Abstract
Objective
We analyze whether decreased emergency department (ED) access results in adverse patient outcomes or changes in the patient health profile for patients with acute myocardial infarction (AMI).
Data
We merge Medicare claims, American Hospital Association annual surveys, Medicare hospital cost reports, and location information for 1995–2005.
Study Design
We define four ED access change categories and estimate a ZIP Code fixed-effects regression models on the following AMI outcomes: mortality rates, age, and probability of percutaneous transluminal coronary angioplasty (PTCA) on day of admission.
Principal Findings
We find a small increase in 30-day to 1-year mortality rates among patients in communities that experience a <10-minute increase in driving time. Among patients in communities with >30-minute increases, we find a substantial increase in long-term mortality rates, a shift to younger ages (suggesting that older patients die en route), and a higher probability of immediate PTCA. Most of the adverse effects disappear after the transition years.
Conclusions
Deterioration in geographic access to ED affects a small segment of the population, and most adverse effects are transitory. Policy planners can minimize the adverse effects by providing assistance to ensure adequate capacity of remaining EDs, and facilitating the realignment of health care resources during the critical transition periods.
Keywords: Emergency department access, acute myocardial infarction, health outcomes
According to the National Center for Health Statistics, the number of emergency departments (EDs) decreased from 4,176 to 3,195 between 1995 and 2005, while annual ED visits increased from 96.5 million to 115.3 million during the same period (Nawar, Niska, and Xu 2007). This trend has been noted as a major issue facing the emergency care system in the United States by the Institute of Medicine (Institute of Medicine 2007; Niska, Bhuiya, and Xu 2010), and literature documenting decreased access to EDs abounds (Institute of Medicine 2007; DeLia and Cantor 2009). However, while there are many anecdotal reports or single-hospital case studies suggesting the adverse effects of overcrowding and closures on patient care (Adams and Biros 2001; Hwang et al. 2006; Pines et al. 2007; Pines and Hollander 2008), there is little systematic empirical evidence to demonstrate these claims.
The principal objective of our research is to examine whether decreased ED access (measured by increased driving time to the nearest ED) results in adverse patient outcomes or changes in patient health profiles. We focus on acute myocardial infarction (AMI) patients, a group that has relatively homogenous patient characteristics and is sensitive to the availability of ED care. Specifically, we address the following research questions:
Does increased driving time to the nearest ED result in increased mortality rates among AMI patients?
Does increased driving time to the nearest ED result in changes in health profile of AMI patients who arrived alive in the hospital?
If decreased ED access has an adverse effect on patient outcomes, is the effect transitory or permanent?
We expand the previous literature on ED access in several ways. First, we capture permanent ED closure even in hospitals that did not close down. Second, we provide national estimates of the effect of decreased ED access on patient outcomes. Third, we examine whether there are changes in patient health profiles when distance to ED changes. Finally, we explore potential temporal effects.
Background and Conceptual Framework
There is little systematic evidence examining whether decreased ED access affects eventual patient outcomes. Few studies link decreased ED access to deterioration in process measures for cardiac patients, none of which use nationally representative data. One study found that ED crowding, as measured by patients’ perceived waiting time, is positively associated with increased rates of patients who are left without being seen (Vieth and Rhodes 2006). Schull and colleagues found that simultaneous ambulance diversion at multiple EDs increased transport times and total out-of-hospital interval delays for cardiac patients (Schull et al. 2003), and that ED crowding is positively associated with increased time to thrombolytic for AMI (Schull et al. 2004).
Aside from the limited studies that link ED access to process measures, we are not aware of any large-scale studies reporting actual changes in patient outcomes due to changes in geographical access to ED. Only one study links hospital closures to health outcomes, reporting on LA County between 1997 and 2003. That study showed that increased distance to the closest hospital, regardless of ED availability, was linked to increased deaths from MI and unintentional injuries (Buchmueller, Jacobson, and Wold 2006).
Acute myocardial infarction is a time-sensitive illness. This study focused on how changes in distance to the closest ED affect health outcomes of AMI patients, taking into account whether the nearest hospital has a cardiac catheterization capacity. We obtained patient characteristics from the Medicare inpatient claims, thereby focusing on AMI patients who survived their acute onset of AMI long enough to generate a hospital admission record. The probability of surviving long enough to have a hospital admission record depends on several factors: age, the initial severity of illness, and time to arrival at ED. Several predictions occur when arrival is delayed, holding all other factors constant:
When travel time increases, older patients are more likely than younger patients to have died en route.
Severity of illness can increase with increased travel time.
People with more severe cases of heart attack have a lower probability of survival than those with milder cases.
When the nearest ED is closed, it effectively delays arrival time to the next ED for such a patient. We hypothesized that decreased ED access would affect patient population in the following ways:
Patients who survived to have hospital records would be younger in areas with decreased ED access than those in areas with no decrease in ED access.
The observed mortality rates of all AMI patients would increase when ED access decreased, but the observed mortality rates of patients who survived to have a hospital record might not.
Due to deterioration of condition associated with delayed time of arrival, patients in areas with decreased ED access would arrive at the hospital with higher probability of needing an immediate procedural intervention.
Study Design
Overview
We took a difference-in-differences approach to estimate the effect of ED closure on AMI health outcomes. Specifically, we identified the effects of ED access by comparing outcomes of AMI population between the following groups: (1) people who live in ZIP Codes with no increase in driving time to their closest ED (the control group); and (2) people who live in ZIP Codes that experience <10-, 10- to 30-, or >30-minute increases in driving time. These time thresholds were chosen based on knowledge of the importance of timely care for AMI patients and the empirical distribution of the driving time change. We implement ZIP Codes fixed-effects models and include year dummies, full interaction of patient demographics information, and several risk adjustment variables as available from claims data. We focus on the AMI population, because AMI usually requires immediate medical attention and is sensitive to the availability of ED care.
Data Sources and Patient Population
The primary data sources for ED availability are the American Hospital Association annual surveys. We linked each patient's ZIP Code with longitude and latitude coordinates of each ZIP Code using Mailer's software (2006). Finally, using the longitude and latitude coordinates of the hospital's physical address or heliport (Horwitz and Nichols 2009), we calculated driving time between each patient to the nearest ED. We modified the AHA data the following ways to minimize reporting errors: (1) we use California OSHPD facility data, an administrative database, to verify ED status for California hospitals; and (2) when hospitals did not report whether they offered a service in a given year, we impute the values using information from adjacent years. Patient data, including patient's mailing ZIP Codes, were obtained from MedPAR.
