Abstract
The long-term outcomes of unselected patients with angina pectoris and a bundle branch block (BBB) on the initial electrocardiogram are not well established. The Olmsted County Chest Pain Study is a community-based cohort of 2271 consecutive patients presenting to three Olmsted County emergency departments with angina from 1985 to 1992. Patients were followed for major adverse cardiovascular events (MACE) including death, myocardial infarction, stroke and revascularization at 30 days and over a median follow-up period of 7.3 years and for mortality only through a median of 16.6 years. Cox models were used to estimate the associations between bundle branch block and cardiovascular outcomes. The mean age of the cohort on presentation was 63 years, with 58% men. MACE at 30 days occurred in 11% with RBBB, 8.8 % with LBBB and 6.4 % in patients without BBB (p=0.17). Over a median follow-up of 7.3 years, patients with BBB were at higher risk for MACE (RBBB HR 1.85, 95% CI 1.44–2.38; p<0.001 and LBBB HR 2.04, 95% CI 1.62–2.56; p<0.001) compared to those without BBB. Over a median of 16.6 years, both BBB groups had lower survival rates than patients without BBB (RBBB HR 2.19, 95% CI 1.73–2.78; p<0.001 and LBBB HR 3.32, 95% CI 2.67–4.13; p ≤ 0.001), but after adjustment for multiple risk factors, an increased risk of mortality for LBBB remained significant. In conclusion, the appearance of LBBB or RBBB in patients presenting with angina predicts adverse long-term cardiovascular outcomes compared to patients without BBB.
Keywords: Bundle-branch Block, Angina, Long term outcomes
In the setting of an acute coronary syndrome (ACS), the prognosis is worse in patients in whom the bundle branch block (BBB) is new and or persistent1–6. However, owing to the uncertainty in reliably differentiating new and old BBB, patients with BBB, especially RBBB, presenting with ACS are managed no differently than those without BBB, though more favorable outcomes have been reported with aggressive management 7,8. The long-term clinical implications of BBB in a community-based cohort with angina are unknown. This analysis from the Olmsted County Chest Pain study was conducted to elucidate the short- and long-term prognostic significance of either BBB in patients presenting to the emergency department (ED) with angina.
METHODS
The complete medical records of eligible patients were obtained through the resources of the Rochester Epidemiology Project (REP) which allows comprehensive capture of details of the health care experiences, including outpatient care, of all residents of Olmsted County, MN (OC)9. The OC Health Care Utilization and Expenditures Database, linked to the REP, contains detailed line-item information on health services utilization and expenditures incurred by every member of the population for as long as they reside in the county. Unlike other geographically defined U.S. communities, a complete health services utilization history is available for all OC residents, including the affiliation of their health care provider, site of care (inpatient, outpatient or nursing home) and participating health insurance plan.
Using written screening logs, we retrospectively identified all residents of Olmsted County, MN presenting to one of the County’s three EDs with angina between January 1, 1985 and December 31, 1992. Complete medical records of the screened population were reviewed by an experienced nurse abstractor, who identified all county residents presenting with a first episode of angina defined according to the Diamond classification on the basis of a new or worsening pattern of ischemic anterior or left lateral chest pain occurring at rest or with minimal exertion and alleviated by sublingual nitroglycerin and/or rest 10. Patients were excluded if they had ST-segment elevation ≥1 mm in two or more contiguous leads suggestive of acute MI on the initial ECG, or an alternate etiology of chest pain, including musculoskeletal pain, pneumonia, pleurisy, pericarditis, gastritis, pulmonary thromboembolism or dissecting aortic aneurysm. Patients who died in the ED (n=11) were also excluded. From the record review, the history of the qualifying episode was abstracted, including the past medical history and findings on physical examination.
The initial ECG was interpreted by a staff cardiologist from the Mayo Clinic and verified by one of the study physicians. RBBB and LBBB were defined using the Minnesota code. A diagnosis of RBBB required all of the following: QRS duration >120 ms in the presence of normal sinus or other supraventricular rhythm; R-wave or RSR’ complex in lead V1; and an R-complex with a prolonged, shallow S-wave in leads V5, V6, aVL or I. Left bundle branch block was coded if all of the following criteria were met: QRS-complex duration >120 ms in the presence of normal sinus or other supraventricular rhythm; QS- or RS-complex in lead V1; broad or notched R-waves in leadsV5 and V6, or an RS pattern; and the absence of Q wave in leads V5, V6 or I.
