Abstract
OBJECTIVE: To develop and assess the feasibility of a novel method for identification, recruitment, and retrospective and prospective evaluation of patients with rare conditions.
PATIENTS AND METHODS: This pilot study is a novel example of “patient-initiated research.” After being approached by several members of an international disease-specific support group on a social networking site, we used it to identify patients who had been diagnosed as having at least 1 episode of spontaneous coronary artery dissection and recruited them to participate in a clinical investigation of their condition. Medical records were collected and reviewed, the original diagnosis was independently confirmed by review of imaging studies, and health status (both interval and current) was assessed via specially designed questionnaires and validated assessment tools.
RESULTS: Recruitment of all 12 participants was complete within 1 week of institutional review board approval (March 18, 2010). Data collection was completed November 18, 2010. All participants completed the study questionnaires and provided the required medical records and coronary angiograms and ancillary imaging data.
CONCLUSION: This study involving patients with spontaneous coronary artery dissection demonstrates the feasibility of and is a successful model for developing a “virtual” multicenter disease registry through disease-specific social media networks to better characterize an uncommon condition. This study is a prime example of patient-initiated research that could be used by other health care professionals and institutions.
From a patient's perspective, being diagnosed as having a rare condition is challenging. Frustration regarding the treating physicians' lack of knowledge about and experience with their specific condition is often compounded by repeated reminders regarding its obscurity. Patients grow tired of hearing how little is known and how “unique” and “unusual” they are, and those with sometimes fatal conditions are often frightened by the seeming “shotgun” or inconsistent approach to management and the explicit and implicit messages that their health care professionals have “no data” to guide treatment recommendations. Patients with rare diseases therefore increasingly seek answers, medical information, and peer support on the Internet. Our study aimed to test the feasibility of collecting retrospective and prospective clinical data and original diagnostic imaging studies from persons self-identified with spontaneous coronary artery dissection (SCAD) in an Internet-based heart disease support network.
First described in 1931, SCAD is a rare, poorly understood cause of myocardial infarction. It occurs in relatively young persons1 and represents a tiny proportion (0.07%-1.1%) of patients undergoing angiography in most registries and series.2-4 Among reported case series ranging from 3 to 47 cases, there is an approximate 2:1 female predominance. About one third of the cases in women occur in the peripartum period. SCAD may present as sudden death,5 angina, or myocardial infarction and may be responsible for as many as 1 of 10 episodes of acute coronary syndrome in women younger than 50 years.2 Despite hundreds of published case reports and small case series,2-4,6-13 to our knowledge only 1 SCAD patient registry has been developed,5 and no data from multicenter clinical trials are available to guide treatment. Because of the paucity of clinical data and inconsistent follow-up and reporting, the prevalence, recurrence rate, and long-term prognosis after SCAD remain uncertain,5,14-18 and the underlying etiology and optimal short- and long-term management are ambiguous.18,19 As with other poorly understood conditions, many survivors are highly active in seeking information from any available source and seek to learn from experiences of others similarly affected.
PATIENTS AND METHODS
A member of a social networking Internet site of geographically diverse women with a self-reported diagnosis of SCAD approached 1 of the authors (S.N.H.) and advocated for further research on her condition. We immediately recognized the value of accessing and comparing the disease experiences and medical records from this relatively large pool of persons with SCAD and the important contributions it could make to our current knowledge of the condition. However, we were uncertain whether we would be able to obtain relevant records and current health status from individuals who lived and had received their medical care throughout the world and were connected only by this Internet site. We designed this pilot study to assess the feasibility of developing a virtual multicenter SCAD registry by recruiting study participants from a social networking Web site and collecting and analyzing their medical records and imaging data. Because minimal data are available on the long-term follow-up of SCAD, the feasibility of prospective data collection was also assessed.
Inspire (http://www.inspire.com) is a social networking site for women with heart disease developed by Women-Heart: The National Coalition for Women with Heart Disease (www.womenheart.org) to provide a venue for sharing information about heart disease, community and medical resources, and networking and support opportunities.