We identified the AMI population by extracting from 100 percent of MedPAR records with 410.x0 or 410.x1 as the principal diagnoses between 1995 and 2005. We employed McClellan et al.'s exclusion criteria to minimize selection bias (McClellan, McNeil, and Newhouse 1994). In addition, we excluded 23 percent of the patient population who were not admitted through the ED, as direct admission to ED is the relevant population based on our conceptual framework. We also excluded 11 percent of patients whose admitted hospital is more than 100 miles away from their mailing ZIP Codes, as those patients are likely not residing at their mailing address or were admitted to hospitals while away from home. We excluded ZIP Codes that experienced multiple changes in distance to their closest ED during the study period (3 percent of the sample) as these patients do not represent patients who have experienced a single change and would not contribute to answering the original research question. Finally, we excluded ZIP Codes that do not have patients both before and after the access change occurred (1 percent). The final sample consisted of approximately 150,000 patients per year from 1996 to 2005 for a total sample size of 1.49 million patient-year observations.
Methods
Defining AMI Outcomes
We examined the following health characteristics of the AMI population: mortality rates (7-day, 30-day, 90-day, 180-day, and 1-year), age at the time of hospital admission, and whether the patient received percutaneous transluminal coronary angioplasty (PTCA) on the day of admission. The three types of outcomes allowed us to explicitly test the hypotheses in the conceptual framework.
Defining Changes in Access to ED
In this study, our key variable of interest is each patient's time to the nearest ED and, more important, whether patients reside in locations where driving time to ED has increased during the study period. We first calculated the distance between each ZIP Code to the nearest ED using the population centroid location of the ZIP Code, separately for each year. The distance calculation based on longitude and latitude coordinates is highly correlated with actual driving distance1(Love and Morris 1979; Phibbs and Luft 1995). Next, we computed the change in distance between adjacent years for each ZIP Code community. To give a better sense of the extent of change each ZIP Code faced and to provide clarity in presenting the multivariate results, we translated changes in distance to changes in driving time using the formula by Phibbs and Luft (Phibbs and Luft 1995; Phibbs 2008). Finally, we classified the communities according to whether the driving time between a community and the nearest ED satisfied the following condition between 1996 and 2005: (1) did not increase (the control group); (2) increased by <10 minutes; or (3) increased by 10–30 minutes; and (4) increased by more than 30 minutes. We divided the treatment groups into the above three categories for easier interpretation of results and to allow for the possibility that the effect might not be linear over travel time. The fixed-effects model effectively compares outcome differences among patients in the treatment group before and after the increase to the driving time occurred, to the change in outcome across years among patients in the control group.
Statistical Methods
We estimated the effect of increased driving time to ED as follows:
| (1) |
where Yijt is the health outcome of patient i residing in ZIP Code j in year t; αt is the year indicators; Inc10jt = 1 for ZIP Code j on and after year t if time to closest ED increases by <10 minutes in year t; 0 otherwise; Inc10_30jt = 1 for ZIP Code j on and after year t if time to closest ED increases by 10–30 minutes in year t; 0 otherwise; Incgt30jt = 1 for ZIP Code j on and after year t if time to closest ED increases by at least 30 minutes in year t; 0 otherwise; cathjt = 1 if the closest ED in ZIP Code j has cath lab available in year t; 0 otherwise; Xijt is a vector of demographics and comorbidity variables of patient i; Wit is a vector of hospital characteristics of patient i's admitted hospital; Zj is the ZIP Codes fixed effects.
We estimate model 1 separately for the health outcomes described above. We used least square fixed-effects models to estimate the effect of ED access on age, a continuous variable. For the mortality and PTCA variables, we use a linear probability model with ZIP Codes fixed effects. Even though a probit or logit model is a natural choice of estimating a dichotomous dependent variable in a cross-sectional data, these models might result in inconsistent estimator in panel data setting, because we are including significant number of ZIP Code fixed effects (Buchmueller, Jacobson, and Wold 2006; Greene 2008). The linear probability models can consistently estimate the effect of changes in driving time on these mortality outcomes (Buchmueller, Jacobson, and Wold 2006). One drawback of the linear probability model is that the predicted probability can be out of bound. As our sample mean of the dependent variable is not close to the boundary, we obtain virtually no out of bound predictions among the 1.49 million observations in our analysis. Another drawback of the linear probability model is that the error term is heteroskedastic. We corrected this problem by estimating heteroskedasticity-robust standard errors (Stock and Watson 2006) for all models that allow for intra ZIP Code correlation among patients who belong to the same ZIP Code.
In model 1, the variables of interest are the three access change indicators (Inc10, Inc10_30, and Incgt 30) that capture the difference-in-differences estimators.2 The control variables, X's, include fully interacted patient demographic covariates (5-year age groups, gender, white, black or other race, counts of comorbidities, and urban or rural residence). In the model where age is the outcome of interest, we do not include age groups when constructing the fully interacted patient demographic covariates. We defined ZIP Codes as being in an urban area if it belonged to a Metropolitan Statistical Area (MSA). We also included a list of disease-related risk adjustment following prior work (Skinner and Staiger 2009); specifically, if patients had peripheral vascular disease, chronic pulmonary disease, dementia, chronic renal failure, diabetes, liver disease, or cancer at the time of admission. Last, we included hospital organizational characteristics of the admitted hospital, including hospital ownership (for-profit, government), size (measured by log transformed total inpatient discharges), and catheterization lab availability.
When the nearest ED closes, patients may only experience temporary adverse effect of the closure, as communities could potentially realign their resources to compensate for the ED closure. In addition, the AHA reporting period for each hospital varies for a given annual survey—a hospital that indicate it no longer offers ED in the 2003 survey might in fact have closed the service sometime in 2002. It is also possible that an ED that closes might already experience difficulties in providing care due to reasons that eventually led to its closure (e.g., lack of available resources) a few years before closure occurred. In model 2, we therefore investigate the potential transitory effect by adding transition indicators. Specifically, for each ED access change category, we allow the effects to differ by the following transition year indicators: 2–3 years before the access change, 1 year before to 1 year after the change, 2–3 years after the change, and 4 or more years after the change.
