Abstract
The aim of this study is to examine the longitudinal relationship of readiness to change, drinking pattern, amount of alcohol consumed, and alcohol-related negative consequences among at-risk and dependent drinkers enrolled in a Screening, Brief Intervention and Referral to Treatment (SBIRT) trial in an emergency department in southern Poland. The study examined 299 patients randomized to either an assessment or intervention condition and followed at 3 and 12 months after initial presentation. Patients indicating a readiness or were unsure of changing drinking behavior were significantly more likely to decrease the maximum number of drinks per occasion and the usual number of drinks in a sitting in the 3-months following study entry when compared to those that rated changing drinking behavior as unimportant. Readiness to change was not predictive of outcomes between the baseline and 12-month follow-up. Drinking outcomes and negative consequences by readiness and research condition were non-significant. This is the first Polish study utilizing SBIRT to enable patients to identify their hazardous drinking and reduce alcohol consumption. While some drinking outcomes improved with motivation, these improvements were not maintained at 12-months following SBIRT. Attention to additional constructs of readiness to change and drinking patterns may augment the effectiveness of SBIRT.
Introduction
The international burden of hazardous and heavy alcohol consumption is related to many health (Cherpitel, Borges, et al., 2009; Greenfield, 2001) and societal problems (Room, Graham, Rehm, Jernigan, & Monteiro, 2003). European countries currently have one of the highest adult per capita alcohol consumption rates in the developed world (Rehm, et al., 2003; Room, et al., 2003), leaving a strong need to identify and assist persons most in need of intervention and treatment. Most problem or dependent drinkers do not seek out formal treatment (Kaskutas, Weisner, & Caetano, 1997; Tucker, 2001) even though elevated levels of drinking can continue for years (Delucchi & Kaskutas, 2010) which leaves a challenging dilemma for clinicians in discriminating which drinkers are most in need of, and responsive to, assistance to reduce drinking. There is substantial evidence that patients presenting to emergency departments for an injury are more likely to be more frequent, heavy, and problem drinkers when compared to the general population (Borges, Cherpitel, Medina-Mora, Mondragon, & Casavuevas, 1998; Cherpitel, 1995; Saitz, 2005), providing for a logical setting for alcohol intervention to take place.
Brief Interventions conducted in the medical settings are designed to provide at-risk and dependent patients with sufficient motivation to change drinking behavior and offer referral to appropriate services to assist them. Systematic and meta-analytic reviews of brief interventions in health care settings have generally found them to be efficacious at decreasing drinking (Ballesteros, Duffy, Querejeta, Arino, & Gonzalez-Pinto, 2004; D’Onofrio & Degutis, 2002; Kaner, 2010) although not all studies have found favorable drinking outcomes for all populations (Field, Baird, Saitz, Caetano, & Monti, 2010; Grothues, et al., 2008). The conflicting evidence of the efficacy of brief interventions in health care settings calls for a greater understanding of the components that promote drinking reductions. This would allow the process to be streamlined by applying the elements that are most helpful to the patient and eliminating those that offer little or no assistance. To date, there is insufficient literature on the mechanisms that provide the greatest change for therapeutic interventions (Nock, 2007).
One important component of the brief intervention, believed to be a catalyst for changing drinking behavior, is the motivation, or readiness to change behavior which has been conceptualized in the Transtheoretical Model (Prochaska & DiClemente, 1986, 1992). This model incorporates stages of change to describe intentional behavior modification to either reinforce a desired behavior or eradicate an undesired one. Though there are five major stages of change (precontemplation, contemplation, preparation, action and maintenance), the process of changing behavior is not identified by discrete, singular events but viewed as a continuing process. Brief interventions designed to decrease alcohol consumption typically target at-risk patients that are in the earlier stages of change (precontemplation, contemplation or preparation) with the central goal of guiding the patient toward gaining sufficient motivation and increasing readiness, which will act as a mechanism to decrease risky drinking behavior (Rollnick, Heather, Gold, & Hall, 1992).
The role of the patient’s motivation to change drinking behavior after administration of a brief intervention is not very clear. While studies have shown an increase in motivation after a brief intervention (Kunz, French, & Bazargan-Hejazi, 2004; Reed, et al., 2005; Stein, et al., 2009), this increase has not always equated to improved drinking outcomes (Stein, et al., 2009; Walton, et al., 2008; Williams, Horton, Samet, & Saitz, 2007) although some evidence of decreased drinking has been found (Maisto, et al., 2001).
Brief interventions not only seek to motivate the patient to decrease alcohol consumption but also to motivate the patient to make the connection between drinking and the physical or social problems (e.g., blackouts, driving while intoxicated) that may be co-occurring. The central goal of the intervention is to decrease both of these behaviors. Similar to the research on the relationship between motivation and drinking, there is not strong evidence that higher motivation results in lowering the number of negative consequences and some studies have even shown an increase in the number of adverse consequences of drinking after receipt of a brief intervention (Walton, et al., 2008; Williams, et al., 2007). However, Stein et al. (Stein, et al., 2009) found primary care patients reported greater readiness to change and lowered negative consequences at follow-up, although this relationship was mitigated by persons who were most highly motivated to change, regardless of the intervention condition.
