Abstract
Purpose
Bangerter filters are designed to cause progressive degradation of distance optotype acuity to predicted levels (density label indicating expected decimal acuity) and are used to treat amblyopia and diplopia. Nevertheless, there are few data reporting induced acuity deficits. We investigated the effect of Bangerter filters on distance and near optotype acuity, vernier acuity, and contrast sensitivity.
Methods
Fifteen subjects with best corrected optotype acuity of at least 20/25 in each eye were blurred sequentially in one eye with 7 Bangerter filters (densities <0.1, 0.1, 0.2, 0.3, 0.4, 0.8, 1.0). At each filter level distance and near optotype acuity (LogMAR), vernier acuity and contrast sensitivity were assessed. Mean log acuities were compared using generalized estimating equation methods.
Results
The 1.0, 0.8, and 0.4 filters degraded distance optotype acuity to a similar degree (mean 0.22, 0.23, and 0.28 logMAR). Subsequent filters progressively degraded acuity: 0.44, 0.57, 0.93, 1.69 logMAR. Near optotype acuity was reduced in a similar pattern. Vernier acuity was minimally degraded by 1.0, 0.8, and 0.4 filters (18, 19, and 20 arcsec), followed by progressive degradation with subsequent filters (31, 35, 113, and 387 arcsec). Contrast sensitivity was minimally reduced with filters 1.0 through 0.2, and then precipitously degraded with 0.1 and <0.1 filters.
Conclusion
The 1.0, 0.8, and 0.4 filters cause similar, minimal degradation of distance and near optotype, and vernier acuity, whereas subsequent filters cause progressive degradation. Contrast sensitivity is not markedly reduced until the 0.1 filter. These results have important implications for using Bangerter filters therapeutically.
Introduction
Bangerter filters are designed to induce mild to moderate degradations in optotype visual acuity.1, 2 Clinically, Bangerter filters are used in the treatment of diplopia2, 3 and amblyopia.4, 5 Nevertheless, there are few data reporting the degree of visual degradation achieved using Bangerter filters or their effect on other measures of visual functions, such as vernier acuity or contrast sensitivity. As it has been shown that amblyopia can differentially degrade optotype acuity, vernier acuity, and contrast sensitivity,6–9 it may be important to identify how Bangerter filters affect individual modalities of visual function. The purpose of this study was to measure the quantitative effect of Bangerter filters on optotype acuity, vernier acuity, and contrast sensitivity.
Subjects and Methods
Subjects
Fifteen subjects aged 22 to 35 (median 24) years were recruited. Ten (67%) of 15 were male and 8 (53%) were Caucasian. All subjects had best corrected visual acuity of 20/25 Snellen or better in each eye, stereoacuity of at least 40 seconds of arc with the Titmus test, orthotropia at distance and near by the simultaneous prism and cover test (SPCT), and no prior history of strabismus or other eye disease. Informed consent was obtained from each study participant. The study was approved by the institutional review board, and data were collected in a manner compliant with the American Health Insurance Portability and Accountability Act.
Methods
Bangerter Filters
Bangerter filters (Fresnel Prism and Lens Co., LLC, Eden Prairie, MN) were applied with water (as recommended by the manufacturer) to the inner surface of plano trial lenses. Seven filter densities were selected: <0.1, 0.1, 0.2, 0.3, 0.4, 0.8, and 1.0 (from most to least dense). The 0.6 filter was not selected, as initial pilot testing showed it did not degrade optotype acuity differently from the 0.8 filter. The same filters were used for all subjects. Mounted filters were placed over one eye, either in trial frames or using Halberg clips over the subject’s spectacles. Testing order was from the most dense (<0.1) to the least dense (1.0) filter. Patients in our study were instructed to not search for a clearer part of the filter. At each filter density, monocular optotype acuity, vernier acuity, and contrast sensitivity were tested for the eye fitted with the filter. At the end of testing, baseline distance optotype acuity (no filter) was assessed monocularly (each eye). Both eyes were tested for each subject, the second eye being tested at a subsequent visit. Testing order was randomized by eye dominance, to determine whether the dominant or non-dominant eye should be tested first. Eye dominance was determined by the distance hole-in-the-card test.