We estimate our models on two samples: on the whole sample and on patients whose ZIP Codes have no more than two hospitals within 10-mile radius (about a 30-minute drive time) in the baseline. Large increases in driving time are more likely to occur in areas with limited access to hospitals. Comparing patient outcomes in those communities directly with the general AMI population may not be a fair comparison. The two sets of analyses allow us to examine whether the results are robust to differences in baseline access to hospitals.
Results
We found that 89.2 percent of the study population did not experience increased driving times to their nearest ED during the study period (including less than 3 percent that experienced decreases in driving time); 8.9, 1.7, and 0.2 percent of patients experienced <10-, 10- to 30-, and >30-minute increase in driving time, respectively. Figure 1 delineates which ZIP Codes are affected by the increased driving time. As the figure shows, large increases tend to occur in mountainous or desert regions.
Figure 1.
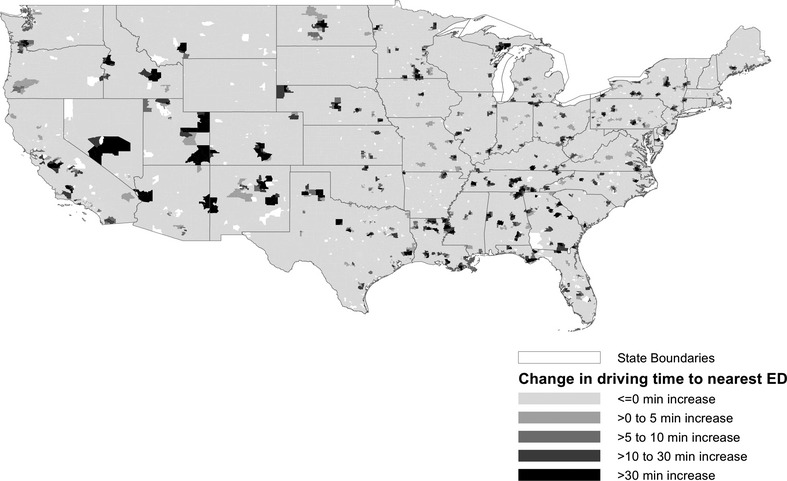
Geographical Distribution of Emergency Department (ED) Access Change between 1996 and 2005
Figure 2 displays the year trend in four AMI outcomes (7-day, 30-day mortality rates, average age, and share receiving PTCA on admission day) between 1996 and 2005. In general, AMI mortality rates have decreased over this time period, consistent with previous literature. There is an increasing trend in the average age of our study population (by about 2.5 years), as well as increased share of patients receiving PTCA on admission day (from 5 percent to 17 percent).
Figure 2.
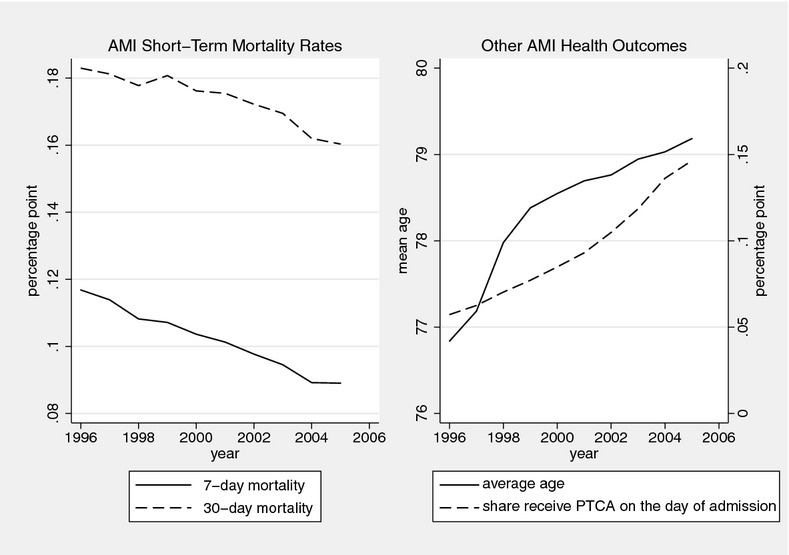
Overall Trend in Acute Myocardial Infarction (AMI) Health Outcomes 1996–2005
Figures 3 and 4 compare the unadjusted trends by the four ED access change categories. As each affected community experiences access change in a different year and we have shown in Figure 2 that trends in all outcomes do not stay flat, we normalize the trend and show the “relative” trend where the average value for each year is normalized to be zero. By construction, the control group is represented by the flat line at zero across all years. As an example, for 7-day mortality rates (Figure 3, left panel), the group of patients that experiences <10-minute or 10- to 30-minute increase in driving time have mortality rates similar or slightly below that of the control group. Among patients with a >30-minute increase in driving time, 7-day mortality rates trend upward 2 years prior to access change, and then downward the year after the change. The trend in age profile (Figure 4, left panel) also shows that the baseline average age in communities with the >30-minute increase tends to be lower than that in the control group; age exhibits a decreasing trend 1 year prior to the change and bounces back to a similar age as at baseline 2 years after the change. As the smallest sample size is in the >30-minute category (shown at the bottom of Table 1), the trend is less smooth compared with the other access change categories. The opposite pattern is observed for the share of patients receiving PTCA on the day of admission: the share spikes upward for this access category 2 years prior to the access change and returns to baseline 2 years after the change.
Figure 3.