The present study seeks to understand readiness to change as a mechanism for behavior change among patients presenting at a Polish emergency department. Reported here is a secondary data analysis of a randomized clinical trial of Screening, Brief Intervention and Referral to Treatment (SBIRT) among at-risk and alcohol dependent patients in southern Poland (Cherpitel, Bernstein, Bernstein, Moskalewicz, & Swiatkiewicz, 2009; Cherpitel, et al., 2010; Cherpitel, Moskalewicz, Swiatkiewicz, Ye, & Bond, 2009). Twelve-month findings from the randomized clinical trial demonstrated brief intervention to help Polish patients improve on several drinking measures, especially the number of drinking days per week and the maximum number of drinks on an occasion. Because this is the first study to utilize brief intervention in an emergency department setting in a Central European country where infrequent but heavy drinking is typical, the present paper seeks to identify if motivation, is associated with drinking outcomes, taking into account the intervention condition in this population.. This work will enhance our understanding of the role of readiness to change and subsequent drinking behaviors within the context of a brief motivational intervention for this European population of at-risk and dependent drinkers, and may inform other populations characterized by similar drinking patterns.
Method
Study design
A sample of adult patients presenting to the emergency department in Sosnowiec, Poland were assessed between 4:00 pm and 12:00 midnight seven days a week over a 23-week period (May – November 2007) for unhealthy alcohol use. Patients screened eligible for the study if replying ‘yes’ to any one of the four items on the Rapid Alcohol Problems Screen (see measures below) during the last year, or reported 11 or more drinks per week for males (6 or more for females), or 4 or more drinks on an occasion for males (3 or more for females) (see Alcohol measures below), applying a somewhat lower standard of screening criteria than the NIAAA guidelines of 15 or more standard drinks per week for males (8 or more for females) or 5 or more standard drinks on an occasion for males (4 or more for females), to better capture risky drinkers in this population. Patients who provided informed consent to participate in the study were randomized using a two-stage process: first they were randomized to screen only or an assessment condition. Only patients that were randomized to the assessment condition are analyzed here because baseline and 3-month readiness to change data were not collected for the screened only group, resulting in a total sample of n=299 patients. After an assessment interview was completed, patients were randomly selected to the intervention condition. A total of 152 of the 299 assessment patients received the intervention which consisted of a 10–15 minute SBIRT session (described below). A detailed description and graphic depiction of study recruitment, randomization, attrition and study methods is described elsewhere (Cherpitel, et al., 2010; Cherpitel, Moskalewicz, et al., 2009).
Measures
Rapid Alcohol Problems Screen (RAPS4)
A RAPS4 is a 4-item measure identifying alcohol dependence. Patients were asked about past year and past three months dependence at the baseline interview and past 3 months at follow-up interviews. Items include a feeling of guilt or remorse after drinking, not remembering things you said or did while drinking, failing to do what was normally expected of you, and taking a drink first thing in the morning. This measure has shown a high degree of sensitivity (93%) and specificity (84%) when examined against ICD-10 and DSM-IV diagnostic criteria for alcohol dependence (Cherpitel, 2000; Cherpitel, et al., 2005)
Readiness to change(RTC)
Instruments used to test readiness in brief intervention settings have generally been concise and easy to administer, thus accommodating the time constraints of busy medical facilities and allowing assessment of a wide range of patients with varying levels of comprehension. The Readiness Ruler, which is a linearization of Prochaska and DiClemente’s stages of change model (Prochaska & DiClemente, 1992), was developed and validated by Rollnick for use in general medical settings (Heather, Smailes, & Cassidy, 2008; Hesse, 2006; Rollnick, et al., 1992). After receipt of assessment, patients were asked to rate their readiness to change their current drinking behavior using a simple ruler graphic on a scale of 1 to 10. A self-reported score of 1 to 3 on the readiness ruler indicates “not ready”, 4–7 indicates “unsure” and 8–10 is indicative of “ready”. These categories correspond loosely to Prochaska and DiClemente’s precontemplation, contemplation and preparation stages of change (Prochaska & DiClemente, 1986)
Negative consequences
The 21-item Short Inventory of Problems (Miller, Tonigan, & Longabaugh, 1995) is a brief version of the 45-item Drinking Inventory of Consequences developed by project MATCH, which includes consequences related to physical, social responsibility, intrapersonal, impulse control and interpersonal domains, and retains six questions having to do with injury and drinking and driving.
