Abstract
Many adolescents and adults with asthma continue to have poorly controlled disease, often attributable to poor adherence to asthma therapy. Failure to adhere to recommended treatment may result from a desire to avoid regular reliance on medications, inappropriate high tolerance of asthma symptoms, failure to perceive the chronic nature of asthma, and poor inhaler technique. Primary care physicians need to find opportunities and methods to address these and other issues related to poor asthma control. Few adolescents or adults with asthma currently have asthma “checkup” visits, usually seeking medical care only with an exacerbation. Therefore, nonrespiratory-related office visits represent an important opportunity to assess baseline asthma control and the factors that most commonly lead to poor control. Tools such as the Asthma Control Test, the Asthma Therapy Assessment Questionnaire, the Asthma Control Questionnaire, and the Asthma APGAR provide standardized, patient-friendly ways to capture necessary asthma information. For uncontrolled asthma, physicians can refer to the stepwise approach in the 2007 National Asthma Education and Prevention Program guidelines to adjust medication use, but they must consider step-up decisions in the context of quality of the patient's inhaler technique, adherence, and ability to recognize and avoid or eliminate triggers. For this review, a literature search of PubMed from 2000 through August 31, 2010, was performed using the following terms (or a combination of these terms): asthma, asthma control, primary care, NAEPP guidelines, assessment, uncontrolled asthma, burden, impact, assessment tools, triggers, pharmacotherapy, safety. Studies were limited to human studies published in English. Articles were also identified by a manual search of bibliographies from retrieved articles and from article archives of the author.
ACQ = Asthma Control Questionnaire; ACT = Asthma Control Test; Asthma APGAR = Asthma Activity limitation/Persistence of symptoms/Triggers/Asthma medications/Response to therapy tool; ATAQ = Asthma Therapy Assessment Questionnaire; FEV1 = forced expiratory volume in 1 second; ICS = inhaled corticosteroid; IgE = immunoglobulin E; LABA = long-acting β2-agonist; NAEPP = National Asthma Education and Prevention Program; SABA = short-acting β2-agonist
Despite the many available options for the management of asthma, a large proportion of adolescents (aged >12 years) and adults with asthma still have uncontrolled disease.1 numerous factors contribute to this problem, most of which can be addressed by the primary care physician. This review identifies factors that impact asthma control in adolescents and adults, provides an overview of the 2007 National Asthma Education and Prevention Program (NAEPP) asthma guidelines for improving symptom control, discusses key assessment times and tools important for translation of those guidelines into practice, and discusses situations in which difficult-to-control asthma may require specialist care.
A literature search of PubMed from 2000 through August 31, 2010, was performed using the following terms (or a combination of these terms): asthma, asthma control, primary care, NAEPP guidelines, assessment, uncontrolled asthma, burden, impact, assessment tools, triggers, pharmacotherapy, safety. Studies were limited to human studies published in English. Articles were also identified by a manual search of bibliographies from retrieved articles and from article archives of the author.
IMPACT OF UNCONTROLLED ASTHMA ON ADOLESCENTS AND ADULTS
Adolescence can be defined by several age ranges, with the most common definition encompassing those aged 12 to 18 years.2 In this age group, asthma is common, affecting up to 22% of high school–aged children,3 and usually inadequately controlled.1,2 the level of control for adults may be higher but still is less than desirable. The Epidemiology and Natural History of Asthma: Outcomes and Treatment Regimens (TENOR) study observed more than 3500 patients aged 13 years or older (mean age, 17.9 years) during a period of several years while they continued to receive their “usual care.” At baseline, 95% of these patients had uncontrolled asthma; during the first 2 years of observation, 83% had uncontrolled asthma at all assessments, and only 1.3% had controlled asthma at all assessments.1
The impact of uncontrolled asthma on quality of life and productivity is substantial. A questionnaire-based study of 108 adolescents (aged 12-18 years) showed that impairment in areas of symptoms, emotions, and activities was significantly higher when asthma was uncontrolled vs controlled (P<.001).2 A higher proportion of adolescents with uncontrolled asthma reported that they missed 1 or more
Article Highlights
Planned asthma visits are helpful, but other opportunities should be used as well, including visits for sports or camp physicals, visits required for school, and visits for any other illness
