content was not different in the control, fructose and glucose groups, but was decreased in the pair-fed animals (Table 2). Thiobarbituric acid reactive substances (TBARS) in the liver, a common metric of oxidative stress and lipid peroxidation, showed that TBARS was increased due to fructose treatment but this was not statistically significant (Figure 5). Importantly, the pair-fed group did not show evidence of increase. In contrast to the plasma data described above, the relative concentrations of CySS and Cys shifted towards a more reduced state (Figure 4). GSH/GSSG ratio, Cys/CySS ratio and % GSSG did not differ across the groups (data not shown).
Figure 3.
% CySS in plasma and liver. CySS was measured as percent of total Cys pool (Cys, CySS and Cys-GSH). Different letters (a,b) indicate statistically significant differences among respective groups. In the pair-fed group, plasma % Cyss was significantly increased while hepatic % Cyss was decreased, indicating oxidation of plasma but not liver.
Figure 4.
Cys/CySS redox potential (EhCySS) in plasma and liver. EhCySS is calculated using Nernst equation and expressed in mV. Different letters (a,b) indicate statistically significant difference among respective groups. In the pair fed group, the EhCySS was oxidized in plasma, while reduced in liver compared to other groups, indicating differential plasma but not hepatic oxidative stress.
Figure 5.
Results of thiobarbituric acid reactive substances (TBARS) assays shows that fructose and glucose feeding do not result in significant increases in hepatic lipid peroxidation. Data was analyzed via one-way ANOVA (p = 0.417).
In contrast to plasma, hepatic % CySS was lower and EhCySS was more reduced in the pair-fed group (Figure 3). EhGSSG in control, fructose, glucose and pair-fed groups were not significantly different. Thus, even though there is an indication of systemic oxidative stress in plasma, the results do not provide evidence for hepatic oxidative stress as measured by the tissue TBARS, Cys/CySS and GSH/GSSG pools.
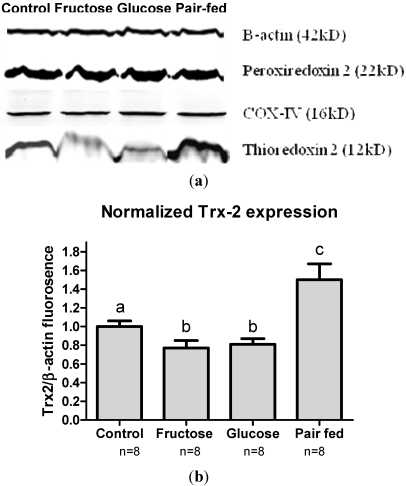
3.6. Antioxidant Protein Expression
Although the measurement of liver Cys/CySS and GSH/GSSG pools do not provide evidence of oxidative stress in the pair-fed group, these measures do not discriminate between effects in different subcellular compartments. Because oxidative stress can cause specific responses in subcellular compartments, we assessed the compartmental effects of fructose and glucose by measuring the abundance of mitochondrial Trx2 and cytoplasmic/nuclear Prx2. The abundance of these key compartment-specific antioxidant proteins was assessed using Western blotting. When normalized to β-actin (Figure 6a), Trx2 abundance was significantly lower in the fructose-fed and glucose-fed groups (23% and 20% lower) respectively, compared to control (Figure 6b). In contrast to that of the carbohydrate fed mice, the pair-fed group had significantly higher (150%) abundance of hepatic Trx2 compared to control. No difference was observed for the cytoplasmic antioxidant Prx2. Measurement of a component of the mitochondrial respiratory apparatus, cytochrome c oxidase IV (COX-IV) was used as a control for mitochondrial abundance, and this showed that the content of mitochondria did not differ among the groups.
Figure 6.
