Abstract
Background
The study examined concurrent illicit heroin use among methadone maintenance clients in China and its association with clients’ demographic characteristics, treatment experience, and personal social network.
Methods
Face-to-face surveys were conducted with 178 clients randomly recruited from six methadone maintenance treatment (MMT) clinics in Sichuan, China. Concurrent heroin use was measured based on self-report of heroin use during the past 30 days and a confirmatory urine morphine test. The participants’ demographic characteristics and treatment factors were measured and examined. The drug use status of their family members and friends was also assessed.
Results
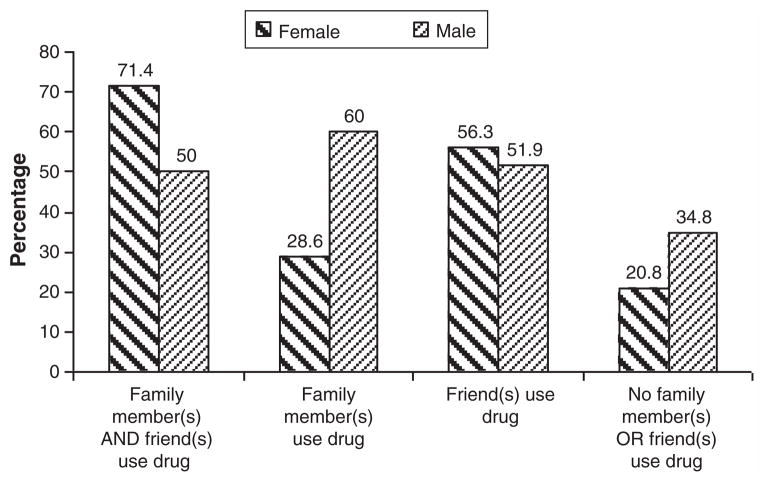
A total of 80 participants (44.9%) who either reported illicit heroin use in the past 30 days or had a positive urine test were defined as using heroin concurrently. Having drug-using friends was significantly associated with increased concurrent heroin use. Longer length of treatment (2 years or longer) was associated with increased concurrent heroin use. Among those who had both drug-using family members and friends, more women (71.4%) than men (50.0%) used heroin. For those who had no drug-using family members or friends, more men (34.8%) than women (20.8%) used heroin.
Discussion
Study findings indicate an urgent need to address concurrent illicit heroin use among MMT clients. Further examination of the influence of social networks on concurrent drug abuse behavior is encouraged. Results also highlight the importance of understanding gender differences in treatment seeking and behavioral changes, which is crucial to the development of gender-specific treatment strategies.
Keywords: Drug use, Methadone maintenance therapy, China
1. Introduction
At the end of 2009, it was estimated that 740,000 (560,000–920,000) people were living with HIV in China, and approximately one-third (32.2%) of these infections were attributable to risk behaviors associated with injecting drug use (Ministry of Health, People’s Republic of China, Joint United Nations Programme on HIV/AIDS, World Health Organization, 2010). According to recent national surveillance data, HIV infection prevalence among drug users is about 6%, which is the highest among all at-risk populations (Ministry of Health, People’s Republic of China, Joint United Nations Programme on HIV/AIDS, World Health Organization, 2010). Heroin remains the major illicit drug in China, with 72.5% of heroin users classified as injecting drug users (IDUs). The prevalence of syringe sharing among IDUs has been estimated at 40% (Xiao, Wu, Luo, & Wei, 2010). In addition to unsafe injecting practices, drug users in China also commonly engage in risky sexual practices that put their partners at a greater risk of HIV infection (Sullivan & Wu, 2007; Wu, Detels, & Zhang, 1996).
Methadone maintenance treatment (MMT) was first introduced to China in 2004 and initialized with eight clinics in five provinces with the highest IDU prevalence (Pang et al., 2007). Since then it has been expanded to a nationwide program encompassing more than 680 clinics serving 242,000 clients by the end of 2009 (Yin et al., 2010). MMT clients pay 10 yuan (U.S. $1.50) for their daily treatment and take methadone once a day under the supervision of a clinic staff. A urine test is required to be taken once a month on a random date. The clinics provide comprehensive services to clients, including psychological counseling, health education, and treatment referral (Lin, Wu, & Detels, 2011). The rapid scale-up of MMT programs has benefited tens of thousands of drug users with decreased drug use and criminality, increased quality of life, and higher rates of employment (Pang et al., 2007; Sullivan & Wu, 2007).
