Abstract
Background
Despite therapeutic progress, many diseases of the eyes and visual pathways still cause persistent visual deficits that make everyday life more difficult in many ways. Rehabilitation aims to compensate for these limitations by optimizing residual vision. The demand for visual rehabilitation will increase markedly in the near future.
Methods
We summarize the state of the art in visual rehabilitation on the basis of a selective review of the literature, including randomized, controlled trials (RCTs) in the Cochrane and PubMed databases as well as Cochrane reviews. We also pay particular attention to studies illustrating an important principle or a clinically established method.
Results
Central visual field defects impair reading. Persons with an absolute central scotoma can regain reading ability by eccentric fixation and text magnification. Many kinds of magnifying visual aids are available. Specific reading training can further improve reading speed. Peripheral field defects impair orientation. Persons with a concentric field defect can be helped by tactile aids, such as a cane, and with orientation and mobility training. Persons with hemianopia can benefit from compensatory saccadic training.
Conclusion
Suitable rehabilitative measures chosen after the thorough diagnostic evaluation of a visual impairment and analysis of its effects can usually restore reading ability, improve orientation, and thereby enhance the patient’s independence and quality of life. As the demand for visual rehabilitation is increasing, steps will need to be taken to make it more widely available. Furthermore, as the scientific basis for visual rehabilitation is currently inadequate in some areas, more research in the field will be needed.
With many diseases of the eyes and visual pathways, persistent visual deficits arise that require rehabilitation. The effects on everyday living are various and need specific rehabilitation measures. These measures aim to compensate for the restrictions by making better use of residual vision.
Estimates based on WHO statistics indicate that there are around 1.2 million visually impaired persons in Germany, more than 160 000 of whom are blind (e1, e2).
In Germany visual impairment is legally defined as reduction of vision to 0.3 or less, and blindness as reduction of vision to 0.02 or narrowing of the visual field to a 5° radius (1, 2). In other nations the legal threshold for the definition of blindness is usually at a higher level of vision (0.1), but mostly without the option for special state support due to blindness.
The requirement for visual rehabilitation is set to rise sharply in the near future: by about 35% among blind and visually impaired persons, and by about 60% for newly occurring blindness (3), mainly because of the increasing number of older patients.
Age-related macular degeneration (AMD) is the most common cause of severe visual impairment in the industrialized nations. Amongst over-85-year-olds, early-stage AMD (without loss of vision) has a prevalence of 30%, while late-stage AMD (with loss of vision) has a prevalence of 13% (4). AMD does not, however, result in total blindness, because usually the peripheral visual field is preserved.
The number of patients with cerebral insults is also going up, because of demographic trends and improved survival rates after stroke (5, e3, e4). Cerebral (usually persistent) visual impairment occurs in about 30% of patients with brain damage (e5).
The spectrum of visual rehabilitation has become much wider in recent years and includes not just the eyes, but also a new understanding of functional compensatory cortical plasticity in the adult visual system (e6, e7). In particular, cortical adaptation strategies such as eccentric fixation (6, 7, e8– e10), visual attention mechanisms (e11– e13), and compensatory eye movements (8, e14, e15) play a role. Functional compensatory cortical plasticity is characterized by reinforcement of synaptic responses and less by spatial reorganization (e6, e16). Understanding the nature of this plasticity promotes the development and implementation of new training methods that will have an increasingly important role in future.
Complex brain injuries after trauma or perinatal hypoxic–ischemic insult—the most common cause of severe visual impairment in children in the Western world (e17– e19)—require multidisciplinary rehabilitation (e20, e21). Given the usually dominating neurological symptoms, cerebral visual impairments are often overlooked. If they are combined with changes to the eyes themselves, this can make rehabilitation even more difficult.
Symptoms of cortical stimulation in the absence of visual input lead to pseudohallucinations, which are often not reported by patients, who fear mental illness, or are misinterpreted by those around the patients. This phenomenon, known as Charles Bonnet syndrome (e22) occurs in 11% to 27% of cases, depending on the severity of visual loss (e23– e26). In addition, those with visual impairment often suffer from depressive disorders because of their reduced quality of life (9, 10, e27, e28).
Literature analysis
The selective literature search was based on searching Cochrane Library Reviews and randomized controlled studies (RCTs) that have appeared in the Cochrane Library and PubMed in the period from 1990 to the beginning of 2011. The following search terms were used: “vision rehabilitation,” “rehabilitation and vision,” “visual rehabilitation and effectiveness,” “neurological rehabilitation and visual,” “hemianopia.” Although a few studies with an evidence level of at least 2b (Table 1a– b) exist in the field of neuropsychological rehabilitation, very little has been published in the field of ophthalmological/optical rehabilitation (“low-vision rehabilitation”) that fulfills strictly scientific requirements.