Long-term outcome data were collected in two phases. In the first phase, data were collected on major adverse cardiovascular events (MACE) consisting of death, MI, stroke and need for urgent revascularization, and on incident heart failure and pacemaker implantation. Study subjects for whom there was no subsequently documented medical care visits in OC were contacted to determine vital status. A letter to the patient’s last recorded address initiated this contact. If there was no response, verification of status was confirmed through telephone contact either with the patient directly or with a family member, physician, medical institution or nursing home. Ninety-three percent of patients were followed through 1995 or later.
In the second phase, the last known alive date or death date as of January 2007 were added. The last known alive date was obtained from patient records of the Mayo Clinic. Dates of death were obtained through State of Minnesota Electronic Death Certificates, State of Minnesota Death Tapes, Olmsted County Electronic Death Certificates and Mayo Clinic records. Thirty-seven patients were excluded in this phase because they refused to allow access to their records for research (as required by Minnesota state).
Patients were sub-classified on the basis of RBBB, LBBB or no BBB (NBBB) and comparisons were made across these groups for MACE and mortality. Thirty-day event rates were compared with Pearson’s chi-square test. Long-term survival rates were estimated by Kaplan-Meier methods and compared using the log-rank statistic. Logistic regression models were used to estimate unadjusted odds ratios for primary MACE within the first 30 days of arrival to the ED. Cox proportional hazards regression models were used to estimate hazard ratios for long-term survival and survival free of MACE. The following covariates were selected for the model on the basis of clinical significance: age, gender, history of smoking, diabetes, hypertension, systolic blood pressure, total serum cholesterol, family history of coronary disease, chronic aspirin use prior to ED presentation, prior MI or history of CAD, prior revascularization, ST-segment depression ≥1 mm on the initial ECG, extracardiac arterial disease, chronic obstructive pulmonary disease (COPD) and pulmonary edema.
RESULTS
During the study period, 6,801 residents of OC presented to an ED with a first episode of acute chest pain. Of these, 2,271 (33.4%) met the criteria for angina and were followed as study subjects for a median of 7.3 years for MACE. Of the ineligible patients, cardiac disease accounted for 6.7% of presenting syndromes, including STEMI in 5.5%, stable angina pectoris in 1.0% and aortic dissection in 0.2%. Non-cardiac causes of chest pain accounted for 36.2% of ineligible patients, in 23.9% the cause of symptoms was not determined, 17.6% were non-residents, and 15.6% refused to participate. After extending follow-up for collection of data on vital status, 2234 study subjects were followed for a median of 16.6 years.
The mean age of the cohort on presentation was 63± 40 (SD) years, 57.5% were men and 14.8% had diabetes (Table 1). Based on the Minnesota criteria, 91 subjects (4%) had RBBB, 102 (4.5%) had LBBB and 2078 had NBBB on the initial ECG. Subjects with RBBB were older, more likely to have a history of CAD (including prior MI or angina) and a diagnosis of hypertension compared to patients with NBBB. Patients with either BBB were typically older with a history of MI, COPD or hypertension but less likely to have smoked tobacco. Women in this cohort were more likely to have LBBB at presentation than men. Patients with either BBB were more often admitted to hospital upon presentation with chest pain.
TABLE 1.