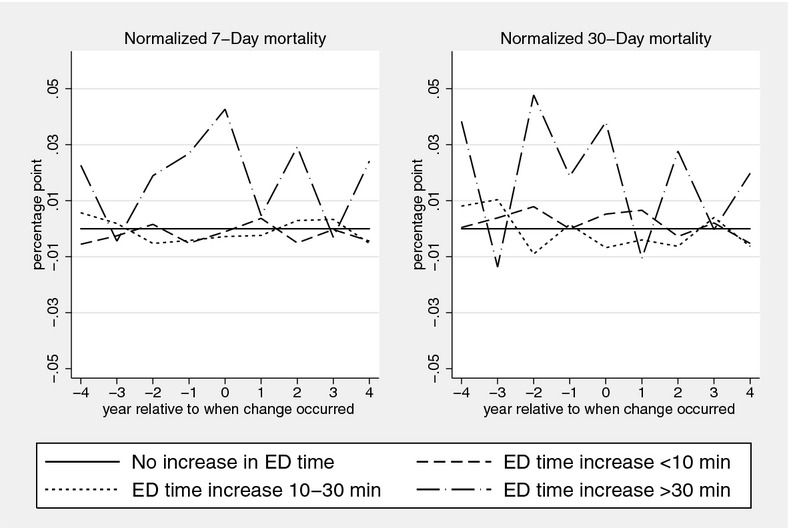
Relative Year Trend in Short-Term Acute Myocardial Infarction (AMI) Mortality Rates by Emergency Department (ED) Access Change Categories
Figure 4.
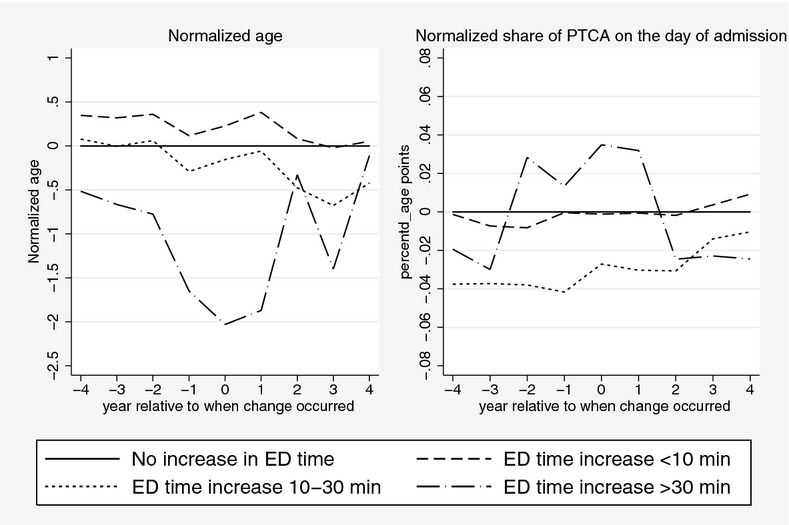
Relative Year Trend in Normalized Age and Percutaneous Transluminal Coronary Angioplasty (PTCA) Procedure by Emergency Department (ED) Access Change Categories
Table 1.
Descriptive Statistics of Patient Population by ED Access Change Categories
| Treatment Groups (Average before Change in Access Occurred) | ||||
|---|---|---|---|---|
| Mean (SD) | Control Group No Increase Driving Time to ED | Increase Time <10 Minutes | Increase Time 10–30 Minutes | Increase Time >30 Minutes |
| Patient characteristics | ||||
| Female | 0.51 | 0.52 | 0.50 | 0.50 |
| (0.50) | (0.50) | (0.50) | (0.50) | |
| African American | 0.07 | 0.10 | 0.07 | 0.09 |
| (0.25) | (0.30) | (0.25) | (0.29) | |
| Other nonwhite race | 0.04 | 0.04 | 0.02 | 0.03 |
| (0.19) | (0.20) | (0.14) | (0.16) | |
| Age | 78.56 | 78.43 | 78.33 | 77.53 |
| (7.87) | (7.85) | (7.80) | (7.66) | |
| Urban location | 0.75 | 0.93 | 0.71 | 0.17 |
| (0.43) | (0.25) | (0.45) | (0.38) | |
| Peripheral vascular disease | 0.08 | 0.07 | 0.08 | 0.07 |
| (0.27) | (0.26) | (0.27) | (0.25) | |
| Chronic pulmonary disease | 0.22 | 0.20 | 0.23 | 0.21 |
| (0.42) | (0.40) | (0.42) | (0.41) | |
| Dementia | 0.04 | 0.04 | 0.04 | 0.03 |
| (0.19) | (0.19) | (0.20) | (0.18) | |
| Chronic renal failure | 0.02 | 0.02 | 0.02 | 0.02 |
| (0.14) | (0.14) | (0.15) | (0.15) | |
| Diabetes | 0.27 | 0.28 | 0.28 | 0.28 |
| (0.44) | (0.45) | (0.45) | (0.45) | |
| Liver diseases | 0.00 | 0.00 | 0.00 | 0.00 |
| (0.06) | (0.06) | (0.05) | (0.04) | |
| Cancer | 0.05 | 0.05 | 0.05 | 0.04 |
| (0.22) | (0.22) | (0.22) | (0.21) | |
| Admitted hospital characteristics | ||||
| For-profit hospitals | 0.12 | 0.16 | 0.18 | 0.23 |
| (0.32) | (0.36) | (0.39) | (0.42) | |
| Government hospitals | 0.11 | 0.06 | 0.13 | 0.14 |
| (0.32) | (0.23) | (0.33) | (0.35) | |
| Total discharges | 11,375 | 8,487 | 5,814 | 1,363 |
| (42,526) | (6,735) | (5,068) | (1,004) | |
| Number of hospitals within 10-mile radius | 2.57 | 4.22 | 1.95 | 1.03 |
| (1.96) | (2.02) | (1.72) | (0.39) | |
| Number of ZIP Codes | 30,050 | 1,867 | 609 | 97 |
| Number of patients | 1,418,613 | 141,746 | 26,817 | 3,187 |
Note. ED, emergency department.
Table 1 presents the descriptive statistics of the independent variables by the four ED access change categories. In general, patient and hospital characteristics do not differ much across the access categories except for the following: patients who experience large increases in driving time are mostly in rural communities (among for those with a >30-minute increase, only 17 percent are in ZIP Codes that belong to a MSA). Their access to hospitals is also more limited: the average number of hospitals within the 10-mile radius in the control group is 2.57 compared with 1.03 hospitals among patients who experience >30-minute increases in driving time.