Table 1. Studies on training in hemianopia.
| a) Studies on training to improve hemianopic reading impairment | |||
| Study | Method | Study design | Evidence level |
| 1. Kerkhoff et al. 1992 (11) | Optokinetic training with moving text | RMD | 2b |
| 2. Zihl 1984 (e32) | |||
| 3. Schütt et al. 2008 (12) | Oculomotor training | ||
| 4. Spytzina et al. 2007 (13) | Optokinetic training with moving text | RCT | 1b |
| 5. Reinhard et al. 2005 (14) | Restorative visual field training with an effect on reading | RMD | 2b |
| b) Compensatory exploratory saccade training to improve hemianopic orientation impairment | |||
| Study | Method | Study design | Evidence level |
| 1. Kerkhoff et al. 1992 (11) | Oculomotor training | RMD | 2b |
| 2. Zihl 1995 (15) | Oculomotor training | RMD | 2b |
| 3. Nelles et al. 2001 (16) | Oculomotor training | RMD | 2b |
| 4. Pambakian et al. 2004 (17) | Search task (single object) | RMD | 2b |
| 5. Bolognini et al. 2005 (e33) | Audiovisual training | RMD | 2b |
| 6. Roth et al. 2009 (18) | Search task (multiple objects) vs. visual field stimulation | RCT | 1b |
| 7. Keller & Lefin-Rank 2010 (e34) | Audiovisual vs. visual | RCT | 1b |
| 8. Lane et al. 2010 (e35) | Oculomotor training vs. attention training | RCT | 1b |
The studies that used optokinetic training reported an improvement in reading speed (studies 1 and 2 by a mean of 40 words (W)/min, study 4 by 20 W/min), but only study 4 was randomized and controlled (evidence level 1b). Study 3, which used oculomotor training, showed an increase in reading speed by 35 W/min (for single words and for numerals). Study 5 investigated the effect of visual field stimulation training to restore the blind half-field on reading ability. The effect of 7 W/min was not clinically relevant.
All studies reported an improvement in exploratory behavior after training, but studies 1–5 were carried out without a control group (evidence level 2b). Hence, the specificity of saccade training was not shown. Study 6 was the first to show the effectiveness of exploratory saccade training under randomized and controlled conditions (evidence level 1b). Study 7 described greater improvement with additional auditory stimuli compared to visual alone. Study 8 showed both methods to have similar effects.
RMD: repeated measurement design, RCT: randomized controlled study with a control group
Note: To the best of the author’s knowledge, all RCTs are included in this table.
In the low-vision literature there were two Cochrane Reviews; however, in the one entitled “Reading aids for adults with low vision” (e29), none of the nine studies included allowed definite conclusions to be drawn, and the same was true of the two studies included in the other review, “Orientation and mobility training for adults with low vision” (e30). A review (e31) on the evidence of expanded optometric therapy also showed that there are practically no randomized controlled studies on this subject.
The calculation of effect sizes in the expanded literature search was possible only to a limited extent, because either standard deviations were not calculated or reported or patient selection had led to data distortion. In addition, in many studies the interventions were described too vaguely for any conclusions to be drawn from them.
For this reason, the present review took account of only those studies that either threw up an interesting scientific question or demonstrated an important principle, or in which clinical experience over many years has shown a positive effect and this method is already established in clinical routine.
The present review is intended to give colleagues from other specialties an insight into the field of visual rehabilitation. It summarizes the present state of knowledge and indicates the most important causes of visual impairment, its impact on tasks of everyday living, and current options for its rehabilitation.
WHO classification
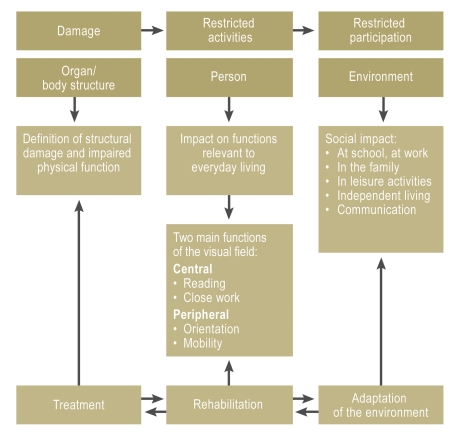
The International Classification of Functioning, Disability and Health (ICF) developed by the World Health Organization (WHO) (20) takes account of three areas that apply well to the visual system (Figure 1):
Figure 1.
The WHO International Classification of Functioning, Disability and Health (ICF) (20) takes account of three areas:
The damage to the organ, the physical function impairment. This is the area where specific therapy usually applies.
The restriction of the person’s activities, i.e., the impact of the organ damage on everyday living. Two main functions of the visual field are distinguished: the central part for close tasks—above all, reading—and the periphery for orientation and mobility. This is where rehabilitation comes in.
Reduced participation in social life, in relation to the person’s environment, with impact on various areas of life. It is often possible to adapt the environment, e.g., by high-contrast or tactile markings (modified from [21]).
Damage to the organ
Restriction of the person’s activities due to the organ damage
Reduced participation by the person in social life.
Diseases of the eyes and visual pathways
Media opacity
Opacities of the media (cataract, corneal dystrophy, vitreous opacity) result in a reduction of vision and contrast and an increased susceptibility to glare—with consequences for the ability to read and to orientate oneself.
Retinopathies
Retinopathies (diabetes, chorioretinitis, high-grade myopia) lead to disseminated retinal lesions and diffuse visual field defects that can disturb orientation and/or reading.
Macular disease/optic atrophy
Macular disease and many cases of optic atrophy result in a central scotoma; that is, an object that is looked at directly disappears into the scotoma and fine details cannot be seen. The primary impact of this is on the ability to read.
Degenerative retinopathies/glaucoma
In degenerative retinopathies and in cases of advanced glaucoma, there is a concentric narrowing of the visual field that restricts the ability to orientate oneself.
Suprachiasmatic lesions of the visual pathways
Suprachiasmatic lesions of the visual pathways lead to homonymous visual field defects, usually hemianopic or quadrant-shaped, that impair orientation and in many cases also reading.
