Abstract
Background
Few studies measure physical activity objectively or at multiple time points during postpartum. We describe physical activity at 3- and 12-months postpartum among a cohort of women using both self-reported and objective measures.
Methods
In total, 181 women completed the 3-month postpartum measures, and 204 women completed the 12-month postpartum measures. Participants wore an Actigraph accelerometer for one week and completed in-home interviews that included questions on physical activity. A cohort of 80 women participated at both time points. Poisson regression models were used to determine whether physical activity differed over time for the cohort.
Results
For the cohort, average counts/minute were 364 at 3-months postpartum and 394 at 12-months postpartum. At both time periods for the cohort, vigorous activity averaged 1 to 3 minutes/day, and moderate activity (NHANES cutpoints) averaged 16 minutes/day. Sedentary time averaged 9.3 hours at 3-months postpartum and 8.8 hours at 12-months postpartum, out of a 19-hour day. Average counts/minute increased and sedentary behavior declined from 3- to 12-months postpartum.
Conclusion
Interventions are needed to help women integrate more moderate to vigorous physical activity and to capitalize on the improvements in sedentary behavior that occur during postpartum.
Introduction
The postpartum period, which extends to one year following the birth of a baby, is a time of transitioning health behaviors for many women. In fact, it may be an opportune time to target interventions to engage more women in physical activity, especially with the high proportion of women retaining gestational weight or gaining further weight.1, 2 A growing body of research supports the benefits of physical activity during postpartum, including improved psychosocial well being, less anxiety and depression, improved cardiovascular fitness, less lactation-induced bone loss, and less urinary stress incontinence.1, 3-5
In support of this, statements on or guidelines for physical activity during pregnancy, with sections addressing postpartum activity, are currently endorsed from several physician organizations in Canada,6 the United Kingdom,7 and the United States (US).8 For example, the 2002 American College of Obstetrics and Gynecology (ACOG) guidelines for pregnant and postpartum women state that prepregnancy exercise routines may be resumed gradually after giving birth, as soon as it is medically and physically safe to do so.8 The guidelines note that many of the physiologic and morphologic changes of pregnancy persist 4 to 6 weeks postpartum but do not provide other specific information regarding postpartum activity. In addition, the US government included a section on pregnancy and postpartum recommendations in its “2008 Physical Activity Guidelines for Americans”.5
Epidemiologic studies of postpartum physical activity generally rely on self-reported physical activity, and even fewer assess physical activity at multiple time points during postpartum. The advantage to more objective measures of physical activity is that they minimize respondent and recall bias. We identified only one study that assessed physical activity during postpartum using objective measures. At 3-months postpartum, 44 low-income women wore a pedometer for three days and recorded an average daily step count of 6262.9 One limitation of this study was the reliance on the women to record the step count each day; this protocol also provided feedback to the participants, which may have influenced their physical activity.
The primary purpose of this study was to describe physical activity at 3- and 12-months postpartum among a cohort of women using both self-reported and objective measures (accelerometry). Secondarily, we sought to describe in detail the methods for imputation used with the accelerometer data, expanded from an article by Catellier et al,10 that can be replicated by others.
Methods
Study
The third phase of the Pregnancy, Infection, and Nutrition (PIN3) Study recruited pregnant women at less than 20 weeks’ gestation seeking prenatal care at clinics associated with the University of North Carolina Hospitals. Trained staff identified women through review of all medical charts of new prenatal patients. Women were not enrolled if they were non-English speaking, under the age of 16 years, carrying multiple gestations, not planning to continue care or deliver at the study hospital, or did not have a telephone from which they could complete the phone interviews. Recruitment began in January 2001 and continued through 2005, with the last birth occurring in December 2005.
The PIN Postpartum Study extended the PIN3 Study, by adding data collection for a subset of study participants who delivered between October 2002 and December 2005. The women who continued to live in the study area and did not become pregnant again were invited to participate in a 3-month and 12-month home visit for data collection. In total, 688 women participated at 3-months postpartum and 550 women participated at 12-months postpartum. The accelerometer portion of the study was added to the cohort procedures in November 2004, with 316 women eligible at 3-months postpartum and 411 women eligible at 12-months postpartum.
Details on reasons for dropout and assessment of selection bias for the PIN3 and PIN Postpartum Study can be found elsewhere.11-13 The study website (http://www.cpc.unc.edu/pin) also provides greater detail on the protocols. All data collection described herein was approved by the University of North Carolina - Chapel Hill Institutional Review Board, and each participant provided their informed consent prior to participation in the studies.
Objective Measurement of Physical Activity
A substudy was conducted among 3- and 12-month postpartum women enrolled into the PIN3 Postpartum Study to collect objectively measured physical activity using the Manufacturing Technology Inc. (MTI) ActiGraph accelerometer. The ActiGraph model #7164 is a small, light-weight uniaxial accelerometer that measures accelerations in the range of 0.05 to 2 G’s with a band limited frequency of 0.25-2.5 Hertz.14 Validity of the monitor as an indicator for physical activity has been demonstrated among adults.15-17 The ActiGraph has also been shown to be a technically reliable instrument, able to detect differing levels of intensity.17-22
From November 2004 to December 2006, women participating in the PIN Postpartum Study were asked to wear the accelerometer for one week at the conclusion of their 3- and 12-month home visits. If they agreed, women were fitted with the accelerometer to be worn on a belt or clip-on pouch over their right hip at the iliac crest. They were asked to remove the monitor for sleeping, bathing, or swimming. Written and verbal instructions, as well as a phone number to call with questions, were provided. Participants mailed the monitor back to the study offices at the conclusion of the 7 days. In thanks for their time, women received $30 at 3-months postpartum and $40 at 12-months postpartum.
ActiGraph accelerometer data were collected with 1-minute epochs, and the monitors were regularly calibrated throughout the study using the calibration machine from MTI. We used an optional setting on the Actigraph to also collect step counts per epoch, as well as counts. Spurious counts or steps were flagged, assessed, and set to missing if determined to be invalid. We defined non-wear time for the accelerometry counts as a period of 60 minutes or more of zeros based on prior work with the data.23 Others 24 report acceptable performance of the step count function, with no differences between actual steps and accelerometer determined steps, except at slow walking speeds. In light of evidence of over-counting of steps during slow walking by the particular Actigraph in use (model #7164), we followed the approach of Tudor-Locket et al 25 and censored the step counts associated with low activity (activity counts below 500/minute). We provide results with and without censored step counts.
Ignoring missing values from the accelerometer can lead to biased estimates of the true level of physical activity.10 Therefore, missing data for both counts and steps were filled by multiple imputation (using SAS MI procedure) through a Markov chain Monte Carlo method. Considering the wearing time of our participants, non-missing accelerometer data falling into the daily time window of 5am to midnight was selected as reference data for the imputation. Indicators of time of day (5am-<6am, 6am-<7am, 7am-<8am, 8am-<12pm,12pm-<2pm, 2pm-<4pm, 4pm-<6pm, 6pm-<8pm, 8pm-<10pm, 10pm-<12am) and weekday versus weekend were used for the imputation procedure. Ten imputed data sets were created and each imputation contained minute-by-minute daily activity counts and step data from 5am to 12am.