Table 2 presents the fixed-effects results for model 1. The top panel shows the results of the overall Medicare AMI ED population. For moderate increases in driving time (<30 minutes), mortality rates do not differ (full regression results available upon request), with one exception: for patients in communities with a <10-minute increase in driving time, 180-day mortality rate rose by 0.6 of one percentage point (p < .10). The last row of the top panel shows that having a catheterization lab in the nearest facility appears to lower the 7-day and 30-day mortality rates by 0.5 of one percentage point, but such an improvement in mortality disappears with the longer time horizon.
Table 2.
Effects of Driving Time on AMI Health Outcomes
| AMI Mortality Rates | Other Outcomes | ||||||
|---|---|---|---|---|---|---|---|
| 7-Day | 30-Day | 90-Day | 180-Day | 1-Year | Age | PTCA on Day of Admission | |
| Whole sample | |||||||
| All years after driving time increased by <10 minutes | −0.0002 | 0.0029 | 0.0046 | 0.0061† | 0.0037 | 0.0716 | −0.0064** |
| (0.0023) | (0.0032) | (0.0035) | (0.0036) | (0.0037) | (0.0636) | (0.0023) | |
| All years after driving time increased by 10–30 minutes | −0.0063 | −0.0098 | −0.0061 | −0.0026 | −0.0072 | −0.0295 | −0.0099* |
| (0.0049) | (0.0067) | (0.0074) | (0.0075) | (0.0075) | (0.1441) | (0.0045) | |
| All years after driving time increased by >30 minutes | 0.0172 | 0.0123 | 0.0258 | 0.0449† | 0.0565* | −0.8168† | 0.0194 |
| (0.0162) | (0.0223) | (0.0254) | (0.0255) | (0.0254) | (0.4303) | (0.0154) | |
| Closest hospital has catheterization lab | −0.0046* | −0.0047* | −0.0034 | −0.0026 | −0.0036 | −0.0887† | 0.0017 |
| (0.0018) | (0.0022) | (0.0025) | (0.0026) | (0.0027) | (0.0476) | (0.0020) | |
| Sample size | 1,485,442 | ||||||
| Comparable sample (two or fewer hospital access in the baseline) | |||||||
| All years after driving time increased by <10 minutes | 0.0095* | 0.0168* | 0.0203** | 0.0197** | 0.0165* | 0.1500 | −0.0091* |
| (0.0048) | (0.0067) | (0.0074) | (0.0075) | (0.0074) | (0.1275) | (0.0043) | |
| All years after driving time increased by 10–30 minutes | −0.0045 | −0.0056 | −0.0045 | −0.0010 | −0.0053 | 0.0570 | −0.0041 |
| (0.0052) | (0.0074) | (0.0083) | (0.0082) | (0.0084) | (0.1719) | (0.0050) | |
| All years after driving time increased by ≥30 minutes | 0.0178 | 0.0126 | 0.0269 | 0.0466† | 0.0574* | −0.7848† | 0.0212 |
| (0.0164) | (0.0225) | (0.0257) | (0.0258) | (0.0257) | (0.4376) | (0.0155) | |
| Closest hospital has catheterization lab | −0.0072** | −0.0060† | −0.0054 | −0.0036 | −0.0056 | −0.0533 | −0.0018 |
| (0.0025) | (0.0032) | (0.0034) | (0.0035) | (0.0036) | (0.0696) | (0.0031) | |
| Sample size | 789,735 | ||||||
Notes. Significant at
p < .10,
p < .05,
p < .01.
AMI, acute myocardial infarction; PTCA, percutaneous transluminal coronary angioplasty.
For patients with >30 minutes increase in driving time, the adverse effect appears in long-term mortality: overall 180-day and 1-year mortality rates increased by five percentage points. The bottom panel of Table 2 reports the results limiting the sample to those patients with access to two or fewer hospitals within 10-mile radius in the baseline. The adverse effects on mortality rates become magnified across all time horizons for patients facing a <10-minute increase in driving time. Specifically, relative to the control group, the mortality rates among this group of patients increased by 1–2 percentage points after the change. The positive and significant increase persists when examining a longer time horizon (up to 1 year after admission). The rest of the results on mortality rates for the other two ED access change categories are similar to the top panel.
The last two columns of Table 2 show the results on age and probability of receiving PTCA on the day of admission. The results are similar in the whole sample and the sample with limited baseline access. For patients experiencing a >30-minute increase in driving time, the effect is consistent with the conceptual framework—the average age declined by 0.8 years but there were no observed differences in the probability of receiving PTCA. For patients experiencing <10-minute increase in driving time, the probability of receiving PTCA dipped by about 0.6–0.9 of one percentage point.
Table 3 shows the estimated effects from model 2 where we add transition indicators for each access change category. Results from this table 2 show how the effects of the transition years are masked when looking only at the overall effect, as in Table. For clarity of presentation, we report only the results of the second sample, which is limited to, at most, two-hospital access within a 10-mile radius at baseline. This sample represents a more comparable control group (whole sample results available upon request). In Table 2, mortality rates increased among patients in areas with a <10-minute increase in driving time after the access change. Table 3 suggests that most of those adverse effects are transitory: the adverse effect peaks mostly 1 year before the change (1.5–3 percentage points, depending on the time horizon), persists at a similar level up to 3 years after the change, but gradually decreases its magnitude beyond the initial 3-year window. The results on age show that the temporary increase in mortality rates is not due to changes in patient population age; there is no difference in age between the control group and this group during the initial 3-year window, although the average increases slightly (by 0.4 of 1 year) beyond this window.
Table 3.