Ability to read
Normal reading
The requirements for the ability to read are adequate resolution of the part of the retina being used (for newspaper print, 0.4 at 25 cm) and adequate size of the reading visual field or perceptual span (3–4 letters to the left of the fixation point and up to 15 letters in the direction of reading) (e36– e38). A normal reader uses the fovea for fixation (Figure 2a). Visual acuity decreases rapidly as retinal eccentricity increases, so letters are seen clearly only in the area of the reading visual field. To see the next complex of letters clearly, the eye needs to move.
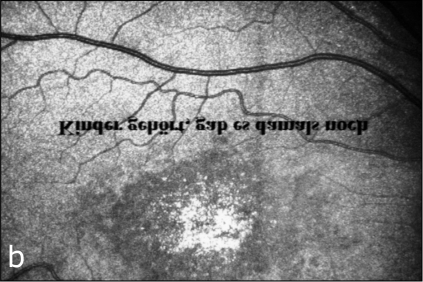
Figure 2.
Examining fixation behavior on the fundus using a scanning laser ophthalmoscope (SLO). The instrument allows simultaneous visualization of the fundus and the text (which appears reversed only to the examiner). This makes it possible to make a direct live recording of the reading process on the retina: a) normal person with central fixation (in this example of the word “gab”), b) patient with juvenile macular degeneration (Stargardt’s maculopathy). The patient reads the text with an eccentric, normal part of the retina above the lesion (and fixates on the word “gab”) (modified from [6, 21]).
Reading impairment
Diseases that cause a scotoma in the center of the visual field result in impairment of reading (for a comprehensive account see [21, 22]). Loss of the ability to read entails severe restriction of independence and quality of life. The most common reason is a central scotoma, which is usually caused by macular disease, less often by optic atrophy. With absolute central scotoma and central fixation, the reading visual field is obscured by scotoma and there is no ability to read. In many patients a useful adaptation occurs spontaneously: They fixate at the edge of the lesion with a normal area of retina (Figure 2b) (6), 21), e9, e10); although resolution is lower here, this can be compensated by magnifying the text. This eccentric fixation can be recognized by direct inspection of the direction of gaze. Figure 3 shows the mechanism on the basis of the bulbus position.
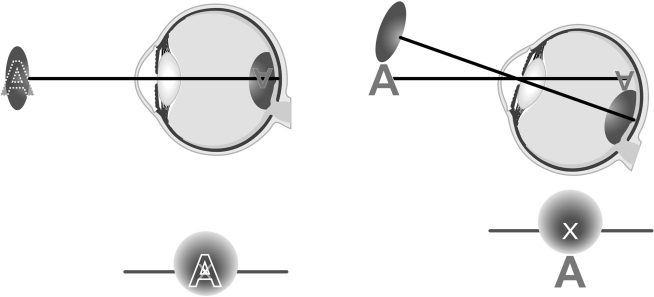
Figure 3.
Examining fixation behavior by observing the bulbus position (direction of gaze) in patients with macular disease (modified from [8]).
Left: With the gaze directed straight forward, the letter A falls directly on the nonfunctioning macula and thus into the central scotoma. The patient is unable to read.
Right: With eccentric fixation, the letter is fixated with a normal part of the retina (in this example, above the lesion); in the visual field it is now below the scotoma. The gaze is directed upward. When this is combined with a magnifying visual aid, reading is now possible.
The combination of eccentric fixation and text magnification is the basis for restoring the ability to read in a patient with central scotoma. For this reason, magnifying visual aids are extremely successful in this patient group. In the author’s own study, out of 530 patients with adult macular degeneration, only 16% could read newspaper print before the consultation; afterwards 94% could do so. They increased their reading speed by an average of 56 words per minute (from 16 [standard deviation (SD) 33]) to 72 [SD 35]) (23) (normal: 180 words/min) (e39). A large range of optical and electronic aids are available (Table 2).
Table 2. Rehabilitation measures in blind or visually impaired patients.
| Reading impairment | Orientation impairment |
Vision aids
|
Vision aids
|
Tactile aids
|
Obstacle detection
|
Acoustic aids
|
Acoustic aids: electronic guidance systems
|
|
Training
|
| All visual impairments | |
Social counseling
| |
*These aids are not yet in routine use
Additional training measures can further improve reading ability. Training for eccentric fixation can be useful in patients who still fixate centrally (e9), but is not generally required, and moreover is a matter of dispute (e40). Training in using the visual aid is important, because with optic aids certain working distances have to be observed. Specific reading training with computer programs that either show single words on the screen or train eye movements during reading improves reading ability in patients with juvenile macular dystrophy by approximately an additional 20 words/min (median)—a statistically significant and clinically relevant effect (24). Whether this success can be extended to patients with AMD remains to be shown.
In patients with ring scotoma there is a central island of vision within a central scotoma, but it can become too small for reading. There is then a discrepancy between relatively good vision (for single letters) and the lack of an ability to read. In such cases rehabilitation can be difficult. Many patients learn, in some cases supported by training (e8, e41), to use an eccentric part of the retina—despite the central vision—to read large print.
In patients with concentric constriction of the visual field, acoustic or tactile aids may be used (Table 2).
In those with homonymous hemianopia, reading ability depends mainly on the distance from the visual field defect to the center, i.e., on the size of the residual visual field (8, e42).
Patients with macular sparing – a seeing area of 2° to 5° in the horizontal in the blind half-field – may be able to read normally. If there is no macular sparing, a high-grade reading impairment will be present, since half of the reading visual field has no function. Some patients can fixate eccentrically despite having intact foveal function, thus shifting the border of their visual field defect toward the hemianopic side, and thus creating for themselves a small area of perception along the visual field border, which improves their ability to read (e43).