(a) Western blots of mitochondrial (Trx2) and cytoplasmic (Prx2) redox proteins in the liver in different study groups. Equal amounts of protein were loaded (20 µg) in each well as indicated by similar β-actin abundance. Similar abundance of COX-IV (mitochondrial control) indicated equal loading of mitochondrial protein. Similar Prx2 abundance signifies no oxidative stress in cytoplasm. Trx2 abundance was decreased in fructose and glucose but increased in pair fed group; (b) When normalized to β-actin, Trx2 abundance decreased in fructose (77%) and glucose (80%) groups while it increased in pair fed (150%) group compared to control (100%). This indicates mitochondrial predisposition to oxidative stress in fructose and glucose groups. Different letters (a,b,c) indicate statistically significant difference among respective groups.
4. Discussion
In the present study, we used a controlled, pair-feeding protocol to test the hypothesis that decreased sulfur amino acid intake contributes to oxidative stress in an fructose-sweetened beverage model of fatty liver. Both fructose and glucose-fed mice developed fatty liver, but animals pair-fed with only sulfur amino acid deficiency did not. Fructose-fed and glucose-fed animals had similar total energy intake compared to control and displayed a similar decrease in hepatic Trx2 abundance when compared to controls. Pair-fed animals had similar sulfur amino acid intake as the fructose-fed mice, and showed increased Trx2 abundance in liver. Together, the results show that sulfur amino acid insufficiency is not the cause of oxidative stress in the models of fructose-sweetened liquid-induced fatty liver. Instead, the results suggest that disproportionately high energy intake from simple sugar (48% and 63% of total energy intake in fructose-fed and glucose-fed mice) may predispose mitochondria to oxidative stress. The carbohydrate-mediated decrease in Trx2 abundance is potentially important in terms of cell viability and liver damage, because Trx2 protects against oxidant-mediated apoptosis and can regulate the mitochondrial permeability transition [56,57].
Fructose-sweetened beverage intake is associated with decreased solid food and protein ingestion in obese and normal weight human subjects [34]. Raben et al. [35] showed a significant decrease in protein intake after consumption of sucrose-containing liquid. In rodents, Jurgens et al. [45] showed that after ad libitum fructose-containing liquid consumption, solid food intake was decreased, but total energy consumption was the same as controls. Our data are consistent with these previous studies showing that fructose-sweetened liquid consumption is associated with decreased solid food consumption, thus leading to insufficient sulfur amino acid intake. Deficiency of methionine, an essential amino acid, has been implicated in alcoholic liver disease and liver cirrhosis [10], secondary to its important role as a precursor of GSH. However, the potential role of dietary methionine in the pathogenesis of fatty liver does not appear to have been previously studied.
Our results on hepatic TG content are similar to those of Ngo Sock et al. [58], who recently showed that hepatic TG content was similar in glucose and fructose-fed rodents. Several metabolic effects of high-fructose diet such as obesity, fatty liver, and insulin resistance can also be observed with high-glucose diet [32,58,59,60,61]. Also, in the long term, the effects of high fructose and high glucose may not be different. As fructose-sweetened beverage consumption is associated with high energy intake [58,59,62], it is unclear whether these hyperenergetic conditions can account for the metabolic effects of fructose [58,59].
Most of the studies on fructose-sweetened liquid and fatty liver use products of lipid peroxidation as markers of oxidative stress and only few studies have evaluated enzymatic antioxidant systems [32,63]. To our knowledge, this is the first study evaluating hepatic mitochondrial and cytoplasmic antioxidant proteins and calculating the redox potentials of major thiol-disulfide couples in fructose-sweetened liquid model of fatty liver. Sumida et al. [64] showed a correlation between serum Trx levels and hepatic fat content in patients with fatty liver and proposed its usefulness in discriminating fatty liver from NASH. That study did not, however, evaluate hepatic Trx levels or specific Trx isoenzymes. Our study measured Trx2 abundance, which was decreased due to fructose and glucose feeding. These results suggest a predisposition to mitochondrial oxidative stress, which could be a pathogenic mechanism of fatty liver. This is different from a rodent study by Mellor et al. [25], which did not reveal any difference in myocardial Trx2 gene abundance due to a high fructose (60%) diet. This discrepancy could be explained by metabolic differences in these two organs as fructose is primarily metabolized in liver.