From the accelerometer, we used the data several ways. First, using counts per minute, we evaluated the raw data provided by the accelerometer without imposing cutpoint decisions. Second, physical activity was calculated as minutes per day (using count thresholds) spent in differing intensities (e.g., light, moderate, vigorous). A number of calibration studies of adults provide count thresholds (e.g., cutpoints) for moderate and vigorous activity. We calculated cutpoints using three of these studies: Freedson et al,15 Swartz et al,26 and summary cutpoints from National Heath and Nutrition Examination Survey (NHANES) data by Troiano et al,27 calculated originally by taking the weighted average of cutpoints from Freedson et al,15 Yngve et al,28 Leenders et al,29 and Brage et al.17 We also classified inactivity at a count of less than or equal to 100 counts per minute.30 Third, using relative values, we report the average percent time per day spent in activity, using threshold cutpoints. Lastly, we used the step data to report censored and uncensored step counts per day.
Self-reported Measure of Physical Activity
At the time PIN3 began, there were no physical activity questionnaires tailored to pregnant women, so a one-week recall questionnaire was developed to be used consecutively during pregnancy and postpartum. The questionnaire was interviewer administered and designed to capture moderate and vigorous activity in the past week, with evidence for validity and reliability reported elsewhere.31 The questionnaire assessed frequency and duration of all moderate and vigorous physical activities the woman participated in, including activity done at work, leisure, for transportation, childcare, adult care, and both indoor and outdoor household activities. Intensity of activity was assessed (i) using a modified Borg scale32 to capture the participant’s perception of intensity, and (ii) using published metabolic equivalent (MET) tables.33, 34 This physical activity questionnaire provided an estimate of (i) the total number of minutes in the past week of moderate and vigorous physical activity, based on their perceived intensity of the activity or classified based on established MET intensities; and (ii) the total number of MET-minutes per week spent in physical activity, based on established MET intensities. Moderate activity was defined two ways: at least 3 METS and at least 4.8 METS (this corresponded to the lower level MET range for moderate activity among 20 to 39 year olds 35). The questionnaire also provided information by mode (e.g., leisure, work, outdoor/indoor household, child/adult care, and transportation activity), for specific activities or groups of activities (e.g., walking, outdoor activities), or by intensity (e.g., moderate, vigorous). This questionnaire was collected similarly during both the 3-month and 12-month postpartum in-home interviews.
Other Measures
Women were asked about their race/ethnicity, education, and parity (live plus still births) during pregnancy. At the 3- and 12-month postpartum in-home interview, women were asked to report their work status, marital status, number of children living in the home, and whether or not they were breastfeeding. Race/ethnicity, education, parity, and general health were collected during pregnancy. Weight and height were measured at the in-home visits for the determination of body mass index (BMI). BMI values were grouped into low (<18.5 kg/m2), normal weight (18.5-<25.0 kg/m2), overweight (25.0-<30.0 kg/m2), and obese (>=30.0 kg/m2).36
Statistical Analysis
All statistical analyses were conducted using SAS version 9.2 (Cary, NC). The relative percentages, means, and medians with interquartile ranges (IQR) of physical activity were reported separately for the 3- and 12-month postpartum women. Accelerometer wear time and percent of data imputed were graphed using SAS. Box and whisker plots of physical activity were graphed using R 37 to compare over time and by whether imputation was used. Participants in the cohort (providing accelerometer data at both 3- and 12-months postpartum) were compared to those who were eligible but did not participate at both time periods using chi-squared tests for categorical measures and nonparametric Mann-Whitney tests for continuous measures.
Adjusted Poisson generalized estimating equations (GEE) for repeated count measures,38 using an independence working correlation, were used to test whether the change in physical activity across the two time points was different among the cohort, with significance set at p<0.05.39 The goodness-of-fit statistics of all models indicated over dispersion, therefore the Pearson scaling adjustment was applied. Adjusted factors included age, education, BMI at 3-months postpartum, and change in BMI from 3- to 12-months postpartum. Other factors were considered but did not confound the associations (marital status, race/ethnicity, general health, parity). We also compared the findings from the accelerometer to the questionnaire using Spearman correlation coefficients with 95% confidence intervals (CI). The SAS MIANALYZE procedure was used to combine results across the ten imputed sets of data.
Results
Description of Sample
In total, 181 of 316 (57%) eligible women completed the 3-month measures and 204 of 411 (50%) eligible women completed the 12-month measures, which included wearing an accelerometer and completing an in-home interview that asked about physical activity. The reasons eligible women did not wear the accelerometer are provided in Table 1. Among these 305 participants, 80 women completed both the 3- and 12-month accelerometer assessments. A description of these women is provided in Table 2.
Table 1.
Enrollment and data collection* among PIN Postpartum Study participants at 3- and 12-months postpartum
| 3-months Postpartum (n=316) |
12-months Postpartum (n=411) |
|||
|---|---|---|---|---|
| n | % | n | % | |
| Successfully enrolled and completed data collection |
181 | 57.3 | 204 | 49.6 |
| Did not enroll due to: | ||||
| … lack of interest or time | 40 | 12.7 | 51 | 12.4 |
| … moving or vacation/travel | 5 | 1.6 | 22 | 5.3 |
| …concern by staff so not invited | 14 | 4.4 | 21 | 5.1 |
| …lack of available accelerometer at the home visit |
15 | 4.8 | 16 | 3.9 |
| …visit at home was time constrained so not invited to participate |
6 | 1.9 | 8 | 2 |
| …ineligibility due to 3-month results | 0 | 0 | 15 | 3.6 |
| …other reasons | 2 | 0.6 | 8 | 2 |
| Successfully enrolled but did not complete data collection because: | ||||
| …did not wear accelerometer or monitor malfunction |
45 | 14.2 | 53 | 12.9 |
| …accelerometer was lost, broken, or never returned |
8 | 2.5 | 13 | 3.2 |
Successful enrollment was defined as completing the consent form and receiving an accelerometer. Successful data collection was defined by wearing the accelerometer and returning it to the study without monitor malfunction. In total, 688 women participated at 3-months postpartum and 550 women participated at 12-months postpartum in the PIN Postpartum Study starting in October 2002. The accelerometer portion of the study was added to the cohort in November 2004, with 316 women eligible at 3-months postpartum and 411 women eligible at 12-months postpartum.