Measurement of Distance Optotype acuity
For all 15 subjects (30 eyes), distance optotype acuity was measured using the electronic M&S Smart System II PC Plus, displaying single letters, with crowding bars, in a random sequence. At each Bangerter filter level, testing consisted of a screening phase followed by threshold determination.10, 11 During the screening phase, one letter was presented at each logMAR step (starting at 20/400 (1.3 logMAR)) until there was an incorrect response. Threshold determination began two logMAR steps above the last correct ‘screening’ response, with 3 of 5 correct responses required to pass each level. The best level passed was recorded as the subject’s distance optotype acuity. If the subject could not identify the 20/400 letter, the subject was moved up to a quarter of the testing distance so that the 20/400 letter subtended 20/1600 (1.9 logMAR). Testing progressed in decreasing 0.1 logMAR steps from that point.
Measurement of Near Optotype acuity
Near optotype acuity testing was added to the protocol after commencement of the study and therefore was only measured in 10 of 15 subjects (13 of 20 eyes). The Near Visual Acuity Test (Lighthouse, International, New York, NY) was used, at a distance of 40 cm. Near optotype acuity measurements were converted to logMAR values based on the test distance and the M value.
Measurement of Vernier acuity
Vernier acuity was measured in all subjects (30 eyes) using vernier offset patterns mounted on cards measuring 56 × 24 cm. Our method was adapted from the protocol described by Holmes and Archer,12 and used three cards with square wave gratings of 0.5 cycles/degree, with offsets of 3.72 mm, 0.93 mm, and 0.23 mm. Each card consisted of two gratings: one with offsets, and one without. The location of the grating with the offset was randomized. Working distances were calculated to subtend angles ranging from 6 seconds of arc to 1920 seconds of arc in logMAR steps (−1.0 to 1.5 logMAR). At each Bangerter filter level, testing started with an initial screening phase, displaying cards in 0.3 logMAR (1 octave) steps until there was an incorrect response. Guessing was discouraged. Threshold testing started at the level of the last correct response and proceeded in 0.1 logMAR steps, requiring 4 of 4 correct responses to pass.
Measurement of Contrast Sensitivity
Contrast sensitivity was measured in all subjects (30 eyes) using Pelli-Robson optotype based contrast sensitivity charts (Clement Clarke International, Harlow, UK), viewed under recommended lighting conditions (between 198–397 Lux) at the standard 1 m distance. Two charts were used and alternated each time the filter was changed. Two of 3 correct responses at each contrast level was considered a pass and thresholds were recorded in log units.
Statistical Analysis
Data were converted to log units for analysis. No systematic differences were found between data from right and left eyes, and therefore data from right and left eyes were combined for analysis, and generalized linear models utilizing generalized estimating equation (GEE) methods were used to account for correlation between the eyes. For all four visual function testing modalities, the mean acuity obtained at each Bangerter filter level was calculated. Paired comparisons of mean acuities were made in a step-wise manner for adjacent filters (including no filter compared to 1.0 filter) using GEE methods. To enable comparison of modalities, each measure of visual function was expressed as a log change from baseline for each filter step. Comparisons of log change from baseline were made between modalities at each filter step using GEE methods with contrasting statements to account for all repeated factors (subjects, eyes, and testing modality). For comparison of distance and near optotype acuities, paired comparisons were made using GEE methods of the eyes from subjects from whom both measures were obtained.
Results
Distance optotype acuity
Distance visual acuity was significantly reduced from baseline for all Bangerter filter densities (P<0.0001 for all comparisons, Figure 1A, supplemental table available at www.jaapos.com). Comparing filters step-wise, mean distance optotype acuity with the least dense (1.0) filter showed a reduction from mean baseline acuity (0.22 logMAR versus −0.03 logMAR; P<0.0001, Figure 1A, supplemental table). Mean acuity with the 0.8 and 0.4 filters (0.23 and 0.28 logMAR respectively) did not show further, statistically significant degradation ( Figure 1A, supplemental table). Progressive degradation was achieved with each subsequent filter density, i.e. 0.3, 0.2, 0.1, and <0.1 filters (mean acuities: 0.44, 0.57, 0.93, and 1.69 logMAR respectively, P<0.0001 for each comparison).
Figure 1.