Despite considerable clinical promise, there are barriers facing current MMT programs in China. Previous studies have reported that many clients continue to engage in drug-using behaviors while undergoing treatment, which results in high drop-out rates from the programs (Lin et al., 2010; Liu et al., 2008; Tang & Hao, 2007). The problem of concurrent drug use among MMT clients is longstanding and widely acknowledged worldwide. In Australia, Mattick et al. (2003) found that over 50% of clients tested positive for opiates in urine samples. In the United States, it was reported that MMT clients tested positive for opiates in 53% to 62% of urine samples (Strain, Bigelow, Liebson, & Stitzer, 1999).
Several factors are associated with concurrent drug use among MMT clients. A higher dose of methadone was reported by most previous studies to be associated with less illicit opiate abuse and longer retention in treatment (Amato et al., 2005; Kamal et al., 2007; Strain et al., 1999). Appropriate psychological counseling and comprehensive services were also correlated with lower rates of drug use (Joe & Simpson, 2001; Lin et al., 2010). Ilgen, Jain, Kim, and Trafton (2008) found that MMT patients with high stress levels may be particularly vulnerable to heroin relapse. Drug users’ personal social circles, especially among sexual partners, were suggested to be associated with continued drug use and injecting behaviors, treatment retention, and higher rates of relapse (Tutten & Jones, 2003; Wasserman, Stewart, & Delucchi, 2001). Gender differences in concurrent heroin use have also been studied among MMT clients, but no statistical significance has been reported (Cao et al., 2010; Kamal et al., 2007).
Although studied in other countries, concurrent heroin use has not been fully investigated in MMT clinics in China given the short history of the program. This study aims to describe a pattern of concurrent heroin use and examine its correlates. We hypothesized that concurrent heroin use would be associated with a client’s demographic characteristics, drug use history, treatment experience, and his or her social network. Gender differences in concurrent heroin use were anticipated. The findings have implications for improving treatment outcomes of MMT programs.
2. Methods
2.1. Study setting and participants
This study was conducted in Sichuan province, China. Based on a 2009 epidemiological report, Sichuan was ranked number four among the provinces having the most drug users in China (Ministry of Health, People’s Republic of China, Joint United Nations Programme on HIV/AIDS, World Health Organization, 2010). Participants in this study were recruited in 2010 from six MMT clinics in Sichuan. Prospective participants were approached randomly by research staff in the waiting rooms of MMT clinics where they normally received services. After receiving a full disclosure of information and a complete description of the study, participants were included in the study after signing informed consent forms. The refusal rate was about 10%. In order to be eligible for the study, participants had to be at least 18 years old and currently receiving MMT at a participating clinic.
The participants were paid 45 yuan (U.S. $7.00) for the assessment. All study documents and procedures for this study were approved by the Institutional Review Board of the University of California, Los Angeles, and the Chinese Center for Disease Control and Prevention.
2.2. Data collection
Face-to-face surveys were conducted in private rooms in the participating clinics by well-trained interviewers. The survey took about 30 to 45 min to complete. Demographic information including gender, age, marital status, education, and income 30 days prior to the interview was collected. We measured three treatment-related factors, including length of treatment, current dosage, and perceived side-effects. The survey also assessed if a participant had any family members or friends who also used drugs. To measure concurrent heroin use in the clinic, the participants were asked how many days in the past 30 days they had used heroin. In addition, a urine specimen was collected and tested for morphine after the survey. A participant was considered as a concurrent heroin user if he or she gave a self-report of using heroin at least 1 day in the previous 30 days or had a positive urine morphine result.
2.3. Data analysis
SAS statistical software (Version 9.1.3) was used for data analysis. First, we compared the proportion of concurrent heroin use across demographic characteristics and treatment experiences. The proportion of heroin use was also compared between participants who had at least one drug-using family member (vs. no such family member) and participants who had at least one drug-using friend (vs. no such friend). P values were generated by using Chi-square test (for those independent variables with two levels) or ANOVA (for those independent variables with more than two levels).
Subsequently, the participants were divided into four groups according to the drug-using status of their family member(s) and/or friend(s). A participant could belong to one of the following four groups: 1) those who had both drug-using family member(s) and friend(s); 2) those who had only drug-using family member(s) but not friends; 3) those who had only drug-using friend(s) but not family members; and 4) those who had no drug-using family members or friends. Gender differences in proportion of concurrent heroin use were compared across the aforementioned four groups.