In addition to controlling allergies and limiting viral infections, important factors in avoiding exacerbations and maintaining control of asthma are knowing and avoiding other triggers, improving adherence, and mastering inhaler technique
Adherence should be approached by asking, “What kinds of problems do you have using all of your asthma medications daily?” Inhaler technique should be reviewed at every visit by having the patient bring his or her inhalers and demonstrate technique with each device
Asthma triggers should be assessed to help prevent exacerbations and loss of control
A formal asthma control tool can ensure that all important aspects of asthma control are assessed and documented for future comparisons
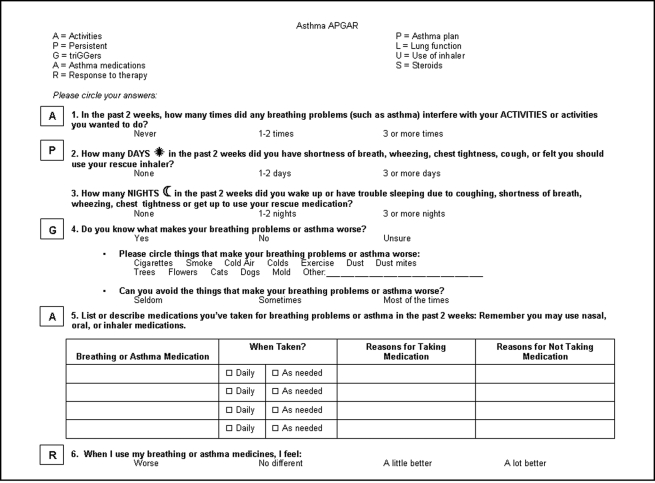
Tools such as the Asthma APGAR (Asthma Activity limitation/Persistence of symptoms/Triggers/Asthma medications/Response to therapy) can provide the primary care physician or other clinician with control assessment and guides to next steps in asthma management
days of school in the prior week (34.0% vs 3.5% of patients with controlled asthma; P<.001), came to school late at least 1 day because of asthma (34.0% vs 3.5%; P<.001), left school early 1 or more days because of asthma (21.3% vs 1.8%; P=.003), and/or developed respiratory symptoms while at school (76.6% vs 29.3%; P<.001).2
As in adolescents, the prevalence of uncontrolled asthma in adults (aged >18 years) is often more than 50%; it was 58.0% in a survey of 2238 adults across the United States.4 Asthma control status in the TENOR study of adults (range, 20-89 years) with difficult-to-treat asthma was inversely correlated with the patient's health-related quality of life (P<.001).5 Asthma care in adults is more costly for those whose lack of control results in urgent, emergency, and hospital-based care. The Medical Expenditure Panel Surveys estimated that direct health care utilization cost for adults with asthma was $18 billion (2008 dollars)6 and increased to $56 billion when productivity and work loss were added.7
REASONS FOR UNCONTROLLED ASTHMA
In adolescents, physical, cognitive, and psychological changes associated with normal adolescent development may add to the challenge of managing asthma.8 Varying by the stage of adolescence, these factors may undermine adherence and therefore compromise asthma control.8 The middle adolescent years (approximately ages 15-16 years) are a particularly vulnerable period, when separation from parents and being part of one's peer group are of primary importance. Resenting the prospect of seeming different from their peers, teenagers may deny, hide, or ignore their asthma symptoms and need for medication.8 This phenomenon is evident in the trend for adolescents with chronic illness to be less adherent than younger children.9 The results of a survey of 49 adolescents (aged 14-20 years) with asthma revealed that the most prominent self-reported reason for nonadherence with their prescribed medication regimen was forgetfulness, which was reported by approximately half of the patients interviewed (n=24).10 the poorly developed abstract thinking skills and the feeling of invulnerability that characterize adolescents may impair their ability to imagine or take seriously the consequences of undertreatment of their asthma.11 During adolescence, care must change from parent-driven to patient (adolescent)-driven asthma management, requiring the adolescent to gain new self-management skills with decreasing levels of direct supervision and intervention by parents and health care professionals.8 The primary care physician can foster this self-management skills development by beginning visits with the parent and adolescent and then excusing the parent to spend most of the visit with only the teenaged patient. This approach may facilitate transfer of asthma care from the parent to the adolescent and provide confidentiality for consultations with adolescent patients to discuss smoking behavior, review inhaler technique, and develop an asthma action plan that is compatible with the adolescent's personal goals and day-to-day schedule.8
Both adolescents and adults may have several factors that contribute to uncontrolled asthma beyond failure to avoid triggers and poor inhaler technique. The gap between patients' perception of the concept of asthma control and the clinical definition of control is considerable. Some patients fail to recognize the severity of symptoms of airflow obstruction. Adults and adolescents appear to tolerate asthma symptoms most health care professionals would find unacceptable, accepting milder exacerbations as “normal,” or mistakenly attribute their symptoms to other causes (such as obesity or lack of fitness).12-14