Baseline characteristics
| Characteristics | Total n=2271 | Bundle Branch Block | p-value | ||
|---|---|---|---|---|---|
| Right (n=91) | Left (n=102) | Neither (n=2078) | |||
| Mean age (Range) | 63 (21–101) | 72 (31–92) | 72 (44–96) | 62 (21–101) | <0.001 |
| Men | 1306 (57.5%) | 66 (72.5%) | 43 (42.2%) | 1197 (57.6%) | <0.001 |
| Diabetes mellitus | 336 (14.8%) | 14 (15.4%) | 18 (17.6%) | 304 (14.6%) | 0.69 |
| Smoked at presentation | 490 (21.6%) | 11 (12.1%) | 15 (14.7%) | 464 (22.3%) | 0.015 |
| Chronic Obstructive Lung disease | 319 (14.1%) | 20 (28%) | 29 (22%) | 270 (13%) | <0.001 |
| Hypertension (>140/90 mmHg) | 1039 (45.8%) | 56 (61.5%) | 56 (54.9%) | 927 (44.6%) | 0.001 |
| Hypercholesterolemia | 794 (35.0%) | 35 (38.5%) | 38 (37.3%) | 721 (34.7%) | 0.67 |
| Prior aspirin use | 395 (17.4%) | 19 (20.9%) | 22 (21.6%) | 354 (17.0%) | 0.33 |
| Any EKG abnormality | 1257 (55.4%) | 91 (100.0%) | 102 100.0%) | 1064 (51.2%) | <0.001 |
| Mean (range) systolic BP @ index date (mmHg) | 153 (60–300) | 155 (65–240) | 149 (60–225) | 153 (68–300) | 0.40 |
| Mean (range) diastolic BP @ index date (mmHg) | 87 (34–170) | 85 (50–130) | 85 (40–145) | 88 (34–170) | 0.054 |
During the first 30 days after presentation, 153 (6.7%) patients suffered at least one primary MACE (Table 2), 11% in those with RBBB, 8.8% in the LBBB group, and 6.4 % in those without BBB (p=0.17). Patients with either BBB had no greater elevation of cardiac enzyme levels at presentation than patients without BBB (RBBB 19.8%, LBBB 20.6%, NBBB 18.0%, p=0.74). Patients with LBBB were more likely to develop clinical heart failure, however, during the first 30 days than those with either RBBB or NBBB (p=0.002) (Table 2).
Table 2.
30-day Rates of Non-fatal Cardiovascular Events*
| Variable | Aggregate n=2271 | Bundle Branch Block | p-value | ||
|---|---|---|---|---|---|
| Right (n=91) | Left (n=102) | Neither (n=2078) | |||
| Death | 57 (2.5%) | 4 (4.4%) | 5 (4.9%) | 48 (2.3%) | 0.13 |
| Cardiovascular Death | 50 (2.2%) | 4 (4.4%) | 4 (3.9%) | 42 (2.0%) | 0.15 |
| Myocardial Infarction | 47 (2.1%) | 3 (3.3%) | 5 (4.9%) | 39 (1.9%) | 0.078 |
| Stroke | 14 (0.6%) | 2 (2.2%) | 0 (0.0%) | 12 (0.6%) | 0.11 |
| Revascularization | 59 (2.6%) | 2 (2.2%) | 1 (1.0%) | 56 (2.7%) | 0.55 |
| Heart failure | 93 (4.1%) | 5 (5.5%) | 11 (10.8%) | 77 (3.7%) | 0.002 |
Excludes deaths in the emergency department during the initial evaluation
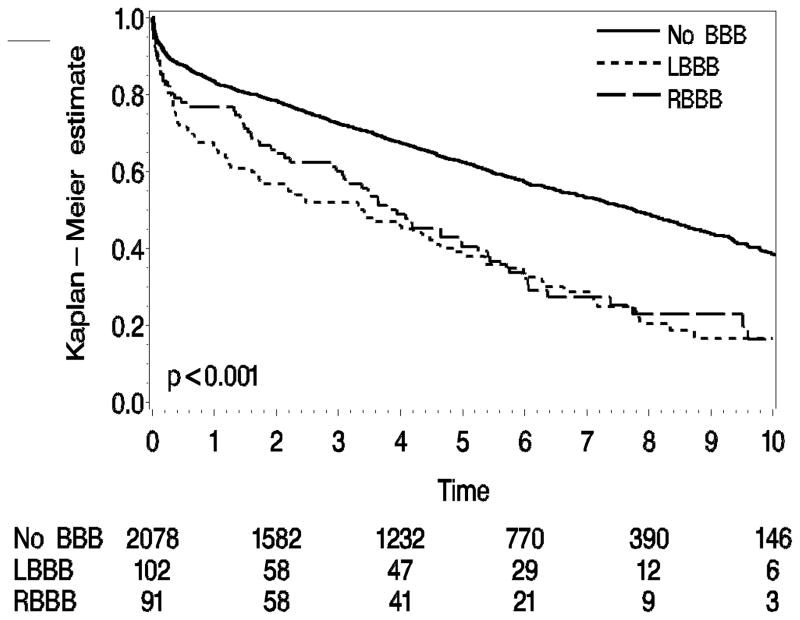
During the first phase of long-term follow-up (median 7.3 years), MACE were recognized in 1136 patients, of whom 709 died. Unadjusted Kaplan-Meier survival curves showed that patients with RBBB or LBBB on the presenting ECG were more likely to develop MACE (Figure 1) than those without BBB. The prognosis with RBBB was no better than with LBBB with respect to MACE during this period (Table 3), but after multivariate adjustment for clinical risk factors, only LBBB was significantly associated (p=0.004) with MACE during follow-up (Table 4). Patients with RBBB were more likely than those with LBBB or NBBB to undergo pacemaker implantation over the 7-year follow-up period (p<0.001) (Table 3). Patients with BBB were more likely to have developed HF over the 7 years (p<0.001) (Table 3).