Finally, a logistic regression model was adopted to estimate the odds ratio of concurrent heroin use by considering the covariates simultaneously. Covariates including participant’s age, years of education completed, marital status (married or divorced; single), higher income (more than 500 yuan in the past 30 days), lower dose (less than 60 ml), side effect, longer treatment (more than 2 years), having at least one drug-using family member and having at least one drug-using friend were controlled in the model. The regression coefficients and their significant levels were recorded.
3. Results
Demographic characteristics, treatment factors, and the drug-using status of participants’ family members or friends are summarized in Table 1. Among the 178 participants, 117 (65.7%) were men. About one-third (N=59; 33.1%) of the participants were younger than 35; 41.6% (N=74) was between 36 and 40, and 25.3% (N=45) was older than 40. Approximately half of the participants (N=90; 50.6%) completed secondary school; 32.0% (N=57) finished high school or higher education, while another 17.4% (N=31) only attended elementary school. Slightly more than half (N=99; 55.6%) of the participants were married or living with a regular partner. The participants in this study reported an average income of 960 yuan (about U.S. $14.40) in the past month, which was much lower than the average monthly income of over 2500 yuan in Sichuan province (Sichuan News, 2011). More than half (N=98; 55.1%) of the participants earned less than 500 yuan (about U.S. $7.50) during the 30 days prior to the study. The average dosage received daily was 55.3 mg (range, 10–240 mg), with 104 (58.4%) participants reporting a methadone daily dose lower than 60 mg. Less than half (N=86; 48.3%) of the participants experienced at least one type of side-effect of methadone. About 42.9% (N=76) had been under methadone treatment for 2 years or longer. Forty (22.5%) participants had at least one drug-using family member and 86 (48.3%) had at least one drug-using friend.
Table 1.
Sample description and concurrent heroin use by demographic characteristics, treatment factors and drug-using status of a participant’s family member(s) and/or friend(s) (N=178).
| Count (%) | Concurrent heroin use
|
P value | |
|---|---|---|---|
| Count (%) | |||
| Gender | 0.6531 | ||
| Male | 117 (65.7) | 54 (46.2) | |
| Female | 61 (34.3) | 26 (42.6) | |
| Age | 0.8237 | ||
| 35 or younger | 59 (33.1) | 26 (44.1) | |
| 36–40 | 74 (41.6) | 32 (43.2) | |
| 41 or older | 45 (25.3) | 22 (48.9) | |
| Education | 0.6683 | ||
| Elementary or lower | 31 (17.4) | 12 (38.7) | |
| Secondary school | 90 (50.6) | 43 (47.8) | |
| High school or higher | 57 (32.0) | 25 (43.9) | |
| Marital status | 0.3385 | ||
| Single | 32 (18.0) | 11 (34.4) | |
| Married or have a regular partner | 99 (55.6) | 45 (45.5) | |
| Divorced, separated or widowed | 47 (26.4) | 24 (51.1) | |
| Income in past 30 days | 0.5537 | ||
| <500 yuan | 98 (55.1) | 46 (46.9) | |
| 500 yuan or more | 80 (44.9) | 34 (42.5) | |
| Current daily methadone dose | 0.3192 | ||
| <60 mg | 104 (58.4) | 50 (48.1) | |
| ≥60 mg | 74 (41.6) | 30 (40.5) | |
| Side effect | 0.4240 | ||
| Yes | 86 (48.3) | 36 (41.9) | |
| No | 92 (51.7) | 44 (47.8) | |
| Length of treatment | 0.0136 | ||
| <2 years | 101 (57.1) | 37 (36.6) | |
| 2 years or longer | 76 (42.9) | 42 (55.3) | |
| Family member(s) uses drug | 0.0698 | ||
| Yes | 40 (22.5) | 23 (57.5) | |
| No | 138 (77.5) | 57 (41.3) | |
| Friend(s) uses drug | 0.0048 | ||
| Yes | 86 (48.3) | 48 (55.8) | |
| No | 92 (51.7) | 32 (34.8) | |
| Total: 80 (44.9) |
Altogether, 80 (44.9%) participants reported concurrent illicit drug use or had a positive urine test, thus classifying them as concurrent heroin users in this study. Respectively, 33.0% (N=59) of participants self-reported illicit drug use at least once in the previous 30 days, and 33.0% (N=59) tested positive. The agreement level of these two measurements is moderate (Kappa=0.47). The proportion of participants who used heroin with methadone is also reported across the categories of each covariate in Table 1. In our univariate analysis, those who had less than 2 years of MMT were significantly more likely to concurrently use heroin than those who had stayed in treatment for more than 2 years (p=0.0136). Concurrent heroin use among participants who had at least one drug-using friend was significantly higher (p=0.0048) compared with those who had no drug-using friends. With the other covariates being controlled (Table 2), longer time in treatment (2 years or longer) was associated with higher odds of concurrent heroin use (OR=2.099; p=0.0264). The odds for participants who had drug-using friends to concurrently use heroin was 2.880 times higher than participants who had no friend using drugs (p=0.0019).