Most participants share their specific cardiac diagnoses on the site, and those with SCAD joined an informal subgroup that allowed mutual support and sharing of personal experiences with their illness. This group was notably large with posts and contributions from more than 70 women, a membership nearly double the size of the largest reported case series of SCAD. Additionally, several members had developed and shared specific research agendas to address their particular questions about SCAD as well as broader areas of inquiry. Anecdotal reports, Internet posts, and personal communication with affected patients suggest widespread psychosocial distress and perceptions of helplessness.
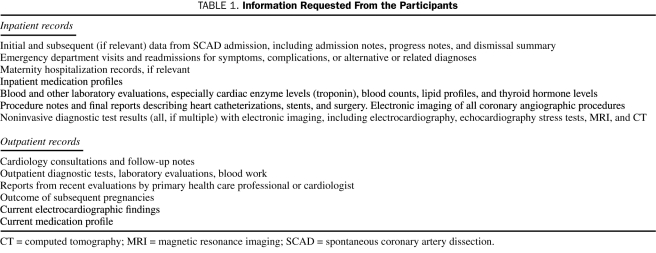
Our study was approved by the Mayo Clinic Institutional Review Board for a pilot of 12 participants. This number of participants was chosen on the basis of recommendations for pilot study design provided by the Mayo Center for Translational Science Activities staff and our estimate of how many medical records requests we would need to demonstrate the feasibility of our process. Those eligible for the study were sent a consent form, the Patient Health Questionnaire (PHQ-9), General Anxiety Disorder scale (GAD-7), the Mayo Clinic Women's Heart Clinic Cardiovascular Risk Assessment, and a SCAD questionnaire developed by our group to provide supplemental information including but not limited to current health status and medical therapies, reproductive plans, daily physical activity, and the presence of known and potential risk factors for SCAD. In addition to analysis of the questionnaire data, the pilot was designed to assess the feasibility of collecting this type of prospective information should the study be expanded to a larger number of persons recruited in this manner. For the retrospective component, we requested that participants obtain and submit complete medical records with an emphasis on their initial SCAD event and subsequent cardiovascular care (Table 1).
TABLE 1.
Information Requested From the Participants
The first 12 women to return the consent form and questionnaires were included in the pilot analysis. Others expressing interest were advised that they would be contacted if we subsequently extended the study. We undertook all measures to deidentify and protect patient data according to the Health Insurance Portability and Accountability Act provisions.
RESULTS
Our study harnessed the “natural” communication among the group to notify potential participants of the planned study via an Internet post by a single member. Active recruitment was unnecessary because, within 7 days of the Mayo Clinic Institutional Review Board approval (March 18, 2010), 18 women had requested study information and enrollment documents, demonstrating group members' eagerness to advance the study of their condition. We arbitrarily elected to enroll the first 12 participants who completed consent forms and questionnaires.
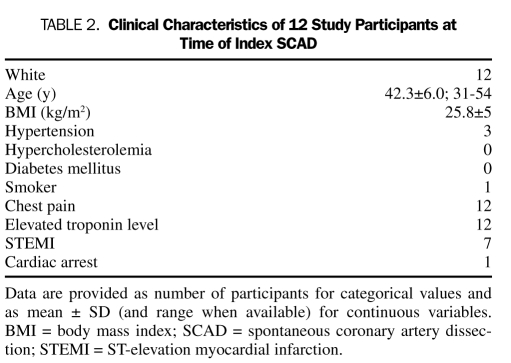
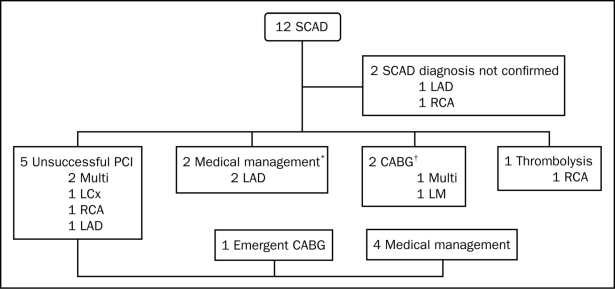
Women were enrolled between 6 months and 7.5 years (mean, 3 years) from their SCAD event, and the mean age ± SD at the event was 42.3±6.0 years (Table 2). All participants were white. Initial treatment took place in the United States (n=8), Canada (n=2), England (n=1), and New Zealand (n=1). All study materials had been received by June 28, 2010, with the exception of 3 coronary angiograms. The last of these was received on November 18, 2010. All participant questionnaires, records, and coronary angiograms were obtained and reviewed, and coronary angiograms were reviewed by an interventional cardiologist (R.G.) to confirm the diagnosis of SCAD. Ten of the angiograms were consistent with the diagnosis of SCAD (Figure 1). Two patients had dissections that could not be confirmed as spontaneous. Data otherwise were complete and are summarized in the Appendix.