Table 2.
| 3-months Postpartum |
12-months Postpartum |
Cohort* | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| (n=181) | (n=204) | (n=80) | ||||
|
|
|
|||||
| n | % | n | % | n | % | |
| Age in years | ||||||
| <20 | 2 | 1 | 1 | 0 | 0 | 0 |
| 20-29 | 79 | 44 | 59 | 29 | 32 | 40 |
| ≥30 | 100 | 55 | 144 | 71 | 48 | 60 |
| Marital status | ||||||
| Not married | 27 | 15 | 20 | 10 | 7 | 9 |
| Married | 154 | 85 | 184 | 90 | 73 | 91 |
| Race/Ethnicity (assessed once during pregnancy) | ||||||
| Nonhispanic White | 133 | 73 | 167 | 82 | 64 | 80 |
| Nonhispanic Black | 32 | 18 | 21 | 10 | 8 | 10 |
| Other | 16 | 9 | 16 | 8 | 8 | 10 |
| Education in years (assessed once during pregnancy) | ||||||
| <=12 | 25 | 14 | 25 | 12 | 11 | 14 |
| 13-15 | 41 | 23 | 34 | 17 | 16 | 20 |
| >=16 | 115 | 64 | 145 | 71 | 53 | 66 |
| General health (assessed once during pregnancy) | ||||||
| Excellent | 68 | 38 | 73 | 36 | 26 | 33 |
| Very Good | 73 | 40 | 87 | 43 | 31 | 39 |
| Good | 31 | 17 | 35 | 17 | 18 | 23 |
| Fair/Poor | 9 | 5 | 9 | 4 | 5 | 6 |
| Body mass index (kg/m^2) | ||||||
| Low (<18.5) | 0 | 0 | 6 | 3 | 0 | 0 |
| Normal (18.5 to <25.0) | 72 | 40 | 112 | 55 | 34 | 43 |
| Overweight (25.0 to <30.0) | 54 | 30 | 45 | 22 | 23 | 29 |
| Obese (>=30.0) | 55 | 30 | 41 | 20 | 23 | 29 |
| Parity (assessed once during pregnancy) | ||||||
| 0 | 87 | 48 | 101 | 50 | 38 | 48 |
| 1 | 65 | 36 | 71 | 35 | 27 | 34 |
| 2 | 20 | 11 | 24 | 12 | 11 | 14 |
| 3+ | 9 | 5 | 8 | 4 | 4 | 5 |
| Number of children in home | ||||||
| 1 | 82 | 45 | 94 | 46 | 37 | 46 |
| 2 | 72 | 40 | 78 | 38 | 29 | 36 |
| 3+ | 27 | 15 | 32 | 16 | 14 | 18 |
| Working status | ||||||
| Not employed | 94 | 52 | 68 | 33 | 40 | 50 |
| Employed | 87 | 48 | 136 | 67 | 40 | 50 |
| Breastfeeding | ||||||
| No | 60 | 33 | 144 | 71 | 21 | 26 |
| Yes | 121 | 67 | 60 | 29 | 59 | 74 |
Measures were from 3-month postpartum interview unless indicated otherwise.
The cohort was defined as participants that completed the accelerometer portion of the study at both 3- and 12-months postpartum.
Women in the cohort were more likely to be married at 3-months postpartum compared to women who were eligible but were not in the cohort (Online Table 1). Otherwise, women in the cohort (n=80) were similar (p>0.05) to eligible women who were not included in the cohort at 3- (n=236) and 12-months postpartum (n=331) when exploring age, race/ethnicity, education, general health, BMI category, parity, number of children in the home, working status, breastfeeding, and self-reported total physical activity.
Objectively-Measured Physical Activity
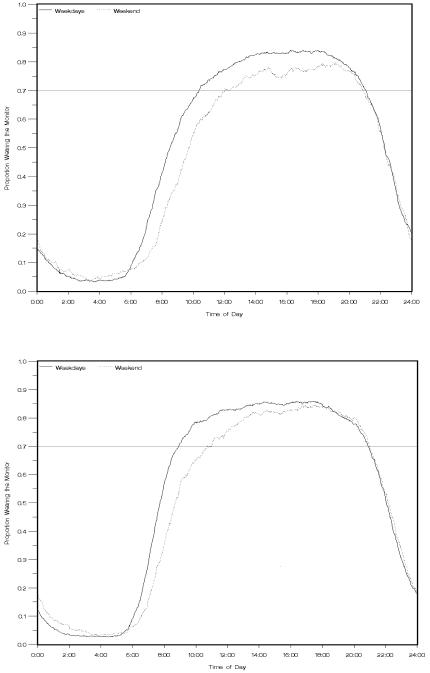
For all participants, average wearing time was 12.2 hours/day (median 12.9 hours/day) at 3-months postpartum and 12.8 hours/day (median 13.2 hours/day) at 12-months postpartum. The wearing time of the accelerometer, separately for weekdays and weekends, is shown in Figure 1 for all 3-month and 12-month postpartum participants. At 3-months postpartum, on the weekdays at least 70% of the women wore the accelerometer from 10:23am to 9:03pm (10.7 hours), and on the weekends at least 70% wore it from 12:00pm to 8:55pm (8.8 hours). At 12-months postpartum, on the weekdays at least 70% of the women wore the accelerometer from 8:54am to 8:53pm (10.3 hours), and on the weekends at least 70% wore it from 10:43am to 8:59pm (12.0 hours). These values, separately for weekdays and weekends and for 3- and 12-months postpartum, were multiplied by 70%, and the resulting values corresponded to our definition of a “compliant day”.
Figure 1.
Cumulative proportion of postpartum participants wearing the accelerometer by time of day, separately for weekdays and weekends. The top graph represents 3-months postpartum women (n=181) and the bottom graph represents 12-months postpartum women (n=204).
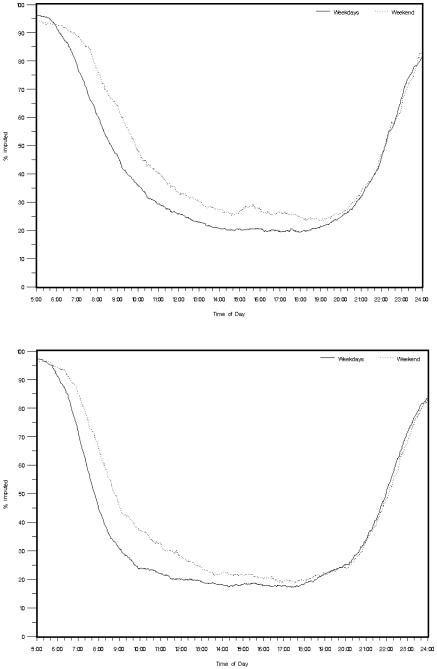
Figure 2 illustrates that most imputation occurred in early mornings and late evenings. Among the counts that were imputed, at 3-months postpartum 43.7% of imputed counts (18.5% of all counts) occurred between 8am and 8pm and 56.3% of imputed counts (23.9% of all counts) occurred earlier (5am-8am) or later (8pm-12am). Similarly at 12-months postpartum, 38.5% of imputed counts (14.9% of all counts) occurred between 8am and 8pm and 61.5% of imputed counts (23.8% of all counts) occurred earlier (5am-8am) or later (8pm-12am).
