Abstract
Objective
Cognitive-behavioral therapy (CBT) is the best-established treatment for binge-eating disorder (BED) but does not produce weight loss. The efficacy of behavioral weight loss (BWL) in obese patients with BED is uncertain. This study compared CBT, BWL, and sequential approach in which CBT is delivered first followed by BWL (CBT+BWL).
Method
125 obese patients with BED were randomly assigned to one of the three manualized treatments delivered in groups. Independent assessments were performed post-treatment and at 6- and 12-month follow-ups.
Results
At 12-month follow-up, intent-to-treat binge-eating remission rates were: 51% (CBT), 36% (BWL), and 40% (CBT+BWL) and mean percent BMI losses were −0.9, −2.1, and 1.5, respectively. Mixed models analyses revealed that CBT produced significantly greater reductions in binge-eating than BWL through 12-month follow-ups and that BWL produced significantly greater percent BMI loss during treatment. The overall significant percent BMI loss in the CBT+BWL was attributable to the significant effects during the BWL component. Binge-eating remission at major assessment points was associated significantly with greater percent BMI loss cross-sectionally and prospectively (i.e., at subsequent follow-ups).
Conclusions
CBT was superior to BWL for producing reductions in binge-eating through 12-month follow-up while BWL produced statistically greater, albeit modest, weight losses during treatment. Binge-eating and psychopathology outcomes were well sustained 12-months after treatment completion. Results do not support the utility of the sequential approach of providing BWL following CBT. Remission from binge-eating was associated with significantly greater percent BMI loss. Findings support BWL as an alternative treatment option to CBT for BED.
Keywords: obesity, binge eating, eating disorders, treatment
Binge-eating disorder (BED), a research category in the DSM-IV (American Psychiatric Association, 1994), is characterized by recurrent binge-eating accompanied by feelings of loss of control and marked distress in the absence of inappropriate weight compensatory behaviors. BED is a prevalent major health problem (Hudson, Hiripi, Pope, & Kessler, 2007). BED has diagnostic validity (Wonderlich, Gordon, Mitchell, Crosby, & Engel, 2009), differs from other eating disorders and obesity (Grilo et al., 2009; Grilo, Hrabosby, White, Allison, Stunkard, & Masheb, 2008), and is strongly associated with obesity and elevated risk for medical/psychiatric co-morbidity (Hudson et al., 2007; Wonderlich et al., 2009).
The treatment literature for BED suggests that several medications have short-term efficacy relative to placebo (Reas & Grilo, 2008) and certain psychological treatments are effective (Wilson, Grilo, & Vitousek 2007). Cognitive-behavioral therapy (CBT) is the best-established treatment (NICE, 2004; Wilson, Wilfley, Agras, & Bryson, 2010). The National Institute of Clinical Excellence (2004) recommendation that CBT is the treatment-of-choice was assigned a “grade-of-A,” reflecting strong empirical evidence. Controlled trials have provided further support for the efficacy of CBT, including “treatment specificity” (Grilo, Masheb, & Wilson, 2005); however, studies have reported little difference between interpersonal psychotherapy (IPT) and CBT delivered via group (Wilfley et al., 2002) or CBT guided-self-help (Wilson et al., 2010). Although CBT generally produces remission rates of 40% to 60% and robust improvements in eating disorder psychopathology it fails to produce weight loss (Wilson et al., 2007).
The association between BED and obesity (Hudson et al., 2007) and the possible heightened risk for developing future metabolic problems (Hudson et al., 2010) highlight the need to find methods to effectively reduce weight - in addition to eliminating binge-eating - in persons with BED. The existing literature of behavioral-weight-loss (BWL) for BED is equivocal and difficult to interpret in light of significant methodological shortcomings, particularly the reliance on self-report questionnaires for the assessment of binge-eating, inclusion of heterogeneous patients with varying sub-threshold levels of BED, and a lack of follow-up data (see Wilson et al., 2007; Wonderlich et al., 2009). Overall, CBT appears more effective for reducing binge-eating and associated psychopathology whereas BWL appears more effective for producing short-term weight loss (e.g., Agras et al.,1994; Wilson et al., 2010) although BWL studies in BED (e.g., Devlin et al., 2005; Grilo & Masheb, 2005) and “binge-eaters” (Goodrick, Poston, Kimball, Reeves, & Foreyt, 1998) often report minimal or no weight losses. Interestingly, the modest short-term weight-loss reported by most studies testing BWL for obese BED patients (see Wilson et al., 2007) is at odds with the greater magnitude of weight-losses reported for obese patients who do not binge-eat receiving BWL recruited for obesity trials (e.g., Foster et al., 2003) and with findings from one obesity treatment study in which a post-hoc re-analysis of outcomes for “binge-eaters” (determined by self-report) revealed superior short-term weight-losses relative to non-binge-eaters (Gladis, Wadden, Vogt, Foster, Kuehnel, & Bartlett, 1998).
The current study, a randomized controlled trial to test the relative efficacy of CBT and BWL for BED and the durability of the outcomes over a 12-month follow-up period, was designed as a test of treatment-specificity and to help answer the clinically important question of whether BWL has efficacy for weight loss in this subgroup of obese patients. This study also tested the utility of a sequential treatment approach in which CBT is delivered first followed by BWL. Given findings from RCTs that binge remission was associated with greater weight losses (Devlin et al., 2005; Grilo et al., 2005; Wilfley et al., 2002), the comparison to the sequential CBT+BWL treatment follows the clinical hypothesis that once CBT reduces binge eating and associated psychopathology, patients will be able achieve greater weight loss with BWL.
Methods
Participants
Participants were 125 consecutively evaluated patients who met full DSM-IV research criteria for BED. Recruitment consisted of print advertisements. Eligibility required age between 18 and 60 years and a body mass index (BMI; weight (kg) divided height (m2)) between 30 and 55, in addition to BED criteria. Exclusionary criteria included: concurrent treatment for eating/weight problems, medical conditions (e.g., diabetes or thyroid problems) that influence eating/weight, severe current neurological or psychiatric conditions requiring alternative treatments (psychosis, bipolar disorder), and pregnancy. The study received Yale IRB-approval. After complete description of the study to participants, written informed consent was obtained.