Several other factors tend to undermine the assessment and treatment of asthma and therefore contribute to suboptimal asthma control. A review of 24 survey studies involving 57,817 children (generally classified as aged <16 years) and adults with asthma revealed that adolescents and adults with asthma, in general, lack knowledge about the underlying causes of asthma symptoms, such as allergies and triggers; have limited knowledge of treatment options, including correct use of medication; and have low expectations of receiving appropriate therapy or having a positive encounter with their health care professional.15
Poor inhaler technique should be considered in patients with asthma that is not well controlled.12 Proper asthma management also must compete with other priorities of both adults (who may be juggling family, work, and care of parents) and adolescents (who divide their time among school, homework, sports, and other activities).11 Both adolescents and adults may have competing health priorities because of the need to care for other chronic diseases in addition to asthma. Finally, many adolescents and adults have fears of dependence on asthma treatment and the adverse effects of regimens that include systemic or inhaled corticosteroids.12,16
KEY OPPORTUNITIES FOR ASSESSMENT OF ASTHMA CONTROL
Although physicians usually limit review or discussion of asthma control to respiratory-related visits, the lack of routine asthma visits and the adverse impact of uncontrolled asthma suggest a need to seize the opportunity of “nontraditional” junctures—ie, office or clinic visits for nonrespiratory reasons—to assess and manage uncontrolled asthma.17 This strategy is particularly important for adolescents, who tend to avoid regular follow-up appointments or consultations with a physician.8 Office visits for nonrespiratory reasons were also proven to be an opportunity for intervention in adults in a multisite, cross-sectional survey study that assessed the prevalence of uncontrolled asthma among adult patients (aged ≥18 years).17 Nearly half of the patients (48.0%) being seen for nonrespiratory reasons had uncontrolled asthma at the time of the visit, and 23.0% had their asthma classified as poorly controlled.17 The results from that study emphasize the importance of assessing asthma control routinely, regardless of the reason for the office visit.17
Potential nontraditional times for the primary care physician to assess asthma control in adolescents include physicals for sports or school and visits for scheduled vaccinations. In adults, opportunities to assess asthma control at nontraditional times include well-women care visits, contraceptive care visits, maternity care visits, and blood pressure or diabetes management checks. In both patient groups, physicians can capture information about asthma control during visits for any condition (especially upper respiratory tract infections, which can negatively affect asthma control), providing a standardized method to determine any required short-term adjustment in asthma therapy and help the person understand when and how to manage long-term therapy.18
Furthermore, the fluctuating nature of asthma may increase the potential for overlooking uncontrolled asthma, thus emphasizing the need for routine assessments of asthma as well as assessments at other office visits.12,19
ASTHMA CONTROL ASSESSMENT APPROACHES
How the Primary Care Physician Can Recognize Poor Asthma Control
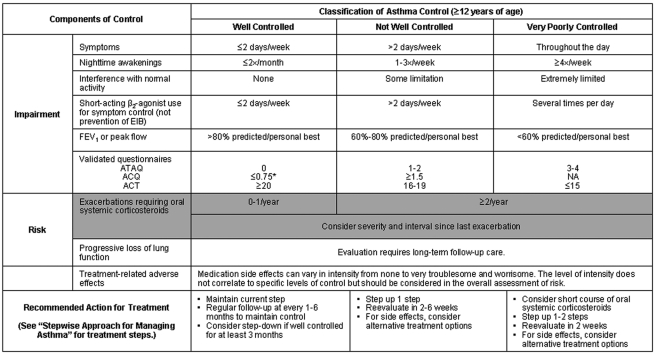
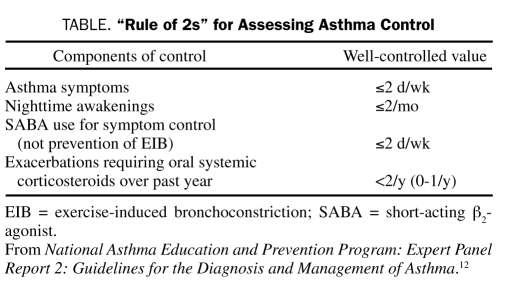
Although many reasons for uncontrolled asthma have been discussed, the first step in addressing these factors is to identify inadequate asthma control.12 The definitions of “well-controlled asthma,” “not well-controlled asthma,” and “very poorly controlled asthma” are outlined in the third report of the National Asthma Education and Prevention Program's Guidelines for the Diagnosis and Management of Asthma (Figure 112). the “Rule of 2s” provides a simplistic but useful, quick overview of asthma control (Table).9 Using the Rules of 2s still requires asking the right questions. For example, asking “How is your asthma?” and not further exploring an answer of “good,” “pretty good,” or “OK” does little to assess asthma control.
FIGURE 1.
Assessing asthma control and adjusting therapy in youths aged 12 years and older and in adults.12 The level of control is based on the most severe impairment or risk category. Assessment of the impairment domain is based on the patient's recall of the previous 2 to 4 weeks and by spirometry or peak flow measures. Symptom assessment for longer periods should reflect a global assessment, such as inquiring whether the patient's asthma is better or worse since the last visit. Before a step-up in therapy: (1) Review adherence to medication, inhaler technique, environmental control, and comorbid conditions. (2) If an alternative treatment option was used in a step, discontinue and use the preferred treatment for that step. ACQ = Asthma Control Questionnaire; ACT = Asthma Control Test; ATAQ = Asthma Therapy Assessment Questionnaire; EIB = exercise-induced bronchconstriction; FEV1 = forced expiratory volume in 1 second. Minimal Important Difference: 1.0 for the ATAQ; 0.5 for the ACQ; not determined for the ACT.
TABLE.