Alcohol measures
The Timeline Follow-Back (Sobell & Sobell, 1992) assessed quantity and frequency of drinking over the last 30 days, the average number of drinks per drinking day and the maximum number of drinks on an occasion. The usual quantity of drinks in a sitting (“On a typical day when you drank, how many standard drinks did you have?”) and the average number of days drinking in a typical week (“On average, how many days per week do you drink alcohol?”) asked past 12 months drinking at baseline and past 3 months at subsequent interviews,
Polish Translation
All instruments had previously undergone translation in Polish, verified by attestation by an expert experienced in cross-cultural investigations from the Polish Institute of Psychiatry and Neurology, and used in other clinical populations in Poland. Interviewers were trained by the authors and supervised by survey research staff from the institute to carry out screening, recruitment, randomization, assessment and follow-up procedures (Cherpitel, Bernstein, et al., 2009).
Intervention
Nurses regularly working in the department were trained in SBIRT, using Brief Negotiation Interviewing which takes about 15–20 minutes to complete, and is a patient-centered intervention utilizing readiness to change (Prochaska & DiClemente, 1992) and elements of motivational interviewing (Miller & Rollnick, 2002). The intervention places emphasis on respectful listening, open-ended questions, and exploration of the pros and cons of alcohol use to help bring about positive behavior change. The session guides the patient to make arguments and find reasons for changing drinking behavior and concludes with the clinician and patient developing a plan for action.
Summary of Analyses
Data were analyzed using SPSS version 17 (SPSS Inc., 2009) and Stata version 10 (Stata Corp., 2005). Chi square and ANOVA statistics were calculated to test for differences in baseline demographic (age, gender, at-risk drinking, and RAPS4) and predictor variables (average number of drinks per day, number of drinking days in a week, maximum number of drinks on an occasion, usual quantity in a sitting, and the number of alcohol-related negative consequences) between the RTC groups. Longitudinal analyses were carried out using random effects regression in Stata to estimate differential change in the outcome measures from baseline to the 3 month follow-up, 3 to 12 month follow-up, and baseline to 12 month follow-up. Models with multiple linear comparisons (Figures 1 and 2 and Tables 3a and 3b) were restricted to a significance level of p≤ 0.01 to avoid type I error. All other comparisons were considered statistically significant at the p≤ .05 level. Outcome measures for the multivariate models were logged to minimize the distribution, which skewed toward zero for all measures.
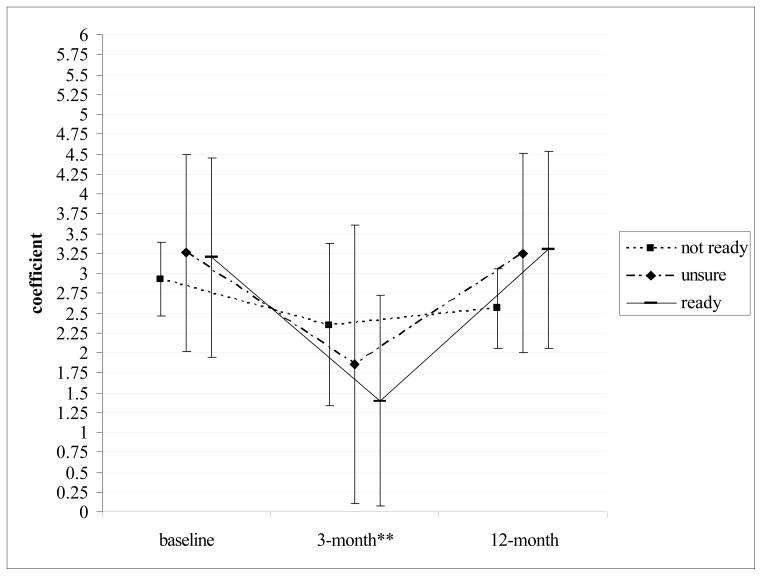
Figure 1.
Random effects regression coefficients and 95% confidence intervals for the logged maximum number of drinks on an occasiona.
a model controls for age and gender.