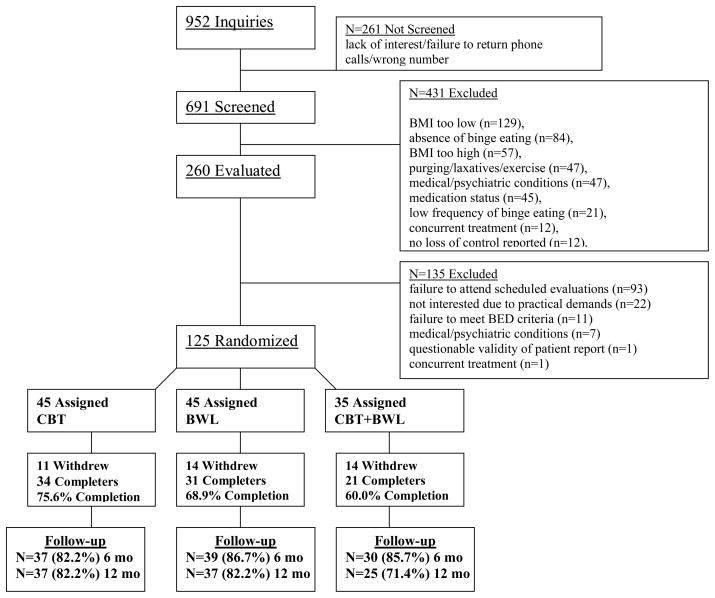
Figure 1 summarizes the flow of participants throughout the study. Nine hundred fifty-two individuals made telephone inquiries and 691 were screened. Two-hundred sixty passed screening and were scheduled for in-person assessments to determine eligibility. Of these, 125 individuals were interested in participating, met eligibility requirements, completed baseline assessments, and were randomized to one of the three treatments.
Figure 1.
The 125 randomized participants had a mean age of 44.8 (SD=9.4) years and mean BMI of 38.8 (SD=5.8). Sixty-seven percent (N=84) of participants were female, 82% (N=102) attended/finished college, and 77% (N=96) were Caucasian (16% (N=20) were African-American, 4% (N=5) were Hispanic, and 3% (N=4) were “other” ethnicity.
Diagnostic Assessments and Repeated Measures
Diagnostic and assessment procedures were performed by trained doctoral-level research-clinicians. DSM-IV psychiatric disorder diagnoses, including BED, were based on the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I/P; First, Spitzer, Gibbon, & Williams, 1996) and personality-disorder diagnoses were determined with the Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV; Zanarini, Frankenberg, Sickel, & Yong, 1996). Inter-rater reliability for diagnoses was good, with kappa coefficients ranging 0.57–1.0; kappa was 1.0 for BED.
Eating Disorder Examination Interview
(EDE; Fairburn & Cooper 1993), a semi-structured, investigator-based interview, was administered to assess eating disorder psychopathology and to confirm the BED diagnosis. The EDE was re-administered at post-treatment and at follow-ups performed 6 and 12 months after treatment completion. The EDE focuses on the previous 28 days except for diagnostic items, which are rated for DSM-IV duration stipulations. The EDE assesses the frequency of objective bulimic episodes (OBE; i.e., binge-eating defined as unusually large quantities of food with a subjective sense of loss of control), which corresponds to the DSM-IV definition of binge-eating. The EDE also comprises four subscales (dietary restraint, eating concern, weight concern, and shape concern) and a total global score. Items are rated on 7-point forced-choice scales (range 0–6), with higher scores reflecting greater severity/frequency. The EDE has well-established inter-rater and test-retest reliability (Grilo, Masheb, Lozano-Blanco, & Barry, 2004) and validity (Grilo, Masheb, & Wilson, 2001). In the present study, inter-rater reliability, determined using N=42 cases, was excellent, with reliability coefficients of 0.99 for OBE frequency and ranging 0.87–0.97 for subscales.
Beck Depression Inventory
(BDI; Beck & Steer, 1987) 21-item version is a well-established self-report (Beck, Steer, & Garbin, 1998) measure of symptoms of depression. The BDI was administered at baseline, bi-monthly during treatment, at post-treatment, and at 6- and 12-month follow-ups.
Weight and height were measured at baseline and again immediately prior to beginning treatment using a trade-legal medical balance-beam scale. Weight was measured bi-weekly throughout treatment, at post-treatment, and at 6- and 12-month follow-ups. BMI was calculated from these measurements.
Randomization and Treatments
Randomization to treatment was performed without any restriction or stratification using a computer-generated sequence. Randomization was determined after formal acceptance into the study and completion of all assessments. Randomization assignment was kept blinded from participants until the start of treatment.
Treatments were delivered by five therapists (doctoral-level psychologists) all with psychotherapy experience and specific clinical experience treating patients with eating disorders and obesity. Treatments were delivered in group sessions (comprising 11–12 participants) co-led by two therapists. The three initial groups, one for each treatment condition, was co-led by one of the investigators (RMM) and one of the therapists, and subsequent therapist pairs always consisted of at least one co-leader experienced in conducting treatment for this study. Each therapist delivered each of the three different treatments. Therapists received intensive training in both CBT and BWL, were monitored via audiotapes of sessions, and received weekly supervision throughout the study by the investigators. Audiotapes were reviewed for adherence to the manualized protocols with specific assessments of session structure, process, and content elements (comprising 12 items). Evaluations were all above 83% compliance, with the modal ratings being 92%–100%.
Cognitive-Behavioral Therapy (CBT)
CBT was administered in 16 group 60-minute sessions over a 24-week period following the manualized protocol (Fairburn et al., 1993). This specific CBT is considered the treatment of choice for BED (NICE, 2004) and has been effectively delivered in groups (Wilfley et al., 2002). CBT is a focal treatment consisting of three overlapping phases. Phase one involves establishing a collaborative therapeutic relationship while focusing on educating the patient about the nature of binge eating and factors thought to maintain the problem. Specific behavioral strategies (e.g., self-monitoring and record keeping) are used to help patients identify problems with their eating patterns while working towards a normal and structured eating pattern. Phase two integrates cognitive restructuring procedures, where patients learn to identify and challenge maladaptive cognitions regarding eating and weight/shape and thoughts that serve as triggers for binge eating. Throughout this phase, focus continues on normalization of eating patterns. Phase three focuses on maintenance of change and relapse prevention.
Behavioral Weight Loss (BWL)
BWL was administered in 16 group 60-minute sessions over a 24-week period following the manualized LEARN Program for Weight Management (Brownell, 2000). This specific BWL is used widely in obesity studies (Foster et al., 2003) and has been previously used in treatment trials with BED (Devlin et al., 2005). LEARN is an acronym for lifestyle, exercise, attitudes, relationships, and nutrition. LEARN focuses on making gradual lifestyle changes with goals of moderate caloric restriction and increased physical activity to produce gradual weight losses. The nutritional guidance follows federal guidelines. This BWL is structured with a series of steps to assess and change eating and activity behaviors. The steps are presented in an additive fashion yet with redundancy to facilitate mastery.
Sequential Cognitive Behavioral Therapy followed by Behavioral Weight Loss (CBT+BWL)
The third treatment condition involved a sequential approach in which CBT was delivered first (16 sessions over 16 weeks) followed by BWL (16 sessions over 24 weeks). The CBT and BWL interventions were delivered in group by the same therapists using the same CBT and BWL protocols as in the monotherapy conditions.