Figure 2.
Proportion of imputed data by time of day at 3-months (top graph) and 12-months (bottom graph) postpartum (sample size for both figures is on the cohort of 80 women using the 10 imputed datasets)
For the overall sample, average counts per minute were 371 at 3-months postpartum and 392 at 12-months postpartum (Table 3). Findings using either the Troiano or Freedson cutpoints were similar, due to the similarity in the cutpoint value. Thus, we do not present moderate or vigorous activity results using the Freedson cutpoint in the tables. Regardless of the cutpoint used, vigorous activity averaged approximately 1 to 2 minutes/day at both time periods. However, moderate activity averaged 17 to 21 minutes/day using Troiano or Freedson cutpoints, but 276 to 287 minutes/day using Swartz cutpoints. Sedentary time averaged 9.2 hours at 3-months postpartum and 8.9 hours at 12-months postpartum. When data were expressed relative to the total wear time, less than 1% of the day was spent in vigorous activities, and 1 to 2% of the day was spent in moderate activities using the Troiano or Freedson cutpoints. Forty-seven to 49% of the day was spent in sedentary behavior. Total average censored steps per day were 15,093 at 3-months and 14,295 at 12-months postpartum.
Table 3.
Accelerometry results for participants at 3- and 12-months postpartum using imputed data, overall and among the cohort
| 3-months Postpartum | 12-months Postpartum | 3-months Postpartum | 12-months Postpartum | p value* | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||||||
| (n=181) | (n=204) | Cohort** (n=80) | Cohort** (n=80) | ||||||||||
|
|
|
||||||||||||
| Mean | Median | IQR | Mean | Median | IQR | Mean | Median | IQR | Mean | Median | IQR | ||
| Counts per minute | 371 | 366 | 329-412 | 392 | 386 | 338-439 | 364 | 357 | 317-408 | 394 | 386 | 347-450 | 0.001 |
| Absolute values (minutes per day): | |||||||||||||
| Troiano et al cutpoints | |||||||||||||
| Light | 1122 | 1126 | 1118-1131 | 1119 | 1122 | 1112-1130 | 1123 | 1126 | 1117-1131 | 1122 | 1125 | 1116-1131 | 0.69 |
| Moderate | 17 | 13 | 9-21 | 19 | 17 | 10-25 | 16 | 13 | 9-21 | 16 | 14 | 9-20 | 0.91 |
| Vigorous | 1 | 0 | 0-0 | 2 | 0 | 0-1 | 1 | 0 | 0-0 | 2 | 0 | 0-1 | 0.22 |
| Swartz et al cutpoints | |||||||||||||
| Light | 862 | 865 | 828-906 | 851 | 857 | 810-900 | 868 | 871 | 841-908 | 845 | 844 | 801-893 | 0.004 |
| Moderate | 276 | 274 | 233-309 | 287 | 279 | 239-328 | 270 | 268 | 230-297 | 293 | 293 | 241-338 | 0.005 |
| Vigorous | 2 | 0 | 0-1 | 2 | 0 | 0-2 | 2 | 0 | 0-1 | 3 | 0 | 0-3 | 0.32 |
| Sedentary behavior | 554 | 555 | 507-600 | 532 | 530 | 479-582 | 560 | 563 | 521-611 | 525 | 517 | 475-570 | <0.001 |
| Relative values (% time per day): | |||||||||||||
| Troiano et al cutpoints | |||||||||||||
| Light | 98 | 99 | 98-99 | 98 | 98 | 98-99 | 99 | 99 | 98-99 | 98 | 99 | 98-99 | 0.69 |
| Moderate | 1 | 1 | 1-2 | 2 | 1 | 1-2 | 1 | 1 | 1-2 | 1 | 1 | 1-2 | 0.91 |
| Vigorous | 0 | 0 | 0-0 | 0 | 0 | 0-0 | 0 | 0 | 0-0 | 0 | 0 | 0-0 | 0.22 |
| Swartz et al cutpoints | |||||||||||||
| Light | 76 | 76 | 73-79 | 75 | 75 | 71-79 | 76 | 76 | 74-80 | 74 | 74 | 70-78 | 0.004 |
| Moderate | 24 | 24 | 20-27 | 25 | 25 | 21-29 | 24 | 23 | 20-26 | 26 | 26 | 21-30 | 0.005 |
| Vigorous | 0 | 0 | 0-0 | 0 | 0 | 0-0 | 0 | 0 | 0-0 | 0 | 0 | 0-0 | 0.32 |
| Sedentary behavior | 49 | 49 | 44-53 | 47 | 46 | 42-51 | 49 | 49 | 46-54 | 46 | 45 | 42-50 | <0.001 |
| Steps per day - uncensored ^ | |||||||||||||
| Total | 26972 | 22992 | 20247-27295 | 24552 | 22849 | 19784-26590 | 29576 | 22416 | 19743-26307 | 26751 | 25739 | 20620-28204 | 0.40 |
| Light | 25297 | 21420 | 18508-26263 | 22777 | 21065 | 18236-24910 | 27138 | 20922 | 18388-24758 | 25213 | 23837 | 19283-26850 | 0.52 |
| Moderate | 1558 | 948 | 623-1701 | 1568 | 1243 | 742-1986 | 1807 | 992 | 640-1791 | 1259 | 1042 | 647-1604 | 0.13 |
| Vigorous | 1095 | 0 | 0-125 | 478 | 0 | 0-159 | 2094 | 0 | 0-126 | 609 | 0 | 0-309 | 0.07 |
| Steps per day - censored ^# | |||||||||||||
| Total | 15093 | 13094 | 11570-15441 | 14295 | 13709 | 11732-15817 | 16545 | 12785 | 11627-15018 | 15131 | 14621 | 12048-16851 | 0.43 |
| Light | 13209 | 11566 | 10116-13933 | 12520 | 11987 | 10026-14021 | 14107 | 11435 | 9998-13380 | 13593 | 12899 | 10432-14722 | 0.71 |
p-value is on the cohort from GEE models adjusted for age (3-mos postpartum), education, BMI (3-mos postpartum), and change in BMI from 3- to 12-mos postpartum
The cohort was defined as participants that completed the accelerometer portion of the study at both 3- and 12-months postpartum.
Intensity levels defined using Troiano et al cutpoints
Steps taken at <500 counts/minute were censored; this did not affect steps taken at moderate or vigorous levels.
The cutpoints on accelerometer counts per minute were defined as follows:
Swartz et al: 574-4944 (moderate); >=4945 (vigorous)
Troiano et al: 2020-5998 (moderate); >=5999 (vigorous)
Sedentary behavior: <=100 per Matthews et al.