The side of visual field loss also matters: It is much worse if it is on the side in the direction of reading. Patients with left-sided hemianopia have difficulty in finding the start of the next line (e42). Tactile aids to improve orientation on the page have proved their value in everyday living (without scientific evidence), especially in left-sided hemianopia (index finger on the start of the line, or a ruler or slightly magnifying ruler).
Earlier studies using moving text (optokinetic training) reported positive effects (11, e32, e44), but a RCT (13) was the first to show the specific effect of this training in right-sided hemianopia (Table 1a).
Orientation and mobility
Normal orientation ability and mobility require an intact peripheral visual field, movement and contrast vision, and normal visual attention. The acoustic and vestibular systems also contribute to spatial orientation.
Patients with concentric constriction of the visual field are impaired in their ability to orientate themselves. In practice, visual, tactile, and acoustic aids are used (Table 2). For patients with sufficient residual vision, small telescopes (“monoculars”) allow street signs, bus numbers, etc., to be made out, as do cut-off filters that increase contrast. In terms of tactile aids, orientation and mobility training is carried out with the long cane. New technology using electronic guidance systems has not come into established use so far, but may perhaps play a more important role in the future (Table 2). Night vision instruments can be used to improve night blindness (e45, e46). Whether visual prostheses, which can evoke a visual impression via “artificial seeing”, will be of use at the everyday level in future cannot be judged at present.
People with hemianopic orientation impairment suffer considerable restrictions in their everyday life: They bump into people and objects and have problems in finding their way about, with the result that they have reduced participation in social life, are unable to drive, and their quality of life declines. Patients make spontaneous saccades to the blind side, thus shifting their visual field border, which is often wrongly interpreted as an improvement in the visual field (e47). This spontaneous adaptation strategy can be supported by training.
Earlier studies reported a positive effect of compensatory eye movement training (11, 15– 17), but the specificity was not shown because of the lack of control groups (Table 1b [e44]). For this reason the authors carried out a RCT which showed for the first time that exploratory saccade training is specifically effective (18, 19). This compensatory training promotes scanning of the blind half of the visual field, and thus better use of the whole field of view (Figure 4). The training consisted of an on-screen number search task and was carried out at home twice daily for 30 min each time, 5 days a week, for 6 weeks.
It resulted in a highly significant improvement in exploratory behavior on the diseased side, with a reduction of reaction time both in the number search task (15.9 ms to 8.4 ms in the experimental group versus 14.2 ms to 11.6 ms in the control group) and in the natural search task (2.2 to 1.7 versus 2.0 to 1.9). Once learned, these strategies were used in everyday life and persisted after the training ended. Improvement occurred even in patients whose visual field defect had existed for years. Quality of life in the social area also improved.
Exploratory saccade training is so simple it can be carried out at home even by people with no previous computer experience (www.medizin.uni-tuebingen.de/augenklinik, www.amd-read.net). Training methods to improve visual searching using paper material use the same approach in principle, but have not been tested in studies (e48, e49).
Training methods that seek to restore the blind half of the visual field through visual stimulation (e.g., [e47, e50]) did not prove to be effective in control studies (14, 18, 19, e51– e54). A distinction must be made between this and the rare, unconscious (irrelevant to everyday living) residual vision (“blindsight”) via direct connections from the superior colliculus to higher visual centers (e7, e55).
Patients with complex brain injury can have various visual disturbances, such as visual field defects, diplopia, hypoaccommodation, eye movement disorders, and deficits in higher cortical processing. An intensive orthoptic diagnostic work-up—which may include prism adaptation and simple training methods using hard (paper) copy to improve visual attention, exploration, and eye–hand coordination—has proved valuable in practice ([e48, e49]) but this has not been scientifically demonstrated.
Social considerations
Rehabilitation includes assessment of the degree of disability with reference to whether the visually impaired person is entitled to carry a disabled person’s identity card, together with an expert witness statement as to whether the patient is legally blind. Receipt of special state support due to blindness is basically regulated by state law. The criteria are given in the guidelines of the German Ophthalmological Society (Deutsche Ophthalmologische Gesellschaft) (1, 25).
Summary
With many visual deficits, effective rehabilitation is possible. It is important to assess functions that are relevant to everyday living. Visual acuity alone means little. Compensatory measures such as vision aids and training aim to optimize residual vision and promote functional compensatory cortical plasticity on the basis of synaptic activation. They need to be adapted to each patient’s individual situation. In most cases it is possible to improve the patient’s independent living and quality of life.
Contemporary visual rehabilitation goes far beyond purely optical care and requires a knowledge of the pathophysiology of each impairment, its impact on everyday living, potential spontaneous adaptation strategies, and the options for intervention. Unfortunately, even today too few treatment facilities and experts are available.
Good interdisciplinary collaboration between ophthalmologists, orthoptists, neurologists, neuropsychologists, and low-vision specialists from various occupational groups is essential. For those in other medical disciplines, it is important to tell patients about the possibilities for rehabilitation. Often these are insufficiently known, and many patients go for years without receiving the care that they need.
With the rising needs and the positive developments expected from new training methods and technology, it is desirable that more young medical professionals should be persuaded to take up the time-consuming but very successful work of visual rehabilitation. In addition, the care offered needs to be extended—in low vision services, in neurological rehabilitation facilities, and in ophthalmologists’ offices, where more time and money need to be made available so that as many patients as possible can be effectively cared for close to home.
In view of the current inadequate position in terms of research studies, more support of research into visual rehabilitation is needed.
