Abstract
Introduction
Malignant neoplasm of the colon is one of the most common gastrointestinal cancers and takes the second place in terms of incidence in the world. In Asian countries compared with Western countries the incidence is a bit lower. In recent years in Poland there has been a disturbing increase in the incidence of this cancer, particularly in the voivodships Mazowieckie, Slaskie, and Wielkopolskie.
Material and methods
Statistical data from the National Cancer Registry on the incidence of colorectal cancer in Poland in 1999-2008, including the provinces which are grouped into provinces of Eastern, Western and Central Poland. We analysed data on both men and women, with the division of colon cancer, rectal folds esico and rectum. The analysis took into account the recognized incidence in absolute numbers and age-standardized incidence rates.
Results
The incidence of colon cancer in 1999 was 3438 cases among men and 3476 women, while in 2008 this number increased in both men and women and for men was 4763, and 4340 for women. In all Polish provinces, in 1999, 2165 men and 1719 women, and in 2008, 3188 men and 2150 women suffered from rectal cancer.
Conclusions
In the years 1999-2008 there was an increase in incidence of cancer of the colon. In Poland, there are territorial differences in the incidence of colorectal cancer described by the standardized incidence ratio. The incidence in Western and Central Poland is generally higher than for Eastern Poland. Probably, these differences have multiple bases.
Keywords: cancer, colon, incidence, statistics, Poland, provinces
Introduction
Incidence is the incidence of new cases of the disease in the studied population (according to the Encyclopedia of Small Statistics). One of the most common cancers in both women and men is cancer of the colon. For both sexes it is the second most common cause of morbidity [1]. However, the prevalence of this disease remains higher in men than in women (35% lower in women) [2].
The most common location of colorectal cancer is the rectum. The disease is often diagnosed by accident or as a result of screening (rectoscopy, colonoscopy). Endoscopic assessment is the most effective method of early detection of neoplastic changes [3]. Delay in diagnosis and the degree of tumour invasion to adjacent tissues have a decisive influence on survival [4].
The epidemiological data suggest that the treatment undertaken in the early stages of the disease (stage A, B1, B2 Astler-Coller) gives a chance for 5-year survival in 90%, 85%, and 70% [1] of cases. The aetiology of this disease is not completely known, although research suggests a number of factors that could affect its development [5]. The most important are genetic factors, high-calorie diet rich in fats and low in fibre, eating highly processed foods containing preservatives and dyes, history of previous malignant or benign tumours of the colon (polyps), breast cancer, ovarian or uterine cancer in women with ulcerative colitis and Crohn’s disease [6]. Most cases are observed after 65 years of age [7]. Changes in incidence are differently shaped over time: in some countries of Northern and Western Europe the incidence is stabilizing or even gradually decreasing [8], while in others it is increasing [9].
In the UK, 106 new cases of colorectal cancer are diagnosed every day [10]. In the United States, colorectal cancer is the third most common cancer in both sexes. In 2005, colon cancer and rectal bending distal segment was diagnosed in 108,100 people and there were 40,800 cases of rectal cancer [11]. In Germany, in 2006 the total number of cases was 68,740 [12]. In France, after a steady increase until 1995, the incidence of colorectal cancer stabilised in both sexes, with a slight decrease in men. In 2010, the projected incidence was 36.5 per 100,000 in men and 24.4 in women [13].
The aim of this study was to analyse morbidity among women and men with cancer of the colon and rectum in Poland in the provinces grouped as Western, Central and Eastern Poland in 1999-2008.
Material and methods
The basis of this analysis was the incidence of cancer of the colon and rectum in the years 1999-2008, included in absolute numbers and described as the standardized incidence rate according to age. We analysed incidence rates for the number of cases per 100 thousand people and standardized so that the population age structure was the same as the population age structure adopted as a standard. The ‘standard world population’ was adopted as the standard population, and data about its structure derived from the annual newsletter ‘Cancer Incidence in Five Continents’, edited by Witold Zatoński and George Tyczyńskiego, issued by the Department of Epidemiology and Cancer Prevention – National Cancer Registry.
The analysis included the incidence by sex and provinces called: Western Poland (voivodship: Zachodniopomorskie, Lubuskie, Dolnośląskie, Greater Poland), Central Poland (Mazowieckie, Pomorskie, Kujawsko-pomorskie, Łódzkie, Świętokrzyskie, Lesser Poland, Silesia, Opole) and Eastern Poland (Warmińsko-mazurskie, Podlaskie, Lubelskie, Podkarpackie). By grouping the provinces the average incidence rate was calculated for the group of provinces based on the ratios for each province (arithmetic average). Statistical data were drawn from the National Institute of Hygiene in Warsaw.