**p≤.01 differences between ‘ready’ and ‘not ready’ from baseline to 3-month outcome.
**p≤.01 differences between ‘unsure’ and ‘not ready’ from baseline to 3-month outcome.
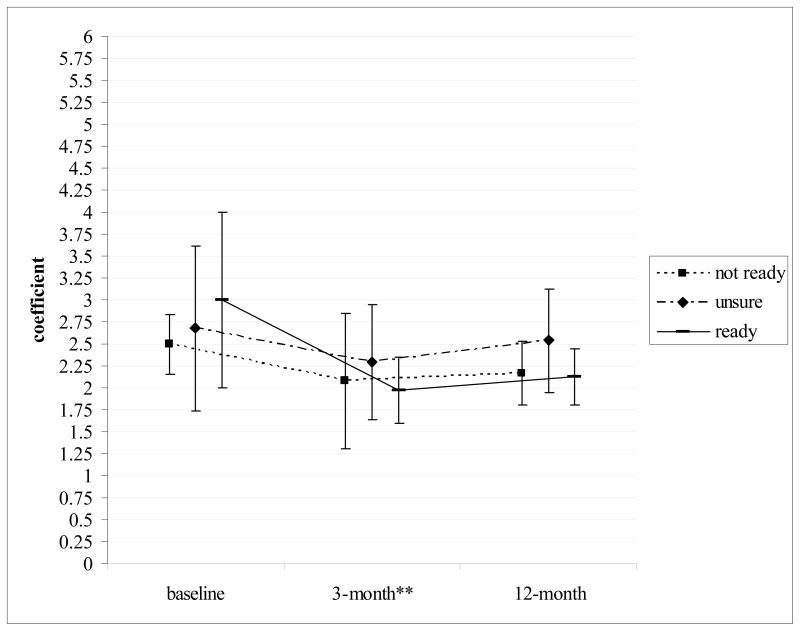
Figure 2.
Random effects regression coefficients and 95% confidence intervals for the logged usual quantity of drinks in a sittinga.
a model controls for age and gender.
** p≤.01 differences between ‘ready’ and ‘not ready’ from baseline to 3-month outcome.
** p≤.01 differences between ‘unsure’ and ‘not ready’ from baseline to 3-month outcome.
Table 3a.
Random effects regression coefficients comparing baseline and 3-month differences between intervention and assessment conditions by readiness to change a.
| change between Ready and Unsure | change between Ready and Not Ready | change between Not Ready and Unsure | ||||
|---|---|---|---|---|---|---|
| β | 95% CI | β | 95% CI | β | 95% CI | |
| Average # of drinks per drinking day | 0.89 | −0.13, 1.89 | 0.26 | −0.61, 1.12 | 0.63 | −0.19, 1.44 |
| # days drink per week | 0.63 | −0.38, 1.63 | 0.40 | −0.47, 1.26 | 0.23 | −0.59, 1.05 |
| Maximum # of drinks per occasion | 1.02 | −0.13, 2.18 | 0.89 | −0.11, 1.88 | 0.14 | −0.81, 1.08 |
| Usual Quantity | 1.08 | 0.23, 1.92 | 0.68 | −0.05, 1.41 | 0.40 | −0.29, 1.09 |
| # of negative consequences | 0.65 | −0.34, 1.64 | 0.54 | −0.32, 1.39 | 0.12 | −0.69, 0.92 |
models control for age and gender
Note: all linear comparisons are non-significant at the p≤.01 level of significance.
Table 3b.
Random effects regression coefficients comparing baseline and 12-month differences between intervention and assessment conditions by readiness to change.a
| change between Ready and Unsure | change between Ready and Not Ready | change between Not Ready and Unsure | ||||
|---|---|---|---|---|---|---|
| β | 95% CI | β | 95% CI | β | 95% CI | |
| Average # of drinks per drinking day | 0.88 | −0.21, 1.97 | 0.31 | −0.64, 1.25 | 0.57 | −0.31, 1.45 |
| # days drink per week | 0.27 | −0.83, 1.37 | −0.08 | −1.03, 0.87 | 0.35 | −0.54, 1.23 |
| Maximum # of drinks per occasion | 1.04 | −0.22, 2.31 | 0.56 | −0.53, 1.65 | 0.48 | −0.53, 1.50 |
| Usual Quantity | 1.05 | 0.13, 1.98 | 0.64 | −0.16, 1.43 | 0.42 | −0.33, 1.16 |
| # of negative consequences | 0.94 | −0.14, 2.01 | 0.45 | −0.48, 1.38 | 0.49 | −0.38, 1.36 |
model controls for age and gender.
Note: all linear comparisons are non-significant at the p≤.01 level of significance.
Results
Using the readiness ruler, the desire to change drinking behavior in this sample of 299 patients showed the majority of patients (54%; n=162) expressed no desire or importance to change (“not ready”), 24% (n=72) were unsure if they would like to change and 22% (n=65) indicated a high desire to change their drinking habits (“ready”) at the baseline interview (Table 1). The three RTC groups were similar on gender and age, with a predominance of men and those under the age of 30. Past year risky drinking behavior was also similar across groups, but the percent reporting alcohol dependence, (i.e., a positive response to any of the RAPS4 items) was significantly lower for those not ready to change (27%) than for those who were unsure (58%) or ready (57%) to change.
Table 1.