Figure 4.
Left: With the gaze directed forward, the blind half-field is obscured. Right: With compensatory eye movements to the hemianopic side, the blind half-field is scanned and the whole field of view used for information gathering. This allows obstacles (in this example, the suitcase) to be recognized in time. Saccade training is effective in training exploratory saccades of this kind (18, 19).
Key Messages.
Diseases of the eye and visual pathways can lead to various restrictions in everyday living which require specific rehabilitation.
Visual rehabilitation goes well beyond the purely optical; it takes account of spontaneous adaptation strategies and promotes functional compensatory cortical plasticity by means of specific training methods.
Visual rehabilitation is very successful, especially in improving reading and orientation ability.
The need for visual rehabilitation is increasing.
The care on offer for visual rehabilitation is inadequate and needs to be expanded.
Acknowledgments
Translated from the original German by Kersti Wagstaff, MA.
Footnotes
Conflict of interest statement
The author is involved in the scientific development of the saccade training software at the University of Tübingen (Visiocoach), but has no financial interest.
References
- 1.Völcker HE, Gramberg-Danielsen B. Schäden des Sehvermögens. Empfehlungen von DOG und BVA von 1994. Ophthalmologe. 1994;91:403–407. [PubMed] [Google Scholar]
- 2.2011. Oktober. Versorgungsmedizin-Verordnung vom 10. Dezember 2008 (BGBl. I S. 2412), zuletzt durch Artikel 1 der Verordnung vom. (BGBl. I S. 2153) geändert. [Google Scholar]
- 3.Knauer C, Pfeiffer N. Erblindung in Deutschland - heute und 2030. Ophthalmologe. 2006;103:735–741. doi: 10.1007/s00347-006-1411-y. [DOI] [PubMed] [Google Scholar]
- 4.Klaver CC, van Leeuwen R, Vingerling JR, de Jong PT. Altersabhängige Makuladegeneration. Berlin: Springer; 2004. Epidemiologie. [Google Scholar]
- 5.Truelsen T, Piechowski-Jozwiak B, Bonita R, Mathers C, Bogousslavsky J, Boysen G. Stroke incidence and prevalence in Europe: a review of available data. European Journal of Neurology. 2006;13:581–598. doi: 10.1111/j.1468-1331.2006.01138.x. [DOI] [PubMed] [Google Scholar]
- 6.Trauzettel-Klosinski S, Teschner C, Tornow RP, Zrenner E. Reading strategies in normal subjects and in patients with macular scotoma - assessed by two new methods of registration. Neuro-Ophthalmol. 1994;14:15–30. [Google Scholar]
- 7.von Noorden G, Mackensen G. Phenomenology of eccentric fixation. Amer J Ophthalmol. 1962;53:642–659. doi: 10.1016/0002-9394(62)91987-6. [DOI] [PubMed] [Google Scholar]
- 8.Trauzettel-Klosinski S, Reinhard J. The vertical field border in human hemianopia and its significance for fixation behavior and reading. Invest Ophthalmol Vis Sci. 1998;39:2177–2186. [PubMed] [Google Scholar]
- 9.Knauer C, Pfeifer N. The value of vision. Graefes Arch Clin Exp Ophthalmol. 2008;246:477–482. doi: 10.1007/s00417-007-0668-4. [DOI] [PubMed] [Google Scholar]
- 10.Rovner BW, Casten RJ. Activity loss and depression in age-related macular degeneration. Am J Geriatr Psychiatry. 2002;10:305–310. [PubMed] [Google Scholar]
- 11.Kerkhoff G, Münßinger U, Haaf E, Eberle-Strauss G, Stögerer E. Rehabilitation of homonymous scotoma in patients with postgeniculate damage of the visual system: saccadic compensation training. Restorative Neurolology and Neuroscience. 1992;4:245–254. doi: 10.3233/RNN-1992-4402. [DOI] [PubMed] [Google Scholar]
- 12.Schuett S, Heywood CA, Kentridge RW, Zihl J. Rehabilitation of hemianopic dyslexia: are words necessary for re-learning oculomotor control? Brain. 2008;131:3156–3168. doi: 10.1093/brain/awn285. [DOI] [PubMed] [Google Scholar]
- 13.Spitzyna G, Wise R, McDonald S, et al. Optokinetic therapy improves text reading in patients with hemianopic alexia. Neurology. 2007;68 doi: 10.1212/01.wnl.0000264002.30134.2a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reinhard J, Schreiber A, Schiefer U, et al. Does visual restitution training change absolute homonymous scotoma? British Journal of Ophthalmology. 2005;89:30–35. doi: 10.1136/bjo.2003.040543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zihl J. Visual scanning behaviour in patients with homonymous hemianopia. Neuropsychologia. 1995;33:287–303. doi: 10.1016/0028-3932(94)00119-a. [DOI] [PubMed] [Google Scholar]
- 16.Nelles G, Esser J, Eckstein A, Tiede A, Gerhard H, Diener HC. Compensatory visual field training for patients with hemianopia after stroke. Neurosci Lett. 2001;306:189–192. doi: 10.1016/s0304-3940(01)01907-3. [DOI] [PubMed] [Google Scholar]