TABLE 2.
Clinical Characteristics of 12 Study Participants at Time of Index SCAD
FIGURE 1.
Coronary angiographic findings and course of treatment among study participants. CABG = coronary artery bypass grafting; LAD = left anterior descending; LCx = left circumflex; LM = left main; Multi = multivessel; PCI = percutaneous coronary intervention; RCA = right coronary artery; SCAD = spontaneous coronary artery dissection.
*1 Postpartum case; †2 Postpartum cases.
DISCUSSION
This unique pilot study demonstrates the feasibility of developing collaborative research initiatives with members of an international disease-specific social networking community. Many organized patient advocacy groups have developed research agendas. However, our highly engaged and committed study participants, linked only via the Internet, demonstrated levels of sophistication and specificity in their patient-initiated research questions that were on par with those developed by formally organized groups. The speed of participant recruitment via the networking site (1 week) was surprising. We did not expect to enroll all of our participants before having the opportunity to post the study on Mayo Clinic's clinical trial Web site and had to turn volunteers away because the institutional review board–approved maximum had been reached.
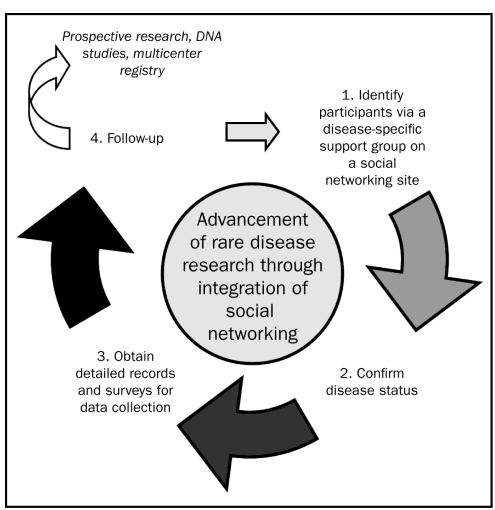
On the basis of our experience with this project using novel recruitment methods and collection of contemporaneous medical records, we propose that this manner of participant recruitment, case ascertainment, and retrospective and prospective data collection (initial SCAD incidents, outcomes, medical management, current physical and mental health status, and overall well-being) could be applied more broadly to the entire SCAD social networking group and customized for the study of other rare diseases (Figure 2).
FIGURE 2.
Flow chart detailing the steps by which social networking sites can be used to recruit study participants with uncommon conditions.
Identifying and recruiting study participants with rare conditions such as SCAD can be a formidable challenge because no single medical center has adequate experience and/or patient volume. A formal multicenter registry will ultimately be necessary to recruit patients early in the acute phase of their condition, and subsequently randomized clinical trials may become feasible. Until it is created, however, this unique model involving self-organized patients with SCAD provides an excellent option for a virtual multicenter registry. The rapid enrollment of participants in this pilot study through a social networking platform suggests a way to harness patient enthusiasm and organize studies that have been heretofore impractical.
Data that could be collected in this manner include clinically relevant information about demographics, natural history in survivors, and treatment patterns. We found the personal narrative prepared by participants about their disease and health care experiences to be extremely helpful in filling in gaps in medical history, clarifying time lines and generally complementing the medical records in a manner similar to obtaining a face-to-face clinical history. As in other registries, findings can generate hypotheses and future inquiry. Our report serves as a proof of concept, and extending enrollment to the almost 100 women with SCAD currently on Inspire.com will produce the largest SCAD registry to date and allow development of an imaging and DNA database to complement the retrospective assessment. Moreover, in the future this process could be extended via online surveys and development of electronic centralized data repositories with direct health record data transfer, assuming data security and Health Insurance Portability and Accountability Act compliance could be ensured.