Demographic characteristics by readiness to change (N=299).
| Not ready (n=162) | Unsure (n=72) | Ready (n=65) | |
|---|---|---|---|
| % | % | % | |
| Male | 86 | 90 | 79 |
| <30 | 56 | 50 | 60 |
| 1+ RAPS | 27 | 58 | 57* |
| Risky Drinking | 88 | 92 | 88 |
p ≤ .05 between group comparisons
Table 2 displays baseline means and standard deviations for outcome measures by RTC group. Cross-sectional ANOVAs, to determine differences between the RTC groups were performed for each outcome measure. The average number of drinks per drinking day and the average number of drinking days per week showed no significant differences between the groups at any time point. However, the maximum number of drinks on an occasion, usual quantity of drinks in a sitting, and number of negative consequences for the ready and unsure groups were significantly higher than for the not ready group.
Table 2.
Baseline drinking measures and negative consequences by readiness to change group.
| Baseline N=299 |
|||
|---|---|---|---|
|
Not ready n=162 |
Unsure n=72 |
Ready n=65 |
|
| x̄ (sd) | x̄ (sd) | x̄ (sd) | |
| average # of drinks per drinking day | 1.7 (2.9) | 2.0 (2.4) | 2.7 (4.8) |
| # days drink per week | 2.6 (2.3) | 2.9 (2.2) | 2.8 (2.3) |
| Maximum # of drinks per occasion | 8.4 (6.7) | 12.0 (9.2) | 11.3 (11.1)* |
| Usual Quantity | 5.1 (3.4) | 7.8 (12.4) | 7.7 (6.9)* |
| # of negative consequences | 0.9 (2.0) | 3.4 (3.8) | 4.1 (4.5)* |
Post-hoc comparison:
p<.05 unsure, ready > not ready
To determine if the RTC groups differed over the course of the study, multivariate random effects models were performed for each of the five drinking outcome measures. Though all of the RTC groups showed declines in drinking, especially between the baseline and 3-month interviews, only the maximum number of drinks on an occasion and the usual quantity of drinks in a sitting showed significant differences between RTC groups (Figures 1 and 2). The average number of drinks per day, the number of drinking days per week, and the number of alcohol-related negative consequences were not statistically significant (results not shown). Figures 1 and 2 depict logged outcomes and control for age and gender with mean coefficients and 95% confidence intervals graphed, for each RTC group at each time point. Group comparison tests were performed to assess the difference in means between group pairs (i.e., not ready vs. ready, ready vs. unsure, unsure vs. not ready) for the periods between the baseline and 3-month, 3-month and 12-month, and the baseline and 12-month outcomes, accounting for nine linear comparisons per outcome measure. Because each outcome measure employed multiple comparisons, a p<0.01 significance level was applied to minimize Type I error. Figure 1 depicts the decline in the maximum number of drinks from the baseline to the 3-month follow-up for the ready (β=3.20 at baseline and 1.40 at 3-month) and unsure (β=3.26 at baseline and 1.86 at 3-month) groups were significantly greater than those that were not ready (β=2.93 at baseline, 2.35 at 3-month) group (p≤ .01 for both comparisons). The ready and unsure groups also significantly decreased the usual quantity of drinks in a sitting (Figure 2; β=2.68 and 3.00 at baseline and β=2.29 and 1.97 at 3 month for unsure and ready, respectively) when compared to those not ready (β=2.50 at baseline, 2.08 at 3-months) to change drinking behavior.
To understand the efficaciousness of SBIRT in relation to RTC, Table 3a and 3b display multivariate random effects regression outcomes that examine a 3-way interaction of readiness, treatment condition, and time of interview. All drinking outcomes control for age and gender, with high RTC drinking behavior (‘ready’) and assigned to the intervention condition as the reference categories. No outcome differences were evident at the p≤ .01 level of significance for either the 3 month or 12 month outcomes.
Discussion
Many SBIRT studies conducted in the emergency department have proven effective in reducing alcohol consumption (Ballesteros, et al., 2004; D’Onofrio & Degutis, 2002), however, only a limited number of studies have identified mechanisms that may help to focus and target the intervention based upon individual characteristics. Prior study of this population has shown promise that SBIRT is an effective tool to help patients decrease drinking and its associated problems in a Polish emergency department setting (Cherpitel, et al., 2010; Cherpitel, Moskalewicz, et al., 2009), however, the association of RTC and subsequent drinking behavior for this population is only modest (Figures 1 and 2). Patients who were unsure of their eagerness to change and those that were ready to change significantly lowered the maximum number of drinks on an occasion and usual number of drinks in a sitting compared to the not-ready group. Significant changes between RTC groups by the 12-month follow-up were not evident for any of the drinking outcomes
Based upon the Transtheoretical Model, it would be expected that patients experiencing more problems, or negative consequences, related to alcohol consumption would also have a higher motivation to change drinking behavior to decrease alcohol-related consequences. In fact, RTC and the number of negative consequences were significantly correlated at the baseline interview (r=.42, p<.001) but higher RTC did not result in a substantial decrease in the number of negative consequences compared to those that were unsure or unready to change. Possibly the negative consequences of those most ready to change have grown to become habitual and, even though there is acknowledgement that drinking habits should change (i.e., reporting higher motivation to change), the consequences that have been acquired are not easily changed during the relatively short period of time the study assessed these changes. It could also be speculated that patients view some of the activities, deemed as bad or negative by researchers, as beneficial. Impulsive acts, such as physical fighting while drinking, may be something enjoyed and not viewed as particularly harmful so there is little intention of changing these behaviors.