Treatment Preferences and Credibility
After providing informed consent, but prior to being informed of randomized treatment assignment, participants provided ratings (which did not influence randomization) regarding preferences and credibility of treatments. Participants were provided a brief description of the CBT and BWL treatments and asked to indicate whether they preferred CBT or BWL and to rate (0–10) the extent to which the treatments were “logical,” the strength of their preferred treatment, and confidence that the treatments would help them to stop binge eating and to lose weight. Overall, treatment preference was roughly evenly split with 55.2% (N=69) reporting preference for CBT, treatments were rated highly as being “logical” (M=8.9, SD=1.3) and with confidence for stopping binge eating (M=7.7, SD=1.7) and for losing weight (M=7.7, SD=1.8). Comparison of those with preference for CBT versus BWL revealed no statistically significant differences for either “logical” or confidence for stopping binge eating but BWL had significantly higher ratings than CBT for confidence for losing weight (M=8.1, SD=1.6 versus M=7.4, SD=1.8; F(1,123)=5.88, p=.017). Randomized treatment groups did not differ significantly in frequency of treatment preferences nor on mean levels of any credibility or confidence ratings.
Statistical Analyses
Sample size calculation was based on findings from controlled trials for BED testing various CBT and BWL methods (Agras et al., 1994; Grilo et al., 2005; Wilfley et al., 2002). Our sample size provided at least 80% power with two-tailed significance levels of 0.05 for detecting 30% difference in binge remission rates and for detecting mean percent BMI difference of 2.5 (SD=4.0) between groups.
Analyses designed to compare treatments were performed for all randomized patients (intent-to-treat). Baseline characteristics (demographic, psychiatric, and clinical variables) for the treatment groups were compared using chi-square analyses for categorical variables and ANOVAs for continuous measures.
The two primary treatment outcome variables were binge eating and weight loss, which were analyzed using two complementary approaches. First, “remission” from binge eating (zero binges (OBEs) during previous 28 days on the EDE) and “percent BMI loss” were defined separately at each of the post-treatment and 6- and 12-month follow-ups; for treatment dropouts and instances of missing data, pre-treatment baseline data were carried forward. Treatment groups were compared on these two variables using chi-square analyses and ANOVAs.
Second, treatment groups were compared on “frequency” of binge eating (OBEs during previous 28 days on the EDE) and “percent BMI loss” using mixed models (SAS PROC MIXED) that use all available data throughout the study without imputation. Mixed models compared treatments on “frequency” of binge eating (baseline, post-treatment, and at 6- and 12-month follow-ups) and percent BMI loss (based on BMI measured every two weeks throughout treatments and at post-treatment in one model, and at the major assessment time points (baseline, post-treatment, and 6- and 12-month follow-ups) in another model. We focused on BMI because it is a useful measure of obesity, is a good estimate of body fat and gauge of medical risk, and can be used for most men and women. To provide additional clinical context for understanding weight changes, we also compared treatments on weight and absolute weight loss. Secondary outcomes, which included continuous measures of eating disorder psychopathology (EDE scores) and depression levels (BDI scores) at post-treatment and 6- and 12-month follow-ups, were also compared across treatments using mixed models.
In each model, fixed effects of treatment condition, time (with the relevant time points for each measure as described above), the interaction of treatment by time, and random subject-level effects were considered. Distributions of all data were examined and transformations were applied if necessary to satisfy model assumptions (e.g., OBE (binge) frequency data were log-transformed) although the tables show untransformed values. For each model, different variance-covariance structures (unstructured, autoregressive with and without heterogeneous variances, compound symmetry with and without heterogeneous variances) were evaluated and the best-fitting structure was selected based on Schwartz Bayesian criterion (BIC).
Finally, analyses tested the association between remission from binge eating and percent BMI loss. ANCOVAs were performed at each major time-point (i.e., post-treatment, 6-, and 12-month follow-ups) and prospectively (i.e., remission at post-treatment predicting percent BMI loss at 6-month follow-up and remission at 6-month follow-up predicting percent BMI loss at 12-month month follow-up).
Results
Randomization and Patient Characteristics
Of the 125 randomized patients, 45 received CBT, 45 received BWL, and 35 received CBT+BWL. Completion rates, which did not differ statistically, were: 76% (N=34) for CBT, 69% (N=31) for BWL, and 60% (N=21) for CBT+BWL. Follow-up (6-and 12-month) assessments were obtained for over 80% of patients (Figure 1)1. Treatment groups did not differ significantly in demographic or psychiatric variables (Table 1) or on pretreatment levels of any outcome variables (Table 2).
Table 1.
Demographic and Clinical Characteristics of 125 Randomized Patients Across Treatments
| Variable | CBT (N=45) | BWL (N=45) | CBT+BWL (N=35) | Test statistic | p value |
|---|---|---|---|---|---|
| Age, mean (SD) | 45.2 (8.5) | 44.6 (10.5) | 44.5 (9.2) | F(2,122)=0.08 | .93 |
| Female, No (%) | 28 (64.4%) | 28 (62.2%) | 28 (80.0%) | X2(2)=3.61 | .16 |
| Ethnicity, No (%)1 | X2(2)=0.42 | .81 | |||
| Caucasian | 34 (75.6) | 36 (80.0) | 26 (74.3) | ||
| African-American | 5 (11.1) | 7 (15.6) | 8 (22.9) | ||
| Hispanic-American | 3 (6.7) | 2 (4.4) | 0 (0) | ||
| Asian | 2 (4.4) | 0 (0) | 1 (2.9) | ||
| Native American | 1 (2.2) | 0 (0) | 0 (0) | ||
| Education, No (%)1 | X2(2)=3.69 | .16 | |||
| College | 27 (60.0) | 20 (44.4) | 14 (40.0) | ||
| Some college | 13 (28.9) | 17 (37.8) | 11 (31.4) | ||
| High School | 5 (11.1) | 7 (15.6) | 10 (28.6) | ||
| Some high school | 0 (0) | 1 (2.2) | 0 (0) | ||
| DSM-IV co-morbidity lifetime, No (%) | |||||
| Any Axis I psychiatric disorder | 28 (62.2) | 36 (80.0) | 23 (65.7) | X2(2)=3.71 | .16 |
| Major depressive disorder | 19 (42.2) | 21 (46.7) | 14 (40.0) | X2(2)=0.38 | .83 |
| Anxiety disorders | 17 (37.8) | 22 (48.9) | 9 (25.7) | X2(2)=4.48 | .11 |
| Alcohol use disorders | 5 (11.1) | 11 (24.4) | 7 (20.0) | X2(2)=2.75 | .25 |
| Drug use disorders | 9 (20.0) | 7 (15.6) | 7 (20.0) | X2(2)=0.38 | .83 |
| Any Axis II personality disorder | 11 (24.4) | 13 (28.9) | 10 (28.6) | X2(2)=0.27 | .87 |
| Age onset BED, mean (SD) | 25.5 (13.0) | 26.6 (12.0) | 27.5 (11.8) | F(2,122)=0.28 | .76 |
Note: Test statistic = chi-square for categorical variables and ANOVAs for dimensional variables.
P values are for two-tailed tests. SD = standard deviation. No = number. BED = binge eating disorder.
denotes that chi-square was performed for two collapsed categories given low frequencies of some variables (i.e., white versus non-white and college graduate versus less than college degree).
Table 2.
