Abstract
Objective
We sought to estimate the impact of knee osteoarthritis (OA) on health care utilization.
Research Design
Using the 2003 Medicare Current Beneficiary Survey, a population-based survey of Medicare beneficiaries linked to Medicare claims, we selected a national cohort of community-dwelling persons aged 65 and older with knee OA and a sex- and age-matched comparison cohort without any form of OA. We distinguished following 4 components of health care utilization: physician (MD) office visits, non-MD office visits, inpatient hospital stays, and emergency department visits. We built multiple regression models to determine whether knee OA affects utilization, controlling for comorbidity count, obesity, functional limitation, education, race, and working status.
Results
A total of 545 Medicare Current Beneficiary Survey participants with knee OA were matched with 1090 OA-free individuals. Mean age in both cohorts was 76 years; approximately 70% were female. Knee OA and OA-free subjects differed significantly in obesity (Knee OA: 37%, OA-free: 20%), % with ≥2 comorbidities (Knee OA: 69%, OA-free: 43%), and functional limitation (Knee OA: 42%, OA-free: 26%). In multivariable regression models, the knee OA cohort had on average 6.0 more annual MD visits (95% confidence interval [CI]: 4.7, 7.4) and 3.8 more non-MD visits (95% CI: 2.8, 4.7) than the OA-free cohort. The knee OA cohort also had 28% more hospital stays (odds ratio [OR] = 1.3, 95% CI: 1.0, 1.6), a difference attributable to total joint replacements.
Conclusions
This first national, population-based study of health care utilization in persons with knee OA documents considerable excess utilization attributable to knee OA, independent of comorbidity, and other patient characteristics.
Keywords: comorbidities, health care utilization, knee osteoarthritis
Knee osteoarthritis (OA) affects approximately 12% of Americans aged 60 and above,1 and accounts for substantial disability among the elderly.2–5 Knee OA is often accompanied by comorbid conditions, functional limitation, and obesity.6–10 Health care utilization is extensive among knee OA patients, including hospital inpatient and ambulatory services.11,12 Prior studies have shown that the cost for health services among persons with OA exceeded those without OA by 1.5- to 2.6-fold.13–17 This burden will increase as the population ages.
Previous research has examined health care utilization and/or cost among OA or arthritis patients in European populations,18–21 community-based cohorts,14,15,22 a state-wide pharmaceutical assistance program,22 HMO populations,12,13,16,23,24 and US Department of Veterans Affairs (VA) populations.25 Only a few of these studies compared OA patients with non-OA patients and controlled for potential confounding factors, such as comorbidity, to determine cost and/or utilization attributable to OA,13,26 and none of these studies has focused solely on knee OA.
The present study aims to compare health care utilization in persons with knee OA to those without OA in a US population-based sample. The study uses a national database linking Medicare claims with detailed survey data and focuses on knee OA, the most debilitating form of OA.2 We hypothesize that knee OA contributes significantly to health care utilization, independent of comorbidities, and functional limitation.
METHODS
Sample
We used data from the 2003 Medicare Current Beneficiary Survey (MCBS) Cost and Use files. The MCBS, sponsored by Centers for Medicare and Medicaid Services, surveys a nationally representative sample of US Medicare beneficiaries and links Medicare billing claims to survey-reported events.27 The 2003 MCBS cost and use sample was drawn from an enrollment list of those eligible for Medicare on January 1, 2002, and continuously enrolled in Medicare from January 1, 2002 into 2003. A supplemental sample is drawn each year to include newly enrolled persons and to replenish the sample for attrition because of death or other reasons, thereby ensuring that the sample remains representative of the US Medicare population. Interviews are conducted 3 times per year to collect information related to health care cost and utilization, including demographics, health status, and physical function.
We selected the knee OA cohort by choosing community-dwelling individuals aged 65 and older who had at least 1 visit in Medicare Part B records or Medicare Part A records (type of service = outpatient), with the International Classification of Diseases, ninth revision, Clinical Modification (ICD-9-CM) diagnostic code of 715. × 6 (OA of knee) or, alternatively, 719.46 (knee pain) plus 715. × 8, 715. × 9, or 715. × 0 (OA at other specified sites, at multiple sites and at unspecified site, respectively). We randomly sampled the OA-free cohort from MCBS community-dwelling persons aged ≥65 who never had a 2003 Part B or Part A (outpatient) Medicare billing record with an ICD-9 code for OA (ICD-9-CM code 715). Two sex- and age-matched OA-free persons were selected for each member of the knee OA cohort.
To ensure greater diagnostic accuracy, Part B claims were used for definition of the knee OA population and for determination of comorbidities only if the procedure code indicated a need for physician contact (such as a physician office visit or surgery).28 We also conducted a sensitivity analysis that excluded patients who had codes indicating a lower extremity joint replacement in 2003.
Data Elements
The data used in the analyses were compiled from following 3 domains: demographic, clinical, and health utilization.