Machado et al. [63] showed that in patients with fatty liver, GSH metabolism is impaired towards oxidation, but plasma antioxidant markers do not correlate with hepatic redox states. We measured plasma redox potentials along with liver redox potentials to assess if there was any correlation between these two compartments. In our pair-fed group, hepatic EhCySS was reduced and Trx2 abundance increased; however plasma EhCySS was oxidized compared to control. These differences indicate that the redox compartments may act independently of each other [46]. Opposite redox effects in plasma and liver may be explained by energy restriction (40% of control in our study) leading to decreased metabolism in liver, which may result in less reactive oxygen species (ROS) formation in mitochondria. Alternatively, energy restriction can induce mitohormesis; an increased formation of ROS within mitochondria that causes an adaptive response providing stress resistance with a long-term reduction of oxidative stress [65]. Lastly, with the pair-fed animals being protein and energy restricted, they exhibited lower sulfur amino acid levels in both plasma and the liver. This can be explained by a marked reduction in protein synthesis and increase in protein half-lives; therefore, a lack of protein intake and decreased protein turnover could result in lower levels of tissue and circulating amino acids.
When comparing fructose-fed animals to glucose-fed animals, both groups had similar sulfur amino acid intake, total caloric intake, plasma and liver redox states and decrease in hepatic Trx2 abundance. A predisposition to hepatic mitochondrial oxidative stress as suggested by decreased Trx2 may be due to disproportionate energy intake from simple sugars, rather than decreased sulfur amino acid intake.
One of the limitations of our study was the design of the pair-fed group. We matched the fructose group for solid food intake but not for total energy intake. Because the restricted diet intake in the pair-fed animals also reduced caloric intake, a more precise design for the sulfur amino acid effect would be to supplement the diet composition of the pair-fed control group with non-carbohydrate energy sources (e.g., lipid) such that caloric intake in all four groups was similar. Future experiments with matched pair feeding according to macronutrient composition could potentially improve the models for fructose-sweetened liquid-induced fatty liver.
5. Conclusion
Fructose-sweetened liquid predisposes the liver to mitochondrial oxidative stress and causes fatty liver without plasma or cytoplasmic oxidative stress. The hypocaloric, pair-fed group displayed plasma, but not hepatic oxidative stress or fatty liver. Therefore, decreased sulfur amino acid intake, as occurs in models commonly used to study fructose-induced fatty liver, is not a cause of hepatic oxidative stress in this model and does not provide an explanation for fructose-induced lipid accumulation in this model.
Acknowledgments
This research was supported by grants from the National Institutes of Health (NIH) K23 DK080953 (M.B.V.), K24 RR023356 (T.R.Z.), R01 ES009047 (D.P.J.) and F32 ES019821 (J.R.R).
Implications
The study rules out a potential artifact of an important model used to study fructose-induced fatty liver. The study additionally shows the potential importance of mitochondrial oxidative stress in pathogenesis of fructose-induced fatty liver and that fructose and glucose-sweetened beverages may have similar hepatic metabolic, as evidenced by the equivalent liver TG outcomes, and redox effects.
Conflict of Interest
The authors declare no conflict of interest.