Figure 1.
Bundle branch block and major adverse cardiovascular events during a median follow-up of 7.3 years.
Table 3.
Long-Term (7-year) Rates of Major Adverse Cardiovascular Events*
| Variable | Aggregate (n=2271) | BUNDLE BRANCH BLOCK | p-value | ||
|---|---|---|---|---|---|
| Right (n=91) | Left (n=102) | Neither (n=2078) | |||
| Total death | 588 (29.8%) | 39 (46.0%) | 64 (65.8%) | 485 (27.2%) | <0.001 |
| Cardiovascular Death | 298 (15.9%) | 23 (30.2%) | 44 (50.1%) | 231 (13.6%) | <0.001 |
| Myocardial Infarction | 294 (15.9%) | 21 (35.3%) | 24 (31.9%) | 249 (14.5%) | <0.001 |
| Stroke | 162 (9.9%) | 7 (13.6%) | 7 (9.9%) | 148 (9.7%) | 0.413 |
| Revascularization | 394 (21.4%) | 17 (25.9%) | 14 (19.3%) | 363 (21.3%) | 0.837 |
| Pacemaker Implantation | 74 (4.2%) | 12 (19.2%) | 5 (5.7%) | 57 (3.5%) | <0.001 |
| Heart failure | 441 (23.0%) | 30 (41.0%) | 48 (59.4%) | 363 (20.6%) | <0.001 |
| Any Event (excluding heart failure and Pacemaker Implantation) | 1006 (49.2%) | 62 (72.6%) | 71 (71.2%) | 873 (46.9%) | <0.001 |
Excludes deaths in the emergency department during the initial evaluation
Table 4.
Hazard Ratios for Major Adverse Cardiovascular Events
| Bundle Branch Block | Unadjusted | Adjusted* | ||
|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | |
| Left | 2.04 (1.62–2.56) | <0.001 | 1.41 (1.11–1.77) | 0.004 |
| Right | 1.85 (1.44–2.38) | <0.001 | 1.07 (0.83–1.38) | 0.613 |
Risks adjusted for age, sex, history of smoking, diabetes, hypertension, systolic blood pressure, total serum cholesterol, family history of CAD, chronic aspirin use prior to ED presentation, prior revascularization, prior MI or history of CAD, ≥1 mm ST-segment depression, extracardiac arterial disease, COPD and pulmonary edema related to ischemia
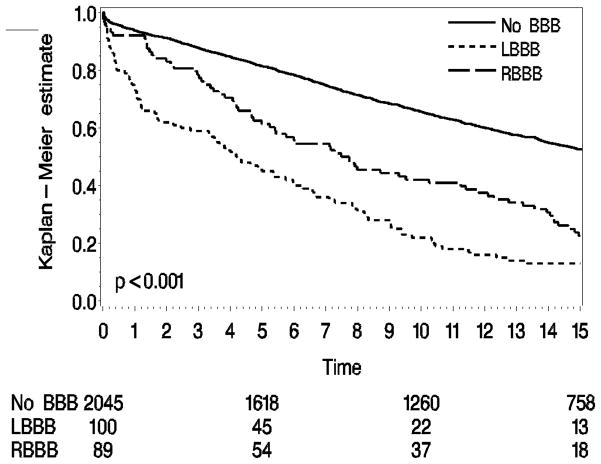
In the second phase of long-term follow-up (median 16.6 years) there were 1208 reported deaths in the cohort. Unadjusted Kaplan-Meier survival curves show lower survival rate for patients with RBBB (23% at 15 years) compared to those without BBB (53%) patients (HR 2.19, 95% CI 1.73–2.78; p<0.001), and a higher hazard ratio for those with LBBB compared (HR 3.32, 95% CI 2.67–4.13; p<0.001) (Figure 2). Deaths in patients with initial BBB were more often due to cardiovascular diseases, including MI and stroke (Table 3). After adjustment for risk factors for mortality, the risk associated with RBBB was no longer statistically significant (HR 1.10, 95% CI 0.86–1.40; p = 0.45) compared to those with NBBB, while the risk associated with LBBB remained (HR 2.02, 95% CI 1.61–2.52; p<0.001).