Clinical Variables Across Treatments at Pre-treatment, Post-treatment, and 6- and 12-Month Follow-ups.
| Variable | Pre-treatment | Post-treatment | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CBT | BWL | CBT+BWL | CBT | BWL | CBT+BWL | |||||||
| M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | |
| Binge episodes/month (EDE) | 15.6 | (8.0) | 14.9 | (8.5) | 17.9 | (9.4) | 2.2 | (3.8) | 4.6 | (11.0) | 3.4 | (9.0) |
| Dietary Restraint (EDE) | 1.7 | (1.2) | 1.6 | (1.3) | 1.8 | (1.4) | 1.4 | (0.8) | 1.6 | (1.1) | 1.5 | (1.1) |
| Eating Concern (EDE) | 2.0 | (1.2) | 2.0 | (1.4) | 2.2 | (1.5) | 0.8 | (1.1) | 1 | (1.0) | 0.5 | (0.6) |
| Shape Concern (EDE) | 3.0 | (1.0) | 3.0 | (0.8) | 3.2 | (1.0) | 2.3 | (1.3) | 2.4 | (1.2) | 2.1 | (1.4) |
| Weight Concern (EDE) | 3.6 | (1.0) | 3.3 | (1.0) | 3.8 | (1.1) | 2.4 | (1.2) | 2.4 | (1.1) | 2.2 | (1.1) |
| Global Score (EDE) | 2.6 | (0.9) | 2.5 | (0.8) | 2.8 | (1.0) | 1.7 | (0.9) | 1.8 | (0.8) | 1.6 | (0.9) |
| Depression (BDI) | 15.2 | (6.9) | 15.9 | (8.4) | 17.4 | (9.3) | 10.1 | (8.8) | 11.1 | (8.3) | 9.7 | (9.2) |
| Body mass index | 39.3 | (6.1) | 38.0 | (5.3) | 39.0 | (6.1) | 38.5 | (5.7) | 35.7 | (5.9) | 38.9 | (6.2) |
| Weight (pounds) | 250.1 | (52.6) | 242.7 | (45.8) | 237.2 | (42.8) | 248.5 | (49.3) | 221.1 | (43.4) | 230.4 | (40.9) |
| Weight loss (pounds) | -- | -- | -- | 1.7 | (11.1) | 8.7 | (14.4) | 7.2 | (13.8) | |||
Remission from Binge Eating and Percent BMI Loss at Major Time Points
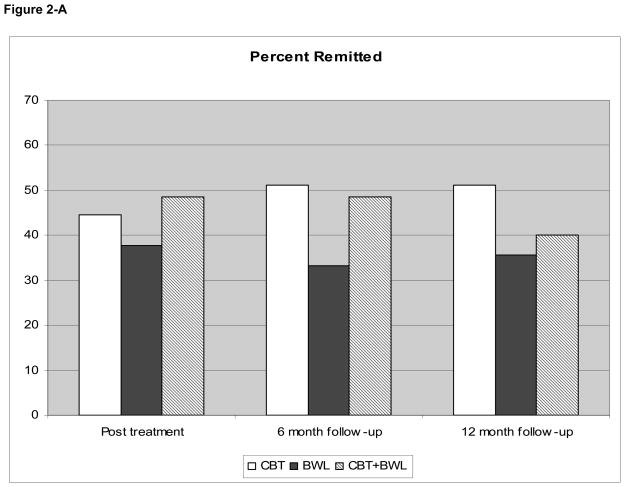
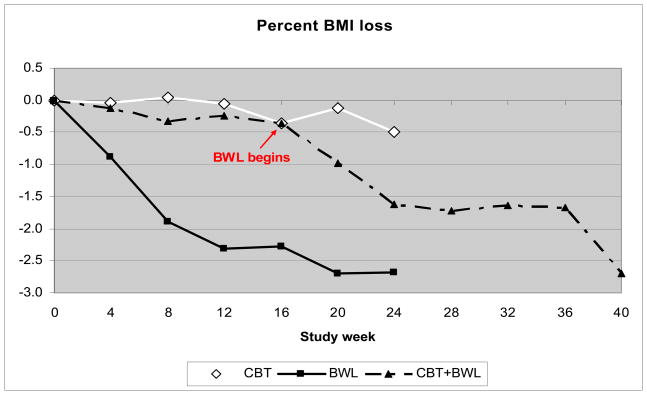
Figure 2 summarizes findings for binge remission (2-A) and percent BMI loss (2-B) at post-treatment and 6- and 12-month follow-ups. Remission rates at post-treatment were 44.4% (CBT), 37.8% (BWL), and 48.6% (CBT+BWL); these rates did not differ significantly across treatments (X2(2)=0.98, p=0.61). At 6-month follow-up, remission rates were: 51.1% (CBT), 33.3% (BWL), and 48.6% (CBT+BWL); these rates did not differ significantly across treatments (X2(2)=3.30, p=0.19). At 12-month follow-up, remission rates were: 51.1% (CBT), 35.6% (BWL), and 40.0% (CBT+BWL); these rates did not differ significantly across treatments (X2(2)= 2.34, p=0.31). To provide further clinical context, we explored whether findings regarding remission rates differed when restricted to treatment completers. Completer-analyses revealed similar non-significant differences between treatments on remission rates, which were as follows for CBT, BWL, and CBT+BWL: at post-treatment (59%, 52%, and 76%), at 6-month follow-up (65%, 48%, and 57%), and at 12-month follow-up (65%, 42%, and 48%).
Figure 2.
Mean percent BMI loss at post-treatment was: −0.5 (SD=3.5) for CBT, −2.6 (SD=5.3) for BWL, and −2.7 (SD=6.0) for CBT+BWL. Specific comparisons revealed that BWL had significantly greater percent BMI loss than CBT (F(1,88)=5.16, p=.03) and that CBT+BWL had significantly greater percent BMI loss than CBT (F(1,78)=4.26, p=.04). At 6-month follow-up, mean percent BMI loss was: −0.5 (SD=5.2) for CBT, −3.3 (SD=8.1) for BWL, and −2.9 (SD=7.6) for CBT+BWL. Specific comparisons at 6-month follow-up indicated BWL had greater percent BMI loss than CBT at a trend level (F(1,88)=3.67, p=.059). At 12-month follow-up, mean percent BMI loss, which did not differ significantly across treatments, was: −0.9 (SD=6.7) for CBT, −2.1 (SD=8.5) for BWL, and −1.5 (SD=7.4) for CBT+BWL.
Frequency of Binge Eating
Table 2 shows binge frequency for the three treatments at the four major assessment points. Mixed models analyses of binge frequency across assessments revealed a significant interaction between treatment and time (F(6,173)=3.46, p=0.003). Follow-up tests indicated the treatments did not differ significantly at post-treatment (F(2,96)=1.48, p=0.23) but differed significantly at the 6-month follow-up (F(2,113)=3.80, p=0.03) and the 12-month follow-up (F(2,106)=3.28, p=0.04). Comparison of specific treatments indicated binge frequency was significantly lower in CBT than BWL at 6-month follow-up (t(114)= 2.68, p=0.009) and 12-month follow-up (t(105)=2.56, p=0.01).