IQR = interquartile range
We conducted a sensitivity analysis by including only women who completed at least 3 weekdays and 1 weekend day using our definition of a compliant day. This reduced the sample size to 153 (84.5%) and 185 (90.7%) at 3- and 12-months postpartum, respectively, and increased the average weekly wear time to 13.5 and 13.9 at 3- and 12-months postpartum. Online Table 2 displays the results with and without imputation on the compliant data. The mean counts dropped to 304 at 3-months and 335 at 12-months postpartum without imputation, but moderate and vigorous activity did not appreciably change with the Troiano or Freedson cutpoints. When we imputed data from 5am to midnight only among these women, the mean counts-and moderate activity were higher than without imputation, but values for vigorous physical activity remained similar.
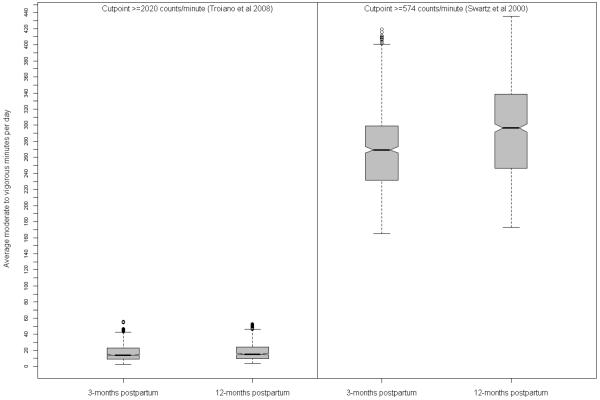
For the cohort of 80 women, average counts per minute significantly increased from 3- to 12-months postpartum (Table 3). When classifying counts into moderate to vigorous physical activity, the box and whisker plots displayed large differences between the Swartz cutpoints, compared to the Troiano cutpoints (Figure 3). Moderate activity increased and light activity decreased from 3- to 12-months postpartum when considering the Swartz cutpoints (Table 3), but did not significantly change when considering the more conservative cutpoints of Troiano and Freedson. Vigorous activity did not change with any of the three cutpoints. Sedentary behavior declined from 3- to 12-months postpartum. Considering relative values, the proportion of time spent in light activity (Swartz cutpoints) and sedentary behavior declined while time in moderate activity (Swartz cutpoints) increased from 3- to 12-months postpartum.
Figure 3.
Box and whisker plots of average moderate to vigorous physical activity per day from the accelerometer using Troiano et al and Swartz et al cutpoints at 3- and 12-months postpartum (n=80)
Self-reported Physical Activity
When we compared the accelerometer results in hours/week to the total self-reported moderate to vigorous physical activity, Spearman correlations ranged from 0.08 to 0.23 with the Troiano, Freedson, and Swartz cutpoints at 3-months postpartum and −0.09 to 0.27 at 12-months postpartum. When using moderate to vigorous MET-hours/week from the questionnaire to compare the accelerometer results in counts/wee, correlations were higher: 0.28 to 0.38 at 3-months postpartum and 0.13 to 0.31 at 12-months postpartum.
Self-reported perceived (hours/week) and absolute (MET-hours/week) physical activity overall and among the cohort of 3- and 12-month postpartum women is displayed in Table 4. For the cohort, work, recreational, outdoor household, child and adult care, and transportation activity did not significantly change from 3- to 12-months postpartum. Moderate to vigorous indoor household activities significantly increased from 3- to 12-months postpartum, using an absolute intensity of >=4.8 METS as the lowest threshold for moderate activities. For total activities, adding all that were self-reported as fairly light, somewhat hard, hard or very hard, or in total did not significantly change from 3- to 12-months postpartum for the cohort. However, total moderate to vigorous MET-hours/week significantly increased from 3- to 12-months postpartum, with 4.8 METS as the lowest threshold for moderate activities.
Table 4.
Self-reported physical activity among women at 3- and 12-months postpartum, overall and among the cohort
| 3-months Postpartum | 12-months Postpartum | 3-months Postpartum | 12-months Postpartum | p value^ | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||||||
| Overall (n=181) | Overall (n=204) | Cohort* (n=80) | Cohort* (n=80) | ||||||||||
|
|
|
||||||||||||
| Mean | Median | IQR | Mean | Median | IQR | Mean | Median | IQR | Mean | Median | IQR | ||
|
|
|
||||||||||||
| Work | |||||||||||||
| Moderate to vigorous hours/week | 0.3 | 0.0 | 0.0-0.0 | 0.3 | 0.0 | 0.0-0.0 | 0.4 | 0.0 | 0.0-0.0 | 0.2 | 0.0 | 0.0-0.0 | 0.24 |
| Moderate to vigorous MET-hours/week (>=3 METS) | 2.0 | 0.0 | 0.0-0.0 | 2.1 | 0.0 | 0.0-0.7 | 2.5 | 0.0 | 0.0-0.0 | 2.3 | 0.0 | 0.0-1.0 | 0.83 |
| Moderate to vigorous MET-hours/week (>=4.8 METS) | 0.6 | 0.0 | 0.0-0.0 | 0.8 | 0.0 | 0.0-0.0 | 0.4 | 0.0 | 0.0-0.0 | 1.3 | 0.0 | 0.0-0.0 | 0.09 |
| Recreational | |||||||||||||
| Moderate to vigorous hours/week | 1.4 | 0.0 | 0.0-1.5 | 1.1 | 0.0 | 0.0-2.0 | 1.5 | 0.0 | 0.0-1.6 | 1.0 | 0.0 | 0.0-1.5 | 0.13 |
| Moderate to vigorous MET-hours/week (>=3 METS) | 7.0 | 0.0 | 0.0-8.3 | 7.9 | 0.0 | 0.0-10.5 | 7.6 | 0.0 | 0.0-0.0 | 9.8 | 0.0 | 0.0-11.3 | 0.58 |
| Moderate to vigorous MET-hours/week (>=4.8 METS) | 3.4 | 0.0 | 0.0-0.0 | 5.9 | 0.0 | 0.0-5.6 | 2.8 | 0.0 | 0.0-0.0 | 7.6 | 0.0 | 0.0-7.1 | 0.07 |
| Outdoor Household | |||||||||||||
| Moderate to vigorous hours/week | 0.1 | 0.0 | 0.0-0.0 | 0.3 | 0.0 | 0.0-0.0 | 0.1 | 0.0 | 0.0-0.0 | 0.2 | 0.0 | 0.0-0.0 | 0.58 |
| Moderate to vigorous MET-hours/week (>=3 METS) | 0.5 | 0.0 | 0.0-0.0 | 2.6 | 0.0 | 0.0-0.0 | 1.2 | 0.0 | 0.0-0.0 | 1.9 | 0.0 | 0.0-0.0 | 0.44 |
| Moderate to vigorous MET-hours/week (>=4.8 METS) | 0.5 | 0.0 | 0.0-0.0 | 1.0 | 0.0 | 0.0-0.0 | 0.6 | 0.0 | 0.0-0.0 | 1.0 | 0.0 | 0.0-0.0 | 0.69 |
| Indoor Household | |||||||||||||