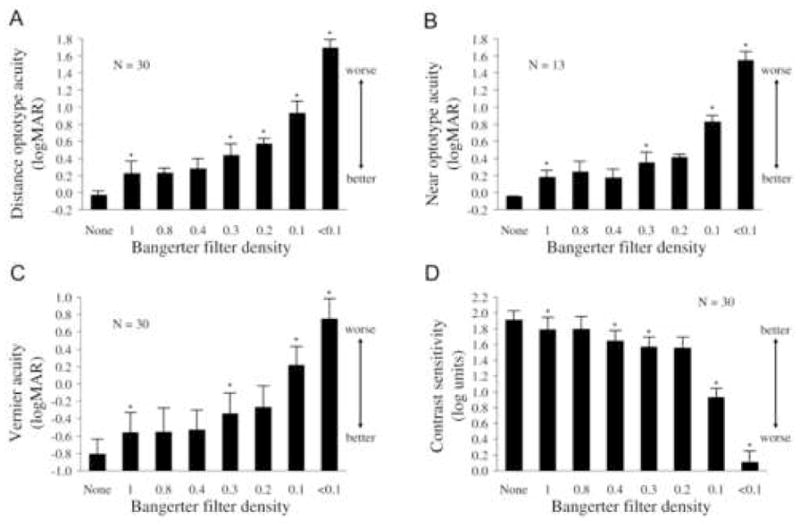
Visual function at each Bangerter filter strength. A) Distance optotype acuity; B) Near optotype acuity; C) Vernier acuity; D) Contrast sensitivity. Bars represent standard deviations and asterisks indicate where the visual acuity at that Bangerter strength was significantly (P<0.05) worse than at the previous Bangerter strength. All filters caused significant worsening for all modalities of visual acuity in comparison with wearing no filter.
Near optotype acuity
Near visual acuity for all Bangerter filter densities was significantly reduced from baseline values (P<0.0001 for all comparisons, Figure 1B, supplemental table). Comparing filters step-wise in the 10 subjects (13 eyes) with near optotype acuity measurements, mean near visual acuity with the least dense (1.0) filter was reduced from mean baseline acuity (0.18 logMAR versus −0.05 logMAR; P<0.0001, Figure 1B, supplemental table). Mean acuity with the 0.8 and 0.4 filters (0.24 and 0.17 logMAR respectively) did not show statistically significant further degradation (Figure 1B, supplemental table). There was further degradation in visual acuity with the 0.3 filter (mean 0.35 logMAR, P<0.0001), although not with the 0.2 filter (decrease from 0.35 to 0.41 logMAR). Progressive degradation was achieved with the 0.1, and <0.1 filters (mean acuities: 0.83 and 1.55 logMAR respectively, P<0.0001).
Comparison of near and distance optotype acuity
Overall, near acuity was degraded on average 0.075 logMAR less than distance acuity (± 0.063, P<0.0001). Comparing filters step-wise for the 13 eyes that had both distance and near optotype acuity measures, there were no significant differences between distance and near acuities without a filter or with the 1.0 or 0.8 density filters. The degradation of near optotype acuity followed a similar pattern to distance optotype acuity; however, near visual acuity was degraded to a lesser degree using the 0.4, 0.3, 0.2, 0.1 and <0.1 density Bangerter filters (P<0.02 for each filter density).
Vernier acuity
The degree of change from baseline was significant for all filter densities (P≤0.0002, Figure 1C, supplemental table). Comparing filters step-wise, mean vernier acuity was significantly reduced with the least dense filter (mean 18 seconds of arc (−0.56 LogMAR)) compared to baseline (10 seconds of arc (−0.81 LogMAR) P<0.0001, supplemental table). The 0.8 and 0.4 filters did not cause further significant reductions in mean vernier acuity (19 and 20 seconds of arc (−0.55 and −0.53 LogMAR) respectively). Progressive degradation was seen for subsequent filter densities, with the exception of the 0.2 filter (Figure 1C, supplemental table).
Contrast Sensitivity
Contrast sensitivity was significantly reduced from baseline values at all Bangerter filter densities (P<0.0001, Figure 1D, supplemental table). Comparing filters step-wise, contrast sensitivity was significantly reduced with the 1.0 filter (least dense, mean 1.79 log units) compared to baseline (mean 1.91 log units, P<0.0001), but no further degradation was seen with the 0.8 filter (1.80 log units). Although additional degradation was observed with each increase in filter density (with the exception of the 0.2 filter, Figure 1D, supplemental table), contrast sensitivity only precipitously degraded using the 0.1 and <0.1 filters.