Table 2.
Logistic regressions on concurrent heroin use among MMT clients (N=178).
| Odds ratio | Confidence limits | P value | |
|---|---|---|---|
| Male | 0.567 | (0.270, 1.192) | 0.1343 |
| Age | 0.975 | (0.913, 1.040) | 0.4366 |
| Year of education | 0.987 | (0.870, 1.120) | 0.8379 |
| Married | 2.032 | (0.747, 5.529) | 0.1652 |
| Divorced | 2.811 | (0.925, 8.537) | 0.0683 |
| Income in past 30 days (>500 yuan) | 0.658 | (0.334, 1.296) | 0.2263 |
| Dose (<60 ml) | 1.666 | (0.848, 3.274) | 0.1383 |
| Side effect (yes) | 0.643 | (0.334, 1.238) | 0.1864 |
| Length of treatment (2 years or longer) | 2.099 | (1.096, 4.020) | 0.0264 |
| Family member(s) uses drug | 2.190 | (0.932, 5.141) | 0.0720 |
| Friend(s) uses drug | 2.880 | (1.475, 5.624) | 0.0019 |
Regarding gender differences (Fig. 1) among those who had both drug-using family members and friends, 71.4% (N=10) of women used heroin compared to 50% (N=2) of men. For those who had only drug-using family members but not friends, 28.6% (N=2) of the women used heroin compared to 60% (N=9) of men. For those who had only drug-using friends but not family members, 56.3% (N=9) of women and 51.9% (N=27) of men used heroin. Among those who had no family members or friends using drugs, more men (N=16; 34.8%) than women (N=5; 20.8%) used heroin. These differences were not statistically significant using Chi-square test or Fisher’s exact test.
Fig. 1.
Gender differences in concurrent heroin use. Probability of concurrent heroin use by drug-using status of a participant’s family member(s) and/or friend(s) across genders.
4. Discussion
Results of our study indicate that a considerable proportion (45%) of MMT clients in China was involved in ongoing illicit opiate misuse. This represents an enduring challenge for treatment services in China. Given the fact that concurrent illicit drug use has significant impacts on methadone adherence (Raffa et al., 2007) and can be attributed to poor treatment outcomes (Magura, Nwakeze, & Demsky, 1998; Rowan-Szal, Chatham, & Simpson, 2000; Sofuoglu, Gonzalez, Poling, & Kosten, 2003; Strain, Stitzer, Liebson, & Bigelow, 1998), this issue needs to be urgently addressed in order to expand the proven benefits of methadone treatment efficacy. Meanwhile, great caution is needed in developing and evaluating both pharmacological and psychosocial interventions for MMT clients who concurrently abuse illicit drugs.
Findings of our study confirm that maintenance clients with substance users in their social network increase the chance of concurrent heroin use (Costenbader, Astone, & Latkin, 2006; Gogineni, Stein, & Friedmann, 2001; Latkin et al., 1995). The role of social support systems in the treatment of substance abuse is by no means simple. Although some social support has a positive impact on treatment outcome in drug addicts (Wills, 1990), drug-using social network members may impede abstinence by making drugs more available. Moreover, these relationships may come to serve as “environmental cues” (e.g., locations, paraphernalia) that elicit craving and withdrawal (Goehl, Nunes, Quitkin, & Hilton, 1993). Identifying supportive others who are not substance users may be an important component of effective treatments. It has been suggested that interventions that aim to supplant drug-using friends with nondrug-using contacts may be most successful in achieving sustained behavioral risk reductions (Costenbader et al., 2006).