Figure 2.
Overall mortality according to category of bundle branch block on the initial ECG over a median follow-up of 16.6 years in patients presenting with angina.
DISCUSSION
Our study is the longest and most comprehensive observation of a population-based cohort of consecutive patients with angina who displayed right or left BBB on the initial ECG. During follow-up, which extended into the current era, the pattern of RBBB on the presenting ECG predicted poor cardiovascular outcomes over 7 years and greater mortality rate of 15 years compared to those without BBB, but these differences were largely attributable to a higher burden of associated risk factors. Patients with RBBB were also more likely to experience HF and to undergo pacemaker implantation during long-term follow-up. For those presenting with LBBB, the relationships to MACE at 7 years and mortality at 16 years were incompletely explained by identifiable concurrent risk factors, though the incidence of HF and need for pacemaker implantation in patients with this conduction pattern was no different than for patients without bundle branch block. Patients with either right or left BBB in this cohort were older than those without BBB and had a higher burden of cardiovascular risk factors, as described in other studies1–5,8,11.
Like other patients with cardiovascular disease, those with BBB span a spectrum of risk that includes low-risk asymptomatic individuals, in whom the ECG abnormalities are detected incidentally 2,12–21, and the long-term cardiovascular outcomes associated with BBB in these are generally benign. On the other hand, the implications of LBBB or RBBB on the initial ECG in patients presenting with an acute coronary syndrome is related to the amount of jeopardized myocardium (Table 5). Impaired ventricular function is associated with adverse outcomes in subjects with BBB and it has been postulated that RBBB might be related to right ventricular dysfunction or ventricular asynchrony 12. A greater extent of myocardial ischemia or impairment of cardiac function may have contributed to the excessive risk of heart failure among patients with RBBB in the population we studied, though we observed no significant differences in the magnitude of initial cardiac enzyme elevations (CK) following the episode of chest pain that qualified them for inclusion. Patients with ACS tracked in the Second National Registry of Myocardial Infarction (NRMI-2), who displayed BBB on the initial ECG received less evidence-based care than those without BBB, perhaps because of delayed or missed diagnosis 3. The MONICA/KORA AMI registry demonstrated dramatic declines in rates of in-hospital complications and 28-day fatality when patients with non-ST-elevation ACS and BBB received more aggressive clinical management 7.
Table 5.