Comparison of distance optotype acuity to vernier acuity and contrast sensitivity
The degree of change in acuity from baseline (in log units) for each Bangerter filter density was similar for distance optotype acuity and vernier acuity with all filters except for the <0.1 (most dense) filter, where distance optotype acuity was more degraded than vernier acuity (P<0.0001, Figure 2). As expected, vernier acuity thresholds were finer than distance optotype acuity thresholds, with an approximately 6.4-fold difference at all Bangerter filter levels. The pattern of degradation appeared to differ between the 3 modalities of visual acuity (Figure 2), with contrast sensitivity being relatively preserved until using the 0.1 and <0.1 filters.
Figure 2.
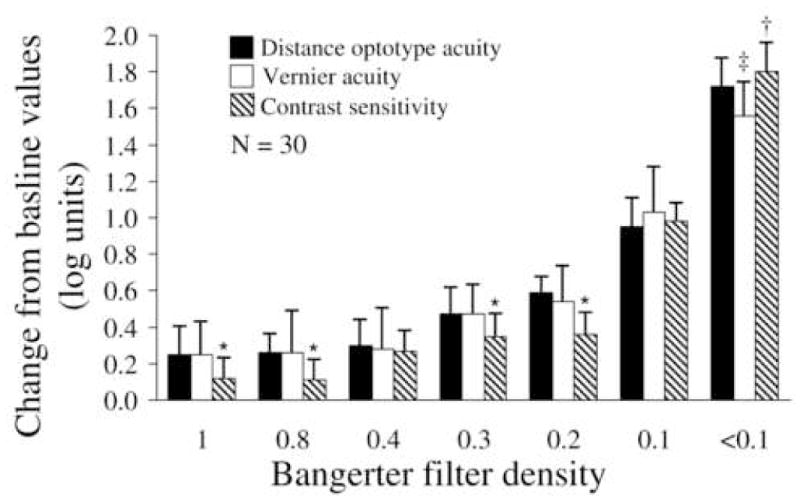
Comparison of distance optotype acuity, vernier acuity, and contrast sensitivity representing log unit change from baseline (no filter). Bars represent standard deviations. * = Contrast sensitivity mean change from baseline significantly less (P<0.05) than change in distance optotype acuity or vernier acuity. † = Contrast sensitivity mean change from baseline significantly greater (P<0.05) than change in mean distance optotype acuity or vernier acuity. ‡ = Vernier acuity mean change significantly less (P<0.0001) than distance optotype acuity.
Discussion
Degradation of visual acuity using Bangerter filters is seen in measures of near optotype acuity, vernier acuity, and contrast sensitivity, as well as in measures of distance optotype acuity. Contrast sensitivity showed less initial degradation than optotype or vernier acuity. Nevertheless, the degree of visual degradation found in our study was not consistent with the degree of degradation expected based on the labeling of the filters.
Bangerter filters are designed to produce diffuse image defocus that degrades optotype acuity to predicted levels,1 the filter label indicating the level of decimal acuity achievable when placed in front of an eye with normal acuity.2 Based on mean acuity values in visually normal adults, we found distance optotype visual acuity did not degrade according to the filter label for nearly all filter densities. Moreover, our data did not show a systematic deviation from expected values. For example, the least dense (1.0) filter designed to allow acuity of 1.0 decimal (20/20 Snellen equivalent) reduced acuity to a mean of 0.22 LogMAR (20/33 Snellen equivalent) in our study cohort. Conversely, the 0.4 filter, intended to degrade to 20/50 Snellen equivalent, only degraded optotype acuity to a mean of 0.28 LogMAR (20/38 Snellen equivalent), i.e. not significantly more than the 1.0 filter (supplemental table). It may therefore be that the full spectrum of filters will not be needed in clinical practice.