Previous research has documented that longer MMT retention produces optimal outcomes, including less heroin use (Gossop, Marsden, Stewart, & Treacy, 2001; Liu et al., 2008), lower mortality rates (Peles, Schreiber, & Adelson, 2010), and reduced criminal activity (Oliver et al., 2010). In contrast, we found in this study that longer treatment duration was positively associated with concurrent heroin use. As these data are associational, it is not possible to assign causation. This finding implies the importance of understanding and addressing the special needs of clients and making individualized treatment plans at different stages of MMT, which will help patient adherence to a long-term treatment program.
The study results revealed gender differences in patterns of concurrent drug use behaviors among MMT clients. When there was no one in a client’s personal network using drugs, men were more likely than women to continue using heroin during methadone treatment. This finding is supported by previous studies that men are usually the initiators of drug use (Tutten & Jones, 2003; Westermeyer & Boedicker, 2000). On the other hand, among those who had both family members and friends using drugs, more women than men concurrently used heroin, which may suggest that women are more passively influenced by peer relationships. As female drug users were more likely than male users to live with drug-using partners (Anglin, Hser, & McGlothlin, 1987), such gender differences can add to the complex challenge of attaining treatment success in women with substance abuse problems. It is recommended that future research should consider gender-related social factors and develop gender-specific treatment strategies in order to optimize treatment effectiveness.
Findings should be interpreted within the context of the study limitations. First, this study used a cross-sectional design that might suffer the limitation of temporal ambiguity; thus, we are not able to make definite causal inferences. Second, the results were based on self-reports that might be subject to inaccuracy, including recall bias and social-desirability bias. Third, the participants self-reported heroin use during the past 30 days, whereas the urine morphine test used in this study could only effectively detect heroin use in the past 7 days. The difference in time frame might be the reason for the moderate level of agreement between the two measures. Finally, the findings were obtained from one province. Drug-using patterns and economic situations may differ considerably in other parts of China.
The present study highlights the need for further examination of the influence of social networks on concurrent drug abuse behaviors for MMT clients. It is recommended that future interventions work with MMT clients to establish their supportive social network while avoiding the negative influence of drug-using contacts. It is also important to enhance sensitivity to gender differences in risk or protective factors that may trigger or reduce substance use among individuals receiving MMT.
Acknowledgments
Role of funding sources
This study was supported by the National Institute of Mental Health (NIMH) grant R34-MH083512. NIMH had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
We would like to thank project team members in Sichuan, Beijing, and Los Angeles for their contributions to this study.
Footnotes
Contributors
Dr. Li contributed to the conception and design of the study and led the study implementation and the writing of the article. Dr. Lin contributed to the writing of the article. Ms. Wan contributed to the summarization and interpretation of study results and data analysis. Dr. Zhang and Ms. Lai contributed to the data collection activities in China, and contributed to the interpretation of the study results.
Conflict of interest
All authors declare that they have no conflicts of interest.
References
- Amato L, Davoli MA, Perucci C, Ferri M, Faggiano FP, Mattick R. An overview of systematic reviews of the effectiveness of opiate maintenance therapies: Available evidence to inform clinical practice and research. Journal of Substance Abuse Treat. 2005;28:321–329. doi: 10.1016/j.jsat.2005.02.007. [DOI] [PubMed] [Google Scholar]