- 17.Pambakian ALM, Mannan SK, Hodgson TL, Kennard C. Saccadic visual search training: a treatment for patients with homonymous hemianopia. J Neurol Neurosurg Psychiatry. 2004;75:1443–1448. doi: 10.1136/jnnp.2003.025957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roth T, Sokolov AN, Messias A, Roth P, Weller M, Trauzettel-Klosinski S. Comparing explorative saccade and flicker training in hemianopia: a randomized controlled study. Neurology. 2009;72:324–331. doi: 10.1212/01.wnl.0000341276.65721.f2. [DOI] [PubMed] [Google Scholar]
- 19.Roth T, Sokolov AN, Messias A, Roth P, Weller M, Trauzettel-Klosinski S. Sakkadentraining verbessert visuelle Exploration bei Hemianopsie. Eine randomisierte kontrollierte Studie. Z prakt Augenheilkd. 2009;30:403–410. [Google Scholar]
- 20.World Health Organisation (WHO) Geneva: 2004. International classification of functioning, disability and health (ICF) [Google Scholar]
- 21.Trauzettel-Klosinski S. Rehabilitation for visual disorders. J Neuro-Ophthalmol. 2010;30:73–84. doi: 10.1097/WNO.0b013e3181ce7e8f. [DOI] [PubMed] [Google Scholar]
- 22.Trauzettel-Klosinski S. Rehabilitation bei Sehbahnschäden. Klin Monatsbl Augenheilkd. 2009;226:897–907. doi: 10.1055/s-0028-1109874. [DOI] [PubMed] [Google Scholar]
- 23.Nguyen NX, Weismann M, Trauzettel-Klosinski S. Improvement of reading speed after providing of low vision aids in patients with age-related macular degeneration. Acta Ophthalmol. 2009;87:849–853. doi: 10.1111/j.1755-3768.2008.01423.x. [DOI] [PubMed] [Google Scholar]
- 24.Nguyen NX, Stockum A, Hahn G, Trauzettel-Klosinski S. Training to improve reading speed in patients with juvenile macular dystrophy: A randomized controlled study. Acta Ophthalmol. 2011;89:e82–e8. doi: 10.1111/j.1755-3768.2010.02081.x. doi: 10.1111/j.1755-3768.2010.02081.x. [DOI] [PubMed] [Google Scholar]
- 25.Rohrschneider K, Bültmann S, Mackensen J. Grundlagen der Begutachtung nach dem Schwerbehindertengesetz und im sozialen Entschädigungsrecht. Ophthalmologe. 2007;104:457–463. doi: 10.1007/s00347-007-1536-7. [DOI] [PubMed] [Google Scholar]
- e1.Bertram B. Blindheit und Sehbehinderung in Deutschland: Ursachen und Häufigkeit. Der Augenarzt. 2005;6:267–268. [Google Scholar]
- e2.Resnikoff S, Pascolini D, Etya´ ale D, Pararajasegaram R, Pokharel GP, Mariotti SP. Global data on visual impairment in the year 2002. Bulletin of the World Health Organization. 2004;82:844–851. [PMC free article] [PubMed] [Google Scholar]
- e3.Feigin VL, Lawes CMM, Bennett DA, Anderson CS. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurology. 2003;2:43–53. doi: 10.1016/s1474-4422(03)00266-7. [DOI] [PubMed] [Google Scholar]
- e4.Rothwell PM, Coull AJ, Silver LE, et al. Population-based study of event-rate, incidence, case fatality, and mortality for all acute vascular events in all arterial territories (Oxford Vascular Study) Lancet. 2005;366:1773–1783. doi: 10.1016/S0140-6736(05)67702-1. [DOI] [PubMed] [Google Scholar]
- e5.Zihl J. Zerebrale Sehstörungen. In: Karnath H-O, Hartje W, Ziegler W, editors. Kognitive Neurologie. Stuttgart: Thieme; 2006. pp. 1–18. [Google Scholar]
- e6.Karmarkar UR, Yang D. Experience-dependent plasticity in adult visual cortex. Neuron. 2006;52:577–585. doi: 10.1016/j.neuron.2006.11.001. [DOI] [PubMed] [Google Scholar]
- e7.Nelles G, Pscherer A, de Greiff A, Gerhard H, Forsting M, Esser J, Diener HC. Eye-movement training-induced changes of visual field representation in patients with post-stroke hemianopia. J Neurol. 2010;257:1832–1840. doi: 10.1007/s00415-010-5617-1. [DOI] [PubMed] [Google Scholar]
- e8.Nilsson UL, Frennesson C, Nilsson SE. Patients with AMD and a large absolute central scotoma can be trained successfully to use eccentric viewing, as demonstrated in a scanning laser ophthalmoscope. Vision Res. 2003;43:1777–1787. doi: 10.1016/s0042-6989(03)00219-0. [DOI] [PubMed] [Google Scholar]
- e9.Messias A, Reinhard J, Velasco e Cruz AA, Dietz K, MacKeben M. Trauzettel-Klosinski S: Eccentric fixation in Stargardt’s disease assessed by Tübingen perimetry. Invest Ophthalmol Vis Sci. 2007;48:5815–5822. doi: 10.1167/iovs.06-0367. [DOI] [PubMed] [Google Scholar]
- e10.Timberlake GT, Mainster MA, Peli E, Augliere RA, Essock EA, Arend LE. Reading with a macular scotoma. I. Retinal location of scotoma and fixation area. Invest Ophthalmol Vis Sci. 1986;27:1137–1147. [PubMed] [Google Scholar]
- e11.Altpeter E, Mackeben M, Trauzettel-Klosinski S. The importance of sustained attention for patients with maculopathies. Vision Research. 2000;40:1539–1547. doi: 10.1016/s0042-6989(00)00059-6. [DOI] [PubMed] [Google Scholar]
- e12.Mackeben M. Placement of new fixation locus after central vision loss is influenced by focal attention. Neuro-Ophthalmol. 2009;33:127–131. [Google Scholar]