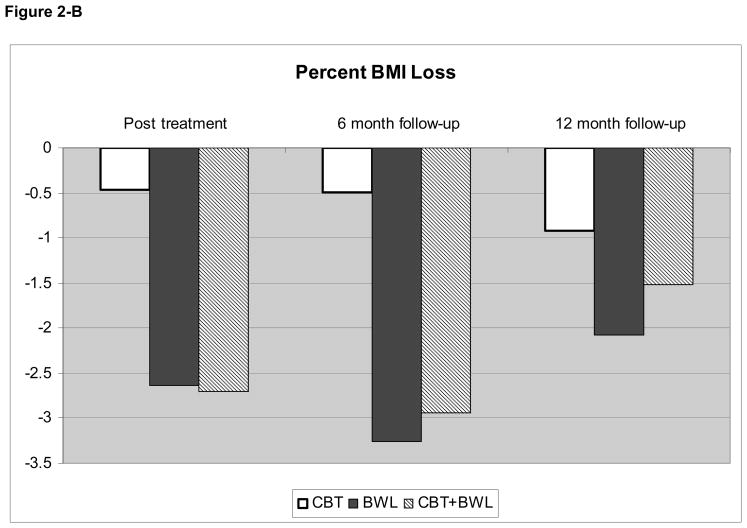
Percent BMI Loss and Weight Changes Over Time
To compare the treatments on percent BMI loss, weight, and absolute weight loss over time, mixed models tested data based on weights measured every two weeks throughout treatment and at post-treatment. Percent BMI loss and absolute weight loss were calculated based on differences and ratios respectively between those values at baseline and the repeated measurements. Figure 3 summarizes the percent BMI loss data shown monthly throughout treatment and at post-treatment and Table 2 summarizes BMI, weight, and absolute weight loss data at the four major assessment points (including 6- and 12-month follow-ups).
Figure 3.
Figure shows percent body mass index (BMI) loss for each of the three treatment conditions throughout the course of treatment. CBT = cognitive behavioral therapy. BWL = behavioral weight loss.
For percent BMI loss (Figure 3), we first fitted a random intercept and slope model for the three treatments which revealed a treatment-by-time interaction at trend level (F(2,97.3)=2.37, p=0.10). Analyses indicated percent BMI loss was significant in the BWL group (t(99.6)=3.70, p=0.0003) and in CBT+BWL group (t(93.3)=2.73, p=0.008) but not in the CBT group (t(99.6)=0.88, p=0.38). Tests of the slope differences indicated improvement (percent BMI loss) was significantly faster in BWL than CBT (t(99.6)=2.08, p=0.04) during treatment. For percent BMI loss at the 6-month and 12-month follow-ups (Table 2), mixed models analyses (considering baseline and post-treatment values) revealed significant time effects but no significant differences between the three treatments.
Similar findings were observed for the two weight variables (weight and absolute weight loss). A random intercept and slope model for the three treatments on repeated measurements revealed a significant treatment-by-time interaction for weight (F(2,103) =3.01, p=0.05) and a non-significant trend interaction for absolute weight loss (F(2,96.8) = 1.95, p=0.15). Analyses indicated significant decreases in weight in BWL (t(103)= − 4.31, p<0.0001) and in CBT+BWL (t(101)= 2.46, p=0.02) but not in the CBT group (t(104)= − 0.99, p=0.32). There was a significant absolute weight loss in the BWL group (t(98.8)= 3.56, p=0.0006) and CBT+BWL group (t(93.1)= 2.57, p=0.01) but not in the CBT group (t(99.1)= 0.99, p=0.33). Tests of the slope differences indicated significantly faster improvements in BWL than CBT for weight (t(104)=2.45, p=0.02) and marginally significantly faster for absolute weight loss (t(98.9)= −1.91, p=0.06) during treatment. For the 6-month and 12-month follow-ups (Table 2), mixed models analyses (considering baseline and post-treatment values) revealed significant time effects but no significant differences between the treatments for either weight or absolute weight loss..
Given the significant differences between BWL and CBT for weight loss and the nature of the three group design that included a sequential CBT+BWL approach, we performed two sets of additional mixed models analyses to clarify further the treatment effects on percent BMI loss, weight, and weight loss. First, we fitted intercept and slope models for the two mono-therapy (CBT and BWL) treatments which revealed significant treatment-by-time interaction for percent BMI loss (F(1,72.1)=3.82, p=0.05), significant treatment-by-time interaction for weight (F(1,75.9)=5.53, p=0.02), and a treatment-by-time interaction at a trend level for absolute weight loss (F(1,72.4)=3.21, p=0.08). Post-hoc testing indicated percent BMI loss was significant in the BWL group (t(72)=3.54, p=0.0007) but not in the CBT group (t(72.3)=0.90, p=0.37). Similarly, post-hoc testing indicated that weight significantly decreased in the BWL group (t(75.8)= − 4.16, p<0.0001) but not in the CBT group (t(76)= − 0.97, p=0.33) and that absolute weight loss was significant in the BWL group (t(72.2)=3.4, p=0.001) but not in the CBT group (t(72.5)=0.99, p=0.33) during treatment.
Second, we performed a within-subject analysis for the CBT+BWL treatment. We fitted a model with a random intercept and with two random slopes (i.e., one for the first phase with CBT and one for the second phase with BWL). For percent BMI loss, the slope for the first 4 months (during CBT) was not significantly different from zero (t(324)=1.06, p=0.29) whereas the slope for the next 6 months (during BWL) was significantly different from zero (t(24.7)=2.68, p=0.02). Similarly, the slope for the first 4 months (during CBT) was not significantly different from zero for both weight (t(26.9)= −1.10, p=0.29) and for absolute weight loss (t(25.7)=0.92, p=0.37) whereas the slope for the subsequent 6 months (during BWL) was significantly different from zero for both weight (t(25.3)= − 2.75, p=0.01) and for absolute weight loss (t(23.2)= 2.50, p=0.02). Thus, consistent with analyses comparing CBT and BWL, this within-subjects analysis revealed that CBT failed to produce weight loss whereas BWL produced weight loss.
Associated Eating Disorder Psychopathology and Depression Levels
Table 2 shows the continuous measures of eating disorder psychopathology and depression levels across treatments at the major assessment points. Mixed models analyses revealed significant time effects (improvements) for all measures but no significant differences among the three treatments on the EDE subscales or BDI.
Binge Remission Associations with Percent BMI Loss
Patients who achieved remission from binge eating at post-treatment (N=54) had significantly greater percent BMI loss than patients without a remission (N=71) both at post-treatment (M=3.4 (SD=5.8) versus M=0.7 (SD=4.1); F(1,123)=9.13, p=0.003) and subsequently at 6-month follow-up (M=4.3 (SD=7.0) versus M=0.6 (SD=6.8); F(1,123)=9.12, p=0.003). At 6-month follow-up, the patients who achieved remission from binge eating (N=55) had significantly greater percent BMI loss than patients without a remission (N=70) both at the 6-month follow-up (M=4.2 (SD=6.8) versus M=0.6 (SD=7.0); F(1,123)=8.51, p=0.004) and subsequently at 12-month follow-up M=3.2 (SD=7.2) versus M=0.2 (SD=7.5); F(1,123)=5.03, p=0.027). At the 12-month follow-up, the patients who achieved remission from binge eating (N=53) had significantly greater percent BMI loss than patients without a remission (N=72) (M=3.5 (SD=6.9) versus M=0.1 (SD=7.7); F(1,123)=6.58, p=0.01).