Results
Tables I and II include the absolute incidence of colorectal cancer in the years 1999-2008, by gender and location of the cancer of the colon and rectum for cancer separately. Tables III to IV present the incidence of colorectal cancer by gender expressed as the standardized incidence rate of Poland's Western, Central and Eastern provinces in the years 1999-2008.
Table I.
Prevalence (in absolute terms) for colon cancer in men and women in Poland in 1999-2008
| Gender | Year | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | |
| Men | 3438 | 3345 | 3689 | 3675 | 4184 | 4205 | 4442 | 4486 | 4743 | 4763 |
| Women | 3476 | 3389 | 3583 | 3575 | 3882 | 3961 | 4123 | 4057 | 4254 | 4340 |
Table II.
Incidence (in absolute terms) of rectal cancer for men and women in Poland in 1999-2008
| Gender | Year | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | |
| Men | 2165 | 2474 | 2597 | 2685 | 2790 | 2716 | 3043 | 3075 | 3149 | 3188 |
| Women | 1719 | 1921 | 1881 | 2032 | 2061 | 1995 | 2092 | 2006 | 2098 | 2150 |
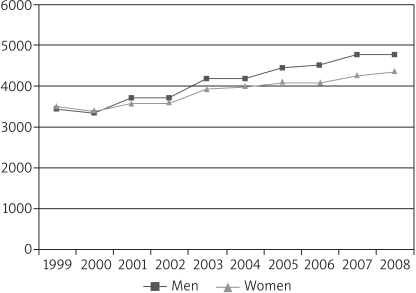
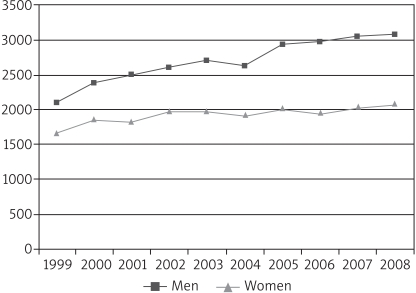
On the basis of data on incidence of cancer of the colon in the years 1999-2008 there can be observed a rise in incidence of cancer of the colon and rectum, both for women and men. In 1999, the incidence of colon cancer was 3438 for men and 3476 for women, and in 2008 respectively 4763 and 4340 (Table I, Figure 1). In 1999, 2165 men and 1719 women suffered from rectal cancer. In subsequent years, the incidence increased, reaching respectively 3188 and 2150 in 2008 (Table II, Figure 2).
Figure 1.
Incidence of colon cancer in men and women in Poland in 1999-2008
Figure 2.
Incidence of rectal cancer in men and women in Poland in 1999-2008
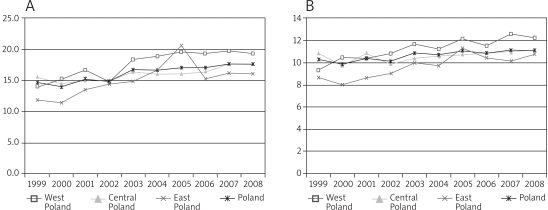
As is apparent from Tables IIIA and IIIB, in 1999 the highest standardized incidence rate for colon cancer is observed for Central Poland at 15.6 for men and 10.9 for women (above the Polish value of 14.6 for men and 10.3 for women), the lowest for Eastern Poland at 11.8 for men and 8.7 for women (below the Polish value). In Western Poland it reached the average level of 14.0 for men and 9.3 for women. In the years 1999-2008 there was an increase in the incidence rate among men, in 2008 amounting to 17.4 for Poland, 19.2 for Western, 17.6 for Central and 16.0 for Eastern Poland. The highest growth rate occurred for the Polish western provinces – a 5.2. For women in 1999-2008 the incidence rate increased and in 2008 reached the level of 11.1, and 12.2 for Western, 10.8 for Eastern, and 11.1 for Central Poland. Change rate trends in 1999-2008 are illustrated in Figures IIIA and IIIB.
Table IIIA.