- Anglin MD, Hser YI, McGlothlin WH. Sex differences in addict careers II: Becoming addicted. American Journal of Drug and Alcohol Abuse. 1987;13:59–71. doi: 10.3109/00952998709001500. [DOI] [PubMed] [Google Scholar]
- Cao XB, Yin WY, Pang L, Zhang CB, Xu JS, Wu ZY. Risk factors which were associated with heroin use during the methadone maintenance treatment among 1301 patients in 9 cities of China. Zhonghua Liu Xing Bing Xue Za Zhi. 2010;31:269–272. [PubMed] [Google Scholar]
- Costenbader EC, Astone NM, Latkin CA. The dynamics of injection drug users’ personal networks and HIV risk behaviors. Addiction. 2006;101:1003–1013. doi: 10.1111/j.1360-0443.2006.01431.x. [DOI] [PubMed] [Google Scholar]
- Goehl L, Nunes E, Quitkin F, Hilton I. Social networks and methadone treatment outcome. The costs and benefits of social ties. American Journal of Drug and Alcohol Use. 1993;19:251–262. doi: 10.3109/00952999309001617. [DOI] [PubMed] [Google Scholar]
- Gogineni A, Stein MD, Friedmann PD. Social relationships and intravenous drug use among methadone maintenance patients. Drug and Alcohol Dependence. 2001;64:47–53. doi: 10.1016/s0376-8716(00)00230-1. [DOI] [PubMed] [Google Scholar]
- Gossop M, Marsden J, Stewart D, Treacy S. Outcomes after methadone maintenance and methadone reduction treatments: Two-year follow-up results from the National Treatment Outcome Research Study. Drug Alcohol Dependence. 2001;62:255–264. doi: 10.1016/s0376-8716(00)00211-8. [DOI] [PubMed] [Google Scholar]
- Ilgen M, Jain A, Kim H, Trafton J. The effect of stress on craving for methadone depends on the timing of last methadone dose. Behaviour Ressear and Therapy. 2008;46:1170–1175. doi: 10.1016/j.brat.2008.05.013. [DOI] [PubMed] [Google Scholar]
- Joe GW, Simpson DD. Relationships between counseling rapport and drug abuse treatment outcomes. Psychiatric Services. 2001;52:1223–1229. doi: 10.1176/appi.ps.52.9.1223. [DOI] [PubMed] [Google Scholar]
- Kamal F, Flavin S, Campbell F, Behan C, Fagan J, Smyth R. Factors affecting the outcome of methadone maintenance treatment in opiate dependence. Irish Journal of Medicine. 2007;100:393–397. [PubMed] [Google Scholar]
- Latkin CA, Mandell W, Oziemkowska M, Celentano D, Vlahov D, Ensminger M, et al. Using social network analysis to study patterns of drug use among urban drug users at high risk for HIV/AIDS. Drug and Alcohol Dependence. 1995;38:1–9. doi: 10.1016/0376-8716(94)01082-v. [DOI] [PubMed] [Google Scholar]
- Lin C, Wu Z, Detels R. Drug users’ perceived barriers against attending methadone maintenance therapy: A qualitative study in China. Substance Use and Misuse. 2011;46:1190–1198. doi: 10.3109/10826084.2011.561905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin C, Wu Z, Rou K, Yin W, Wang C, Shoptaw S, et al. Structural-level factors affecting implementation of the methadone maintenance therapy program in China. Journal of Substance Abuse Treatment. 2010;38:119–127. doi: 10.1016/j.jsat.2009.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu EW, Wu ZY, Liang T, Shen LM, Zhong H, Wang B, et al. Risk factors associated with continued heroin use during methadone maintenance treatment in Guizhou province, China. Zhonghua Yu Fang Yi Xue Za Zhi. 2008;42:875–878. [PubMed] [Google Scholar]
- Magura S, Nwakeze PC, Demsky S. Pre- and in-treatment predictors of retention in methadone treatment using survival analysis. Addiction. 1998;93:51–60. doi: 10.1046/j.1360-0443.1998.931516.x. [DOI] [PubMed] [Google Scholar]
- Mattick RP, Ali R, White JM, O’Brien S, Wolk S, Danz C. Buprenorphine versus methadone maintenance therapy: A randomized double blind trial with 405 opioid-dependent patients. Addiction. 2003;98:441–452. doi: 10.1046/j.1360-0443.2003.00335.x. [DOI] [PubMed] [Google Scholar]
- Ministry of Health, People’s Republic of China, Joint United Nations Programme on HIV/AIDS, World Health Organization. 2009 estimates for the HIV/AIDS epidemic in China. 2010 Retrieved from www.unaids.org.cn/download/2009%20China%20Estimation%20Report-En.pdf.