Discussion
This study tested the relative efficacy of two group treatments for BED - CBT, an established “treatment of choice” (NICE, 2004), and BWL, a widely-used treatment that is logical to test given the equivocal findings and well-known challenge of producing weight loss in this subgroup of obese patients (Wilson et al., 2007; Reas & Grilo, 2008). This study also tested a sequential approach in which CBT is delivered first followed by BWL. Overall, the three treatments produced robust improvements in binge-eating and eating disorder psychopathology that were well sustained during 12-months following the completion of treatments. CBT was superior to BWL for producing reductions in binge-eating frequency through 12-month follow-ups. BWL produced statistically greater, albeit modest, weight losses throughout treatment and at post-treatment, but by 12-month follow-ups the superiority over CBT was no longer statistically significant. The treatments did not differ significantly in their effects on associated eating disorder psychopathology or depression. Our findings do not support the utility of the sequential approach of providing BWL following CBT as the longer more intensive treatment did not enhance binge-eating or weight-loss outcomes compared to CBT or BWL alone. Remission from binge-eating was associated with significantly greater percent BMI loss concurrently and prospectively (i.e., at subsequent follow-ups).
CBT and BWL treatments produced robust improvements in binge-eating that were well sustained through 12-months following treatment. At 12-month follow-up, binge remission rates were 51% for CBT, 36% for BWL, and 40% for CBT+BWL. Few direct comparisons of these outcomes to the literature can be made as most prior research with BWL is difficult to interpret because of methodological limitations (poor measurement, inclusion of uncertain “binge-eaters” and sub-threshold BED determined by self-report) and lack of longer-term follow-up. The 51% binge-eating remission rate for group CBT in this study at 12-month follow-up is substantially higher than the 21% remission rate for group CBT reported by Peterson and colleagues (2009) and slightly lower than the 59% remission rate reported by Wilfley et al (2002) for group CBT. The 36% binge remission rate for group BWL in this study at 12-month follow-up is similar to the 40% remission rated reported by Wilson et al (2010) for individual BWL.
No direct comparison of the observed robust improvements in binge-eating with the pharmacotherapy-only literature for BED is possible as no published placebo-controlled trials have reported follow-up data (see Reas & Grilo, 2008). Nonetheless, we offer the following general comparison in the interest of providing broader context for interpreting our outcomes for CBT and BWL given that some guidelines (NICE, 2004) include certain pharmacology-only treatments as alternative or second-line approaches to CBT. Our binge-eating remission rates for CBT and BWL at 12-month follow-up (based on rigorous EDE assessments requiring four weeks of abstinence from binge-eating) compare favorably with short-term (all range 6–16 weeks, except for one 24-week study) post-treatment remission rates reported by pharmacotherapy studies (based on less stringent one one-week end-point rates) (see Reas & Grilo, 2008). Noteworthy also is that one placebo-controlled pharmacotherapy study of a medication since withdrawn from the market (Stunkard, Berkowitz, Tanrikut, Reiss, & Young, 1996) reported high rates of binge-eating relapse occurring rapidly (one to four months) after medication discontinuation. To date, only two studies have directly compared CBT and medication; one placebo-controlled 16-week trial found CBT was superior to fluoxetine for achieving binge-eating remission (Grilo et al., 2005) and one open-label comparative trial reported that CBT was superior to two different SSRI antidepressants (fluoxetine and fluovaxamine) both at post-treatment and at 12-month follow-up (Ricca et al., 2001). Lastly, Devlin and colleagues (2007) reported 2-year follow-up data suggesting good overall durability of BWL combination treatments for BED, with adjunctive CBT enhancing binge-eating outcomes and fluoxetine enhancing depression outcomes, but neither CBT nor fluoxetine enhancing weight loss. Collectively, with these broader findings from the pharmacotherapy for BED literature as context, our robust outcomes sustained at 12-months follow-up suggest the use of CBT as a primary intervention and support BWL as a reasonable alternative treatment particularly given its widespread availability.
Although CBT and BWL did not differ significantly in the proportion of participants achieving binge-eating remission, CBT was significantly superior to BWL for producing reductions in binge-eating frequency that were evident at 12-months following the completion of treatments. Wilson and colleagues (2010) reported no significant differences between individual-guided-self-help-CBT and BWL on either binge-eating remission rates or frequency at 12-month follow-ups, but by 24-month follow-up, individual-guided-self-help-CBT had significantly greater remission rates. Consistent with Wilson et al (2010), the present study also found that BWL produced statistically greater, albeit modest, weight losses that were maintained and evident 12-months after treatment (−2.1 mean percent BMI loss).
CBT and BWL resulted in substantial improvements in associated eating-disorder psychopathology and depression levels through 12-month follow-ups that did not differ significantly between treatments. These findings are consistent with two rigorous RCTs that reported similar overall robust improvements that did not differ significantly between group-CBT and group-IPT (Wilfley et al., 2002), and individual-guided-self-help-CBT and individual-BWL (Wilson et al., 2010) at 12-month follow-ups.
We note several relative strengths and limitations as context for interpreting our findings. Our assessment and manualized treatment protocols were delivered by highly trained and carefully monitored doctoral research-clinicians. We note our follow-up data collection rates (overall, 82% of 6- and 12-month follow-ups were successfully completed, although only 71.4% of the 12-month follow-ups for the sequential CBT+BWL were obtained) represent a potential relative limitation and context for interpreting our maintenance findings2. Our findings may not generalize to the delivery of CBT or BWL by more “naturalistic” treatment delivery systems. Our findings pertain only for the time period of 12 months after completion and discontinuation of treatments. The one longer-term treatment study found that by 24-months follow-up that IPT and CBT guided self-help showed some advantages over BWL. Thus, future studies should aim to perform even longer-term follow-ups. Our patient group was characterized by diverse gender and ethnic composition and a pattern of clinical characteristics consistent with those reported in epidemiologic studies of BED (Hudson et al., 2007) and the rates of minority groups in the study’s geographic region. Our findings for the modest effects of BWL on weight-loss can only generalize to obese persons with BED who seek treatment for BED and can not speak to the issue of weight losses with BWL in obesity treatment studies (e.g., Foster et al., 2003). The absence of an untreated control group also represents a limitation. Although specific treatments such as CBT have well-established effectiveness for reducing binge-eating (Wilson et al., 2007), a control condition would have provided important information about what happens to weight in untreated obese persons with BED.