“Rule of 2s” for Assessing Asthma Control
Spirometry, specifically forced expiratory volume in 1 second (FEV1) expressed as %FEV1 predicted or as a proportion of forced vital capacity (FEV1/FVC), can be included in the assessment of asthma control. Spirometry can be accomplished successfully in the primary care office20 and may be helpful. For people with mild to lesser levels of moderate asthma, the FEV1 may be normal except during exacerbations, and currently no data have been published to confirm or deny the value of repeated or annual spirometry in this group. For adolescents and adults with a baseline low FEV1 (before therapy) and those who are poorly able to perceive symptoms, repeated FEV1 testing may be important in assessing control and monitoring any evidence of remodeling that can lead to a path of declining FEV1 despite therapy. Various biomarkers, such as airway hyperresponsiveness, eosinophils or eosinophilic cationic protein in blood or sputum, fractional exhaled nitric oxide concentration, serum IgE, number of positive skin tests, hydrogen ion concentration, inflammatory mediators, and various metabolites in an exhaled breath condensate, have been proposed as potential tests that may provide greater ease of use, simplicity, and accuracy in assessing severity of risk. Unfortunately, none of these can currently be done easily and cost-effectively in most primary care offices. In addition, several of the biomarkers require further evaluation and validation before they can be considered routine tools for clinical care.12
Tools to Facilitate Asking the Right Questions
The NAEPP Expert Panel recommends the use of validated tools to help ensure that the right questions are asked regarding asthma impairment and risk.12 Both daily diaries and control scores can provide this format. The diary should include a record of symptoms and/or peak flow, use of asthma medication, any restrictions in activity due to asthma, and triggers of exacerbations; the self-assessment questionnaire should be completed by the patient and/or a family member periodically (usually at a follow-up visit) to capture the patient's and family's impression of asthma control, self-management skills, and overall satisfaction with care.12 However, daily diaries are seldom used regularly or filled out completely by the patient.21-23 Some of the validated instruments of this kind are the Asthma Control Test (ACT), the Asthma Therapy Assessment Questionnaire (ATAQ), the Asthma Control Questionnaire (ACQ), and the Asthma Activity limitation/Persistence of symptoms/Triggers/Asthma medications/Response to therapy tool (Asthma APGAR).12,24,25 The ATAQ has been used primarily in research settings, whereas the ACQ, ACT, and Asthma APGAR have been used in clinical practice.26 The ACt and ACQ have a special version for children; the Asthma APGAR is considered usable for patients of any age.25,27,28 Both the ACQ and the ACT have been delivered in home-based settings and have shown comparable results whether mailed to the patient or completed in the office.25,29,30
The ACT is a 5-question survey used to assess limitations in work or home activities, shortness of breath, nighttime awakenings, rescue inhaler use, and patients' self-perception of asthma control during the past 4 weeks.12,31 The ACT has been validated to show that the scores are equal to an asthma specialist's evaluation of control.31 Additionally, the ACT has been shown to be an effective and practicable method for assessing asthma control across several ethnicities, including whites, African Americans, and Asians.29,32 A Spanish-language version of the ACT is also available for evaluating and discriminating asthma control.33
The ATAQ assesses asthma control by means of 4 scored questions covering 4 dimensions of asthma: nocturnal awakenings, resultant limitation of activities, overuse of quick-relief medications assessed relative to the prior 4 weeks and last 12 months, and the patient's self-perception of poor control assessed relative to the prior 4 weeks.12,34 The ATAQ has been validated to show that it can predict future risk for health care use.35
The ACQ is a 6-question survey used to measure nighttime awakenings, patients' perceptions of severity of symptoms on awakening in the morning, and limitations in activities, shortness of breath, wheeze, and rescue inhaler use during the past week. The ACQ also includes a seventh question for the clinic staff that focuses on the patient's FEV1.24 This questionnaire has been validated to show that it is comparable to the ACT questionnaire for assessing asthma control.36
The control scores obtained with these tools require the physician or other clinician to then formulate questions to ask about factors that may be adversely affecting the patient's asthma control. For example, the physician will need to ask about adherence to the patient's medication regimen and whether anything in the environment makes the patient's asthma worse.12
The Asthma APGAR (Figure 2) is a 6-question instrument that assesses the frequency of activity limitations due to asthma, daytime and nighttime symptoms, asthma medications taken (adherence), and rescue inhaler use during the prior 2 weeks, as well as knowledge of common factors that adversely affect control, such as personal triggers and effective trigger avoidance, medication adherence, and patient-perceived response to therapy.25 The Asthma APGAR patient control score is further linked to an algorithm that helps primary care physicians determine what steps to take on the basis of the patient's response to the full set of APGAR questions.25 The asthma guidelines include all the information necessary to recommend next steps, but the information is scattered throughout the many pages of the guidelines, which may make this information difficult to retrieve and the guideline recommendations difficult to follow in clinical practice.26 The Asthma APGAR algorithm provides asthma care information in one place, making the information easily accessible in clinical practice.25
FIGURE 2.
Asthma APGAR questionnaire. From J Asthma Allergy,25 with permission.
An asthma control assessment can be completed at any visit, usually by the patient while waiting for the physician or other clinician, and can be given either by the receptionist in the waiting room or by the staff escorting the patient to the examination room. Having the patient complete this information before the physician or other clinician comes into the room can save time and reinforce to the adolescent or adult the importance of information on symptoms and missed or modified activities and, when the Asthma APGAR is used, information on triggers, adherence, and locus of control.