References
- 1.Vos M.B., Kimmons J.E., Gillespie C., Welsh J., Blanck H.M. Dietary fructose consumption among US children and adults: The Third National Health and Nutrition Examination Survey. Medscape J. Med. 2008;10:160. [PMC free article] [PubMed] [Google Scholar]
- 2.Wolf A., Bray G.A., Popkin B.M. A short history of beverages and how our body treats them. Obes. Rev. 2008;9:151–164. doi: 10.1111/j.1467-789X.2007.00389.x. [DOI] [PubMed] [Google Scholar]
- 3.Bray G.A., Nielsen S.J., Popkin B.M. Consumption of high-fructose corn syrup in beverages may play a role in the epidemic of obesity. Am. J. Clin. Nutr. 2004;79:537–543. doi: 10.1093/ajcn/79.4.537. [DOI] [PubMed] [Google Scholar]
- 4.Le K.A., Tappy L. Metabolic effects of fructose. Curr. Opin. Clin. Nutr. Metab. Care. 2006;9:469–475. doi: 10.1097/01.mco.0000232910.61612.4d. [DOI] [PubMed] [Google Scholar]
- 5.Havel P.J. Dietary fructose: Implications for dysregulation of energy homeostasis and lipid/carbohydrate metabolism. Nutr. Rev. 2005;63:133–157. doi: 10.1301/nr.2005.may.133-157. [DOI] [PubMed] [Google Scholar]
- 6.Bocarsly M.E., Powell E.S., Avena N.M., Hoebel B.G. High-fructose corn syrup causes characteristics of obesity in rats: Increased body weight, body fat and triglyceride levels. Pharmacol. Biochem. Behav. 2010;97:101–106. doi: 10.1016/j.pbb.2010.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anstee Q.M., Goldin R.D. Mouse models in non-alcoholic fatty liver disease and steatohepatitis research. Int. J. Exp. Pathol. 2006;87:1–16. doi: 10.1111/j.0959-9673.2006.00465.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Basciano H., Federico L., Adeli K. Fructose, insulin resistance, and metabolic dyslipidemia. Nutr. Metab. (Lond.) 2005;2:5. doi: 10.1186/1743-7075-2-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bizeau M.E., Pagliassotti M.J. Hepatic adaptations to sucrose and fructose. Metabolism. 2005;54:1189–1201. doi: 10.1016/j.metabol.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 10.Cave M., Deaciuc I., Mendez C., Song Z., Joshi-Barve S., Barve S., McClain C. Nonalcoholic fatty liver disease: Predisposing factors and the role of nutrition. J. Nutr. Biochem. 2007;18:184–195. doi: 10.1016/j.jnutbio.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 11.Howard B.V., Wylie-Rosett J. Sugar and cardiovascular disease: A statement for healthcare professionals from the Committee on Nutrition of the Council on Nutrition, Physical Activity, and Metabolism of the American Heart Association. Circulation. 2002;106:523–527. doi: 10.1161/01.cir.0000019552.77778.04. [DOI] [PubMed] [Google Scholar]
- 12.Le K.A., Bortolotti M. Role of dietary carbohydrates and macronutrients in the pathogenesis of nonalcoholic fatty liver disease. Curr. Opin. Clin. Nutr. Metab. Care. 2008;11:477–482. doi: 10.1097/MCO.0b013e328302f3ec. [DOI] [PubMed] [Google Scholar]
- 13.Stanhope K.L., Havel P.J. Fructose consumption: Recent results and their potential implications. Ann. N. Y. Acad. Sci. 2010;1190:15–24. doi: 10.1111/j.1749-6632.2009.05266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davail S., Rideau N., Bernadet M.D., Andre J.M., Guy G., Hoo-Paris R. Effects of dietary fructose on liver steatosis in overfed mule ducks. Horm. Metab. Res. 2005;37:32–35. doi: 10.1055/s-2005-861029. [DOI] [PubMed] [Google Scholar]