Obtaining complete medical records is crucial for this type of review. Our participants were highly motivated to provide all requested records. We were impressed with the successful collection of original diagnostic coronary artery imaging for review in all of our pilot participants despite their geographic diversity, the challenges of our medical record retrieval system, and the lack of participants' pre-existing clinical relationship with the investigators. Several participants asked their personal physicians to contact us to confirm our data needs, and 3 potential study participants' physicians contacted an investigator (S.N.H.) at the patients' request to ensure that our study was “legitimate.” Given the possibility of Internet scams and the fact that the patients had not yet received communication directly from the Mayo Clinic study team, this reflects appropriate caution. In future studies, posting key information available on Mayo Clinic's Web site for institutional clinical trials before the notice goes “viral” on the patients' social networking site will be important.
As an offshoot of and surrogate for in-person disease-specific support groups, patients have organized online to share experiences and provide mutual support for well over a decade. The best-funded and most prominent disease-focused platforms tend to aggregate around more common conditions such as diabetes mellitus and breast cancer. In-person support groups for conditions as rare as SCAD are impractical if not impossible. On the basis of current estimates of prevalence, only a few dozen SCAD survivors are likely to reside in even a large metropolitan area. An online site with no geographic limitations is more likely to reach critical mass.
Social networking tools have had important health and humanitarian effects ranging from crowd-sourced epidemiology studies to earthquake relief.20,21 Projects such as Ushahidi (www.ushahidi.com) have enabled populations affected by a mass incident to easily pool and organize their knowledge. New York University professor Clay Shirky calls platforms like these mechanisms for harnessing society's “cognitive surplus.”20 Our approach differed from these projects in that it applied social tools not in headline-grabbing localized events such as pandemics and earthquakes, but rather to an unusual condition unnoticed by the broader population because those affected are widely dispersed.
Building patient registries has traditionally been costly, particularly for rare conditions in which multiple centers are needed to achieve sufficient size. Busy clinician investigators also have many competing demands for attention that may hinder their ability to organize a registry, which requires outreach to other centers and convincing peers to cooperate, adding organizational overhead costs for coordination. This pilot study strongly suggests that social networking tools can catalyze community action and that the energy and commitment of affected patients can overcome inertia and reduce registry costs. The singular motivation and focus of patients with little-understood conditions, combined with the natural organizing framework in a social networking site, may significantly improve the timeliness and cost-effectiveness of research in these conditions.
Women, younger patients, and patients with uncommon medical conditions for which no consensus exists on etiology, treatment, and prognosis might be expected to search more broadly for answers to their questions on the Internet or through other less conventional sources of medical information compared with men, older patients, and those with more common disorders.22 After our study was under way, we were contacted by a number of persons with SCAD or their family members about clinical and research questions. They were not members or aware of the original Internet networking group. Although not systematically assessed, these persons reported that they had heard of our SCAD research from a variety of sources, including specific Internet search activity, personal blogs, Facebook, “word of mouth” through other SCAD patients, and Mayo Clinic Web sites. This suggests that the inherent interconnectivity of the Internet, combined with a strong drive to acquire hard-to-find health information, can be leveraged even more extensively in the future.
Using lessons learned from this pilot study, we will expand our study to recruit eligible participants via standard methods as well as through communication with this and other heart disease–based social networking sites. Ultimately, we aim to provide a higher-powered, descriptive database including prospective biospecimen and DNA collection, physical and mental well-being assessment of participants, and comparisons with age- and sex-matched controls. With collaborating centers, we plan to develop a prospective trial to further guide short- and long-term treatment because, as demonstrated by our cohort and others,2-4,6-13 significant variability exists in the short- and long-term management of SCAD.
LIMITATIONS
This pilot was limited by its design to reporting on a small and highly selected group of female survivors of SCAD from a single social networking site. We acknowledge an unavoidable selection bias and recognize that our findings may not be generalizable because our study group is a convenience sample including only female survivors of SCAD with Internet access who belong to a single networking group. However, the pool of interested participants is large (although broadly dispersed) in relation to the prevalence of the condition, and expanding the study to other online groups and men will reduce selection bias. In a condition with a reported sudden death rate of up to 50%,5 this study does not represent the full spectrum of SCAD. Our group has been contacted by family members of several persons who died of SCAD. We plan to explore the feasibility of integrating the data provided by these families into our virtual registry.