MANAGING UNCONTROLLED ASTHMA
Stepwise Approach for Achieving and Maintaining Asthma Control
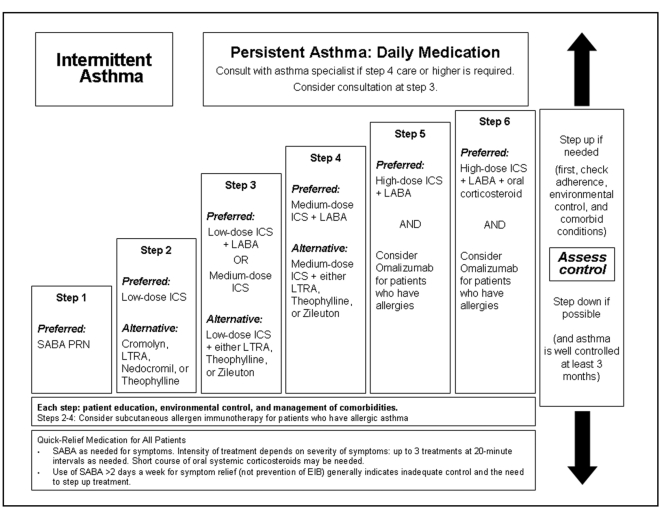
The Expert Panel 3 outlines a stepwise approach for managing asthma in adolescents (aged ≥12 years) and adults that spans a range of treatments, including as-needed short-acting β2-agonists (SABA), inhaled corticosteroids (ICSs), leukotriene modifiers, long-acting β2-agonists (LABA), theophylline, omalizumab (for patients with allergic asthma), and oral corticosteroids (Figure 3).12 Before step-up therapy is initiated, however, the guidelines advise assessing adherence, inhaler technique, environmental control, and comorbid conditions,12 a critical step that is often ignored.37,38 stepping up is of little value if the patient either has not been taking the lower-dose medication (poor adherence) or has not been getting the medication into the lungs because of poor inhaler technique.
FIGURE 3.
Stepwise approach for managing asthma in youths aged 12 years and older and in adults.12 EIB = exercise-induced bronchospasm; ICS = inhaled corticosteroid; LABA = long-acting inhaled β2-agonist; LTRA = leukotriene receptor antagonist; PRN = as needed; SABA = inhaled short-acting β2-agonist.
Step therapy provides useful guidance in selecting initial therapy based on asthma severity and in changing therapy after the potentially modifiable risk factors for poor control, such as poor adherence, have been addressed. The recommended step 1 treatment, for patients with intermittent asthma, is as-needed SABA therapy. Steps 2 through 6 are gradually intensified daily treatments for patients with persistent asthma. The preferred treatment for these steps is ICS, at escalating doses, with the addition of LABA at steps 3 through 6. Despite the US Food and Drug Administration's decision to issue a safety warning label for all LABAs, the Expert Panel 3 Report recommended the use of LABA as an adjunct therapy to ICS in patients whose asthma cannot be controlled with moderate daily doses of ICS.12 The Food and Drug Administration issued slightly different guidance, suggesting that LABA therapy be used for short durations until asthma control is achieved and then step-down therapy be attempted. Step-down therapy will work for many patients whose asthma can be controlled with long-term ICS therapy with or without the addition of other controller medications, such as montelukast.39 However, in other patients, step-down therapy will result in loss of asthma control requiring long-term use of combination therapy.12,40 Step 6 therapy adds an oral corticosteroid to the regimen. Alternative treatments for steps 2 through 4 may include leukotriene receptor antagonists, theophylline, or zileuton, depending on the step of treatment, with the alternative treatment added onto ICS at steps 3 and 4.
When full therapeutic doses of theophylline are used, serum theophylline levels must be monitored because of significant toxicities at high serum levels and variations in individual patients' metabolic clearance of the drug.12 Low (subtherapeutic)-dose theophylline can be used with limited monitoring as add-on therapy in step 5 or 6.
When patients are taking zileuton, hepatic enzymes should be monitored because of the chance of liver enzyme elevation, which requires discontinuation of zileuton therapy.
Although all people with asthma should have a SABA inhaler for quick relief, use of the SABA regularly for more than 2 days per week is considered a sign of poor control. Oral corticosteroids are used to quiet an exacerbation but should be avoided when possible by maintaining good control.12
No inhaler should ever be prescribed without providing education on inhaler technique for the specific type of inhaler. In addition, inhaler technique should be evaluated at each asthma- or respiratory-related visit and at nonrespiratory visits when asthma control is assessed. Repeated demonstrations, observation of the patient's technique, and reinforcement of proper inhaler technique are essential.12 In one study, rates of correct inhaler use increased from 57.4% at the beginning of therapy to almost 100% correct inhaler use after repeated instructions.41
Importance of Addressing Triggers
The 2 main environmental factors responsible for the development, persistence, and perhaps severity of asthma are airborne allergens and pollutants plus viral respiratory tract infections.12 Important common allergens in sensitized individuals include house-dust mites, animal dander, and cockroaches.12,42 Rates and severity of exacerbations have been linked to exposure to tobacco smoke, air pollution, and occupational substances.12
IgE plays a primary role in the mediation of allergens in asthma, activating the release of mediators from mast cells to initiate acute bronchoconstriction and perpetuate underlying airway inflammation.12,42 Given that more than half of individuals with asthma are atopic (ie, they tend to develop IgE antibodies after allergen exposure) and that allergen exposure can make asthma more severe and cause exacerbations in these patients, identification and control of triggers are essential components of management of allergic asthma.43,44
Patients must understand that exposure to certain allergens can lead to a worsening of asthma and that inexpensive strategies are available for limiting or removing allergens and irritants from their homes.12,45 Those strategies are tailored to the known allergen and require a thoroughly elicited history and perhaps in vitro or in vivo allergy testing to determine specific allergies. Moving a pet to which the adolescent or adult is sensitized from sleeping in the patient's bedroom to sleeping in another room may improve nighttime symptoms. For the grass-allergic adolescent or adult, having someone else mow the lawn and not allowing the grass to go to seed may be helpful. When allergen avoidance proves ineffective, more aggressive approaches, such as allergen immunotherapy and immunomodulator therapy, should be considered.