- 15.Mendeloff A.I., Weichselbaum T.E. Role of the human liver in the assimilation of intravenously administered fructose. Metabolism. 1953;2:450–458. [PubMed] [Google Scholar]
- 16.Ouyang X., Cirillo P., Sautin Y., McCall S., Bruchette J.L., Diehl A.M., Johnson R.J., Abdelmalek M.F. Fructose consumption as a risk factor for non-alcoholic fatty liver disease. J. Hepatol. 2008;48:993–999. doi: 10.1016/j.jhep.2008.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Assy N., Nasser G., Kamayse I., Nseir W., Beniashvili Z., Djibre A., Grosovski M. Soft drink consumption linked with fatty liver in the absence of traditional risk factors. Can. J. Gastroenterol. 2008;22:811–816. doi: 10.1155/2008/810961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huang D., Dhawan T., Young S., Yong W.H., Boros L.G., Heaney A.P. Fructose impairs glucose-induced hepatic triglyceride synthesis. Lipids Health Dis. 2011;10:20. doi: 10.1186/1476-511X-10-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wei Y., Wang D., Topczewski F., Pagliassotti M.J. Fructose-mediated stress signaling in the liver: Implications for hepatic insulin resistance. J. Nutr. Biochem. 2007;18:1–9. doi: 10.1016/j.jnutbio.2006.03.013. [DOI] [PubMed] [Google Scholar]
- 20.Bray G.A. Soft drink consumption and obesity: It is all about fructose. Curr. Opin. Lipidol. 2010;21:51–57. doi: 10.1097/MOL.0b013e3283346ca2. [DOI] [PubMed] [Google Scholar]
- 21.Busserolles J., Gueux E., Rock E., Mazur A., Rayssiguier Y. Substituting honey for refined carbohydrates protects rats from hypertriglyceridemic and prooxidative effects of fructose. J. Nutr. 2002;132:3379–3382. doi: 10.1093/jn/132.11.3379. [DOI] [PubMed] [Google Scholar]
- 22.Busserolles J., Gueux E., Rock E., Demigne C., Mazur A., Rayssiguier Y. Oligofructose protects against the hypertriglyceridemic and pro-oxidative effects of a high fructose diet in rats. J. Nutr. 2003;133:1903–1908. doi: 10.1093/jn/133.6.1903. [DOI] [PubMed] [Google Scholar]
- 23.Wei Y., Wang D., Pagliassotti M.J. Fructose selectively modulates c-jun N-terminal kinase activity and insulin signaling in rat primary hepatocytes. J. Nutr. 2005;135:1642–1646. doi: 10.1093/jn/135.7.1642. [DOI] [PubMed] [Google Scholar]
- 24.Vos M.B., Weber M.B., Welsh J., Khatoon F., Jones D.P., Whitington P.F., McClain C.J. Fructose and oxidized low-density lipoprotein in pediatric nonalcoholic fatty liver disease: A pilot study. Arch. Pediatr. Adolesc. Med. 2009;163:674–675. doi: 10.1001/archpediatrics.2009.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mellor K., Ritchie R.H., Meredith G., Woodman O.L., Morris M.J., Delbridge L.M. High-fructose diet elevates myocardial superoxide generation in mice in the absence of cardiac hypertrophy. Nutrition. 2010;26:842–848. doi: 10.1016/j.nut.2009.08.017. [DOI] [PubMed] [Google Scholar]
- 26.Kelley G.L., Allan G., Azhar S. High dietary fructose induces a hepatic stress response resulting in cholesterol and lipid dysregulation. Endocrinology. 2004;145:548–555. doi: 10.1210/en.2003-1167. [DOI] [PubMed] [Google Scholar]
- 27.Lee O., Bruce W.R., Dong Q., Bruce J., Mehta R., O’Brien P.J. Fructose and carbonyl metabolites as endogenous toxins. Chem. Biol. Interact. 2009;178:332–339. doi: 10.1016/j.cbi.2008.10.011. [DOI] [PubMed] [Google Scholar]