Demographic Data
Age, race, sex, education, and working status were obtained from the MCBS survey. Race was stratified as “white” and “nonwhite”; educational attainment as “≤ high school” and “> high school”; and working status as a positive or negative response to a question asking whether the person was “now working at a job or business.”
Clinical Data
Body mass index (BMI) was calculated from self-reported height and weight. A BMI of ≥30 kg/m2 was considered obese.29 Functional status was categorized as poor if the survey respondent indicated “a lot of difficulty” or “inability” to walk one-quarter mile mile or 2 to 3 blocks. Comorbidity assignments were based on ICD-9-CM diagnostic codes recorded in the following types of Medicare claims: Part B, hospital inpatient and outpatient (Part A), and skilled nursing facility. The 6 comorbidity categories used in this analysis were cardiovascular disease, chronic obstructive pulmonary disease, diabetes, psychiatric disorders, cancer, and musculoskeletal diseases, excluding all types of OA. These conditions were selected because they are chronic, highly prevalent in the elderly, and generate high use of health resources.30 Specific ICD-9 codes underlying these conditions in the present analysis are outlined in Table 1.
TABLE 1.
Classification of Comorbidities by ICD-9 Code
| Comorbidity | ICD-9 Codes |
|---|---|
| Cancer | 140–208, 230–234 |
| Cardiovascular disease | 410–414, 428 |
| Other musculoskeletal diseases | 274, 710–714, 716–739 and not 711.0 |
| Diabetes | 250 |
| Psychiatric disorders | 296–311 |
| Chronic obstructive pulmonary disease | 490–496, 500–508 |
ICD indicates International Classification of Diseases.
Health Care Utilization
MD and non-MD office visits were determined from Medicare Part B claims and Part A outpatient records. Emergency department (ED) visits and inpatient stays were identified from hospital inpatient Medicare Part A records. ED visits were coded using revenue center codes 0450–0459. Each claim was categorized as a visit except in the following cases: only one claim per day per specialist type was counted; laboratory claims were counted as non-MD visits only on days lacking an MD visit; and multiple claims on the same day for the same category of service were counted as one visit. Non-MD visits included radiology facility bills separate from the radiologist claim, as well as nurse, physical therapist, and chiropractor encounters and laboratory studies.
Statistical Analysis
Factors associated with utilization of each of 4 domains, MD visits, non-MD visits, ED visits, and inpatient stays, were examined in univariate and multivariable analyses using the SAS Survey Procedures in SAS Version 9.1,31 applying sampling weights provided in MCBS data files. Hospital measures (ED visits and hospital stays) were examined as continuous (number of visits) and dichotomous (any versus none) outcomes, and ambulatory usage measures (MD and non-MD visits) were examined as continuous (number of visits) variables. Multivariable logistic regression models adjusting for demographic and clinical factors were built to examine the association between knee OA and 2 binary hospital outcomes: any ED visit and any hospital stay. Multivariable linear regression models were built to estimate adjusted rates of ambulatory resource utilization in the knee OA and OA-free cohorts. Independent factors considered included comorbidity count (0–1 vs. ≥2), functional limitation, obesity, education, race, and working status. In addition, we performed separate multivariable regression models to estimate ambulatory usage stratified by each of the following variables: sex, comorbidity count, educational level, and obesity.
This project was approved by the Partners HealthCare Institutional Review Board.
RESULTS
Description of the Study Cohorts
Of the community-dwelling Medicare beneficiaries aged ≥65 in the MCBS survey sample, 545 (5.4%) met our criteria for inclusion in the knee OA cohort. More than 97% of the knee OA cohort had ICD-9 diagnosis codes for knee OA and the remaining 2.4% (N = 13) had codes for knee pain accompanied by codes for OA at unspecified, multiple, or other-specified sites. The age- and sex-matched knee OA and OA-free cohorts had similar racial distributions. However, the knee OA cohort had higher rates of obesity, number of comorbidities, and functional limitation (Table 2).
TABLE 2.
Cohort Characteristics*
| Parameter | Knee OA (N = 545) |
OA-Free (N = 1090) |
|---|---|---|
| Age (mean, SE) | 76.1 (0.25) | 76.1 (0.17) |
| N (%) | N (%) | |
| Female | 379 (69.3) | 758 (70.6) |
| Race | ||
| White | 472 (87.1) | 951 (87.2) |
| Black | 53 (9.0) | 83 (7.4) |
| Other | 20 (3.8) | 55 (5.3) |
| Obesity (BMI ≥30 kg/m2) | 194 (36.9) | 208 (19.9) |
| Comorbidity count | ||
| 0 | 29 (4.9) | 236 (22.0) |
| 1 | 146 (26.0) | 369 (34.9) |
| 2 | 174 (32.1) | 252 (22.8) |
| ≥3 | 196 (37.0) | 233 (20.4) |
| Functional limitation | 245 (41.9) | 316 (25.9) |
| Education ≤ high school | 170 (29.3) | 330 (27.9) |
| Working at a job or business | 42 (9.0) | 106 (11.8) |
P < 0.0001 for obesity, comorbidity count, and functional limitation; P > 0.15 for all other parameters.