Incidence of colon cancer in 1999-2008 (standardized coefficient) in Western, Central, Eastern Poland – men
| Region | Year | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | |
| West Poland | 14.0 | 15.1 | 16.6 | 14.7 | 18.3 | 18.8 | 19.4 | 19.1 | 19.5 | 19.2 |
| Central Poland | 15.6 | 14.4 | 15.0 | 15.0 | 16.4 | 16.1 | 15.9 | 16.3 | 17.7 | 17.6 |
| East Poland | 11.8 | 11.4 | 13.5 | 14.5 | 14.9 | 16.5 | 20.5 | 15.3 | 16.3 | 16.0 |
| Poland | 14.6 | 14.0 | 15.2 | 14.9 | 16.8 | 16.5 | 17.0 | 17.0 | 17.6 | 17.4 |
Table IIIB.
Incidence of colon cancer in 1999-2008 (standardized coefficient) in Western, Central, Eastern Poland – women
| Region | Year | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | |
| West Poland | 9.3 | 10.5 | 10.4 | 10.8 | 11.7 | 11.2 | 12.1 | 11.5 | 12.6 | 12.2 |
| Central Poland | 10.9 | 9.8 | 10.9 | 9.9 | 10.4 | 10.6 | 10.7 | 10.9 | 11.0 | 11.1 |
| East Poland | 8.7 | 8.0 | 8.6 | 9.0 | 10.0 | 9.7 | 11.3 | 10.5 | 10.1 | 10.8 |
| Poland | 10.3 | 9.9 | 10.4 | 10.1 | 10.9 | 10.7 | 11.1 | 10.9 | 11.1 | 11.1 |
Figure 3.
Incidence of colon cancer in 1999-2008 (standardized coefficient) for Western, Central, Eastern Poland. A – men, B – women
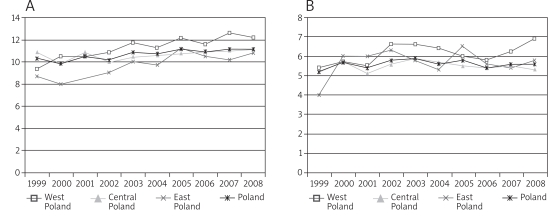
As is apparent from Table IVA and IVB, in 1999, the standardized incidence rate of rectal cancer (C20) was lower than that of colon cancer and showed little territorial difference, reaching in males the average level of 9.3 for the provinces of Western (10.1), Central (9.0) and Eastern Poland (7.9). For women, it reached respectively 5.4, 5.2, 5.1 and 4.0. In the years 1999-2008 there was an increase in incidence rate in both men and women, in 2008 reaching respectively for Polish males 11.8, in Western 12.6, Central 11.7, and Eastern Poland 12.6. For women the values were respectively 6.9, 5.3, and 5.8. Change rate trends in 1999-2008 are illustrated in Figures IVA and IVB.
Table IVA.
Incidence of rectal cancer (C20) in 1999-2008 (standardized coefficient) in Western, Central, Eastern Poland – men
| Region | Year | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | |
| West Poland | 10.1 | 11.3 | 11.4 | 12.4 | 11.8 | 11.4 | 13.5 | 12.6 | 13.1 | 12.6 |
| Central Poland | 9.0 | 10.5 | 10.6 | 11.1 | 11.0 | 11.0 | 11.5 | 11.4 | 11.5 | 11.7 |
| East Poland | 7.9 | 10.8 | 11.8 | 9.9 | 11.5 | 11.6 | 11.9 | 12.1 | 11.9 | 12.6 |
| Poland | 9.3 | 10.5 | 10.8 | 11.0 | 11.3 | 10.8 | 11.7 | 11.8 | 11.8 | 11.8 |
Table IVB.
Incidence of rectal cancer (C20) in 1999-2008 (standardized coefficient) in Western, Central, Eastern Poland – women
| Region | Year | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | |
| West Poland | 5.4 | 5.7 | 5.5 | 6.6 | 6.6 | 6.4 | 6.0 | 5.8 | 6.2 | 6.9 |
| Central Poland | 5.2 | 5.7 | 5.1 | 5.6 | 5.9 | 5.7 | 5.5 | 5.4 | 5.5 | 5.3 |
| East Poland | 4.0 | 6.0 | 6.0 | 6.3 | 5.8 | 5.3 | 6.5 | 5.6 | 5.4 | 5.8 |
| Poland | 5.2 | 5.7 | 5.4 | 5.8 | 5.9 | 5.6 | 5.8 | 5.4 | 5.6 | 5.6 |
Figure 4.