Similar to other brief intervention studies conducted in medical settings (Stein, et al., 2009; Williams, et al., 2007), we did not see a significant difference between SBIRT condition and RTC. In fact, all groups showed improvement on every outcome measure at the 3 month follow-up. It is possible that the traumatic event of arriving to the emergency department may have acted as the catalyst to change drinking behavior. The stress of admission may ‘prime’ all patients to reflect on their overall health and the reasons for arrival, giving rise to increased motivation to change risky behaviors. This alone may act as the significant wake-up call to decrease alcohol consumption Perhaps this is why we see some differences between the readiness groups (but not SBIRT by readiness groups) at the 3-month interview, when the hospital visit and the assessment are somewhat freshly recalled. However, this was not maintained by the one year follow-up, indicating that possibly a “booster” session with a trained SBIRT interviewer between the 3- and 12-month interviews, would allow patients to recall their hospital visit and reassess their motivation to change drinking habits.
Nonetheless, the stress and reflection on the consequences of drinking presents an ideal opportunity for clinicians to address risky and binge drinking behavior with the patient. Indeed, the receptiveness to the assessment or intervention was positive with a subsample of patients (n=145) who were asked upon discharge if they found it helpful. Nearly 98% expressed satisfaction, demonstrating receptiveness to change.
This study demonstrates strength by having follow-up interviews up to one year post-admission, but findings should be taken with consideration of the study limitations. Evaluation of RTC pertained only to the conditions of assessment and intervention; a control condition could not be used for the present paper due to a lack of assessment for readiness at the baseline interview. Identifying the mechanisms of change to tailor the brief intervention process would be most helpful using a variety of measures designed to identify motivation. Using additional measures in conjunction with motivation measures could help identify which patients are most likely to be responsive to a brief intervention would also be advantageous for future studies. Measures of self-efficacy, perception of problems, and intention to drink have been associated with a reduction of drinking in emergency department and primary care settings (Bertholet, Cheng, Palfai, Samet, & Saitz, 2009; Daeppen, Bertholet, Gmel, & Gaume, 2007; Williams, et al., 2007) and may serve useful to tailor the brief intervention to the needs of the individual.
This is the first study examining RTC and SBIRT for at-risk drinkers presenting at an emergency department in Poland. Additional attention to the constructs of RTC in relation to drinking patterns may help to augment the effectiveness of SBIRT.
Acknowledgments
This study was funded by a grant from the National Institute on Alcohol Abuse and Alcoholism (NIAAA, R21 AA016081-01). NIAAA had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript. or the decision to submit the paper for publication.
Contributor Information
Rachael A. Korcha, Email: rkorcha@arg.org, Alcohol Research Group, 6475 Christie Avenue, Suite 400, Emeryville, CA, USA, 510-597-3440, Fax: 510-985-6459.
Cheryl J. Cherpitel, Alcohol Research Group, 6475 Christie Avenue, Suite 400, Emeryville, CA, USA.
Jacek Moskalewicz, Institute of Psychiatry and Neurology, Sobieskiego 9, 02-957 Warsaw, POLAND.
Grazyna Swiatkiewicz, Institute of Psychiatry and Neurology, Sobieskiego 9, 02-957 Warsaw, POLAND.
Jason Bond, Alcohol Research Group, 6475 Christie Avenue, Suite 400, Emeryville, CA, USA.
Yu Ye, Alcohol Research Group, 6475 Christie Avenue, Suite 400, Emeryville, CA, USA.