OA indicates osteoarthritis; SE, standard error; BMI, body mass index.
Utilization of Health Care Services ED Visits
The knee OA cohort averaged 0.8 annual ED visits, and 36% visited the ED at least once in the year while the OA-free cohort averaged 0.4 ED visits and 27% visited the ED at least once in the year. Among those visiting the ED in 2003, the knee OA cohort averaged 0.8 more visits than the OA-free cohort (2.3 vs. 1.5 visits). Univariate analyses showed that subjects in the knee OA cohort were more likely to visit the ED than persons in the OA-free cohort (odds ratio [OR] = 1.5, 95% confidence interval [CI]: 1.3, 1.8) (Table 3). In multivariable models controlling for knee OA status, comorbidities, obesity, functional status, race, education, and working status, the independent predictors of visiting the ED at least once within the year included ≥2 comorbidities (OR = 3.0, 95% CI: 2.5, 3.7), functional limitation (OR = 2.1, 95% CI: 1.7, 2.6), and high school or less education (OR = 1.3, 95% CI: 1.1, 1.6) (Table 3). After adjusting for covariates, the data did not provide evidence that knee OA was associated with higher likelihood of ED use (OR = 1.1, 95% CI: 0.9, 1.3). A sensitivity analysis of 483 knee OA patients, and 966 sex- and age-matched controls, which excluded patients who received a lower extremity joint replacement during the year of study, yielded similar results, and suggested no association between knee OA status and ED utilization (OR = 1.2, 95% CI: 0.9, 1.5). The impact of knee OA on ED visits differed for men and women. Men with knee OA were about 76% more likely to be seen in an ED compared with those without OA, but such an effect of knee OA was not observed among women (P value for interaction 0.02).
TABLE 3.
Unadjusted and Adjusted Analysis of Emergency Department (ED) Visits and Inpatient Hospital Stays in the 2003 Medicare Current Beneficiary Survey (MCBS)
| Any Emergency Department Visit | Any Inpatient Hospital Stay | |||||||
|---|---|---|---|---|---|---|---|---|
| Covariates | Any Visit (%) | Mean* | Unadjusted OR (CI†) |
Adjusted ‡ OR (CI) |
Any Visit (%) | Mean* | Unadjusted OR (CI†) |
Adjusted‡ OR (CI) |
| Cohort | ||||||||
| OA-free | 26.8 | 1.5 | 1.0 | 1.0 | 19.9 | 1.5 | 1.0 | 1.0 |
| Knee OA | 36.2 | 2.3 | 1.55 (1.30, 1.84)§ | 1.11 (0.92, 1.35) | 32.2 | 1.8 | 1.91 (1.57, 2.32)§ | 1.28 (1.03, 1.60)§ |
| Comorbidities | ||||||||
| 0–1 | 17.2 | 1.2 | 1.0 | 1.0 | 9.3 | 1.2 | 1.0 | 1.0 |
| >2 | 41.8 | 2.0 | 3.47 (2.87, 4.20)§ | 2.99 (2.46, 3.65)§ | 37.8 | 1.7 | 5.95 (4.75, 7.46)§ | 4.98 (3.92, 6.33)§ |
| Obesity | ||||||||
| Not obese | 29.2 | 1.7 | 1.0 | 1.0 | 23.5 | 1.6 | 1.0 | 1.0 |
| Obese | 32.0 | 2.0 | 1.14 (0.92, 1.40) | 0.84 (0.67, 1.06) | 25.7 | 1.6 | 1.13 (0.92, 1.39) | 0.73 (0.56, 0.96)§ |
| Functional status | ||||||||
| Not limited | 23.0 | 1.6 | 1.0 | 1.0 | 16.8 | 1.5 | 1.0 | 1.0 |
| Limited | 45.2 | 2.1 | 2.76 (2.28, 3.33)§ | 2.12 (1.72, 2.61)§ | 39.9 | 1.7 | 3.28 (2.69, 3.99)§ | 2.49 (2.02, 3.07)§ |
| Race | ||||||||
| White | 29.7 | 1.7 | 1.0 | 1.0 | 24.0 | 1.6 | 1.0 | 1.0 |
| Nonwhite | 31.9 | 2.8 | 1.11 (0.80, 1.54) | 0.93 (0.64, 1.34) | 24.8 | 1.9 | 1.05 (0.79, 1.40) | 0.86 (0.61, 1.20) |
| Education | ||||||||
| > High school | 27.0 | 1.7 | 1.0 | 1.0 | 21.3 | 1.6 | 1.0 | 1.0 |
| < High school | 37.2 | 2.0 | 1.60 (1.35, 1.90)§ | 1.32 (1.11, 1.59)§ | 31.1 | 1.6 | 1.66 (1.36, 2.03)§ | 1.34 (1.06, 1.70)§ |
| Working status | ||||||||
| Not working | 30.8 | 1.8 | 1.0 | 1.0 | 24.8 | 1.6 | 1.0 | 1.0 |
| Working | 21.7 | 1.6 | 0.62 (0.43, 0.90)§ | 0.88 (0.58, 1.32) | 17.7 | 1.7 | 0.66 (0.44, 0.98)§ | 1.02 (0.68, 1.53) |
Mean of those with any ED visit or inpatient hospital stay in 2003.