Allergen immunotherapy involves administration of allergens, during a course of 3 to 5 years, to modify immunoreactive responses to these allergens.12,46 Both sublingual and injected forms of desensitization therapy should be administered by trained personnel in a physician's office so that severe or life-threatening reactions (which occur rarely) can be treated appropriately.12
Several immunomodulators have been tested for their ability to provide long-term asthma control or steroid-sparing effects, or both.12 However, evidence does not support use of methotrexate, soluble interleukin 4 receptor, humanized monoclonal antibody against interleukin 5, recombinant interleukin 12, cyclosporine, intravenous immunoglobulin, gold, troleandomycin, or colchicine for the treatment of asthma.12 Omalizumab is the only immunomodulator recommended by the Expert Panel 3 for the treatment of asthma based on current evidence.12
Omalizumab is a monoclonal antibody that inhibits the binding of IgE to the high-affinity IgE receptor on basophils and mast cells, thereby limiting mediator release in response to allergen exposure.47 Few primary care physicians administer omalizumab, but they often help the patient decide about possible therapy and referral to an allergist for this treatment. Therefore, understanding the basics of the risks and benefits of omalizumab is important. The drug is indicated for treatment of moderate to severe persistent asthma in adolescents and adults whose asthma is inadequately controlled with ICS and who have proof of sensitivity to a perennial aeroallergen.47 In the 2007 asthma guidelines, this therapy is reserved for adjunctive therapy in steps 5 and 6 (the highest steps) of treatment.12 Patients may ask about the warning label commonly called a “black box warning,” and primary care physicians need to know that it addresses the 0.2% risk of anaphylaxis noted from spontaneous postmarketing reports.12 Probably because of in-office administration, adherence with this therapy has been reported to be higher than that for combination ICS plus LABA.47
REFERRAL TO OR CONSULTATION WITH A SPECIALIST
Referral to an asthma specialist (allergist, pulmonologist, or primary care physician with expertise in asthma) is recommended for adolescent or adult patients whose regular primary care physician is having difficulty achieving or maintaining asthma control; when additional education is required beyond that available in the primary care office; when therapy requires long-term high-dose ICS; or when an exacerbation occurs that requires hospitalization, especially intensive care. Each primary care physician should make this decision on the basis of his or her personal expertise and experience.12 A consultation that returns management of asthma to the primary care setting or comanagement by the primary care and specialty physicians provides the benefits of asthma expertise and the medical home environment.12
CONCLUSION
Despite the many available options for the management of asthma, a large proportion of adolescent (aged >12 years) and adult patients still have uncontrolled asthma. The impact of uncontrolled asthma is substantial in these patients, causing decrements in quality of life and in productivity and attendance at school and the workplace. Numerous factors, most commonly poor adherence, poor inhaler technique, and failure to assess control adequately, contribute to this problem, all of which can be addressed by the primary care physician. Office or clinic visits for nonrespiratory reasons represent a golden opportunity for asthma assessment and improved management. The use of tools such as the ACT, the ACQ, the ATAQ, or the Asthma APGAR can facilitate guideline-concordant care and may improve outcomes for all patients with asthma.
Supplementary Material
Acknowledgments
I thank Kristin Carlin, RPh, MBA, for writing assistance in the preparation of the submitted manuscript.