Previous Studies of Right Bundle Branch Block and Outcomes in Various Populations
| Author | Publication Year | Sample Size | Nature of population | Increase in Mortality |
|---|---|---|---|---|
| Rotman | 1975 | 237,000 | U.S Air Force | No |
| Schneider | 1981 | 5,209 | Framingham | Yes |
| Fleg | 1983 | 1,142 | Healthy men | No |
| Eriksson | 1988 | 855 | Birth cohort | Yes |
| Fahy | 1995 | 110,000 | Screening | Yes |
| Menotti | 2001 | 11,860 | Healthy | Yes |
| Miller | 2005 | 723 | Asymptomatic | Yes |
| Barsheshet | 2008 | 4,102 | Heart failure | Yes |
| Hesse | 2001 | 7,073 | Referred for Nuclear stress test | Yes |
| Freedman | 1987 | 15,609 | Chronic coronary disease | Yes |
| Ricou | 1991 | 1,634 | Post Myocardial Infarction | Yes |
| Current study | 2011 | 2,271 | Angina Pectoris | Yes |
The high long-term MACE and death rates in patients with LBBB group is concordant with previous studies, while the attenuation of rates of adverse events in patients presenting with RBBB after adjustment for other prognostic variables suggests that RBBB may be an immediately available marker of associated risk factors that carry important clinical implications for years into the future. Detection of RBBB should therefore not be dismissed as benign but instead trigger more aggressive short and long-term strategies to reduce the risk, with particular attention to factors associated with the development of clinical HF. While the incremental risk of cardiovascular mortality in patients with LBBB has been attributed to myocardial dysfunction 22 HF and arrhythmic death 23, the mechanisms behind the adverse prognosis associated with RBBB in patients presenting with ACS have not been elucidated 3,5,12. Our data suggest, however, that adverse outcomes in patients presenting with RBBB in the setting of angina are distinct from those responsible for the elevated risk of MACE and mortality in patients with initial LBBB, even when other risk factors are considered.
Prolongation of the QRS interval on the ECG, a sine qua non of BBB, has been implicated in ventricular dysynchrony, systolic and diastolic dysfunction, impaired exercise tolerance, arrhythmias and sudden death 24–26. The higher rate of pacemaker implantation we observed in patients with initial RBBB implies a propensity to degeneration of cardiac conduction over time, and failure to detect this increment in pacemaker requirement among those with initial LBBB may be related to their lower survival rate.
While the strength of our study is its lengthy and comprehensive follow-up, the study must be ultimately interpreted in an appropriate context. Only the first ECG recorded at the time of presentation was analyzed, leaving the duration of BBB defects uncertain. Subsequent ECGs were not uniformly available, so patients with transient BBB limited to the acute period could not be distinguished from those with persistent conduction defects, and the patients we identified with BBB could not be compared with those who has no BBB on the initial ECG but later developed conduction defects of this type. Similarly, we lack data on troponin as a marker of ischemia, fascicular blocks, the time to development of complete heart block or heart failure, renal function, ventricular function and the presence or absence of concurrent cardiovascular diseases of other types, including valvular and congenital heart disease or cardiomyopathy, which could mediate the relationships between conduction disturbances and prognosis. The retrospective approach to abstraction of baseline data limits the capture of confounding variables to those documented at the time of presentation with chest pain. It is possible that observations in the predominantly Caucasian cohort may not apply to members of other ethnic groups and the same constraints apply to their extrapolation to specific patient subgroups. However, the outcomes we report are statistically robust and reflect the actual clinics course of patients in this cohort, most of whom presumably received evidence-based treatment throughout the follow-up period.
Our study reaffirms the importance of LBBB and underscores the significance of RBBB on the initial ECG in the initial risk-stratification of patients presenting with angina.
Acknowledgments
We acknowledge Jonathan L. Halperin MD for his masterful editorial comments.
This study was made possible by the Rochester Epidemiology Project (Grant #R01-AR30582 from the National Institute of Arthritis and Musculoskeletal and Skin Diseases).