- 28.Nseir W., Nassar F., Assy N. Soft drinks consumption and nonalcoholic fatty liver disease. World J. Gastroenterol. 2010;16:2579–2588. doi: 10.3748/wjg.v16.i21.2579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Du D., Shi Y.H., Le G.W. Oxidative stress induced by high-glucose diet in liver of C57BL/6J mice and its underlying mechanism. Mol. Biol. Rep. 2010;37:3833–3839. doi: 10.1007/s11033-010-0039-9. [DOI] [PubMed] [Google Scholar]
- 30.Delbosc S., Paizanis E., Magous R., Araiz C., Dimo T., Cristol J.P., Cros G., Azay J. Involvement of oxidative stress and NADPH oxidase activation in the development of cardiovascular complications in a model of insulin resistance, the fructose-fed rat. Atherosclerosis. 2005;179:43–49. doi: 10.1016/j.atherosclerosis.2004.10.018. [DOI] [PubMed] [Google Scholar]
- 31.Nyby M.D., Abedi K., Smutko V., Eslami P., Tuck M.L. Vascular Angiotensin type 1 receptor expression is associated with vascular dysfunction, oxidative stress and inflammation in fructose-fed rats. Hypertens. Res. 2007;30:451–457. doi: 10.1291/hypres.30.451. [DOI] [PubMed] [Google Scholar]
- 32.Du D., Shi Y.H., Le G.W. Oxidative stress induced by high-glucose diet in liver of C57BL/6J mice and its underlying mechanism. Mol. Biol. Rep. 2010;37:3833–3839. doi: 10.1007/s11033-010-0039-9. [DOI] [PubMed] [Google Scholar]
- 33.Miller A., Adeli K. Dietary fructose and the metabolic syndrome. Curr. Opin. Gastroenterol. 2008;24:204–209. doi: 10.1097/MOG.0b013e3282f3f4c4. [DOI] [PubMed] [Google Scholar]
- 34.Rodin J. Comparative effects of fructose, aspartame, glucose, and water preloads on calorie and macronutrient inta. Am. J. Clin. Nutr. 1990;51:428–435. doi: 10.1093/ajcn/51.3.428. [DOI] [PubMed] [Google Scholar]
- 35.Raben A., Vasilaras T.H., Moller A.C., Astrup A. Sucrose compared with artificial sweeteners: Different effects on ad libitum food intake and body weight after 10 wk of supplementation in overweight subjects. Am. J. Clin. Nutr. 2002;76:721–729. doi: 10.1093/ajcn/76.4.721. [DOI] [PubMed] [Google Scholar]
- 36.Vartanian L.R., Schwartz M.B., Brownell K.D. Effects of soft drink consumption on nutrition and health: A systematic review and meta-analysis. Am. J. Public Health. 2007;97:667–675. doi: 10.2105/AJPH.2005.083782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.DiMeglio D.P., Mattes R.D. Liquid versus solid carbohydrate: Effects on food intake and body weight. Int. J. Obes. Relat. Metab. Disord. 2000;24:794–800. doi: 10.1038/sj.ijo.0801229. [DOI] [PubMed] [Google Scholar]
- 38.Tordoff M.G., Alleva A.M. Effect of drinking soda sweetened with aspartame or high-fructose corn syrup on food intake and body weight. Am. J. Clin. Nutr. 1990;51:963–969. doi: 10.1093/ajcn/51.6.963. [DOI] [PubMed] [Google Scholar]
- 39.De Castro J.M. The effects of the spontaneous ingestion of particular foods or beverages on the meal pattern and overall nutrient intake of humans. Physiol. Behav. 1993;53:1133–1144. doi: 10.1016/0031-9384(93)90370-u. [DOI] [PubMed] [Google Scholar]
- 40.Mattes R.D. Dietary compensation by humans for supplemental energy provided as ethanol or carbohydrate in fluids. Physiol. Behav. 1996;59:179–187. doi: 10.1016/0031-9384(95)02007-1. [DOI] [PubMed] [Google Scholar]