REFERENCES
- 1. Sullivan SD, Rasouliyan L, Russo PA, Kamath T, Chipps BE. Extent, patterns, and burden of uncontrolled disease in severe or difficult-to-treat asthma. Allergy. 2007;62(2):126-133 [DOI] [PubMed] [Google Scholar]
- 2. Schmier JK, Manjunath R, Halpern MT, Jones ML, Thompson K, Diette GB. The impact of inadequately controlled asthma in urban children on quality of life and productivity. Ann Allergy Asthma Immunol. 2007;98(3):245-251 [DOI] [PubMed] [Google Scholar]
- 3. Eaton DK, Kann L, Kinchen S, et al. ; Centers for Disease Control and Prevention (CDC) Youth risk behavior surveillance: United States, 2009. MMWR Surveill Summ. 2010;59(5):1-142 [PubMed] [Google Scholar]
- 4. Stanford RH, Gilsenan AW, Ziemiecki R, Zhou X, Lincourt WR, Ortega H. Predictors of uncontrolled asthma in adult and pediatric patients: analysis of the Asthma Control Characteristics and Prevalence Survey Studies (ACCESS). J Asthma. 2010;47(3):257-262 [DOI] [PubMed] [Google Scholar]
- 5. Chen H, Gould MK, Blanc PD, et al. Asthma control, severity, and quality of life: quantifying the effect of uncontrolled disease. J Allergy Clin Immunol. 2007;120(2):396-402 [DOI] [PubMed] [Google Scholar]
- 6. Sullivan PW, Ghushchyan VH, Slejko JF, Belozeroff V, Globe DR, Lin SL. The burden of adult asthma in the United States: evidence from the Medical Expenditure Panel Survey. J Allergy Clin Immunol. 2011;127(2):363-369 [DOI] [PubMed] [Google Scholar]
- 7. Barnett SB, Nurmagambetov TA. Costs of asthma in the United States: 2002-2007. J Allergy Clin Immunol. 2011;127(1):145-152 [DOI] [PubMed] [Google Scholar]
- 8. Towns SJ, van Asperen PP. Diagnosis and management of asthma in adolescents. Clin Respir J. 2009;3(2):69-76 [DOI] [PubMed] [Google Scholar]
- 9. DiMatteo MR. Variations in patients' adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42(3):200-209 [DOI] [PubMed] [Google Scholar]
- 10. Buston KM, Wood SF. Non-compliance amongst adolescents with asthma: listening to what they tell us about self-management. Fam Pract. 2000;17(2):134-138 [DOI] [PubMed] [Google Scholar]
- 11. Edgecombe K, Latter S, Peters S, Roberts G. Health experiences of adolescents with uncontrolled severe asthma. Arch Dis Child. 2010;95(12):985-991 [DOI] [PubMed] [Google Scholar]
- 12. US Department of Health and Human Services (DHS); National Institutes of Health (NIH) National Asthma Education and Prevention Program: Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. Bethesda, MD: National Institutes of Health, National Heart Lung and Blood Institute; 2007. NIH publication no: 97-4051 http://www.ncbi.nlm.nih.gov/books/NBK2358/ Accessed may 12, 2011 [Google Scholar]
- 13. Long AA. Addressing unmet needs in asthma care. P&T Digest. 2005;30(11):16-22 http://www.ptcommunity.com/ptdigest/0511_ptd_asthma/PTD_asthma_PT.pdf Accessed May 12, 2011 [Google Scholar]
- 14. Fuchs HJ, Borowitz DS, Christiansen DH, et al. ; Pulmozyme Study Group Effect of aerosolized recombinant human DNase on exacerbations of respiratory symptoms and on pulmonary function in patients with cystic fibrosis. N Engl J Med. 1994;331(10):637-642 [DOI] [PubMed] [Google Scholar]
- 15. Holgate ST, Price D, Valovirta E. Asthma out of control? A structured review of recent patient surveys. BMC Pulm Med. 2006;(6)(suppl 1):S2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Janson S, Becker G. Reasons for delay in seeking treatment for acute asthma: the patient's perspective. J Asthma. 1998;35(5):427-435 [DOI] [PubMed] [Google Scholar]
- 17. Mintz M, Gilsenan AW, Bui CL, et al. Assessment of asthma control in primary care. Curr Med Res Opin. 2009;25(10):2523-2531 [DOI] [PubMed] [Google Scholar]
- 18. Walter MJ, Castro M, Kunselman SJ, et al. Predicting worsening asthma control following the common cold. Eur Respir J. 2008;32(6):1548-1554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Carlton BG, Lucas DO, Ellis EF, Conboy-Ellis K, Shoheiber O, Stempel DA. The status of asthma control and asthma prescribing practices in the United States: results of a large prospective asthma control survey of primary care practices. J Asthma. 2005;42(7):529-535 [DOI] [PubMed] [Google Scholar]
- 20. Yawn BP, Enright PL, Lemanske RF, Jr, et al. Spirometry can be done in family physicians' offices and alters clinical decisions in management of asthma and COPD. Chest. 2007;132(4):1162-1168 [DOI] [PubMed] [Google Scholar]
- 21. Juniper EF, Bousquet J, Abetz L, Bateman ED. Identifying `well-controlled' and `not well-controlled' asthma using the Asthma Control Questionnaire. Respir Med. 2006;100(4):616-621 [DOI] [PubMed] [Google Scholar]
- 22. Juniper EF, O'Byrne PM, Ferrie PJ, King DR, Roberts JN. Measuring asthma control: clinic questionnaire or daily diary? Am J Respir Crit Care Med. 2000;162(4, pt 1):1330-1334 [DOI] [PubMed] [Google Scholar]