Results from previous studies of visual degradation using Bangerter filters are conflicting. A study by Mitsuyu and Zimmer13 found that Bangerter filters did indeed reduce acuity as predicted by the filter label, whereas a study by Janknecht and Funk14 found mean acuities did not correspond to predicted levels. The study by Janknecht and Funk,14 while confirming our finding that mean acuity levels are not consistent with the filter label, found markedly different acuities to those we report in this present study. It is possible that, due to the manufacturing process, filters of the same labeled density do not achieve comparable reductions in visual acuity or that density may not be uniform across the entire filter 3, 14 (The Reproducibility of Blur with a Bangerter Filter. Repka MX et al. Poster presentation, AAPOS 2006; Evaluation of Bangerter Filters as a Predictable Means of Blurring Vision. Bustos DE, Donahue SP. Poster presentation, ARVO 2006). Patients in our study were instructed to not search for a clearer part of the filter. In view of reported variability, it would seem prudent to confirm the level of acuity degradation achieved with a given filter before using it for treatment.
While Bangerter filters were designed to degrade optotype acuity, their effect on vernier acuity may be important, especially when used for the treatment of amblyopia. Levi and Klein6, 7 and others8, 15 have shown that vernier acuity is reduced more in strabismic amblyopia than in anisometropic amblyopia. Prior to our study we had speculated that Bangerter filters might differentially affect vernier and optotype acuity, but in fact we found similar levels of degradation (log units) (Figure 2). It would be interesting to study whether preferentially degrading one type of visual acuity might be advantageous in the treatment of different types of amblyopia. Nevertheless, Bangerter filters do not appear to selectively affect vernier or optotype acuity.
When analyzing the effect of Bangerter filters on near optotype acuity there was generally less degradation than that found at distance (supplemental table). As for distance acuity, the 0.8 and 0.4 filters did not appear to cause more degradation of acuity than the 1.0 filter. It is possible that part of this difference between distance and near acuity is due to the difference in the construct of the tests, but we did not observe a difference between distance and near acuity at baseline without the filter, or at low density filters. In the context of ambylopia treatment, the proportion of time spent doing distance versus near activities and the differential effect of Bangerter filters on distance optotype acuity may be worthy of further study.
Bangerter filters did not degrade contrast sensitivity as markedly as optotype or vernier acuity until using the more dense 0.1 and <0.1 filters. As illustrated using the 0.2 filter, the degree of change from baseline (log units) was significantly greater for optotype and vernier acuity, compared to contrast sensitivity (Figure 2). Contrast sensitivity became degraded to the same extent as optotype and vernier only when using the 0.1 filter, and then became preferentially degraded using the most dense (<0.1) filter. The degree of contrast sensitivity degradation found in this present study is similar to that reported by Smith and Hung,16 who studied the effect of the 0.4, 0.1 and <0.1 Bangerter filters on contrast sensitivity. Although only testing 3 filter densities, Smith and Hung16 also found contrast did not reduce by >1 log unit until using the <0.1 filter. This relative preservation of contrast sensitivity using lower density 1.0 to 0.2 density filters suggests that if Bangerter filters are effective in amblyopia therapy, this effect might not be due to degradation of contrast sensitivity, a topic worthy of further study.
There are several weaknesses to our study. Firstly, the results of this study might not be generalizable to clinical populations. All included subjects were young, visually normal adults, and Bangerter filters might have a different effect on the acuity of the better seeing eye of a child with amblyopia. Another limitation of our study is that we used the same filters for all measurements, and acuity degradation may vary for different batches of filters. Nevertheless, our study was designed to investigate the effect of the same filter across four modalities of visual function throughout a cohort of individuals. Finally, for two of the four tests, randomized presentation was not possible, and therefore a learning effect may have occurred, but if there was a learning effect we would have expected it across all filters, which we did not observe.
Bangerter filters degrade optotype and vernier acuity in visually normal adults, but have a less marked effect on contrast sensitivity at lower filter densities. Our finding that the degree of visual degradation is not always as predicted by the filter label indicates the need for careful evaluation of induced acuity deficits when using Bangerter filters in clinical practice. Further study is needed to explore the implications of our findings for clinical populations with diplopia and amblyopia.
Supplementary Material
Acknowledgments
Supported by National Institutes of Health Grants EY015799 and EY011751 (JMH), Research to Prevent Blindness, Inc., New York, NY (JMH as Olga Keith Weiss Scholar and an unrestricted grant to the Department of Ophthalmology, Mayo Clinic), and Mayo Foundation, Rochester, MN.