Effects of Timing of Change on AMI Health Outcomes
| AMI Mortality Rates | Other Outcomes | ||||||
|---|---|---|---|---|---|---|---|
| 7-Day | 30-Day | 90-Day | 180-Day | 1-Year | Age | PTCA on Day of Admission | |
| Driving time increased by <10 minutes | |||||||
| 2–3 years before access change | 0.0055 | 0.0209* | 0.0140 | 0.0128 | 0.0105 | 0.0619 | −0.0066 |
| (0.0066) | (0.0085) | (0.0099) | (0.0099) | (0.0102) | (0.1722) | (0.0053) | |
| 1 year before to 1year after | 0.0151** | 0.0309** | 0.0302** | 0.0284** | 0.0236** | 0.0962 | −0.0101† |
| (0.0057) | (0.0072) | (0.0088) | (0.0087) | (0.0088) | (0.1557) | (0.0057) | |
| 2–3 years after access change | 0.0117 | 0.0251* | 0.0257* | 0.0228† | 0.0207† | 0.3349† | −0.0187* |
| (0.0075) | (0.0100) | (0.0107) | (0.0117) | (0.0108) | (0.1916) | (0.0079) | |
| 4+ years after access change | 0.0013 | 0.0169† | 0.0189† | 0.0234* | 0.0154 | 0.4413* | −0.0153† |
| (0.0073) | (0.0097) | (0.0111) | (0.0118) | (0.0112) | (0.2128) | (0.0089) | |
| Driving time increased by 10–30 minutes | |||||||
| 2–3 years before access change | −0.0107† | −0.0138† | −0.0123 | −0.0161† | −0.0207* | 0.3329* | −0.0068 |
| (0.0059) | (0.0075) | (0.0090) | (0.0089) | (0.0098) | (0.1639) | (0.0042) | |
| 1 year before to 1year after | −0.0118† | −0.0110 | −0.0093 | −0.0066 | −0.0124 | 0.1943 | −0.0100† |
| (0.0062) | (0.0086) | (0.0091) | (0.0087) | (0.0091) | (0.2099) | (0.0057) | |
| 2–3 years after access change | 0.0023 | −0.0094 | −0.0062 | −0.0094 | −0.0174 | 0.2104 | 0.0029 |
| (0.0085) | (0.0115) | (0.0131) | (0.0136) | (0.0137) | (0.2745) | (0.0081) | |
| 4+ years after access change | −0.0048 | −0.0265† | −0.0264† | −0.0175 | −0.0280† | 0.3879 | 0.0066 |
| (0.0100) | (0.0136) | (0.0149) | (0.0149) | (0.0159) | (0.3117) | (0.0128) | |
| Driving time increased by >30 minutes | |||||||
| 2–3 years before access change | −0.0034 | −0.0053 | −0.0220 | 0.0027 | 0.0062 | 0.0949 | 0.0174 |
| (0.0142) | (0.0196) | (0.0212) | (0.0258) | (0.0257) | (0.4330) | (0.0185) | |
| 1 year before to 1year after | 0.0172 | 0.0061 | 0.0097 | 0.0390 | 0.0565* | −1.0677* | 0.0390* |
| (0.0197) | (0.0257) | (0.0280) | (0.0271) | (0.0287) | (0.5030) | (0.0161) | |
| 2–3 years after access change | 0.0120 | 0.0217 | 0.0236 | 0.0637† | 0.0659* | 0.1653 | −0.0036 |
| (0.0252) | (0.0262) | (0.0301) | (0.0332) | (0.0327) | (0.6539) | (0.0247) | |
| 4+ years after access change | 0.0135 | 0.0080 | 0.0535 | 0.0884* | 0.0760* | 0.3865 | 0.0224 |
| (0.0231) | (0.0309) | (0.0357) | (0.0393) | (0.0374) | (0.7005) | (0.0344) | |
| Sample size | 789,735 | ||||||
Notes. Significant at
p < .10,
p < .05,
p < .01;
estimate based on comparable sample (two or fewer hospital access in the baseline).
AMI, acute myocardial infarction; PTCA, percutaneous transluminal coronary angioplasty.
Similar to model 1, we do not find any noticeable increase in mortality rates or transition effect on age and probability of receiving PTCA among patients experiencing 10- to 30-minute increase in driving time. For patients living in communities that experience a >30-minute increase, we observe an alarming trend in long-term mortality rates. The 1-year mortality rates increase by 5.6 percentage points during the initial transition years, and this increase does not wane; the increase in 1-year mortality rates persists and rises to almost eight percentage points beyond the first 3 years.
The last two columns of Table 3 show that the drop in average age that we observed in Table 2 is temporary. The average age dropped by 1 year only during the initial transition time (from 1 year before to 1 year after the change occurred). Similarly, the share of patients receiving PTCA on the day of admission only temporarily increased by 3.9 percentage points during that window.
Sensitivity Analysis
Our sample does not include patients who died upon arrival or in the ED; those patients only have outpatient records. We obtained authorization to access 3 years of outpatient records (1996, 2000, and 2005) and explored several issues related to this excluded group. First, we found that less than 7 percent of the AMI population has outpatient claims only. Second, this group has much higher mortality rates than the patients that eventually were admitted to the hospital: their average in-hospital mortality rate is 22 percent in 1996 compared with 14 percent in the main sample. When we added this group to our original sample, the pattern observed in Figures 3 and 4 remains similar, and our conclusions on the key ED access change variables remain the same.
We also investigated whether the change in access could have differential effects among patients with different initial travel times. We estimated a model that included an interaction term between the initial travel time and the three change categories. None of the interaction terms was statistically significant.
Discussion
Hospital-based EDs are, as stated by the Institute of Medicine (2007), at a “breaking point,” with increasing ED utilization and decreasing number of EDs available. In this paper, we assemble a longitudinal national dataset to address a key issue regarding the relationship between ED access and patient outcomes. Our empirical results provide the first national estimates of the effect of ED access on health outcomes for the AMI population and can be summarized as follows: first, ED access deterioration, as measured by increased driving time to the nearest ED, affects less than 11 percent of the population. Second, small increases in driving time (<10 minutes) have a small adverse effect on mortality rates, and the magnitude of the effect is greater for those with limited access to hospitals at baseline. Third, large increases in driving time (>30 minutes) increase the observed long-term mortality rates and also change the health profile of the admitted patients (younger age, and higher probability of receiving PTCA on the day of admission). Last, the observed adverse effects are mostly temporary: all outcomes return to pre-access-change levels beyond the initial 3-year transition window, except for long-term mortality rates for those facing a >30-minute increase—the effect lingers and, in fact, escalates when looking beyond the transition window.
It is important to recognize that we focus exclusively on geographic access alone and its effect on patient outcomes. While this is an important aspect of access, especially for illness where time is critical, there are other ED access issues that we cannot address in this study, such as financial or cultural barriers. Persons in communities with “easy” geographic access to ED could still experience worse outcomes if other barriers worsen over time.