- e13.Pilz K, Braun C, Altpeter E, MacKeben M, Trauzettel-Klosinski S. Modulation of visual stimulus discrimination by sustained focal attention: an MEG study. Invest Ophthalmol Vis Sci. 2006;47:1225–1229. doi: 10.1167/iovs.04-1338. [DOI] [PubMed] [Google Scholar]
- e14.Bischoff P, Lang J, Huber A. Macular sparing as a perimetric artifact. Am J Ophthalmol. 1995;199:72–80. doi: 10.1016/s0002-9394(14)73816-4. [DOI] [PubMed] [Google Scholar]
- e15.White JM, Bedell HE. The oculomotor reference in humans with bilateral macular disease. Invest Ophthal Vis Sci. 1990;31:1149–1161. [PubMed] [Google Scholar]
- e16.Sale A, De Pasquale R, Bonaccorsi J, Pietra G, Olivieri D, Berardi N, Maffei L. Visual perceptual learning induces long-term potentiation in the visual cortex. Neuroscience. 2011;172:219–225. doi: 10.1016/j.neuroscience.2010.10.078. [DOI] [PubMed] [Google Scholar]
- e17.Dutton GN, Jacobson LK. Cerebral visual impairment in children. Semin Neonatol. 2001;6:477–485. doi: 10.1053/siny.2001.0078. [DOI] [PubMed] [Google Scholar]
- e18.Hoyt CS. Visual function in the brain-damaged child. Eye. 2003;17:369–384. doi: 10.1038/sj.eye.6700364. [DOI] [PubMed] [Google Scholar]
- e19.Hoyt CS. Brain injury and the eye. Eye. 2007;21:1285–1289. doi: 10.1038/sj.eye.6702849. [DOI] [PubMed] [Google Scholar]
- e20.Crooks CY, Zumsteg JM, Bell KR. Traumatic brain injury: A review of practice management and recent advance. Physical Medicine and Rehabilitation Clinics of North America. 2007;18 doi: 10.1016/j.pmr.2007.06.005. [DOI] [PubMed] [Google Scholar]
- e21.Thurman D. New York: John Wiley and sons; 2001. The epidemiology and economics of head trauma; 327 pp. [Google Scholar]
- e22.Bonnet C. Copenhagen: C. & A. Philibert 1760; Essai analytique sur les facultés de l’âme. [Google Scholar]
- e23.Khan JC, Shahid H, Thurlby DA, Yates JR, Moore AT. Charles Bonnet syndrome in age-related macular degeneration: the nature and frequency of images in subjects with end-stage disease. Ophthalmic Epimemiol. 2008;15:202–208. doi: 10.1080/09286580801939320. [DOI] [PubMed] [Google Scholar]
- e24.MenonG J, Rahman I, Menon S, Dutton GN. Complex visual halluzinations in the visually impaired: The Charles Bonnet Syndrome. Survey Ophthalmol. 2003;48:58–72. doi: 10.1016/s0039-6257(02)00414-9. [DOI] [PubMed] [Google Scholar]
- e25.Teunisse RJ, Cruysberg JRM, Verbeek A, Zitman FG. The Charles Bonnet Syndrome: A large Prospective study in the Netherlands. A study of the prevalence of the Charles Bonnet syndrome and associated factors in 500 patients attending the University Department of Ophthalmology at Nijmegen. Brit J Psychiatr. 1995;166:254–267. doi: 10.1192/bjp.166.2.254. [DOI] [PubMed] [Google Scholar]
- e26.Vojnikovic B, Radeljak S, Dessardo S, et al. What associates Charles Bonnet syndrome with age-related macular degeneration? Coll Antropol. 2010;34:45–48. [PubMed] [Google Scholar]
- e27.Lotery A, Xu X, Zlatava G, Loftus J. Burden of illness, visual impairment and health resource utilisation of patients with neovascular age-related macular degeneration: results from the UK cohort of a five-country cross-sectional study. Br J Ophthalmol. 2007;91:1303–1307. doi: 10.1136/bjo.2007.116939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e28.Rovner BW, Casten RJ. Preventing late-life depression in age-related macular degeneration. Am J Geriatr Psychiatry. 2008;16:454–459. doi: 10.1097/JGP.0b013e31816b7342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e29.Virgili G, Acosta R. Reading aids for adults with low vision. Cochrane Database of Systematic Reviews. 2006;(4) doi: 10.1002/14651858.CD003303.pub4. Art. No.: CD003303. DOI: 10.1002/14651858.CD003302.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e30.Virgili G, Rubin G. Orientation and mobility training for adults with low vision. Cochrane Database of Systematic Reviews. 2010;(5) doi: 10.1002/14651858.CD003925.pub3. Art. No.: CD003925. DOI: 10.1002/14651858.CD003925.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e31.Barrett BT. A critical evaluation of the evidence supporting the practice of behavioural vision therapy. Ophthal Physiol Opt. 2009;29:4–25. doi: 10.1111/j.1475-1313.2008.00607.x. [DOI] [PubMed] [Google Scholar]
- e32.Zihl J, Krischer C, Meissen Z. Die hemianopische Lesestörung und ihre Behandlung. Nervenarzt. 1984;55 [PubMed] [Google Scholar]
- e33.Bolognini N, Rasi F, Coccia M, Làdavas E. Visual search improvement in hemianopia patients after audio-visual stimulation. Brain. 2005;128:2830–2842. doi: 10.1093/brain/awh656. [DOI] [PubMed] [Google Scholar]