Incidence of rectal cancer (C20) in 1999-2008 (standardized coefficient) for Western, Central, Eastern Poland. A – men, B – women
Discussion
Malignant tumours of the colon are a major cause of morbidity and mortality world wide. They are more prevalent in developed countries than in developing countries, which may indicate a link with the horizontal life. In the UK every day 106 new cases of colon cancer are diagnosed [10]. In the United States, colorectal cancer is the third most common cancer in both sexes. In 2005, 108,100 people were diagnosed with colon cancer and rectal bending distal segment and 40,800 with rectal cancer [11]. In Germany, in 2006 the total number of cases stood at 68,740 [12]. There are differently shaped incidence changes over time: in some countries of Northern and Western Europe the incidence is stabilizing and even gradually decreasing [8], while in others it is increasing [9].
As is clear from the statistical data, colorectal cancer affects both sexes, but it is significantly more frequent in men, regardless of location of the tumour. In Poland, the epidemiological situation regarding this disease is alarming. Since 1999 we can observe an increase in incidence in both sexes expressed in absolute numbers. The rise in incidence rates is also illustrated by Polish and province groups standardized rates (with the exception of the above-mentioned colon cancer in women). In both locations, higher colorectal cancer incidence rates occur in men than in women, which indicates the relationship of this type of cancer with sex. Hormone substrate is considered one of the reasons for these differences.
In women, the first pregnancy at a young age, oral contraception and oestrogen replacement therapy are associated with reduced risk of developing colorectal cancer [14, 15]. In the Women's Health Initiative study, hormone replacement therapy showed 40% reduction in the risk of colorectal cancer [16]. In total, these data suggest that oestrogen and/or progestins protect against colon cancer. Territorial differences expressed in averaged standardized incidence rate for groups of provinces of Western, Central and Eastern Poland appear to be interesting. Thus, for colon cancer (C18) in 1999, the highest incidence rate (above the Polish figure) occurred in males in the Polish Central provinces.
However, by 2008 the growth rate was higher in Western and Eastern than in Central Poland. For women at the same time there was a slight drop in the rate in Central Poland and growth in Western (above the figure for Poland) and Eastern Poland (slightly below the Polish figure). In the case of rectal cancer (C20) in 1999, the highest incidence rate occurred in Western Poland, for both men and women (above the Polish value), as was also the case in 2008.
For the years 1999-2008 between the Western, Central and Eastern Polish provinces there are territorial differences in the incidence of colorectal cancer (expressed as the mean standardized incidence ratio), but higher incidence generally refers to the Western and Central Polish provinces rather than Eastern Poland.
The explanation for the observed differences requires further territorial epidemiological studies. They may depend on factors affecting the increased incidence of cancer (e.g., diet, socioeconomic status, genetic factors) as well as on factors affecting the rate of detectability (e.g., access to screening, patients' awareness, experience, doctors).
Summarizing the above results, we can conclude that for the two locations of colon cancer, increased incidence is observed for cancers of the colon, and it occurs more often in men than in women. Perhaps this is due to a diet rich in fats, particularly animal fats, which not only causes obesity, but also increases the risk for colon cancer. Drinking too much alcohol and smoking also may play a role in the development of colorectal cancer [17]. Smokers are 20-30% more likely to die of colon cancer than non-smokers [18]. Differences in the incidence of colorectal cancer among men and women may result from differential expression of oestrogen receptors, which may play a significant role in the pathogenesis of this tumour.
Oestrogens are used to reduce menopausal symptoms and for preservation of bone mineral density. Recent epidemiological studies suggest that combined oestrogen and progestin in hormone replacement therapy reduces the incidence of colorectal cancer in postmenopausal women [19, 20]. Other epidemiological studies suggest that oestrogen withdrawal increases the risk of MSI-positive colorectal cancer [21]. Therefore, hormone replacement therapy plays such a prominent role and oestrogens seem to have a protective effect against this type of cancer.
In conclusion, the increase in the incidence of colorectal cancer may be the result of the increased availability of endoscopic examinations. The differences in incidence between western and eastern Poland may result from the better economic situation of inhabitants of the west, and hence of a diet rich in conserved foods. Lack of territorial differences in the number of cases in Poland may be the result of the general access to rectoscopic examination throughout the country. The differences in the incidence of colorectal cancer among men and women may be associated with the hormonal substrate.
Testing for colon cancer may be relevant to the analysis of the causes of territorial differences in the incidence of mortality. Differences in mortality may, inter alia, indicate the dominant role of either dietary factors or the availability of medical care. Irrespective of the epidemiological studies, the results of many years of genetic research can play an important role in the analysis of the causes of morbidity of colorectal cancer.