The study has several limitations. First, our distance variable is based on the longitude and latitude information of the ZIP Code's population center. Even though this distance measure is highly correlated with driving distance, two people from the same ZIP Code might have very different access to the same ED, especially in rural areas. Similarly, we cannot take into account traffic conditions, mountain roads, and bodies of water in our calculation of driving time. In addition, we do not capture the actual ED capacity on the day a patient suffers from AMI—a particular ZIP Code could face no change in driving time to the nearest ED, but if the ED is on diversion on the day he needs access (i.e., the ED was overcrowded and ambulances were being diverted to other EDs), that still results in decreased access for such a patient. On the opposite end of the scenario, a patient living in the affected communities might not experience changes in driving time if he already bypasses his closest ED before closure. However, the experience and outcome of that patient in his regularly attended hospital could be different pre and postclosure, especially since closure of the nearest ED could affect his regularly attended hospital's ability to deliver care in a timely fashion due to increased patient load. All the limitations described above introduce measurement errors in our measure of access change and could cause attenuation bias in our estimated effect on outcomes. Therefore, our estimated effects should be considered as lower bound.
Second, our patient population consists of Medicare patients who are not in managed care plans, since MedPAR is the only source of data with reliable outcome information at the national level for multiple years. Patient characteristics might have changed within this sample as more elderly patients move into managed care settings. We believe the movement to managed care would have a minimal impact on our estimated ED access effect, since there is no evidence to suggest that such movement is systematically linked to changes in area ED access.
Third, our data do not allow us to capture quality of prehospital care (i.e., care of the patient by paramedics in the ambulance en route to the hospital). If changes in the quality of EMS care vary systematically with changes in ED availability, our estimation would be biased. However, we are not aware of studies that show such a relationship. We are also not aware that time between dispatch and arrival of EMS should be influenced by ED closure in the area. The EMS community acknowledges that delays to the ED are detrimental, and we capture that dimension by using driving time as the proxy.
Finally, we are unable to ascertain whether the closed hospitals are systematically different in quality than those that remain opened. It is possible that ED closures were due to smaller or poorer-performing hospitals. Given this, however, our findings would be conservative since mortality would be biased downward if better hospitals preferentially survived. Similarly, while PTCA was used as a proxy for more severe illness due to delay in ED arrival, it is possible that the rates of PTCA were higher in patients who traveled further because their next available ED was a higher volume, more tertiary center, where PTCA was available and therefore utilized. However, our model controls for cath lab availability and our results show that the increase in PTCA is only temporary, whereas we would expect the PTCA rate to persist at a higher level if the increased PTCA rate were due to better access to catheterization lab as a result of the nearby closure.
Our findings raise several important issues regarding the resource allocation of the emergency care system in general. While worse geographic access can cause a delay in care, it is only one contributing factor. Our findings of adverse effects on mortality rates among communities experiencing only a small increase in driving time may indicate potential problems facing remaining nearby hospitals when one ED closes. These affected communities are mostly in urban settings with dense population where the EDs are already experiencing overcrowding. The influx of patients that the remaining hospitals have to absorb is likely to exacerbate the overcrowding conditions in their EDs and may potentially cause the spike in mortality that we observed. We further explored this possibility by examining changes in annual ED admissions with AMI before and after the closure among hospitals that are identified as the nearest ED for each community. We found that average admissions went up by 6.5 percent (p < .01) among communities that experienced a <10-minute increase. We also found that the average admission went up by 7 percent among EDs in communities experiencing a >30-minute increase in driving time (but not statistically significant due to small sample size).3
Even though only a very small segment of the population experienced a large increase in driving time to the nearest ED, the adverse effect of ED access deterioration surfaces in multiple dimensions. Unlike the communities with small increases in driving time where all adverse effects disappear beyond the first 3 years, the increase in long-term mortality rates for this segment of the population is substantial and persistent. The drop in average age among admitted patients is consistent with our conceptual framework predicting that patients in these communities who survive to have hospital records are younger than those in the control group, as older patients are more likely to die en route, given large increases in driving time.
In an exploratory analysis, we also noted that the number of AMI hospital admissions for this group dropped, relative to the other treatment and control groups during the transition years, an observation consistent with the conceptual framework. This implies that the true effect on mortality rates is even larger, when we take into account the potentially preventable deaths from this segment of patients, absent the large increase in driving time. In addition, the implications for medical costs and loss of quality of life may not be trivial when we consider that those who experienced large increases in driving time had a higher probability of receiving PTCA immediately, compared with the control group during the transition years. The deterioration in condition might have been prevented in the absence of such change of access.
Our estimated effects should be considered the lower bound of the true effect because we only observed patients who survived to have a hospital record. Future research to confirm these findings would require capturing a more comprehensive patient population, as well as better adjustment for clinical illness. Such knowledge is critical to validate the effects of such decreased availability of services on patient outcomes. In addition, there are other conditions where time is critical and affects a larger segment of the population (such as severe cases of asthma, sepsis, or trauma). Examining these conditions could reveal different issues regarding the role of ED access on patient outcomes and provide additional insight on the best practice of resource allocation to optimize emergency care services as a whole.
Overall, there is reason to be optimistic: almost all of the adverse effects disappear after 4 years. ED closure, and the accompanying change in access for the affected population, is not necessarily detrimental if the closure allows patients to get to better quality hospitals that have the capacity to absorb the additional patient load. Our results suggest that policy planners can minimize the adverse effects during the transition years by facilitating the realignment of health care resources during this critical period. Potential solutions might involve providing assistance to ensure adequate capacity at remaining operating EDs in the area before closures occur, and improved coordination between and among prehospital and hospital systems.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: We would like to thank Jean Roth (National Bureau of Economic Research) for helping to extract the Medicare data; Shouzu Lin (VA, Menlo Park) for excellent programming assistance; Laurence Baker (Stanford University) for helpful comments throughout the project; Tanja Srebotnjak (Ecologic Institute, Berlin, Germany) for her assistance in the generation of the map; and Amy J. Markowitz (UCSF) for copy editing. This project was supported by the Robert Wood Johnson Foundation's Changes in Health Care Financing and Organization initiative (grant 63974). In addition, Hsia was supported in part by a grant under the Robert Wood Johnson Foundation's Physician Faculty Scholars Program and the National Institutes of Health/National Center for Research Resources, University of California, San Francisco Clinical and Translational Science (KL2 RR024130). The views expressed herein are those of the authors and do not necessarily reflect the views of the funder or authors’ affiliated institutions.