References
- Ballesteros J, Duffy JC, Querejeta I, Arino J, Gonzalez-Pinto A. Efficacy of brief interventions for hazardous drinkers in primary care: systematic review and meta-analyses. Alcoholism: Clinical and Experimental Research. 2004;28:608–618. doi: 10.1097/01.alc.0000122106.84718.67. [DOI] [PubMed] [Google Scholar]
- Bertholet N, Cheng DM, Palfai TP, Samet JH, Saitz R. Does readiness to change predict subsequent alcohol consumption in medical inpatients with unhealthy alcohol use? Addictive Behaviors. 2009;34:636–640. doi: 10.1016/j.addbeh.2009.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges G, Cherpitel CJ, Medina-Mora ME, Mondragon L, Casavuevas L. Alcohol consumption in emergency room patients and the general population: a population based study. Alcoholism: Clinical and Experimental Research. 1998;22:1986–1991. [PubMed] [Google Scholar]
- Cherpitel CJ. Accidents and injuries from alcohol. In: Jaffe JH, editor. Encyclopedia of Drugs and Alcohol. Vol. 1. New York: Macmillan Publishing Co; 1995. pp. 8–10. [Google Scholar]
- Cherpitel CJ. A brief screening instrument for problem drinking in the emergency room: the RAPS4. Journal of Studies on Alcohol. 2000;61:447–449. doi: 10.15288/jsa.2000.61.447. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ, Bernstein E, Bernstein J, Moskalewicz J, Swiatkiewicz G. Screening, Brief Intervention and Referral to Treatment (SBIRT) in a Polish emergency room: challenges in a cultural translation of SBIRT. Journal of Addictions Nursing. 2009;20:127–131. doi: 10.1080/10884600903047618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherpitel CJ, Borges G, Giesbrecht N, Hungerford D, Peden M, Poznyak V, Room R, Stockwell T. Alcohol and Injuries: Emergency department studies in an international perspective. Geneva, Switzerland: World Health Organization; 2009. [Google Scholar]
- Cherpitel CJ, Korcha R, Moskalewicz J, Swiatkiewicz G, Ye Y, Bond J. Screening, brief intervention and referral to treatment (SBIRT): 12-month outcomes of a randomized controlled clinical trial in a Polish emergency department. Alcoholism: Clinical and Experimental Research. 2010;34:1922–1928. doi: 10.1111/j.1530-0277.2010.01281.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherpitel CJ, Moskalewicz J, Swiatkiewicz G, Ye Y, Bond J. Screening, brief intervention and referral to treatment (SBIRT) in a Polish emergency department: three-month outcomes of a randomized controlled clinical trial. Journal of Studies on Alcohol and Drugs. 2009;70:982–990. doi: 10.15288/jsad.2009.70.982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherpitel CJ, Ye Y, Bond J, Borges G, Cremonte M, Marais S, Poznyak V, Sovinova H, Moskalewicz J, Swiatkiewicz G. Cross-national performance of the RAPS4/RAPS4-QF for tolerance and heavy drinking: data from 13 countries. Journal of Studies on Alcohol. 2005;66:428–432. doi: 10.15288/jsa.2005.66.428. [DOI] [PubMed] [Google Scholar]
- D’Onofrio G, Degutis LC. Preventive care in the emergency department: screening and brief intervention for alcohol problems in the emergency department: a systematic review. Academic Emergency Medicine. 2002;9:627–638. doi: 10.1111/j.1553-2712.2002.tb02304.x. [DOI] [PubMed] [Google Scholar]
- Daeppen JB, Bertholet N, Gmel G, Gaume J. Communication during brief intervention, intention to change, and outcome. Substance Abuse. 2007;28:43–51. doi: 10.1300/J465v28n03_05. [DOI] [PubMed] [Google Scholar]
- Delucchi K, Kaskutas LA. Following problem drinkers over 11 years: understanding changes in alcohol consumption. Journal of Studies on Alcohol and Drugs. 2010:71. doi: 10.15288/jsad.2010.71.831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field CA, Baird J, Saitz R, Caetano R, Monti PM. The Mixed Evidence for Brief Intervention in Emergency Departments, Trauma Care Centers, and Inpatient Hospital Settings: What Should We Do? Alcoholism: Clinical and Experimental Research. 2010;34:2004–2010. doi: 10.1111/j.1530-0277.2010.01297.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield TK. Individual risk of alcohol-related disease and problems. In: Heather N, Peters TJ, Stockwell T, editors. International Handbook of Alcohol Problems and Dependence. New York: John Wiley; 2001. pp. 413–437. [Google Scholar]
- Grothues JM, Bischof G, Reinhardt S, Meyer C, John U, Rumpf HJ. Differences in help seeking rates after brief intervention for alcohol use disorders in general practice patients with and without comorbid anxiety or depressive disorders. Int J Methods Psychiatr Res. 2008;17(Suppl 1):S74–77. doi: 10.1002/mpr.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heather N, Smailes D, Cassidy P. Development of a Readiness Ruler for use with alcohol brief interventions. Drug and Alcohol Dependence. 2008;98:235–240. doi: 10.1016/j.drugalcdep.2008.06.005. [DOI] [PubMed] [Google Scholar]
- Hesse M. The Readiness Ruler as a measure of readiness to change poly-drug use in drug abusers. Harm Reduction Journal. 2006;3:3. doi: 10.1186/1477-7517-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaner E. Brief alcohol intervention: time for translational research. Addiction. 2010;105:960–961. 964–965. doi: 10.1111/j.1360-0443.2009.02848.x. [DOI] [PubMed] [Google Scholar]