- e34.Keller I, Lefin-Rank G. Improvement of visual search after audiovisual exploration training in hemianopic patients. Neurorehabilitation and Neural Repair. 2010;24:666–673. doi: 10.1177/1545968310372774. [DOI] [PubMed] [Google Scholar]
- e35.Lane AR, Smith DT, Ellison A, Schenk T. Visual exploration training is no better than attention training for treating hemianopia. Brain. 2010;133:1717–1728. doi: 10.1093/brain/awq088. [DOI] [PubMed] [Google Scholar]
- e36.Aulhorn E. Über Fixationsbreite und Fixationsfrequenz beim Lesen gerichteter Konturen. Pflügers Arch Physiol. 1953;257:318–328. doi: 10.1007/BF00363531. [DOI] [PubMed] [Google Scholar]
- e37.Legge GE, Ahn SJ, Klitz TS, Luebker A. Psychophysics of reading - XVI .The visual span in normal and low vision. Vision Research. 1997;37:1999–2010. doi: 10.1016/s0042-6989(97)00017-5. [DOI] [PubMed] [Google Scholar]
- e38.McConkie GW, Rayner K. Asymmetry of the perceptual span in reading. Bulletin of the Psychonomic Society. 1976;8:365–368. [Google Scholar]
- e39.Hahn GA, Penka D, Gehrlich C, et al. New standardised texts for assessing reading performance in four European languages. Brit J Ophthalmol. 2006;90:480–484. doi: 10.1136/bjo.2005.087379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e40.Stelmack JA, Massof RW, Stelmack TR. Is there a standard of care for eccentric viewing training? Journal of Rehabilitation Research & Development. 2004;41:729–738. doi: 10.1682/jrrd.2003.08.0136. [DOI] [PubMed] [Google Scholar]
- e41.Nilsson UL. Visual rehabilitation with and without educational training in the use of optical aids and residual vision. A prospective study of patients with advanced age-related macular degeneration. Clinical Vision Sciences. 1990;6:3–10. [Google Scholar]
- e42.Trauzettel-Klosinski S, Brendler K. Eye movements in reading with hemianopic field defects: the significance of clinical parameters. Graefe`s Arch Clin Exp Ophthalmol. 1998;236:91–102. doi: 10.1007/s004170050048. [DOI] [PubMed] [Google Scholar]
- e43.Trauzettel-Klosinski S. Eccentric fixation in hemianopic field defects - a valuable strategy to improve reading ability and an indication for cortical plasticity. Neuro - Ophthalmol. 1997;18:117–131. [Google Scholar]
- e44.Bouwmeester L, Heutink J, Lucas C. The effect of visual training for patients with visual field defects due to brain damage: a systematic review. J Neurol Neurosurg Psychiatry. 2007;78:555–564. doi: 10.1136/jnnp.2006.103853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e45.Friedburg C, Serey L, Sharpe LT, Trauzettel-Klosinski S, Zrenner E. Evaluation of the night vision spectacles on patients with impaired night vision. Graefe’s Arch Clin Exp Ophthalmol. 1999;237:125–136. doi: 10.1007/s004170050207. [DOI] [PubMed] [Google Scholar]
- e46.Rohrschneider K, Spandau U, Wechsler S, Blankenagel A. Einsatz einer neuen Nachtsichtbrille (DAVIS) Klin Monatsbl Augenheilk. 2000;217:88–93. doi: 10.1055/s-2000-10390. [DOI] [PubMed] [Google Scholar]
- e47.Kasten E, Wüst S, Behrens-Baumann W. Computer-based training for the treatment of partial blindness. Nat Med. 1998;4:1083–1087. doi: 10.1038/2079. [DOI] [PubMed] [Google Scholar]
- e48.Kerkhoff G. Neurovisuelle Rehabilitation nach Hirnschädigung. Ergotherapie. 2000;1:53–56. [Google Scholar]
- e49.Paul C. Reha-Sehtraining; Therapieleitfaden für Orthoptistinnen. Ravensburg: Praefcke. 1999 [Google Scholar]
- e50.Zihl J, von Cramon D. Restitution of visual function in patients with cerebral blindness. J Neurol Neurosurg Psychiatry. 1979;42:312–322. doi: 10.1136/jnnp.42.4.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e51.Balliet R, Blood KM, Bach-Y-Rita P. Visual field rehabilitation in the cortically blind? J Neurol Neurosurg Psychiatry. 1985;48:1113–1124. doi: 10.1136/jnnp.48.11.1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e52.Horton JC. Disappointing results from Nova Vision`s visual restoration therapy. British J Ophthalmol. 2005;89:1–2. doi: 10.1136/bjo.2004.058214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e53.Horton, JC Vision restoration therapy: confounded by eye movements. British J Ophthalmol. 2005;89:792–794. doi: 10.1136/bjo.2005.072967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e54.Schreiber A, Vonthein R, Reinhard J, Trauzettel-Klosinski S, Connert C, Schiefer U. Effect of visual restitution training on absolute homonymous scotomas. Neurology. 2006;67:143–145. doi: 10.1212/01.wnl.0000223338.26040.fb. [DOI] [PubMed] [Google Scholar]
- e55.Huxlin KR, Martin T, Kelly K, Riley M, Friedman D, Burgin WS, Hayhoe M. Perceptual relearning of complex visual motion after V1 damage in humans. J Neurosci. 2009;29:3981–3991. doi: 10.1523/JNEUROSCI.4882-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]