CONCLUSION
Our pilot demonstrates successful social networking–enabled research participant engagement and recruitment among members of an international disease-specific online community and outlines a novel methodology to obtain retrospective and prospective data from persons with uncommon, poorly understood conditions. Our pilot serves as a model as we develop a more extensive, much-needed retrospective and prospective study of SCAD. This process of recruiting research trial participants with self-identified conditions from social networking Internet sites represents a mechanism to develop a novel “multicenter disease registry” that could be replicated to study and propel medical advances in other uncommon conditions that may not otherwise be subjects of active investigation.
APPENDIX. Summary Data From SCAD Pilot Study Participants
The clinical characteristics of patients at the time of their initial spontaneous coronary artery dissection (SCAD) event are summarized in Table 2. None withdrew from the study. All participants were white women. Most women had few or no conventional cardiovascular risk factors and were otherwise healthy and active. Of the participants, 9 exercised regularly, and 4 exercised 30 to 60 minutes more than 3 times per week. All presented initially with chest pain and elevated troponin levels. In our participants, 1 or more of each of the major coronary arteries were affected: left main (n=1), left anterior descending (n=4), left circumflex (n=1), right (n=3), and multivessel dissection (n=3). The participant course of care is outlined in Figure 1.
At the time of SCAD, no women were actively receiving treatment for infertility, 1 was taking oral contraceptives, 1 was taking an estrogen and progesterone combination (Prempro), and 3 were postpartum (14, 60, and 120 days from parturition). One described a history of fertility treatment more than 10 years before her SCAD episode. Another with postpartum SCAD had undergone previous medical and in vitro fertilization therapy and carried a fibrillin-1 gene abnormality. One was diagnosed as having fibromuscular dysplasia involving the carotid and vertebral arteries. Of the participants, 2 had premorbid diagnoses of rheumatoid arthritis, and 2 others had thyroid dysfunction. One patient had recurrence of SCAD 2 months after the initial dissection.
Seven participants endorsed a diagnosis of depression, anxiety, or a combination thereof. The mean ± SD Patient Health Questionnaire (PHQ-9) score was 3.1±2.7, with a range of 1 to 9. The mean General Anxiety Disorder scale (GAD-7) score was 3.5±3.5, with a range of 0 to 13. When asked whether the diagnosis or treatment of SCAD had affected quality of life, 7 participants replied “yes,” and 1 replied “I don't know.” When asked if their history of SCAD had affected pregnancy plans, 5 replied “yes.” One woman reported having a hysterectomy solely because of her history of SCAD, and another woman indicated that she would terminate any future pregnancies for the same reason. One woman planned to attempt a pregnancy despite her history of SCAD, and 1 woman was pregnant at the time of the survey.
Supplementary Material
Acknowledgments
The authors would like to acknowledge assistance from members of the cardiovascular secretarial staff, including Cynthia Allen and Laura Brusse.
Footnotes
For editorial comment, see page 836
REFERENCES
- 1. Pretty HC. Dissecting aneurysm of coronary artery in a woman aged 42: rupture. Br Med J. 1931;1:667 [Google Scholar]
- 2. Vanzetto G, Berger-Coz E, Barone-Rochette G, et al. Prevalence, therapeutic management and medium-term prognosis of spontaneous coronary artery dissection: results from a database of 11,605 patients. Eur J Cardiothorac Surg. 2009;35(2):250-254 [DOI] [PubMed] [Google Scholar]
- 3. Mortensen KH, Thuesen L, Kristensen IB, Christiansen EH. Spontaneous coronary artery dissection: a Western Denmark Heart Registry study. Catheter Cardiovasc Interv. 2009;74(5):710-717 [DOI] [PubMed] [Google Scholar]