- 41.Reid M., Hammersley R., Hill A.J., Skidmore P. Long-term dietary compensation for added sugar: Effects of supplementary sucrose drinks over a 4-week period. Br. J. Nutr. 2007;97:193–203. doi: 10.1017/S0007114507252705. [DOI] [PubMed] [Google Scholar]
- 42.Mattes R.D., Campbell W.W. Effects of food form and timing of ingestion on appetite and energy intake in lean young adults and in young adults with obesity. J. Am. Diet. Assoc. 2009;109:430–437. doi: 10.1016/j.jada.2008.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mattes R.D. Fluid energy-Where’s the problem? J. Am. Diet. Assoc. 2006;106:1956–1961. doi: 10.1016/j.jada.2006.10.026. [DOI] [PubMed] [Google Scholar]
- 44.Bergheim I., Weber S., Vos M., Kramer S., Volynets V., Kaserouni S., McClain C.J., Bischoff S.C. Antibiotics protect against fructose-induced hepatic lipid accumulation in mice: Role of endotoxin. J. Hepatol. 2008;48:983–992. doi: 10.1016/j.jhep.2008.01.035. [DOI] [PubMed] [Google Scholar]
- 45.Jurgens H., Haass W., Castaneda T.R., Schurmann A., Koebnick C., Dombrowski F., Otto B., Nawrocki A.R., Scherer P.E., Spranger J., et al. Consuming fructose-sweetened beverages increases body adiposity in mice. Obes. Res. 2005;13:1146–1156. doi: 10.1038/oby.2005.136. [DOI] [PubMed] [Google Scholar]
- 46.Go Y.M., Jones D.P. Redox compartmentalization in eukaryotic cells. Biochim. Biophys. Acta. 2008;1780:1273–1290. doi: 10.1016/j.bbagen.2008.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jones D.P., Liang Y. Measuring the poise of thiol/disulfide couples in vivo. Free Radic. Biol. Med. 2009;47:1329–1338. doi: 10.1016/j.freeradbiomed.2009.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jones D.P., Park Y., Gletsu-Miller N., Liang Y., Yu T., Accardi C.J., Ziegler T.R. Dietary sulfur amino acid effects on fasting plasma cysteine/cystine redox potential in humans. Nutrition. 2011;27:199–205. doi: 10.1016/j.nut.2010.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nkabyo Y.S., Gu L.H., Jones D.P., Ziegler T.R. Thiol/disulfide redox status is oxidized in plasma and small intestinal and colonic mucosa of rats with inadequate sulfur amino acid intake. J. Nutr. 2006;136:1242–1248. doi: 10.1093/jn/136.5.1242. [DOI] [PubMed] [Google Scholar]
- 50.Jonas C.R., Estivariz C.F., Jones D.P., Gu L.H., Wallace T.M., Diaz E.E., Pascal R.R., Cotsonis G.A., Ziegler T.R. Keratinocyte growth factor enhances glutathione redox state in rat intestinal mucosa during nutritional repletion. J. Nutr. 1999;129:1278–1284. doi: 10.1093/jn/129.7.1278. [DOI] [PubMed] [Google Scholar]
- 51.Ishii S., Iizuka K., Miller B.C., Uyeda K. Carbohydrate response element protein directly promotes lipogenic enzyme gene transcription. Proc. Natl. Acad. Sci. USA. 2004;101:15597–15602. doi: 10.1073/pnas.0405238101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jones D.P., Carlson J.L., Mody V.C., Cai J., Lynn M.J., Sternberg P. Redox state of glutathione in human plasma. Free Radic. Biol. Med. 2000;28:625–635. doi: 10.1016/s0891-5849(99)00275-0. [DOI] [PubMed] [Google Scholar]
- 53.Jones D.P., Carlson J.L., Samiec P.S., Sternberg P., Jr., Mody V.C., Jr., Reed R.L., Brown L.A. Glutathione measurement in human plasma. Evaluation of sample collection, storage and derivatization conditions for analysis of dansyl derivatives by HPLC. Clin. Chim. Acta. 1998;275:175–184. doi: 10.1016/S0009-8981(98)00089-8. [DOI] [PubMed] [Google Scholar]