Footnotes
Disclosure: The authors have no conflicts to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hindman MC, Wagner GS, JaRo M, Atkins JM, Scheinman MM, DeSanctis RW, Hutter AH, Jr, Yeatman L, Rubenfire M, Pujura C, Rubin M, Morris JJ. The clinical significance of bundle branch block complicating acute myocardial infarction. 1. Clinical characteristics, hospital mortality, and one-year follow-up. Circulation. 1978;58:679–688. doi: 10.1161/01.cir.58.4.679. [DOI] [PubMed] [Google Scholar]
- 2.Ricou F, Nicod P, Gilpin E, Henning H, Ross J., Jr Influence of right bundle branch block on short- and long-term survival after acute anterior myocardial infarction. J Am Coll Cardiol. 1991;17:858–863. doi: 10.1016/0735-1097(91)90865-7. [DOI] [PubMed] [Google Scholar]
- 3.Go AS, Barron HV, Rundle AC, Ornato JP, Avins AL. Bundle-branch block and inhospital mortality in acute myocardial infarction. National Registry of Myocardial Infarction 2 Investigators. Ann Intern Med. 1998;129:690–697. doi: 10.7326/0003-4819-129-9-199811010-00003. [DOI] [PubMed] [Google Scholar]
- 4.Melgarejo-Moreno A, Galcera-Tomas J, Garcia-Alberola A, Valdes-Chavarri M, Castillo-Soria FJ, Mira-Sanchez E, Gil-Sanchez J, Allegue-Gallego J. Incidence, clinical characteristics, and prognostic significance of right bundle-branch block in acute myocardial infarction: a study in the thrombolytic era. Circulation. 1997;96:1139–1144. doi: 10.1161/01.cir.96.4.1139. [DOI] [PubMed] [Google Scholar]
- 5.Brilakis ES, Wright RS, Kopecky SL, Reeder GS, Williams BA, Miller WL. Bundle branch block as a predictor of long-term survival after acute myocardial infarction. Am J Cardiol. 2001;88:205–209. doi: 10.1016/s0002-9149(01)01626-5. [DOI] [PubMed] [Google Scholar]
- 6.Guerrero M, Harjai K, Stone GW, Brodie B, Cox D, Boura J, Grines L, O'Neill W, Grines C. Comparison of the prognostic effect of left versus right versus no bundle branch block on presenting electrocardiogram in acute myocardial infarction patients treated with primary angioplasty in the primary angioplasty in myocardial infarction trials. Am J Cardiol. 2005;96:482–488. doi: 10.1016/j.amjcard.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 7.Kuch B, Heier M, von Scheidt W, Kling B, Hoermann A, Meisinger C. 20-year trends in clinical characteristics, therapy and short-term prognosis in acute myocardial infarction according to presenting electrocardiogram: the MONICA/KORA AMI Registry (1985–2004) J Intern Med. 2008;264:254–264. doi: 10.1111/j.1365-2796.2008.01956.x. [DOI] [PubMed] [Google Scholar]
- 8.Pope JH, Ruthazer R, Kontos MC, Beshansky JR, Griffith JL, Selker HP. The impact of electrocardiographic left ventricular hypertrophy and bundle branch block on the triage and outcome of ED patients with a suspected acute coronary syndrome: a multicenter study. Am J Emerg Med. 2004;22:156–163. doi: 10.1016/j.ajem.2004.02.020. [DOI] [PubMed] [Google Scholar]
- 9.Kurland LT, Molgaard CA. The patient record in epidemiology. Sci Am. 1981;245:54–63. doi: 10.1038/scientificamerican1081-54. [DOI] [PubMed] [Google Scholar]
- 10.Diamond GA. A clinically relevant classification of chest discomfort. J Am Coll Cardiol. 1983;1:574–575. doi: 10.1016/s0735-1097(83)80093-x. [DOI] [PubMed] [Google Scholar]
- 11.Thrainsdottir IS, Hardarson T, Thorgeirsson G, Sigvaldason H, Sigfusson N. The epidemiology of right bundle branch block and its association with cardiovascular morbidity--the Reykjavik Study. Eur Heart J. 1993;14:1590–1596. doi: 10.1093/eurheartj/14.12.1590. [DOI] [PubMed] [Google Scholar]
- 12.Barsheshet A, Leor J, Goldbourt U, Garty M, Schwartz R, Behar S, Luria D, Eldar M, Glikson M. Effect of bundle branch block patterns on mortality in hospitalized patients with heart failure. Am J Cardiol. 2008;101:1303–1308. doi: 10.1016/j.amjcard.2007.12.035. [DOI] [PubMed] [Google Scholar]