CI = 95% confidence interval.
Adjusted models predict resource utilization from logistic regression models using all covariates in table.
Significant odds ratios.
OR indicates odds ratio; OA, osteoarthritis.
Hospital Stays
The knee OA cohort averaged more hospitalizations per person-year than the OA-free cohort (0.6 vs. 0.3), but had a shorter mean length of stay (5.3 vs. 6.7 days for OA-free). About 32% of the knee OA cohort was hospitalized at least once, contrasted with 20% of the OA-free cohort (Table 3). Among those patients with any hospital stays in 2003, the knee OA cohort averaged 0.3 more hospital stays than OA-free patients. In multivariable analysis, being in the knee OA cohort remained associated with a higher likelihood of having at least one annual hospitalization, although the effect was greatly diminished by covariate adjustment (OR = 1.3, 95% CI: 1.0, 1.6). Having ≥2 comorbidities (OR = 5.0, 95% CI: 3.9, 6.3) and functional limitation (OR = 2.5, 95% CI: 2.0, 3.1) continued to be strongly associated with hospitalization. Educational level of high school or less was also associated with a higher probability of hospitalization (OR = 1.3, 95% CI: 1.1, 1.7), whereas obesity was associated with a lower probability of hospital stay (OR = 0.7, 95% CI: 0.6, 1.0). Our data did not suggest that the impact of knee OA on hospital inpatient utilization differed between men and women.
In a sensitivity analysis that excluded patients who had a lower extremity joint replacement during the study year, membership in the knee OA cohort was no longer a significant predictor of hospitalization (OR=0.8, 95% CI: 0.6, 1.0). Again, the presence of ≥2 comorbidities and functional limitation had a substantial effect on hospitalizations, (OR = 4.5, 95% CI: 3.3, 6.0 and OR = 2.2, 95% CI: 1.7, 2.9, respectively).
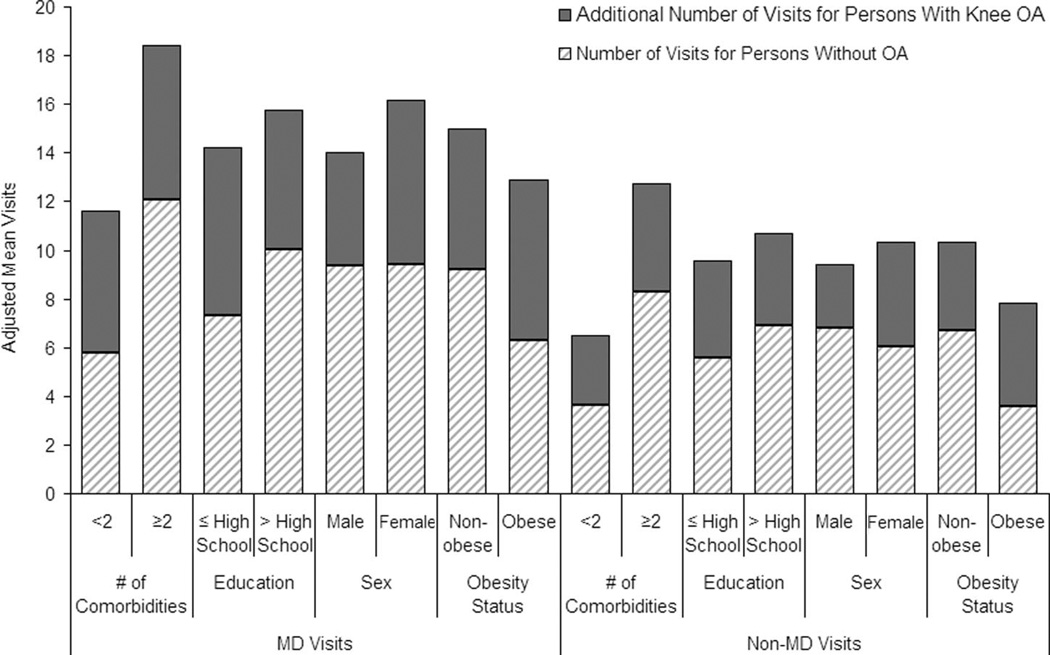
Ambulatory Services
The knee OA cohort averaged 18.4 MD visits and 13.3 non-MD visits per person-year, whereas the OA-free cohort averaged 10.0 MD visits and 7.9 non-MD visits (Table 4). Knee OA status and comorbidity count were the predominant factors affecting annual ambulatory utilization in univariate analyses. Subjects with ≥2 comorbidities had over 2-fold more MD visits (17.4 vs. 7.9) and non-MD visits (13.3 vs. 5.8) than those with <2 comorbidities. The differences in utilization by knee OA status and comorbidity count were statistically significant at the P < 0.0001 level. In multivariable analysis controlling for all covariates listed in Table 4, knee OA status remained strongly associated with both measures of ambulatory utilization (6.0 more annual adjusted mean visits to physicians, 3.8 more annual adjusted mean visits to nonphysicians, P < 0.0001). Having ≥2 comorbidities also was an important predictor of ambulatory visits (8.0 more annual adjusted mean MD visits, 6.7 more annual adjusted mean non-MD, P < 0.0001). A more modest predictor of increased MD visits was education above high school (1.7 more annual adjusted mean visits, P = 0.007) (Table 4); weaker predictors of more non-MD visits were white race (1.5 more annual adjusted mean visits, P = 0.01), not working (1.5 more annual visits, P = 0.02), and education above high school (1.2 