| Moderate to vigorous hours/week | 0.5 | 0.0 | 0.0-0.0 | 0.5 | 0.0 | 0.0-0.0 | 0.2 | 0.0 | 0.0-0.0 | 0.4 | 0.0 | 0.0-0.0 | 0.35 |
| Moderate to vigorous MET-hours/week (>=3 METS) | 0.7 | 0.0 | 0.0-0.0 | 4.0 | 0.0 | 0.0-3.2 | 2.4 | 0.0 | 0.0-2.3 | 3.6 | 0.0 | 0.0-3.8 | 0.24 |
| Moderate to vigorous MET-hours/week (>=4.8 METS) | 0.7 | 0.0 | 0.0-0.0 | 0.6 | 0.0 | 0.0-0.0 | 0.1 | 0.0 | 0.0-0.0 | 0.7 | 0.0 | 0.0-0.0 | 0.05 |
| Child and Adult Care | |||||||||||||
| Moderate to vigorous hours/week | 0.8 | 0.0 | 0.0-0.1 | 1.0 | 0.0 | 0.0-0.2 | 0.9 | 0.0 | 0.0-0.1 | 0.8 | 0.0 | 0.0-0.0 | 0.76 |
| Moderate to vigorous MET-hours/week (>=3 METS) | 5.4 | 0.0 | 0.0-6.0 | 9.6 | 1.2 | 0.0-9.0 | 5.5 | 0.0 | 0.0-7.7 | 8.7 | 0.0 | 0.0-5.8 | 0.21 |
| Moderate to vigorous MET-hours/week (>=4.8 METS) | 0.2 | 0.0 | 0.0-0.0 | 0.4 | 0.0 | 0.0-0.0 | 0.1 | 0.0 | 0.0-0.0 | 0.1 | 0.0 | 0.0-0.0 | 0.86 |
| Transportation ** | |||||||||||||
| Moderate to vigorous hours/week | 0.1 | 0.0 | 0.0-0.0 | 0.1 | 0.0 | 0.0-0.0 | 0.1 | 0.0 | 0.0-0.0 | 0.1 | 0.0 | 0.0-0.0 | 0.67 |
| Moderate to vigorous MET-hours/week (>=3 METS) | 0.7 | 0.0 | 0.0-0.0 | 1.1 | 0.0 | 0.0-0.0 | 0.6 | 0.0 | 0.0-0.0 | 0.5 | 0.0 | 0.0-0.0 | 0.68 |
| Overall | |||||||||||||
| Total hours/week in “fairly light” activities | 2.9 | 1.7 | 0.2-3.5 | 4.4 | 2.0 | 0.3-4.6 | 3.1 | 1.4 | 0.2-4.0 | 4.5 | 1.4 | 0.0-4.0 | 0.21 |
| Total hours/week in “somewhat hard” activities | 2.5 | 0.7 | 0.0-3.0 | 2.6 | 1.2 | 0.0-3.5 | 2.7 | 0.7 | 0.0-2.7 | 2.1 | 0.7 | 0.0-3.0 | 0.27 |
| Total hours/week in “hard or very hard” activities | 0.6 | 0.0 | 0.0-0.0 | 0.7 | 0.0 | 0.0-0.0 | 0.6 | 0.0 | 0.0-0.0 | 0.5 | 0.0 | 0.0-0.0 | 0.81 |
| Total moderate to vigorous hours/week | 3.1 | 1.3 | 0.0-4.0 | 3.3 | 1.6 | 0.0-4.3 | 3.3 | 1.3 | 0.0-3.9 | 2.6 | 1.0 | 0.0-3.9 | 0.54 |
| Total hours/week | 6.0 | 3.8 | 1.7-7.3 | 7.6 | 4.8 | 1.6-9.5 | 6.4 | 4.0 | 1.7-7.6 | 7.1 | 3.5 | 1.2-7.6 | 0.27 |
| Total moderate to vigorous MET-hours/week (>=3 METS) | 19.7 | 12.9 | 3.5-24.8 | 27.1 | 16.0 | 4.8-33.5 | 19.8 | 13.8 | 4.2-24.8 | 26.8 | 12.2 | 3.8-28.6 | 0.19 |
| Total moderate to vigorous MET-hours/week (>=4.8 METS) | 5.2 | 0.0 | 0.0-5.5 | 8.7 | 0.2 | 0.0-10.3 | 4.1 | 0.0 | 0.0-4.5 | 10.6 | 0.3 | 0.0-11.3 | 0.02 |
| Total MET-hours/week | 22.8 | 16.1 | 5.6-27.2 | 30.0 | 18.6 | 6.4-38.3 | 23.4 | 16.7 | 5.8-26.8 | 28.6 | 13.8 | 3.9-29.5 | 0.32 |
The cohort was defined as participants that completed the accelerometer portion of the study at both 3- and 12-months postpartum.
There were no transportation activities that were >=4.8 METS so it is not reported.
p-value is on the cohort sample from GEE models adjusted for age at 3-months postpartum, education, BMI at 3-months postpartum, and change in BMI from 3- to 12-months postpartum Moderate to vigorous hours/week included activities that were self-reported as “somewhat hard” and “hard or very hard”.
Total hours per week included activities that were self-reported as “fairly light”, “somewhat hard”, and “hard or very hard”.
Moderate to vigorous MET-hours per week was classified using >=3 METS and >=4.8 METS.
IQR=interquartile range; MET=metabolic equivalent
Discussion
The primary purpose of this paper was to describe physical activity among a cohort of postpartum women and secondarily to detail the imputation methods used for the accelerometer data for others to use.
Physical Activity Among Postpartum Women
We found for the cohort of 80 women, average counts per minute significantly increased from 3- to 12-months postpartum. Moderate activity increased and light activity decreased from 3- to 12-months postpartum when considering the Swartz cutpoints, but did not significantly change when considering the more conservative cutpoints of Troiano and Freedson. Sedentary behavior declined from 3- to 12-months postpartum. Interestingly, the changes in moderate activity were not detected using the self-reported questionnaire, except for indoor household activities using absolute intensity (>=4.8 METS), which was designed to capture moderate and vigorous physical activity. This may be due to higher measurement error and recall bias associated with self-report. The low correlations we found between the questionnaire and the accelerometer were similar to our findings from a validation study among a different group pregnant women.31
When comparing to the 2003-04 NHANES national sample, moderate to vigorous physical activity (using the Troiano et al cutpoints 27) among women 20 to 29 years was 24 minutes/day and for 30 to 39 years was 21 minutes/day. This is higher than the values obtained by the cohort of women in our study; the women achieved 17 minutes/day at 3-months postpartum and 18 minutes/day at 12-months postpartum using these same cutpoints. Using the 2003-04 NHANES data, Matthews et al 30 reported that sedentary behavior was 7.7 hours/day among women 20 to 29 years and 7.3 hours/day among women 30 to 39 years. The values we obtained for the cohort were higher (9.3 hours/day at 3-months postpartum and 8.8 hours/day at 12-months postpartum), in part due to the imputation we performed since we had complete data over a 19 hour day. Tudor-Locke et al 25 reported on the 2005-06 NHANES national sample, indicating that women 20 years and older averaged 5756 censored steps/day and 8882 uncensored steps/day, which is quite a bit higher than our sample.