References
- 1.Didkowska J, Wojciechowska H, Tarnowski W, Katonski WA. Nowotwory złośliwe w Polsce w 2000 roku. Warszawa: Centrum Onkologii – Instytut; 2003. [Google Scholar]
- 2.American Cancer Society. Colorectal Cancer Facts and Figures Special Edition. Atlanta, GA: American Cancer Society; 2005. [Google Scholar]
- 3.Macafee DAL, Scholefield JH. Population based endoscopic screening for colorectal cancer. Gut. 2003;52:323–6. doi: 10.1136/gut.52.3.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lenin B. Colorectal cancer. ACP Medicine. Available at: http://www.medscape.com/view-article/502838 . 2005.
- 5.Chao A, Thun MJ, Connell CJ, et al. Meat consumption and risk of colorectal cancer. JAMA. 2005;293:172–82. doi: 10.1001/jama.293.2.172. [DOI] [PubMed] [Google Scholar]
- 6.Eaden JA, Abrams KR, Mayberry JF. The risk of colorectal cancer in ulcerative colitis: a meta-analysis. Gut. 2001;48:526–35. doi: 10.1136/gut.48.4.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Herman RM. Proctologic. 2008;9:30. [Google Scholar]
- 8.Jemal A, Hun MJ, Ries LA, et al. Annual report to the nation on the status of cancer 1975-2005, featuring trends in lung cancer, tobacco use, and tobacco control. J Natl Cancer Inst. 2008;100:1672–94. doi: 10.1093/jnci/djn389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Center MM, Jemal A, Smith RA, Ward E. Worldwide variations in colorectal cancer. CA Cancer J Clin. 2009;59:366–78. doi: 10.3322/caac.20038. [DOI] [PubMed] [Google Scholar]
- 10.http://www.infocancerresearchk.org .
- 11.Fatima A, Hangar Robin P. Boushey, incidence, mortality, survival, and risk factors. Clin Colon Rectal Surg. 2009;22:191–7. doi: 10.1055/s-0029-1242458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brener H, Altenhofen L, Hoffmeister M. Eight years of colonoscopic bowel cancer screening in Germany initial findings and projections. Dtsch Arztebl Int. 2010;107:753–9. doi: 10.3238/arztebl.2010.0753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jooste V, Remontet L, Colonna M, et al. Trends in the incidence of digestive cancers in France between 1980 and 2005 and projections for the year 2010. Eur J Cancer Prev. 2011 Apr 6; doi: 10.1097/CEJ.0b013e3283465426. [DOI] [PubMed] [Google Scholar]
- 14.Calle EE, Miracle-McMahill HL, Thun MJ, Heath CW., Jr Estrogen replacement therapy and risk of fatal colon cancer in a prospective cohort of postmenopausal women. J Natl Cancer Inst. 1995;87:517–23. doi: 10.1093/jnci/87.7.517. [DOI] [PubMed] [Google Scholar]
- 15.Broeders MJ, Lambe M, Baron JA, Leon DA. History of childbearing and colorectal cancer risk in women aged less than 60: an analysis of Swedish routine registry data 1960-1984. Int J Cancer. 1996;66:170–5. doi: 10.1002/(SICI)1097-0215(19960410)66:2<170::AID-IJC5>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 16.Macafee DAL, Scholefield JH. Population based endoscopic screening for colorectal cancer. Gut. 2003;52:323–6. doi: 10.1136/gut.52.3.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Banasaz M, Norin E, Midtvedt T. reference title. Microb Ecol Health Dis. 2001;13:135–42. [Google Scholar]
- 18.http://creativecommons.org/licenses/by/2.5/
- 19.Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women's Health Initiative randomized controlled trial. J Am Med Assoc. 2002;288:321–33. doi: 10.1001/jama.288.3.321. [DOI] [PubMed] [Google Scholar]
- 20.Nelson HD, Humphrey LL, Nygren P, Teutsch SM, Allan JD. Postmenopausal hormone replacement therapy: scientific review. J Am Med Assoc. 2002;288:872–81. doi: 10.1001/jama.288.7.872. [DOI] [PubMed] [Google Scholar]
- 21.Slattery ML, Potter JD, Curtin K, et al. Estrogens reduce and withdrawal of estrogens increase risk of microsatellite instability-positive colon cancer. Cancer Res. 2001;61:126–30. [PubMed] [Google Scholar]