more annual adjusted mean visits, P = 0.02). Females in the knee OA cohort had 6.7 more annual MD visits than OA-free females, whereas males with knee OA had 4.7 more annual MD visits than OA-free males (P value for interaction 0.008). Similarly, females in the knee OA cohort had 4.3 more non-MD visits than OA-free females, whereas males with knee OA had 2.6 more non-MD visits than OA-free males (P value for interaction 0.02). Four separate stratified multivariable analyses were done; 1 stratified by comorbidity count, 1 by educational level, 1 by sex, and 1 by obesity. These analyses showed that the population of patients with knee OA visited physicians and nonphysicians substantially more than OA-free patients in all comorbidity count, educational level, sex, and obesity status strata (Fig. 1). Each of these utilization differences between knee OA and OA-free patients was significant at P ≤ 0.0003.
TABLE 4.
Unadjusted and Adjusted* Mean Annual Ambulatory Resource Utilization
| Annual Physician Visits | Annual Non-Physician Visits | |||||||
|---|---|---|---|---|---|---|---|---|
| Raw | Adjusted* | Raw | Adjusted* | |||||
| Covariates | Mean | P | Mean | P | Mean | P | Mean | P |
| Cohort | ||||||||
| OA-free | 10.03 | <0.0001 | 9.81 | <0.0001 | 7.88 | <0.0001 | 6.80 | <0.0001 |
| Knee OA | 18.39 | 15.85 | 13.34 | 10.58 | ||||
| Comorbidities | ||||||||
| 0–1 | 7.90 | <0.0001 | 8.85 | <0.0001 | 5.85 | <0.0001 | 5.34 | <0.0001 |
| >2 | 17.40 | 16.82 | 13.29 | 12.03 | ||||
| Obesity | ||||||||
| Not obese | 12.01 | 0.0002 | 12.54 | 0.45 | 9.30 | 0.002 | 8.74 | 0.83 |
| Obese | 15.17 | 13.12 | 10.88 | 8.63 | ||||
| Functional status | ||||||||
| Not limited | 11.73 | <0.0001 | 12.40 | 0.19 | 9.18 | 0.0005 | 8.89 | 0.31 |
| Limited | 15.22 | 13.27 | 10.85 | 8.48 | ||||
| race | ||||||||
| White | 12.97 | 0.14 | 13.49 | 0.05 | 9.89 | 0.02 | 9.46 | 0.01 |
| Nonwhite | 11.70 | 12.18 | 8.30 | 7.92 | ||||
| education | ||||||||
| > High school | 13.07 | 0.17 | 13.69 | 0.007 | 9.96 | 0.11 | 9.30 | 0.02 |
| < High school | 12.14 | 11.98 | 9.11 | 8.08 | ||||
| Working status | ||||||||
| Not working | 13.07 | 0.02 | 13.22 | 0.36 | 9.95 | 0.0006 | 9.42 | 0.02 |
| Working | 10.98 | 12.45 | 7.73 | 7.95 | ||||
Means are adjusted by all covariates in the table.
OA indicates osteoarthritis.
FIGURE 1.
MD and Non-MD Visits in 2003 Medicare Beneficiaries: Knee OA and OA-free Populations. The darker segments of bars represent an additional utilization of MD/non-MD visits by those with knee OA. All models include comorbidity count, age, sex, race, education, obesity, functional status, and working status. All comparisons between knee OA and OA-free cohorts within comorbidity count, educational level, sex, and obesity categories are significant at a level of P = 0.0003.
DISCUSSION
This study examined health care utilization patterns among knee OA patients in a national population sample. We found that knee OA patients had significantly more adjusted mean MD and non-MD visits than OA-free patients. This excess usage (6.0 visits to physicians and 3.8 visits to nonphysician providers) is attributable to knee OA, independent of the effects of comorbidity, obesity, functional status, and other patient characteristics.