In the 2003-04 NHANES data, 60% of women 20 to 39 years achieved at least 4 of 7 valid days of wearing time, defined as at least 10 hours/day.27 We defined wearing time specific to the women we measured and differently for weekends and weekdays since the wearing times differed. Recalculating to be comparable to the 10 hours/day for at least 4 days standard similar to NHANES, in our sample 80% of women (145/181) achieved this at 3-months postpartum and 86% of women (176/204) achieved this at 12-months postpartum.
Imputation of Missing Accelerometer Counts
A challenge with using accelerometry data is that at times data are missing, with the assumption that women were not wearing the monitor due to reasons such as participation in water activities, sleep, or noncompliance. Using our data, on average 70% of women wore the monitor 7.5 hours on weekdays and 6.2 hours on weekends at 3-months postpartum and 8.4 hours on weekdays and 7.2 hours on weekends at 12-months postpartum (Figure 1). If we had summarized the recorded data only, there is a chance that these results could be biased, especially since the total accelerometer count per day would likely be underestimated if any activity occurred while the accelerometer was not being worn.
One strategy often used is to include in the analysis only days that accumulate a minimum amount of wearing time. This appropriate amount of wearing time varies across studies, and these periods of time are likely associated with sedentary and light behavior.40 However, they may also be associated with moderate to vigorous activity if participants engage in water activities.
The strengths of the imputation procedures include principled handling of missing data, acknowledgment of uncertainty in imputation by imputing multiple datasets, the ability to take into account day- and time-specific factors, and the subsequent ability through imputation to standardize all accelerometer count days to a single 19 hour time period. However, there are some limitations. First, by defining the wearing time from 5am to midnight for the imputation, which covered the time most women wore the monitor, it may have ignored information from women who were shift workers. Second, as in other studies, it is not clear when the monitor is not being worn if it is due to noncompliance, sleeping, or water activity. Accompanying accurate daily diary data on time-specific activities would enable the imputation model to account for such activities during non-wearing time.
Study Limitations
Several limitations of this work should be acknowledged. The generalizability of this study may be limited, as the women were volunteers from central North Carolina. Due to attrition, a subsequent pregnancy between 3- and 12-months postpartum, and other factors, the women were not necessarily representative of the original pregnancy cohort. Confirmation of these findings in population-based cohorts of postpartum women is needed. While we had physical activity measures at two time points during postpartum, it might be useful to assess physical activity more frequently over the time period to detect more precise patterns.
Conclusions
Most women in our sample did not meet recommendations for physical activity. Traditional postpartum medical care in the U.S. ends around 6 weeks after delivery, and at that time women may or may not receive advice at that time on physical activity.41 Thus, postpartum women may not be aware of the benefits and importance of physical activity during the postpartum time period. Interventions are needed to help postpartum women integrate more moderate to vigorous physical activity and to capitalize on the improvements in sedentary behavior that occurred from 3- to 12-months postpartum in this study.
Supplementary Material
Acknowledgment and Funding Sources
Funding for this study was provided by the National Institutes of Health (NIH) / National Cancer Institute (#CA109804). Data collection was supported by NIH / National Institute of Child Health and Human Development (#HD37584), NIH General Clinical Research Center #RR00046), and NIH / National Institute of Diabetes and Digestive and Kidney Diseases (#DK 061981). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The PIN Study is a joint effort of many investigators and staff members whose work is gratefully acknowledged. We also thank the anonymous reviewers for their helpful comments.
References Cited
- 1.Larson-Meyer DE. Effect of postpartum exercise on mothers and their offspring: a review of the literature. Obes Res. 2002 Aug;10(8):841–853. doi: 10.1038/oby.2002.114. [DOI] [PubMed] [Google Scholar]
- 2.Siega-Riz AM, Viswanathan M, Moos MK, et al. A systematic review of outcomes of maternal weight gain according to the Institute of Medicine recommendations: birthweight, fetal growth, and postpartum weight retention. Am J Obstet Gynecol. 2009 Oct;201(4):339, e331–314. doi: 10.1016/j.ajog.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 3.Pivarnik JM, Chambliss H, Clapp J, III, et al. Impact of physical activity during pregnancy and postpartum on chronic disease risk. Med Sci Sports Exerc. 2006 May;38(5):989–1006. doi: 10.1249/01.mss.0000218147.51025.8a. [DOI] [PubMed] [Google Scholar]
- 4.Sampselle C, Seng J, Yeo S, Killion C, Oakley D. Physical activity and postpartum well-being. J Obstet Gynecol Neonatal Nurs. 1999;28:41–49. doi: 10.1111/j.1552-6909.1999.tb01963.x. [DOI] [PubMed] [Google Scholar]
- 5.U.S. Department of Health and Human Services . 2008 Physical Activity Guidelines for Americans. Washington, D.C.: 2008. [Google Scholar]
- 6.Davies G, Wolfe L, Mottola M, MacKinnon C. Joint SOGC/CSEP clinical practice guideline: Exercise in pregnancy and the postpartum period. Can J Appl Physiol. 2003;28(3):330–341. [PubMed] [Google Scholar]
- 7.Royal College of Obstetricians and Gynaecologists Exercise in pregnancy. RCOG Statement No. 4 - January 2006. [Accessed September 1, 2009]. at http://www.rcog.org.uk/files/rcog-corp/uploaded-files/RCOGStatement4ExercisePregnancy2006.pdf.