Our findings indicate that CBT and BWL are effective for treating BED, produce benefits that are durable through 12-months post-treatment, but fail to produce substantial weight losses. Weight loss has generally been an elusive outcome in treatment studies for BED, including most studies testing BWL for obese patients with BED (Wilson et al. 2007). We found no support for the utility of sequencing BWL after a course of CBT; although statistically significant weight losses were observed after the start of the BWL, the total improvements were not superior to those of BWL by itself. However, our weight loss findings, while modest, converge with previous reports that abstinence from binge-eating is associated with weight loss (Agras et al., 2007; Devlin et al., 2005; Grilo et al., 2005; Wilfley et al., 2002; Wilson et al., 2010). Our analyses extended those findings by showing that binge-eating remission at each assessment point was associated prospectively with significantly greater weight losses. Patients who achieved binge-eating abstinence at post-treatment had a mean 4.3% BMI loss at 6-month follow-up and patients who were binge abstinent at 6-month follow-up had a mean 3.5% BMI loss at 12-month follow-up. These findings suggest that stopping binge-eating may play a role in subsequent weight control. As further context for interpreting these seemingly modest weight losses, we note that two recent studies reported that many patients with BED report gaining substantial amounts of weight prior to seeking treatment (Barnes, Blomquist, & Grilo, 2011; Blomquist, Barnes, White, Masheb, Morgan, & Grilo, 2011). For example, Blomquist et al (2011) found that patients with BED reported a mean 15.1 pound weight-gain during the year prior to seeking treatment. Collectively, the findings provide further support for the effectiveness of CBT for BED, provide support for BWL as an alternative treatment to CBT for BED (particularly given its wide-spread availability), and highlight the importance of abstinence from binge-eating for weight loss.
Table 3.
| Variable | 6-Month Follow-up | 12-Month Follow-up | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CBT | BWL | CBT+BWL | CBT | BWL | CBT+BWL | |||||||
| M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | |
| Binge episodes/month (EDE) | 2.7 | (8.5) | 5.5 | (7.6) | 3.2 | (7.8) | 2.4 | (8.1) | 4.6 | (6.0) | 4.0 | (8.4) |
| Dietary Restraint (EDE) | 1.4 | (1.1) | 1.5 | (1.0) | 1.3 | (1.1) | 1.2 | (1.1) | 1.4 | (1.1) | 1.1 | (1.2) |
| Eating Concern (EDE) | 0.7 | (0.9) | 0.8 | (0.8) | 0.5 | (0.6) | 0.6 | (0.8) | 0.6 | (0.6) | 0.6 | (0.7) |
| Shape Concern (EDE) | 2.0 | (1.2) | 2.4 | (1.3) | 2.0 | (1.3) | 2.1 | (1.4) | 2.2 | (1.3) | 1.8 | (1.2) |
| Weight Concern (EDE) | 2.1 | (1.1) | 2.4 | (0.9) | 1.9 | (1.1) | 2.3 | (1.1) | 2.3 | (1.1) | 2.0 | (1.0) |
| Global Score (EDE) | 1.6 | (0.8) | 1.8 | (0.7) | 1.4 | (0.9) | 1.5 | (0.8) | 1.6 | (0.8) | 1.4 | (0.9) |
| Depression (BDI) | 8.1 | (7.3) | 11.1 | (8.7) | 10.1 | (9.9) | 9.1 | (7.9) | 9.6 | (7.7) | 9.7 | (9.3) |
| Body mass index | 38.7 | (5.7) | 36.6 | (6.8) | 38.2 | (5.3) | 38.3 | (6.0) | 36.6 | (6.5) | 38.7 | (5.6) |
| Weight (pounds) | 246.0 | (48.4) | 231.7 | (52.1) | 231.7 | (44.2) | 243.4 | (50.6) | 230.6 | (49.1) | 229.9 | (39.0) |
| Weight loss (pounds) | 1.9 | (14.9) | 9.1 | (21.7) | 9.6 | (22.8) | 3.1 | (18.7) | 5.4 | (21.2) | 6.2 | (24.5) |
Note: CBT = cognitive behavioral therapy. BWL = behavioral weight loss. M = mean; SD = standard deviation. EDE = eating disorder examination interview; BDI = beck depression inventory
Acknowledgments
This research was supported by National Institutes of Health grant R01 DK49587 (Dr. Grilo). Preparation of this manuscript was also partly supported by NIH grant K24 DK070052 (Dr. Grilo).
Footnotes
Standard procedures were used to maximize data collection rates at each assessment point. Participants were provided “subject payments” ($100 for completing the 6- and 12-month follow-ups) as a token our appreciation and to partly compensate them for their time. Scheduling of assessments was performed well ahead of time to facilitate ease of scheduling and participants were reminded of upcoming appointments via both mailings and telephone calls. Participants who cancelled or missed assessments were immediately contacted to reschedule and research-clinicians provided extremely flexible scheduling. In terms of contacting participants, research-clinicians followed protocols involving repeated attempts to contact participants using multiple methods (telephone, cell phone, letters mailed through U.S. postal service, letters sent via courier service). Research-clinicians also contacted “locators” (family members and/or friends) that participants had provided written informed consent (and contact information) for us to contact in the event of difficulty reaching them directly.
For context, we note that our data collection rates at 12-month follow-ups (82.2% for CBT, 82.2% for BWL, and 71.4% for CBT+BWL) are considerably higher than those in some major recent CBT trials (e.g., Peterson et al., 2010) but quite similar to the data collection rates for BWL (78%) and CBT (86%) at 12-months by Wilson et al (2010). The slightly lower 71.4% collection rate for the CBT+BWL is comparable or slightly higher than similar trials testing long intensive combined treatments (Devlin et al., 2005, 2007).