After controlling for comorbidity, we did not find that knee OA contributed to excess utilization of ED resources, but we found that knee OA patients were about 30% more likely to have a hospital stay than OA-free subjects. Since this association was not found in sensitivity analyses, which excluded patients who had a lower extremity joint replacement during the study year, it appears that the increase in hospital stays in knee OA patients may be attributed to joint replacement surgeries. Yelin and Felts32 found that among patients with OA, the rate of hospitalization is 50% more for persons with at least one more comorbid condition and that more than 91% of the hospitalizations in those with OA occurred among those with at least one additional comorbidity. Thus, the higher rates of inpatient utilization previously reported for OA patients24 are probably due in part to comorbid conditions.
Whereas previous research has documented significant utilization among OA patients, this study is the first to our knowledge to examine utilization attributable to knee OA in a national population sample. Nationally representative data are critical for projecting accurate estimates of utilization for the US population and informing health care policy.
Most prior studies on utilization and/or cost in OA have studied European populations,18–21 a state-wide Medicare program,22 community-based cohorts,14,15,22 HMO populations,12,13,16,23,24 and VA populations.25 However, there are 2 studies of OA in national population samples that report findings on ambulatory utilization consistent with ours.33,34 Kramer et al found that OA patients had 10.9 physician visits on average in 1 year compared with 6.5 for the general population, or an excess of 4.4 MD visits for OA patients.33 This observation compares well with the 6.0 excess annual MD visits by knee OA patients observed in the present study.
In addition to general changes in health care from 1989 to 2003, distinctive findings in our study may reflect our focus on knee OA rather than OA of any joint, as in Kramer et al.33 Prior studies examining OA without reference to joint may have introduced heterogeneity in estimation of health care utilization. For example, utilization for hand and knee OA may differ because of differences in treatment protocols and disability consequences of upper extremity and lower extremity OA.
Whereas previous studies have documented significant outpatient utilization by OA patients, the question remains whether this increased utilization is due to OA specifically or to potentially confounding factors, such as comorbidity, functional limitation, and obesity.9,10 Dunlop et al address this question in the context of arthritis and rheumatic conditions generally.26 Their study observed increased outpatient utilization by arthritis patients as compared with nonarthritic controls after controlling for demographics and comorbid conditions.
The present study adds to the literature by addressing the question of health care utilization attributable to knee OA. Similar to the work of Dunlop et al performed in arthritis of diverse etiologies, we observed an independent effect of knee OA on ambulatory utilization. Our findings demonstrate that although persons with knee OA are more likely to have concomitant comorbidities and to be obese, the excess ambulatory health service utilization is not confounded by these factors. The increased utilization of MD and non-MD visits observed in the knee OA cohort persisted after controlling for comorbidity, obesity, functional limitation, and demographic characteristics and on stratification by sex, comorbidity, obesity, and education.
The present study has important differences from the work of Dunlop et al.26 Our study used Medicare billing data rather than patient self-report questionnaires and interviews. Medicare data files, with codes for diagnosis, procedure, and provider type, allow more certainty about diagnoses and utilization and eliminate the risk of reporting bias. Also, our focus on knee OA reduces the heterogeneity inherent in a general arthritis outcome. In contrast to Dunlop et al, we were able to quantify resource utilization, allowing us to assess the magnitude of the effect of knee OA on health care utilization. Whereas studies in primary care settings systematically exclude patients who visit orthopedists or other specialists directly,18,20 our study uses survey data that includes such patients, irrespective of provider type. Furthermore, the components of utilization we measured represent a comprehensive overview of medical resources.
The knee OA and OA-free cohorts reported in this manuscript consist of those seeking care, which leads to an undercounting of mild disease. This may account for the lower prevalence of knee OA found in this study compared with that reported in national surveys. We examined several strategies for increasing sensitivity, but all required compromise in specificity and, therefore, in positive predictive value of the algorithm for identifying knee OA cases. The trade-off between sensitivity and specificity of claims-based algorithms is well described.35 We chose to optimize specificity over sensitivity to maximize correct classification in both knee OA and OA-free cohorts. Because of substantial discordance between survey and claims data, we were unable to incorporate survey responses into the knee OA case definition; the reliance on claims likely led to a sample with more severe OA because a claim implies seeking medical attention for the problem.
Whereas the use of Medicare insurance claims brings certain strengths, these data source also has limitations. The analysis did not include aspects of utilization not reimbursed by Medicare, such as routine physical examinations, screening tests, and alternative therapies. Our utilization estimates may be low, as suggested by Harrold et al,36 who found that the use of data with OA diagnosis validated by medical chart review leads to substantially higher estimates of health utilization by OA patients. Furthermore, we examined all visits for knee OA patients and did not distinguish between OA-related and unrelated utilization. Consequently, some medical care may have been for comorbid conditions causally unrelated to OA. Although we recognize that knee OA can be a prominent disabling condition in younger ages, the nature of the data we used for the current analysis (Medicare claims) limits generalizability of our findings to populations with knee OA aged ≥65. Reason for the visit could offer important additional insights into health care utilization patterns among persons with knee OA, but this information was not available in Medicare claims. Our analysis focused on comparing health care utilization in a knee OA cohort with the OA-free population. Comparing different OA sites (eg, hands vs. hips vs. knees) was outside the scope of this article.