- 23. Hyland ME, Kenyon CA, Allen R, Howarth P. Diary keeping in asthma: comparison of written and electronic methods. BMJ. 1993;306(6876):487-489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Juniper EF, O'Byrne PM, Guyatt GH, Ferrie PJ, King DR. Development and validation of a questionnaire to measure asthma control. Eur Respir J. 1999;14(4):902-907 [DOI] [PubMed] [Google Scholar]
- 25. Yawn BP, Bertram S, Wollan P. Introduction of Asthma APGAR tools improve asthma management in primary care practices. J Asthma Allergy. 2008;1:1-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Yawn BP, Brenneman SK, Allen-Ramey FC, Cabana MD, Markson LE. Assessment of asthma severity and asthma control in children. Pediatrics. 2006;118(1):322-329 [DOI] [PubMed] [Google Scholar]
- 27. Liu AH, Zeiger R, Sorkness C, et al. Development and cross-sectional validation of the Childhood Asthma Control Test. J Allergy Clin Immunol. 2007;119(4):817-825 [DOI] [PubMed] [Google Scholar]
- 28. Juniper EF, Gruffydd-Jones K, Ward S, Svensson K. Asthma Control Questionnaire in children: validation, measurement properties, interpretation. Eur Respir J. 2010;36(6):1410-1416 [DOI] [PubMed] [Google Scholar]
- 29. Schatz M, Mosen DM, Kosinski M, et al. Validity of the Asthma Control Test completed at home. Am J Manag Care. 2007;13(12):661-667 [PubMed] [Google Scholar]
- 30. Pinnock H, Juniper EF, Sheikh A. Concordance between supervised and postal administration of the Mini Asthma Quality of Life Questionnaire (MiniAQLQ) and Asthma Control Questionnaire (ACQ) was very high. J Clin Epidemiol. 2005;58(8):809-814 [DOI] [PubMed] [Google Scholar]
- 31. Nathan RA, Sorkness CA, Kosinski M, et al. Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol. 2004;113(1):59-65 [DOI] [PubMed] [Google Scholar]
- 32. Zhou X, Ding FM, Lin JT, et al. Validity of Asthma Control Test in Chinese patients. Chin Med J (Engl). 2007;120(12):1037-1041 [PubMed] [Google Scholar]
- 33. Vega JM, Badia X, Badiola C, et al. Validation of the Spanish version of the Asthma Control Test. J Asthma. 2007;44(10):867-872 [DOI] [PubMed] [Google Scholar]
- 34. Vollmer WM, Markson LE, O'Connor E, et al. Association of asthma control with health care utilization and quality of life. Am J Respir Crit Care Med. 1999;160(5, pt 1):1647-1652 [DOI] [PubMed] [Google Scholar]
- 35. Vollmer WM, Markson LE, O'Connor E, Frazier EA, Berger M, Buist AS. Association of asthma control with health care utilization: a prospective evaluation. Am J Respir Crit Care Med. 2002;165(2):195-199 [DOI] [PubMed] [Google Scholar]
- 36. Wallenstein GV, Carranza-Rosenzweig J, Kosinski M, Blaisdell-Gross B, Gajria K, Jhingran P. A psychometric comparison of three patient-based measures of asthma control. Curr Med Res Opin. 2007;23(2):369-377 [DOI] [PubMed] [Google Scholar]
- 37. Cabana MD, Rand CS, Becher OJ, Rubin HR. Reasons for pediatrician nonadherence to asthma guidelines. Arch Pediatr Adolesc Med. 2001;155(9):1057-1062 [DOI] [PubMed] [Google Scholar]
- 38. Cabana MD. A randomized trial of primary care provider prompting to enhance preventive asthma therapy. J Pediatr. 2005;147(5):708 [DOI] [PubMed] [Google Scholar]
- 39. Lemanske RF, Jr, Mauger DT, Sorkness CA, et al. Step-up therapy for children with uncontrolled asthma receiving inhaled corticosteroids. N Engl J Med. 2010;362(11):975-985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. US Department of Health and Human Services (DHS); US Food and Drug Administration FDA Drug Safety Communication: New Safety Requirements for Long-Acting Inhaled Asthma Medications Called Long-Acting Beta-Agonists (LABAs). Rockville, MD: MedWatch Online; Published February 18, 2010. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm200776.htm Accessed May 12, 2011 [Google Scholar]
- 41. Kamps AW, Brand PL, Roorda RJ. Determinants of correct inhalation technique in children attending a hospital-based asthma clinic. Acta Paediatr. 2002;91(2):159-163 [DOI] [PubMed] [Google Scholar]
- 42. Platts-Mills TA. The role of immunoglobulin E in allergy and asthma. Am J Respir Crit Care Med. 2001;164(8, pt 2):S1-S5 [DOI] [PubMed] [Google Scholar]
- 43. Arbes SJ, Jr, Gergen PJ, Vaughn B, Zeldin DC. Asthma cases attributable to atopy: results from the Third National Health and Nutrition Examination Survey. J Allergy Clin Immunol. 2007;120(5):1139-1145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Casale TB, Martin RJ. Clinical importance of identifying immunoglobulin E-mediated disease in patients with asthma. Clin Cornerstone. 2009;9(3):20-29 [DOI] [PubMed] [Google Scholar]
- 45. Morgan WJ, Crain EF, Gruchalla RS, et al. Results of a home-based environmental intervention among urban children with asthma. N Engl J Med. 2004;351(11):1068-1080 [DOI] [PubMed] [Google Scholar]
- 46. Nagata M, Nakagome K. Allergen immunotherapy in asthma: current status and future perspectives. Allergol Int. 2010;59(1):15-19 [DOI] [PubMed] [Google Scholar]
- 47. XOLAIR (omalizumab) [prescribing information]. South San Francisco, CA: Genentech, Inc. 2010. http://www.gene.com/gene/products/information/pdf/xolair-prescribing.pdf Accessed May 12, 2011 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.