- 54.Johnson J.M., Strobel F.H., Reed M., Pohl J., Jones D.P. A rapid LC-FTMS method for the analysis of cysteine, cystine and cysteine/cystine steady-state redox potential in human plasma. Clin. Chim. Acta. 2008;396:43–48. doi: 10.1016/j.cca.2008.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Halvey P.J., Watson W.H., Hansen J.M., Go Y.M., Samali A., Jones D.P. Compartmental oxidation of thiol-disulphide redox couples during epidermal growth factor signalling. Biochem. J. 2005;386:215–219. doi: 10.1042/BJ20041829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.He M., Cai J., Go Y.M., Johnson J.M., Martin W.D., Hansen J.M., Jones D.P. Identification of thioredoxin-2 as a regulator of the mitochondrial permeability transition. Toxicol. Sci. 2008;105:44–50. doi: 10.1093/toxsci/kfn116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chen Y., Yu M., Jones D.P., Greenamyre J.T., Cai J. Protection against oxidant-induced apoptosis by mitochondrial thioredoxin in SH-SY5Y neuroblastoma cells. Toxicol. Appl. Pharmacol. 2006;216:256–262. doi: 10.1016/j.taap.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 58.Ngo Sock E.T., Le K.A., Ith M., Kreis R., Boesch C., Tappy L. Effects of a short-term overfeeding with fructose or glucose in healthy young males. Br. J. Nutr. 2010;103:939–943. doi: 10.1017/S0007114509992819. [DOI] [PubMed] [Google Scholar]
- 59.Tappy L., Le K.A., Tran C., Paquot N. Fructose and metabolic diseases: New findings, new questions. Nutrition. 2010;26:1044–1049. doi: 10.1016/j.nut.2010.02.014. [DOI] [PubMed] [Google Scholar]
- 60.McDevitt R.M., Bott S.J., Harding M., Coward W.A., Bluck L.J., Prentice A.M. De novo lipogenesis during controlled overfeeding with sucrose or glucose in lean and obese women. Am. J. Clin. Nutr. 2001;74:737–746. doi: 10.1093/ajcn/74.6.737. [DOI] [PubMed] [Google Scholar]
- 61.Stanhope K.L., Schwarz J.M., Keim N.L., Griffen S.C., Bremer A.A., Graham J.L., Hatcher B., Cox C.L., Dyachenko A., Zhang W., et al. Consuming fructose-sweetened, not glucose-sweetened, beverages increases visceral adiposity and lipids and decreases insulin sensitivity in overweight/obese human. J. Clin. Invest. 2009;119:1322–1334. doi: 10.1172/JCI37385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tappy L., Le K.A. Metabolic effects of fructose and the worldwide increase in obesity. Physiol. Rev. 2010;90:23–46. doi: 10.1152/physrev.00019.2009. [DOI] [PubMed] [Google Scholar]
- 63.Machado M.V., Ravasco P., Jesus L., Marques-Vidal P., Oliveira C.R., Proenca T., Baldeiras I., Camilo M.E., Cortez-Pinto H. Blood oxidative stress markers in non-alcoholic steatohepatitis and how it correlates with diet. Scand. J. Gastroenterol. 2008;43:95–102. doi: 10.1080/00365520701559003. [DOI] [PubMed] [Google Scholar]
- 64.Sumida Y., Nakashima T., Yoh T., Furutani M., Hirohama A., Kakisaka Y., Nakajima Y., Ishikawa H., Mitsuyoshi H., Okanoue T., et al. Serum thioredoxin levels as a predictor of steatohepatitis in patients with nonalcoholic fatty liver disease. J. Hepatol. 2003;38:32–38. doi: 10.1016/s0168-8278(02)00331-8. [DOI] [PubMed] [Google Scholar]
- 65.Ristow M., Zarse K. How increased oxidative stress promotes longevity and metabolic health: The concept of mitochondrial hormesis (mitohormesis) Exp. Gerontol. 2010;45:410–418. doi: 10.1016/j.exger.2010.03.014. [DOI] [PubMed] [Google Scholar]