This first national, population-based study of health care utilization in knee OA documents considerable ambulatory usage attributable to knee OA, independent of the effects of comorbidity, functional limitation, obesity, and patient demographic characteristics. Furthermore, our results suggest that the additional inpatient health resource utilization previously reported as due to knee OA can be attributed to the number of comorbidities rather than knee OA per se, except in the case of hospital stays for joint replacement surgery. Nationally representative utilization data are critical for informing health care policy, particularly in the allocation of limited funds in the current environment of rising health care costs. Our finding of 9.8 excess ambulatory (MD and non-MD) visits per year attributable to knee OA suggests that OA treatment and prevention innovations represent opportunities to reduce a significant burden on the US health care system.
Acknowledgments
Supported in part by NIH/NIAMS R01 AR053112, P60 AR 47782, NIH K24 AR 02123 and Arthritis Foundation Innovative Research Grant (to E.L.).
REFERENCES
- 1.Dillon CF, Rasch EK, Gu Q, et al. Prevalence of knee osteoarthritis in the United States: arthritis data from the Third National Health and Nutrition Examination Survey 1991–94. J Rheumatol. 2006;33:2271–2279. [PubMed] [Google Scholar]
- 2.Breedveld FC. Osteoarthritis—the impact of a serious disease. Rheumatology (Oxford) 2004;43 suppl 1:i4–i8. doi: 10.1093/rheumatology/keh102. [DOI] [PubMed] [Google Scholar]
- 3.Guccione AA, Felson DT, Anderson JJ, et al. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. Am J Public Health. 1994;84:351–358. doi: 10.2105/ajph.84.3.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reginster JY. The prevalence and burden of arthritis. Rheumatology (Oxford) 2002;41 suppl 1:3–6. [PubMed] [Google Scholar]
- 5.Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58:26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ettinger WH, Davis MA, Neuhaus JM, et al. Long-term physical functioning in persons with knee osteoarthritis from NHANES. I: effects of comorbid medical conditions. J Clin Epidemiol. 1994;47:809–815. doi: 10.1016/0895-4356(94)90178-3. [DOI] [PubMed] [Google Scholar]
- 7.Coggon D, Reading I, Croft P, et al. Knee osteoarthritis and obesity. Int J Obes Relat Metab Disord. 2001;25:622–627. doi: 10.1038/sj.ijo.0801585. [DOI] [PubMed] [Google Scholar]
- 8.Axford J, Heron C, Ross F, et al. Management of knee osteoarthritis in primary care: pain and depression are the major obstacles. J Psychosom Res. 2008;64:461–467. doi: 10.1016/j.jpsychores.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 9.Kadam UT, Jordan K, Croft PR. Clinical comorbidity in patients with osteoarthritis: a case-control study of general practice consulters in England and Wales. Ann Rheum Dis. 2004;63:408–414. doi: 10.1136/ard.2003.007526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gabriel SE, Crowson CS, O’Fallon WM. Comorbidity in arthritis. J Rheumatol. 1999;26:2475–2479. [PubMed] [Google Scholar]
- 11.Gupta S, Hawker G, Laporte A, et al. The economic burden of disabling hip and knee osteoarthritis (OA) from the perspective of individuals living with this condition. Rheumatology. 2005;44:1531–1537. doi: 10.1093/rheumatology/kei049. [DOI] [PubMed] [Google Scholar]
- 12.Lanes SF, Lanza LL, Radensky PW, et al. Resource utilization and cost of care for rheumatoid arthritis and osteoarthritis in a managed care setting: the importance of drug and surgery costs. Arthritis Rheum. 1997;40:1475–1481. doi: 10.1002/art.1780400816. [DOI] [PubMed] [Google Scholar]
- 13.Lee DW, Meyer JW, Clouse J. Implications of controlling for comorbid conditions in cost-of-illness estimates: a case study of osteoarthritis from a managed care system perspective. Value Health. 2001;4:329–334. doi: 10.1046/j.1524-4733.2001.44012.x. [DOI] [PubMed] [Google Scholar]
- 14.Gabriel SE, Crowson CS, Campion ME, et al. Direct medical costs unique to people with arthritis. J Rheumatol. 1997;24:719–725. [PubMed] [Google Scholar]
- 15.Gabriel SE, Crowson CS, Campion ME, et al. Indirect and nonmedical costs among people with rheumatoid arthritis and osteoarthritis compared with nonarthritic controls. J Rheumatol. 1997;24:43–48. [PubMed] [Google Scholar]
- 16.MacLean CH, Knight K, Paulus H, et al. Costs attributable to osteoarthritis. J Rheumatol. 1998;25:2213–2218. [PubMed] [Google Scholar]