- Oliver P, Keen J, Rowse G, Ewins E, Griffiths L, Mathers N. The effect of time spent in treatment and dropout status on rates of convictions, cautions and imprisonment over 5 years in a primary care-led methadone maintenance service. Addiction. 2010;105:732–739. doi: 10.1111/j.1360-0443.2009.02856.x. [DOI] [PubMed] [Google Scholar]
- Pang L, Hao Y, Mi G, Wang C, Luo W, Rou K, et al. Effectiveness of first eight methadone maintenance treatment clinics in China. AIDS. 2007;21:s103–s107. doi: 10.1097/01.aids.0000304704.71917.64. [DOI] [PubMed] [Google Scholar]
- Peles E, Schreiber S, Adelson M. 15-year survival and retention of patients in a general hospital-affiliated methadone maintenance treatment (MMT) center in Israel. Drug and Alcohol Dependence. 2010;107:141–148. doi: 10.1016/j.drugalcdep.2009.09.013. [DOI] [PubMed] [Google Scholar]
- Raffa JD, Grebely J, Tossonian H, Wong T, Viljoen M, Khara M, et al. The impact of ongoing illicit drug use on methadone adherence in illicit drug users receiving treatment for HIV in a directly observed therapy program. Drug and Alcohol Dependence. 2007;10(89):306–309. doi: 10.1016/j.drugalcdep.2007.02.007. [DOI] [PubMed] [Google Scholar]
- Rowan-Szal GA, Chatham LR, Simpson DD. Importance of identifying cocaine and alcohol dependent methadone clients. The American Journal on Addictions. 2000;9:38–50. doi: 10.1080/10550490050172218. [DOI] [PubMed] [Google Scholar]
- Sichuan News. Average wage in 2010 increased to 33,112 yuan in Sichuan Province. 2011 Retrieved from http://scnews.newssc.org/system/2011/06/16/013202576.shtml.
- Sofuoglu M, Gonzalez G, Poling J, Kosten TR. Prediction of treatment outcome by baseline urine cocaine results and self-reported cocaine use for cocaine and opioid dependence. American Journal of Drug and Alcohol Abuse. 2003;29:713–727. doi: 10.1081/ada-120026256. [DOI] [PubMed] [Google Scholar]
- Strain EC, Bigelow GE, Liebson IA, Stitzer ML. Moderate vs. high dose methadone in treatment of opiate dependence. The Journal of American Medical Association. 1999;281:1000–1005. doi: 10.1001/jama.281.11.1000. [DOI] [PubMed] [Google Scholar]
- Strain EC, Stitzer ML, Liebson IA, Bigelow GE. Useful predictors of outcome in methadone-treated patients: Results from a controlled clinical trial with three doses of methadone. Journal of Maintenance in the Addictions. 1998;1:15–28. [Google Scholar]
- Sullivan GS, Wu Z. Rapid scale up of harm reduction in China. International Journal of Drug Policy. 2007;18:118–128. doi: 10.1016/j.drugpo.2006.11.014. [DOI] [PubMed] [Google Scholar]
- Tang YL, Hao W. Improving drug addiction treatment in China. Addiction. 2007;102:1057–1063. doi: 10.1111/j.1360-0443.2007.01849.x. [DOI] [PubMed] [Google Scholar]
- Tutten M, Jones HE. A partner’s drug-using status impacts women’s drug treatment outcome. Drug and Alcohol Dependence. 2003;70:327–330. doi: 10.1016/s0376-8716(03)00030-9. [DOI] [PubMed] [Google Scholar]
- Wasserman DA, Stewart AL, Delucchi KL. Social support and abstinence from opiates and cocaine during opioid maintenance treatment. Drug and Alcohol Dependence. 2001;65:65–75. doi: 10.1016/s0376-8716(01)00151-x. [DOI] [PubMed] [Google Scholar]
- Westermeyer J, Boedicker AE. Course, severity, and treatment of substance abuse among women versus men. American Journal of Drug and Alcohol Abuse. 2000;26:523–535. doi: 10.1081/ada-100101893. [DOI] [PubMed] [Google Scholar]
- Wills TA. Multiple networks and substance use. Special Issue: Social support in social and clinical psychology. Journal of Social and Clinical Psychology. 1990;9:78–90. [Google Scholar]
- Wu Z, Detels R, Zhang JP. Risk factors for intravenous drug use and sharing equipment among young male drug users in southwest China. AIDS. 1996;10:1017–1024. doi: 10.1097/00002030-199610090-00013. [DOI] [PubMed] [Google Scholar]
- Xiao L, Wu Z, Luo W, Wei X. Quality of life of outpatients in methadone maintenance treatment clinics. Journal of Acquired Immune Deficiency Syndrome. 2010;53:s116–s120. doi: 10.1097/QAI.0b013e3181c7dfb5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin W, Hao Y, Sun X, Gong X, Li F, Li J, et al. Scaling up the national methadone maintenance treatment program in China: Achievements and challenges. International Journal of Epidemiology. 2010;39:29–37. doi: 10.1093/ije/dyq210. [DOI] [PMC free article] [PubMed] [Google Scholar]