- Kaskutas LA, Weisner C, Caetano R. Predictors of help seeking among a longitudinal sample of the general population, 1984–1992. Journal of Studies on Alcohol. 1997;58:155–161. doi: 10.15288/jsa.1997.58.155. [DOI] [PubMed] [Google Scholar]
- Kunz FM, Jr, French MT, Bazargan-Hejazi S. Cost-effectiveness analysis of a brief intervention delivered to problem drinkers presenting at an inner-city hospital emergency department. Journal of Studies on Alcohol. 2004;65:363–370. doi: 10.15288/jsa.2004.65.363. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Conigliaro J, McNeil M, Kraemer K, Conigliaro RL, Kelley ME. Effects of two types of brief intervention and readiness to change on alcohol use in hazardous drinkers. Journal of Studies on Alcohol. 2001;62:605–614. doi: 10.15288/jsa.2001.62.605. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Preparing people for change. 2. New York, NY: Guilford Press; 2002. [Google Scholar]
- Miller WR, Tonigan JS, Longabaugh R. Project MATCH Monograph Series 4. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health; 1995. The Drinker Inventory of Consequences (DrInC): An instrument for assessing adverse consequences of alcohol abuse [NIH Pub. No. 95-3911] [Google Scholar]
- Nock MK. Conceptual and design essentials for evaluating mechanisms of change. Alcoholism: Clinical and Experimental Research. 2007;31:4S–12S. doi: 10.1111/j.1530-0277.2007.00488.x. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC. Toward a comprehensive model of change. In: Miller WR, Heather N, editors. Treating Addictive Behaviors: Processes of change. New York, NY: Plenum Press; 1986. pp. 3–27. [Google Scholar]
- Prochaska JO, DiClemente CC. Stages of change in the modification of problem behaviors. Progress in Behavior Modification. 1992;28:183–218. [PubMed] [Google Scholar]
- Reed DN, Jr, Wolf B, Barber KR, Kotlowski R, Montanez M, Saxe A, Coffey DC, Pollard M, Fitzgerald HE, Richardson JD. The stages of change questionnaire as a predictor of trauma patients most likely to decrease alcohol use. Journal of the American College of Surgeons. 2005;200:179–185. doi: 10.1016/j.jamcollsurg.2004.10.020. [DOI] [PubMed] [Google Scholar]
- Rehm J, Rehn N, Room R, Monteiro M, Gmel G, Jernigan D, Frick U. The global distribution of average volume of alcohol consumption and patterns of drinking. European Addiction Research. 2003;9:147–156. doi: 10.1159/000072221. [DOI] [PubMed] [Google Scholar]
- Rollnick S, Heather N, Gold R, Hall W. Development of a short ‘readiness to change’ questionnaire for use in brief, opportunistic interventions among excessive drinkers. British Journal of Addiction. 1992;87:743–754. doi: 10.1111/j.1360-0443.1992.tb02720.x. [DOI] [PubMed] [Google Scholar]
- Room R, Graham K, Rehm J, Jernigan D, Monteiro M. Drinking and its burden in a global perspective: policy considerations and options. European Addiction Research. 2003;9:165–175. doi: 10.1159/000072223. [DOI] [PubMed] [Google Scholar]
- Saitz R. Clinical practice. Unhealthy alcohol use. New England Journal of Medicine. 2005;352:596–607. doi: 10.1056/NEJMcp042262. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline Follow-Back: a technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen JP, editors. Measuring Alcohol Consumption: Psychosocial and biological methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- SPSS Inc. PASW Statistics. Chicago, IL: SPSS, Inc; 2009. p. 18. [Google Scholar]
- Stata Corp. Stata Statistical Software: Release 9.0. College Station, TX: Stata Corporation; 2005. [Google Scholar]
- Stein LA, Minugh PA, Longabaugh R, Wirtz P, Baird J, Nirenberg TD, Woolard RF, Carty K, Lee C, Mello M, Becker B, Gogineni A. Readiness to change as a mediator of the effect of a brief motivational intervention on posttreatment alcohol-related consequences of injured emergency department hazardous drinkers. Psychology of Addictive Behaviors. 2009;23:185–195. doi: 10.1037/a0015648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JA. Resolving problems associated with alcohol and drug misuse: understanding relations between addictive behavior change and the use of services. Substance Use & Misuse. 2001;36:1501–1518. doi: 10.1081/ja-100106961. [DOI] [PubMed] [Google Scholar]
- Walton MA, Goldstein AL, Chermack ST, McCammon RJ, Cunningham RM, Barry KL, Blow FC. Brief alcohol intervention in the emergency department: moderators of effectiveness. Journal of Studies on Alcohol and Drugs. 2008;69:550–560. doi: 10.15288/jsad.2008.69.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams EC, Horton NJ, Samet JH, Saitz R. Do brief measures of readiness to change predict alcohol consumption and consequences in primary care patients with unhealthy alcohol use? Alcoholism: Clinical and Experimental Research. 2007;31:428–435. doi: 10.1111/j.1530-0277.2006.00324.x. [DOI] [PubMed] [Google Scholar]