- 17.Kotlarz H, Gunnarsson CL, Fang H, et al. Insurer and out-of-pocket costs of osteoarthritis in the US. Evidence from national survey data. Arthritis Rheum. 2009;60:3546–3553. doi: 10.1002/art.24984. [DOI] [PubMed] [Google Scholar]
- 18.Rosemann T, Joos S, Szecsenyi J, et al. Health service utilization patterns of primary care patients with osteoarthritis. BMC Health Serv Res. 2007;7:169. doi: 10.1186/1472-6963-7-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rosemann T, Gensichen J, Sauer N, et al. The impact of concomitant depression on quality of life and health service utilisation in patients with osteoarthritis. Rheumatol Int. 2007;27:859–863. doi: 10.1007/s00296-007-0309-6. [DOI] [PubMed] [Google Scholar]
- 20.Rosemann T, Grol R, Herman K, et al. Association between obesity, quality of life, physical activity and health service utilization in primary care patients with osteoarthritis. Int J Behav Nutr Phys Act. 2008;5:4. doi: 10.1186/1479-5868-5-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ethgen O, Kahler KH, Kong SX, et al. The effect of health related quality of life on reported use of health care resources in patients with osteoarthritis and rheumatoid arthritis: a longitudinal analysis. J Rheumatol. 2002;29:1147–1155. [PubMed] [Google Scholar]
- 22.Dominick KL, Ahern FM, Gold CH, et al. Health-related quality of life and health service use among older adults with osteoarthritis. Arthritis Rheum. 2004;51:326–331. doi: 10.1002/art.20390. [DOI] [PubMed] [Google Scholar]
- 23.Cronan TA, Shaw WS, Gallagher RA, et al. Predicting health care use among older osteoarthritis patients in an HMO. Arthritis Care Res. 1995;8:66–72. doi: 10.1002/art.1790080203. [DOI] [PubMed] [Google Scholar]
- 24.Mapel DW, Shainline M, Paez K, et al. Hospital, pharmacy, and outpatient costs for osteoarthritis and chronic back pain. J Rheumatol. 2004;31:573–583. [PubMed] [Google Scholar]
- 25.Dominick KL, Dudley TK, Coffman CJ, et al. Comparison of three comorbidity measures for predicting health service use in patients with osteoarthritis. Arthritis Rheum. 2005;53:666–672. doi: 10.1002/art.21440. [DOI] [PubMed] [Google Scholar]
- 26.Dunlop DD, Manheim LM, Song J, et al. Health care utilization among older adults with arthritis. Arthritis Rheum. 2003;49:164–171. doi: 10.1002/art.11003. [DOI] [PubMed] [Google Scholar]
- 27.Adler GS. A profile of the Medicare Current Beneficiary Survey. Health Care Financ Rev. 1994;15:153–163. [PMC free article] [PubMed] [Google Scholar]
- 28.Sugarman JR, Reiber GE, Baumgardner G, et al. Use of the therapeutic footwear benefit among diabetic medicare beneficiaries in three states, 1995. Diabetes Care. 1998;21:777–781. doi: 10.2337/diacare.21.5.777. [DOI] [PubMed] [Google Scholar]
- 29.WHO. Global Burden of Disease (GBD) 2000: Version 2 Estimates. [Accessed August 20, 2009];2002 Available at: http://www.who.int/healthinfo/global_burden_disease/estimates_regional_2000_v2/en/index.html.
- 30.Roche JJ, Wenn RT, Sahota O, et al. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331:1374. doi: 10.1136/bmj.38643.663843.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.SAS. Statistical Analysis System. Version 9.1.3. Cary, NC: SAS Institute; pp. 2002–2004. [Google Scholar]
- 32.Yelin EH, Felts WR. A summary of the impact of musculoskeletal conditions in the United States. Arthritis Rheum. 1990;33:750–755. doi: 10.1002/art.1780330520. [DOI] [PubMed] [Google Scholar]
- 33.Kramer JS, Yelin EH, Epstein WV. Social and economic impacts of four musculoskeletal conditions. A study using national community-based data. Arthritis Rheum. 1983;26:901–907. doi: 10.1002/art.1780260712. [DOI] [PubMed] [Google Scholar]
- 34.Felts W, Yelin E. The economic impact of the rheumatic diseases in the United States. J Rheumatol. 1989;16:867–884. [PubMed] [Google Scholar]
- 35.Rector TS, Wickstrom SL, Shah M, et al. Specificity and sensitivity of claims-based algorithms for identifying members of Medicare+Choice health plans that have chronic medical conditions. Health Serv Res. 2004;39:1839–1858. doi: 10.1111/j.1475-6773.2004.00321.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Harrold LR, Yood RA, Straus W, et al. Challenges of estimating health service utilization for osteoarthritis patients on a population level. J Rheumatol. 2002;29:1931–1936. [PubMed] [Google Scholar]