Disclosures: None.
Disclaimers: None.
Notes
While Google maps or a MapQuest approach might be appropriate for study of local areas, it is not feasible for our study that uses national data over 10 years, as the former approach creates time-dependent bias in the calculation (road conditions and traffic conditions can vary drastically over 10 years). Our approach, while imperfect, affords a consistent derivation of driving time over our entire study period that has been validated with prior studies.
Because the AHA reporting period for each hospital varies for a given annual survey, we mark the access change indicator as the one the year before the hospital indicates its ED closure (i.e., a hospital that indicates no ED service availability in the 2003 survey might, in fact, have closed the service sometime in 2002).
We do not observe such high increases in average patient loads among communities with 10- to 30-minute increases in driving time (admissions increased by 0.4.%, p > .10), which is consistent with our finding of no adverse effect on mortality outcomes.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- Adams JG, Biros MH. The Endangered Safety Net: Establishing a Measure of Control. Academic Emergency Medicine. 2001;8(11):1013–5. doi: 10.1111/j.1553-2712.2001.tb01106.x. [DOI] [PubMed] [Google Scholar]
- Buchmueller T, Jacobson M, Wold C. How Far to the Hospital?The Effect of Hospital Closures on Access to Care. Journal of Health Economics. 2006;25(4):740–61. doi: 10.1016/j.jhealeco.2005.10.006. [DOI] [PubMed] [Google Scholar]
- DeLia D, Cantor J. Emergency Department Utilization and Capacity. Princeton, NJ: The Robert Wood Johnson Foundation; 2009. Research Synthesis Report. [Google Scholar]
- Greene WH. Econometric Analysis. Upper Saddle River, NJ: Prentice Hall; 2008. [Google Scholar]
- Horwitz JR, Nichols A. Hospital Ownership and Medical Services: Market Mix, Spillover Effects, and Nonprofit Objectives. Journal of Health Economics. 2009;28(5):924–37. doi: 10.1016/j.jhealeco.2009.06.008. [DOI] [PubMed] [Google Scholar]
- Hwang U, Richardson LD, Sonuyi TO, Morrison RS. The Effect of Emergency Department Crowding on the Management of Pain in Older Adults with Hip Fracture. Journal of the American Geriatrics Society. 2006;54(2):270–5. doi: 10.1111/j.1532-5415.2005.00587.x. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Hospital-Based Emergency Care: At the Breaking Point. Washington, DC: Institute of Medicine; 2007. [Google Scholar]
- Love RF, Morris JG. Mathematical Models of Road Travel Distances. Management Science. 1979;252:130–9. [Google Scholar]
- Mailer's Software. ZIP*Data. San Clemente, CA: Melissa Data; 2006. [Google Scholar]
- McClellan M, McNeil BJ, Newhouse JP. Does More Intensive Treatment of Acute Myocardial Infarction in the Elderly Reduce Mortality? Analysis Using Instrumental Variables. Journal of the American Medical Association. 1994;272(11):859–66. [PubMed] [Google Scholar]
- Nawar EW, Niska RW, Xu J. National Hospital Ambulatory Medical Care Survey: 2005 Emergency Department Summary. Advance Data. 2007;(386):1–32. [PubMed] [Google Scholar]
- Niska R, Bhuiya F, Xu J. National Hospital Ambulatory Medical Care Survey: 2007 Emergency Department Summary. National Health Statistics Report. 2010;(26):1–31. [PubMed] [Google Scholar]
- Phibbs C. 2008. Patient Incurred Cost – How Do I Estimate Travel Costs? [accessed on May 7, 2008]. Available at: http://www.herc.research.va.gov/resources/faq_h02.asp.
- Phibbs C, Luft H. Correlation of Travel Time on Roads Versus Straight Line Distance. Medical Care Research and Review. 1995;52(4):532–42. doi: 10.1177/107755879505200406. [DOI] [PubMed] [Google Scholar]
- Pines JM, Hollander JE. Emergency Department Crowding Is Associated with Poor Care for Patients with Severe Pain. Annals of Emergency Medicine. 2008;51(1):1–5. doi: 10.1016/j.annemergmed.2007.07.008. [DOI] [PubMed] [Google Scholar]
- Pines JM, Localio AR, Hollander JE, Baxt WG, Lee H, Phillips C, Metlay JP. The Impact of Emergency Department Crowding Measures on Time to Antibiotics for Patients with Community-Acquired Pneumonia. Annals of Emergency Medicine. 2007;50(5):510–6. doi: 10.1016/j.annemergmed.2007.07.021. [DOI] [PubMed] [Google Scholar]
- Schull MJ, Morrison LJ, Vermeulen M, Redelmeier DA. Emergency Department Gridlock and Out-of-Hospital Delays for Cardiac Patients. Academic Emergency Medicine. 2003;10(7):709–16. doi: 10.1111/j.1553-2712.2003.tb00064.x. [DOI] [PubMed] [Google Scholar]
- Schull MJ, Vermeulen M, Slaughter G, Morrison L, Daly P. Emergency Department Crowding and Thrombolysis Delays in Acute Myocardial Infarction. Annals of Emergency Medicine. 2004;44(6):577–85. doi: 10.1016/j.annemergmed.2004.05.004. [DOI] [PubMed] [Google Scholar]
- Skinner J, Staiger DO. Technology Diffusion and Productivity Growth in Health Care. 2009 doi: 10.1162/REST_a_00535. NBER Working Paper 14865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stock JH, Watson MW. Heteroskedasticity-Robust Standard Errors for Fixed Effects Panel Data Regression. Cambridge, MA: National Bureau of Economic Research; 2006. NBER Technical Working Paper Series No. t0323. [Google Scholar]
- Vieth T, Rhodes K. The Effect of Crowding on Access and Quality in an Academic ED. American Journal of Emergency Medicine. 2006;24(7):787–94. doi: 10.1016/j.ajem.2006.03.026. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