Footnotes
No conflicting relationships exist
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bangerter A. Die okklusion in der pleoptik und orthoptik. Klin Monatsbl Augenheilkd. 1960;136:305–31. [Google Scholar]
- 2.McIntyre A, Fells P. Bangerter foils: a new approach to the management of pathological intractable diplopia. Br Orthopt J. 1996;53:43–7. [Google Scholar]
- 3.Silverberg M, Schuler E, Veronneau-Troutman S, Wald K, Schlossman A, Medow N. Nonsurgical management of binocular diplopia induced by macular pathology. Arch Ophthalmol. 1999;117:900–3. doi: 10.1001/archopht.117.7.900. [DOI] [PubMed] [Google Scholar]
- 4.Lang J. Scientific essay: An efficient treatment and new criteria for cure of strabismic amblyopia: Reading and Bangerter foils. Binocul Vis Strabismus Q. 1999;14:9–10. [PubMed] [Google Scholar]
- 5.Iacobucci IL, Archer SM, Furr BA, Beyst Martonyi EJ, Del Monte MA. Bangerter Foils in the Treatement of Moderate Amblyopia. Am Orthopt J. 2001;51:84–91. doi: 10.3368/aoj.51.1.84. [DOI] [PubMed] [Google Scholar]
- 6.Levi DM, Klein SA. Hyperacuity and amblyopia. Nature. 1982;298:268–70. doi: 10.1038/298268a0. [DOI] [PubMed] [Google Scholar]
- 7.Levi DM, Klein SA. Differences in vernier discrimination for grating between strabismic and anisometropic amblyopes. Invest Ophthalmol Vis Sci. 1982;23:398–407. [PubMed] [Google Scholar]
- 8.Birch EE, Swanson WH. Hyperacuity deficits in anisometropic and strabismic amblyopes with known ages of onset. Vision Res. 2000;40:1035–40. doi: 10.1016/s0042-6989(00)00011-0. [DOI] [PubMed] [Google Scholar]
- 9.Hess RF, Bradley A. Contrast perception above threshold is only minimally impaired in human amblyopia. Nature. 1980;287:463–4. doi: 10.1038/287463a0. [DOI] [PubMed] [Google Scholar]
- 10.Camparini M, Cassinari P, Ferrigno L, Macaluso C. ETDRS-Fast: Implementing psychophysical adaptive methods to standardized visual acuity measurement with ETDRS charts. Invest Ophthalmol Vis Sci. 2001;42:1226–31. [PubMed] [Google Scholar]
- 11.Beck RW, Moke PS, Turpin AH, Ferris FL, Sangiovanni JP, Johnson CA, et al. A computerized method of visual acuity testing: adaptation of the early treatment of diabetic retinopathy study testing protocol. Am J Ophthalmol. 2003;135:194–205. doi: 10.1016/s0002-9394(02)01825-1. [DOI] [PubMed] [Google Scholar]
- 12.Holmes JM, Archer SM. Vernier acuity cards: a practical method for measuring vernier acuity in infants. J Pediatr Ophthalmol Strabismus. 1993;30:312–4. doi: 10.3928/0191-3913-19930901-10. [DOI] [PubMed] [Google Scholar]
- 13.Mitsuyu M, Zimmer EM. Bangerter occlusives versus spherical convex lenses in the evaluation of visual acuity by visually evoked cortical potentials. Dev Ophthalmol. 1984;9:115–22. doi: 10.1159/000409813. [DOI] [PubMed] [Google Scholar]
- 14.Janknecht P, Funk J. Optic nerve head analyzer and Heidelberg retina tomograph: relative error and reproducibility of topographic measurements in a model eye with simulated cataract. Graefes Arch Clin Exp Ophthalmol. 1995;233:523–9. doi: 10.1007/BF00183434. [DOI] [PubMed] [Google Scholar]
- 15.Cox JF, Suh S, Leguire LE. Vernier acuity in amblyopic and nonamblyopic children. Journal of Pediatric Ophthalmology & Strabismus. 1996;33:39–46. doi: 10.3928/0191-3913-19960101-11. [DOI] [PubMed] [Google Scholar]
- 16.Smith EL, 3rd, Hung LF. Form-deprivation myopia in monkeys is a graded phenomenon. Vision Res. 2000;40:371–81. doi: 10.1016/s0042-6989(99)00184-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