Trial Registration: clinicaltrials.gov Identifier: NCT00537758
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ccp
References
- Agras WS, Telch CF, Arnow B, Eldredge K, Wilfley DE, Raeburn SD, Henderson J, Marnell M. Weight loss, cognitive-behavioral, and desipramine treatments in binge eating disorder: an additive design. Behavior Therapy. 1994;25:209–238. [Google Scholar]
- Agras WS, Telch CF, Arnow B, Eldredge K, Marnell M. One-year follow-up of cognitive-behavioral therapy for obese individuals with binge eating disorder. Journal of Consulting and Clinical Psychology. 1997;65:343–347. doi: 10.1037//0022-006x.65.2.343. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual. 4. Washington, DC: American Psychiatric Association; 1994. (DSM-IV) [Google Scholar]
- Barnes RD, Blomquist KK, Grilo CM. Exploring pretreatment weight trajectories in obese patients with binge eating disorder. Comprehensive Psychiatry. 2011;52:312–318. doi: 10.1016/j.comppsych.2010.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer R, Garbin M. Psychometric properties of the Beck Depression Inventory: 25 years of evaluation. Clinical Psychology Review. 1998;8:77–100. [Google Scholar]
- Beck AT, Steer R. Manual for revised Beck Depression Inventory. New York: Psychological Corporation; 1987. [Google Scholar]
- Blomquist KK, Barnes RD, White MA, Masheb RM, Morgan PT, Grilo CM. Exploring weight gain in year before treatment for binge eating disorder: A different context for interpreting limited weight losses in treatment studies. International Journal of Eating Disorders. 2011;44:435–439. doi: 10.1002/eat.20836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brownell KD. The LEARN program for weight management. Vol. 2000. Dallas, TX: American Health; 2000. [Google Scholar]
- Devlin MJ, Goldfein JA, Petkova E, Jiang H, Raizman PS, Wolk S, Mayer L, Carino J, Bellace D, Kamenetz C, Dobrow I, Walsh BT. Cognitive behavioral therapy and fluoxetine as adjuncts to group behavioral therapy for binge eating disorder. Obesity Research. 2005;13:1077–1088. doi: 10.1038/oby.2005.126. [DOI] [PubMed] [Google Scholar]
- Devlin MJ, Goldfein JA, Petkova E, Liu L, Walsh BT. Cognitive behavioral therapy and fluoxetine for binge eating disorder: Two-year follow-up. Obesity. 2007;15:1702–1709. doi: 10.1038/oby.2007.203. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge eating: nature, assessment, and treatment. 12. New York: Guilford Press; 1993. pp. 317–360. [Google Scholar]
- Fairburn CG, Marcus MD, Wilson GT. Cognitive-behavioral therapy for binge eating and bulimia nervosa: a comprehensive treatment manual. In: Fairburn CG, Wilson GT, editors. Binge eating: nature, assessment, and treatment. New York: Guilford Press; 1993. pp. 361–404. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV Axis I disorders - patient Edition (SCID-I/P, Version 2.0) New York: New York State Psychiatric Institute; 1996. [Google Scholar]
- Foster GD, Wyatt HR, Hill JO, McGuckin BG, Brill C, Mohammed BS, Szapary PO, Rader DJ, Edman JS, Klein S. A randomized trial of a low-carbohydrate diet for obesity. New England Journal of Medicine. 2003;348:2082–2090. doi: 10.1056/NEJMoa022207. [DOI] [PubMed] [Google Scholar]
- Gladis MM, Wadden TA, Vogt R, Foster G, Kuehnel RH, Bartlett SJ. Behavioral treatment of obese binge eaters: do they need different care? Journal of Psychosomatic Research. 1998;44:375–384. doi: 10.1016/s0022-3999(97)00262-6. [DOI] [PubMed] [Google Scholar]
- Goodrick KG, Poston WSC, Kimball KT, Reeves RS, Foreyt JP. Nondieting versus dieting treatment for overweight binge-eating women. Journal of Consulting and Clinical Psychology. 1998;66:363–368. doi: 10.1037//0022-006x.66.2.363. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Crosby RD, Masheb RM, White MA, Peterson CB, Wonderlich SA, …Mitchell JE. Overvaluation of shape and weight in binge eating disorder, bulimia nervosa, and sub-threshold bulimia nervosa. Behaviour Research and Therapy. 2009;47:692–696. doi: 10.1016/j.brat.2009.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Hrabosky JI, White MA, Allison KC, Stunkard AJ, Masheb RM. Overvaluation of shape and weight in binge eating disorder and overweight controls: refinement of BED as a diagnostic construct. Journal of Abnormal Psychology. 2008;117:414–419. doi: 10.1037/0021-843X.117.2.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM. A randomized controlled comparison of guided self-help cognitive behavioral therapy and behavioral weight loss for binge eating disorder. Behaviour Research and Therapy. 2005;43:1509–1525. doi: 10.1016/j.brat.2004.11.010. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, Lozano-Blanco C, Barry DT. Reliability of the Eating Disorder Examination in patients with binge eating disorder. International Journal of Eating Disorders. 2004;35:80–85. doi: 10.1002/eat.10238. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, Wilson GT. A comparison of different methods for assessing the features of eating disorders in patients with binge eating disorder. Journal of Consulting and Clinical Psychology. 2001;69:317–322. doi: 10.1037//0022-006x.69.2.317. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, Wilson GT. Efficacy of cognitive behavioral therapy and fluoxetine for the treatment of binge eating disorder: a randomized double-blind placebo-controlled comparison. Biological Psychiatry. 2005;57:301–309. doi: 10.1016/j.biopsych.2004.11.002. [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survery Replication. Biological Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson JI, Lalonde JK, Coit CE, Tsuang MT, McElroy SL, Crow SJ, Pope HG., Jr Longitudinal study of the diagnosis of components of the metabolic syndrome in individuals with binge-eating disorder. American Journal of Clinical Nutrition. 2010;91:1568–1573. doi: 10.3945/ajcn.2010.29203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Clinical Excellence (NICE) NICE Clinical Guideline No. 9. London: National Institute for Clinical Excellence; 2004. Eating Disorders – Core Interventions in the treatment and management of anorexia nervosa, bulimia nervosa, related eating disorders. [Google Scholar]
- Peterson CB, Mitchell JE, Crow SJ, Crosby RD, Wonderlich SA. The efficacy of self-help group treatment and therapist-led group treatment for binge eating disorder. American Journal of Psychiatry. 2009;166:1347–1354. doi: 10.1176/appi.ajp.2009.09030345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reas DL, Grilo CM. Review and meta-analysis of pharmacotherapy for binge-eating disorder. Obesity. 2008;16:2024–2038. doi: 10.1038/oby.2008.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ricca V, Mannucci E, Mezzani B, Moretti S, Di Bernardo M, Bertelli M, et al. Fluoxetine and fluvoxamine combined with individual cognitive-behaviour therapy in binge eating disorder: a one-year follow-up study. Psychotherapy and Psychosomatics. 2001;70:298–306. doi: 10.1159/000056270. [DOI] [PubMed] [Google Scholar]
- Stunkard A, Berkowitz R, Tanrikut C, Reiss E, Young L. D-fenfluramine treatment of binge eating disorder. American Journal of Psychiatry. 1996;153:1455–1459. doi: 10.1176/ajp.153.11.1455. [DOI] [PubMed] [Google Scholar]
- Wilfley DE, Welch RR, Stein RI, Spurrell E, Cohen L, Saelens B, …Matt GE. A randomized comparison of group cognitive-behavioral-therapy and group-interpersonal-psychotherapy for the treatment of overweight individuals with binge-eating disorder. Archives of General Psychiatry. 2002;59:713–721. doi: 10.1001/archpsyc.59.8.713. [DOI] [PubMed] [Google Scholar]
- Wilson GT, Grilo CM, Vitousek KM. Psychological treatments of eating disorders. American Psychologist. 2007;62:199–216. doi: 10.1037/0003-066X.62.3.199. [DOI] [PubMed] [Google Scholar]
- Wilson GT, Wilfley DE, Agras WS, Bryson SW. Psychological treatments of binge eating disorder. Archives of General Psychiatry. 2010;67:94–101. doi: 10.1001/archgenpsychiatry.2009.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wonderlich SA, Gordon KH, Mitchell JE, Crosby RD, Engle SG. The validity and clinical utility of binge eating disorder. International Journal of Eating Disorders. 2009;42:687–705. doi: 10.1002/eat.20719. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Sickel AE, Yong L. The Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV) Belmont, MA: McLean Hospital; 1996. [Google Scholar]