- 13.Eriksson P, Wilhelmsen L, Rosengren A. Bundle-branch block in middle-aged men: risk of complications and death over 28 years. The Primary Prevention Study in Goteborg, Sweden. Eur Heart J. 2005;26:2300–2306. doi: 10.1093/eurheartj/ehi580. [DOI] [PubMed] [Google Scholar]
- 14.Fahy GJ, Pinski SL, Miller DP, McCabe N, Pye C, Walsh MJ, Robinson K. Natural history of isolated bundle branch block. Am J Cardiol. 1996;77:1185–1190. doi: 10.1016/s0002-9149(96)00160-9. [DOI] [PubMed] [Google Scholar]
- 15.Hesse B, Diaz LA, Snader CE, Blackstone EH, Lauer MS. Complete bundle branch block as an independent predictor of all-cause mortality: report of 7,073 patients referred for nuclear exercise testing. Am J Med. 2001;110:253–259. doi: 10.1016/s0002-9343(00)00713-0. [DOI] [PubMed] [Google Scholar]
- 16.Miller WL, Ballman KV, Hodge DO, Rodeheffer RJ, Hammill SC. Risk factor implications of incidentally discovered uncomplicated bundle branch block. Mayo Clin Proc. 2005;80:1585–1590. doi: 10.4065/80.12.1585. [DOI] [PubMed] [Google Scholar]
- 17.Rotman M, Triebwasser JH. A clinical and follow-up study of right and left bundle branch block. Circulation. 1975;51:477–484. doi: 10.1161/01.cir.51.3.477. [DOI] [PubMed] [Google Scholar]
- 18.Fleg JL, Das DN, Lakatta EG. Right bundle branch block: long-term prognosis in apparently healthy men. J Am Coll Cardiol. 1983;1:887–892. doi: 10.1016/s0735-1097(83)80204-6. [DOI] [PubMed] [Google Scholar]
- 19.Freedman RA, Alderman EL, Sheffield LT, Saporito M, Fisher LD. Bundle branch block in patients with chronic coronary artery disease: angiographic correlates and prognostic significance. J Am Coll Cardiol. 1987;10:73–80. doi: 10.1016/s0735-1097(87)80162-6. [DOI] [PubMed] [Google Scholar]
- 20.Menotti A, Mulder I, Kromhout D, Nissinen A, Feskens EJ, Giampaoli S. The association of silent electrocardiographic findings with coronary deaths among elderly men in three European countries. The FINE study. Acta Cardiol. 2001;56:27–36. doi: 10.2143/AC.56.1.2005590. [DOI] [PubMed] [Google Scholar]
- 21.Schneider JF, Thomas HE, Jr, Sorlie P, Kreger BE, McNamara PM, Kannel WB. Comparative features of newly acquired left and right bundle branch block in the general population: the Framingham study. Am J Cardiol. 1981;47:931–940. doi: 10.1016/0002-9149(81)90196-x. [DOI] [PubMed] [Google Scholar]
- 22.Stenestrand U, Tabrizi F, Lindback J, Englund A, Rosenqvist M, Wallentin L. Comorbidity and myocardial dysfunction are the main explanations for the higher 1-year mortality in acute myocardial infarction with left bundle-branch block. Circulation. 2004;110:1896–902. doi: 10.1161/01.CIR.0000143136.51424.38. [DOI] [PubMed] [Google Scholar]
- 23.Bogale N, Orn S, James M, McCarroll K, de Luna AB, Dickstein K. Usefulness of either or both left and right bundle branch block at baseline or during follow-up for predicting death in patients following acute myocardial infarction. Am J Cardiol. 2007;99:647–650. doi: 10.1016/j.amjcard.2006.09.113. [DOI] [PubMed] [Google Scholar]
- 24.Ciampi Q, Petruzziello B, Della Porta M, Caputo S, Manganiello V, Astarita C, Villari B. Effect of intraventricular dyssynchrony on diastolic function and exercise tolerance in patients with heart failure. Eur J Echocardiogr. 2009;10:907–913. doi: 10.1093/ejechocard/jep094. [DOI] [PubMed] [Google Scholar]
- 25.Grines CL, Bashore TM, Boudoulas H, Olson S, Shafer P, Wooley CF. Functional abnormalities in isolated left bundle branch block. The effect of interventricular asynchrony. Circulation. 1989;79:845–853. doi: 10.1161/01.cir.79.4.845. [DOI] [PubMed] [Google Scholar]
- 26.McAnulty JH, Rahimtoola SH, Murphy E, DeMots H, Ritzmann L, Kanarek PE, Kauffman S. Natural history of “high-risk” bundle-branch block: final report of a prospective study. N Engl J Med. 1982;307:137–143. doi: 10.1056/NEJM198207153070301. [DOI] [PubMed] [Google Scholar]