- 8.ACOG Exercise during pregnancy and the postpartum period. Obstet Gynecol. 2002;99(1):171–173. doi: 10.1016/s0029-7844(01)01749-5. ACOG Committee Opinion No. 267. [DOI] [PubMed] [Google Scholar]
- 9.Wilkinson S, Huang CM, Walker LO, Sterling BS, Kim M. Physical activity in low-income postpartum women. J Nurs Scholarsh. 2004;36(2):109–114. doi: 10.1111/j.1547-5069.2004.04022.x. [DOI] [PubMed] [Google Scholar]
- 10.Catellier DJ, Hannan PJ, Murray DM, et al. Imputation of missing data when measuring physical activity by accelerometry. Med Sci Sports Exerc. 2005 Nov;37(11 Suppl):S555–562. doi: 10.1249/01.mss.0000185651.59486.4e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Borodulin K, Evenson K, Wen F, Herring A, Benson A. Physical activity patterns during pregnancy. Med Sci Sports Exerc. 2008;40(11):1901–1908. doi: 10.1249/MSS.0b013e31817f1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Borodulin K, Evenson KR, Herring AH. Physical activity patterns during pregnancy through postpartum. BMC Womens Health. 2009;9:32. doi: 10.1186/1472-6874-9-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Siega-Riz AM, Herring AH, Carrier K, Evenson KR, Dole N, Deierlein A. Sociodemographic, perinatal, behavioral, and psychosocial predictors of weight retention at 3 and 12 months postpartum. Obesity. 2009 Dec 24; doi: 10.1038/oby.2009.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Trost S, McIver K, Pate R. Conducting accelerometer-based activity assessments in field-based research. Med Sci Sports Exerc. 2005;37(11 Suppl):S531–S543. doi: 10.1249/01.mss.0000185657.86065.98. [DOI] [PubMed] [Google Scholar]
- 15.Freedson P, Melanson E, Sirard J, Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc. 1998;30:777–781. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- 16.Hendelman D, Miller K, Baggett C, Debold E, Freedson P. Validity of accelerometry for the assessment of moderate intensity physical activity in the field. Med Sci Sports Exerc. 2000;32:S442–449. doi: 10.1097/00005768-200009001-00002. [DOI] [PubMed] [Google Scholar]
- 17.Brage S, Wedderkopp N, Franks P, Andersen L, Froberg K. Reexamination of validity and reliability of the CSA monitor in walking and running. Med Sci Sports Exerc. 2003;35:1447–1454. doi: 10.1249/01.MSS.0000079078.62035.EC. [DOI] [PubMed] [Google Scholar]
- 18.Metcalf B, Curnow J, Evans C, Voss L, Wilkin T. Technical reliability of the CSA activity monitor: The EarlyBird Study. Med Sci Sports Exerc. 2002;34(9):1533–1537. doi: 10.1097/00005768-200209000-00022. [DOI] [PubMed] [Google Scholar]
- 19.Brage S, Brage N, Wedderkopp N, Froberg K. Reliability and validity of the Computer Science and Applications accelerometer in a mechanical setting. Meas Phys Educ Exerc Sci. 2003;7:101–119. [Google Scholar]
- 20.Welk G, Schaben J, Morrow J., Jr. Reliability of accelerometry-based activity monitors: A generalizability study. Med Sci Sports Exerc. 2004;36:1637–1645. [PubMed] [Google Scholar]
- 21.Esliger D, Tremblay M. Technical reliability assessment of three accelerometer models in a mechanical setup. Med Sci Sports Exerc. 2006;38(12):2173–2181. doi: 10.1249/01.mss.0000239394.55461.08. [DOI] [PubMed] [Google Scholar]
- 22.McClain J, Sisson S, Tudor-Locke C. Actigraph accelerometer interinstrument reliability during free-living in adults. Med Sci Sports Exerc. 2007;39(9):1509–1514. doi: 10.1249/mss.0b013e3180dc9954. [DOI] [PubMed] [Google Scholar]
- 23.Evenson K, Terry J., Jr Assessment of differing definitions of accelerometer nonwear time. Res Q Exerc Sport. 2009;80(2):355–362. doi: 10.1080/02701367.2009.10599570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Le Masurier G, Tudor-Locke C. Comparison of pedometer and accelerometer accuracy under controlled conditions. Med Sci Sports Exerc. 2003;35:867–871. doi: 10.1249/01.MSS.0000064996.63632.10. [DOI] [PubMed] [Google Scholar]
- 25.Tudor-Locke C, Johnson WD, Katzmarzyk PT. Accelerometer-determined steps per day in US adults. Med Sci Sports Exerc. 2009 Jul;41(7):1384–1391. doi: 10.1249/MSS.0b013e318199885c. [DOI] [PubMed] [Google Scholar]
- 26.Swartz A, Strath S, Bassett D, Jr., O’Brien W, King G, Ainsworth B. Estimation of energy expenditure using CSA accelerometers at hip and wrist sites. Med Sci Sports Exerc. 2000;32:S450–456. doi: 10.1097/00005768-200009001-00003. [DOI] [PubMed] [Google Scholar]
- 27.Troiano R, Berrigan D, Dodd K, Masse L, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 28.Yngve A, Nilsson A, Sjostrom M, Ekelund U. Effect of monitor placement and of activity setting on the MTI accelerometer output. Med Sci Sports Exerc. 2003;35:320–326. doi: 10.1249/01.MSS.0000048829.75758.A0. [DOI] [PubMed] [Google Scholar]
- 29.Leenders N, Nelson T, Sherman W. Ability of different physical activity monitors to detect movement during treadmill walking. Intl J Sport Med. 2003;24:43–50. doi: 10.1055/s-2003-37196. [DOI] [PubMed] [Google Scholar]
- 30.Matthews C, Chen K, Freedson P, et al. Amount of time spent in sedentary behaviors in the United States, 2003-2004. Am J Epidemiol. 2008;167(7):875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Evenson KW. Measuring physical activity in pregnant women using a structured one-week recall questionnaire: evidence for validity and reliability. Intl J Nutr Physical Activity. 2010;7:21. doi: 10.1186/1479-5868-7-21. F. Available at http://www.ijbnpa.org/content/27/21/21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Borg G, Linderholm H. Perceived exertion and pulse rate during graded exercise in various age groups. Acta Med Scand. 1974;472:194–206. [Google Scholar]
- 33.Ainsworth B, Haskell W, Leon A, et al. Compendium of physical activities: Classification of energy costs of human physical activities. Med Sci Sports Exerc. 1993;25:71–80. doi: 10.1249/00005768-199301000-00011. [DOI] [PubMed] [Google Scholar]
- 34.Ainsworth B, Haskell W, Whitt M, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sport Exer. 2000;32(9 supplement):S498–S516. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 35.Pollock M, Gaesser G, Butcher J, et al. American College of Sports Medicine Position Stand: The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Medicine and Science in Sports and Exercise. 1998;30(6):975–991. doi: 10.1097/00005768-199806000-00032. [DOI] [PubMed] [Google Scholar]
- 36.National Institutes of Health. National Heart Lung and Blood Institute Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: The evidence report. Obes Res. 1998;6(supplement 2):S51–S209. [PubMed] [Google Scholar]
- 37.R Development Core Team . R: A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2010. [Google Scholar]
- 38.Liang K-Y, Zeger S. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73(1):13–22. [Google Scholar]
- 39.Zeger S, Liang K. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–130. [PubMed] [Google Scholar]
- 40.Masse L, Fuemmeler B, Anderson C, et al. Accelerometer data reduction: A comparison of four reduction algorithms on select outcome variables. Med Sci Sports Exerc. 2005;37(11 supplement):S544–S554. doi: 10.1249/01.mss.0000185674.09066.8a. [DOI] [PubMed] [Google Scholar]
- 41.Ferrari R, Siega-Riz A, Evenson K, Moos M, Melvin C, Herring A. Provider advice about weight loss and physical activity in the postpartum period. J Women Health. 2010;19(3):397–406. doi: 10.1089/jwh.2008.1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.