- 4. Hering D, Piper C, Hohmann C, Schultheiss HP, Horstkotte D. Prospective study of the incidence, pathogenesis and therapy of spontaneous, by coronary angiography diagnosed coronary artery dissection [article in German]. Z Kardiol. 1998;87(12):961-970 [DOI] [PubMed] [Google Scholar]
- 5. Fontanelli A, Olivari Z, La Vecchia L, et al. ; DISCOVERY Investigators Spontaneous dissections of coronary arteries and acute coronary syndromes: rationale and design of the DISCOVERY, a multicenter prospective registry with a case-control group. J Cardiovasc Med (Hagerstown). 2009;10(1):94-99 [DOI] [PubMed] [Google Scholar]
- 6. Motreff P, Souteyrand G, Dauphin C, Eschalier R, Cassagnes J, Lusson JR. Management of spontaneous coronary artery dissection: review of the literature and discussion based on a series of 12 young women with acute coronary syndrome. Cardiology. 2010;115(1):10-18 [DOI] [PubMed] [Google Scholar]
- 7. Jorgensen MB, Aharonian V, Mansukhani P, Mahrer PR. Spontaneous coronary dissection: a cluster of cases with this rare finding. Am Heart J. 1994;127(5):1382-1387 [DOI] [PubMed] [Google Scholar]
- 8. DeMaio SJ Jr, Kinsella SH, Silverman ME. Clinical course and long-term prognosis of spontaneous coronary artery dissection. Am J Cardiol. 1989;64(8):471-474 [DOI] [PubMed] [Google Scholar]
- 9. Maeder M, Ammann P, Angehrn W, Rickli H. Idiopathic spontaneous coronary artery dissection: incidence, diagnosis and treatment. Int J Cardiol. 2005;101(3):363-369 [DOI] [PubMed] [Google Scholar]
- 10. Zampieri P, Aggio S, Roncon L, et al. Follow up after spontaneous coronary artery dissection: a report of five cases. Heart. 1996;75(2):206-209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pasalodos Pita J, Vasquez Gonzalez N, Perez Alvarez L, Vasquez Rodriguez JM, Castro Bieras A. Spontaneous coronary artery dissection. Cathet Cardiovasc Diagn. 1994;32(1):27-32 [DOI] [PubMed] [Google Scholar]
- 12. Nishikawa H, Nakanishi S, Nishiyama S, Nishimura S, Seki A, Yamaguchi H. Primary coronary artery dissection observed at coronary angiography. Am J Cardiol. 1988;61(8):645-648 [DOI] [PubMed] [Google Scholar]
- 13. Celik SK, Sagcan A, Altintig A, Yuksel M, Akin M, Kultursay H. Primary spontaneous coronary artery dissections in atherosclerotic patients: report of nine cases with review of the pertinent literature. Eur J Cardiothorac Surg. 2001;20(3):573-576 [DOI] [PubMed] [Google Scholar]
- 14. Thompson EA, Ferraris S, Gress T, Ferraris V. Gender differences and predictors of mortality in spontaneous coronary artery dissection: a review of reported cases. J Invasive Cardiol. 2005;17(1):59-61 [PubMed] [Google Scholar]
- 15. Kamran M, Guptan A, Bogal M. Spontaneous coronary artery dissection: case series and review. J Invasive Cardiol. 2008;20:553-559 [PubMed] [Google Scholar]
- 16. Basile C, Lucarelli K, Langialonga T. Spontaneous coronary artery dissection: one more extrarenal manifestation of autosomal dominant polycystic kidney disease? J Nephrol. 2009;22(3):414-416 [PubMed] [Google Scholar]
- 17. Borczuk AC, van Hoeven KH, Factor SM. Review and hypothesis: the eosinophil and peripartum heart disease (myocarditis and coronary artery dissection): coincidence or pathogenetic significance? Cardiovasc Res. 1997;33(3):527-532 [DOI] [PubMed] [Google Scholar]
- 18. Shamloo BK, Chintala RS, Nasur A, et al. Spontaneous coronary artery dissection: aggressive vs. conservative therapy. J Invasive Cardiol. 2010;22(5):222-228 [PubMed] [Google Scholar]
- 19. Hoye A. Spontaneous coronary artery dissection: time for a concerted effort to better understand this rare condition. J Invasive Cardiol. 2010;22(5):229-230 [PubMed] [Google Scholar]
- 20. Ushahidi-Haiti@Tufts University Haiti: the 2010 earthquake in Haiti. http://haiti.ushahidi.com Accessed July 6, 2011
- 21. Freifeld CC, Chunara R, Mekaru SR, et al. Participatory epidemiology: use of mobile phones for community-based health reporting. PLoS Med. 2010;7(12):e1000376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Atkinson NL, Saperstein SL, Pleis J. Using the internet for health-related activities: findings from a national probability sample. J Med Internet Res. 2009;11(1):e4 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.