Abstract
The present case report describes a patient with an artificial mitral valve and dual chamber pacemaker implanted due to perioperative complete atrio-ventricular block. One year later an upgrade to cardiac resynchronization therapy (CRT) combined with ICD function was performed due to significant progression of heart failure symptoms. Beneficial effects of CRT are demonstrated, but unfavourable haemodynamic consequences of right atrial appendage pacing are also underlined. Important interatrial conduction delay during atrial paced rhythm resulted in a significant time difference between optimal sensed and paced atrio-ventricular delay (AVD). This report provides a practical outline how to determine the interatrial delay and the sensed-paced AVD offset under echocardiography in patients treated with CRT.
Keywords: cardiac resynchronization therapy, atrio-ventricular delay, echocardiography, atrial pacing, heart failure
Introduction
Cardiac resynchronization therapy (CRT) is an effective treatment in patients with medically refractory heart failure, severe left ventricular (LV) dysfunction, and prolonged QRS duration [1]. The response to CRT depends on several factors, including device settings. Optimally programmed atrio-ventricular delay (AVD) can affect the acute haemodynamic response and may influence the magnitude of clinical improvement under chronic pacing [2]. There are scarce data regarding the AVD optimization in CRT patients during atrial-paced compared with atrial-sensed biventricular pacing. The present case report shows how to determine the optimal AVD during echocardiographic examination and underlines possible marked differences between atrial-sensed and atrial-paced rhythms in CRT patients.
Case report
A 55-year-old white male had an artificial mitral valve implanted due to severe mitral insufficiency in the course of the degenerative process, and a dual chamber pacemaker because of perioperative third degree atrio-ventricular block. One year later he was admitted to our hospital because of chronic heart failure exacerbation (NYHA III). Before admission the patient was treated with bisoprolol 5 mg, perindopril 10 mg, spironolactone 25 mg and furosemide 80 mg. Intravenous furosemide (120 mg) and spironolactone (100 mg) were administered. The ECG showed permanent VAT pacing (atrially triggered ventricular pacing) of 67 bpm. Echocardiography demonstrated normal artificial mitral valve function, depressed LV ejection fraction (27%), enlarged LV end-diastolic (62 mm) and left atrial diameter (50 mm), preserved atrio-ventricular synchrony, but prominent interventricular and intra-LV dyssynchrony (Table I). Coronary angiography revealed no abnormalities. Five days after admission the patient successfully underwent the DDD pacemaker upgrade to CRT-D (Boston Scientific, Cognis 100-D) with the defibrillating lead placed in the right ventricular apex, LV lead in the postero-lateral vein and the previously implanted atrial lead remained in the right atrial appendage (RAA). A week after implantation the patient improved significantly (NYHA II), the LV ejection fraction was 33%, and mechanical dyssynchrony diminished (Table I). The device was optimized under echocardiography. The greatest aortic velocity time integral and the lowest interventricular mechanical delay (IVMD) were obtained with 30 ms LV pre-excitation. The resting AVD was optimized to provide the longest transmitral filling time without A wave truncation from pulsed wave Doppler analysis of the LV filling [2]. The optimal AVD during atrial-sensed rhythm (70-72 bpm) was 30 ms, which was the shortest AVD available in the device (Figure 1). In contrast, the optimal AVD during atrial-paced rhythm (75 bpm) was as long as 190 ms (Figure 2). Biventricular capture with AVD 190 ms was confirmed by the constant value of IVMD and unchanged QRS morphology on the ECG. Interatrial delay (IAD) during atrial-paced rhythm (75 bpm) was 140 ms (Figure 3). During atrial-sensed rhythm the IAD was 50 ms. In the Cognis 100-D device the greatest sensed-paced offset of the AVD is 100 ms. The CRT-D device was programmed in the DDD mode with a basic rate of 60 bpm to promote the VAT pacing, with the sensed AVD of 30 ms and paced AVD of 130 ms. As Holter monitoring had revealed so far predominant atrial-sensed rhythm (80% in the VAT mode) we concentrated on the optimal sensed AVD. Additionally, as the incidence of atrial fibrillation in CRT recipients may be related to the percentage of atrial paced rhythm, we decided to promote native atrial rhythm in this patient [3]. After 6 months the patient was still in NYHA II.
Table I.
Clinical and echocardiographic parameters before and after upgrading to cardiac resynchronization therapy (CRT) and device optimization
| Parameters | Before CRT implantation | 7 days after CRT | ||||
|---|---|---|---|---|---|---|
| Nominal VVD/AVD | LV+30 Nominal AVD | LV+30 Atrial sensed rhythm (optimal AVDs 30 ms) | LV+30 Atrial paced rhythm (optimal AVDp 190 ms) | |||
| Heart failure functional class | (NYHA) | III | II | |||
| Heart rate [bpm] | 67 | 70-72 | 75 | |||
| Left atrial dimension [mm] | (N: 19-40) | 50 | 48 | |||
| IVS wall thickness [mm] | (N: 6-11) | 13 | 13 | |||
| Posterior wall thickness [mm] | (N: 6-11) | 13 | 13 | |||
| LVEDD [mm] | (N: 37-56) | 62 | 62 | |||
| LVESD [mm] | (N: 21-40) | 47 | 45 | |||
| LVEDVI [ml/m2] | (N: 50-90) | 75 | 75 | |||
| LVEDV/LVESV [ml] | 128/93 | 128/83 | ||||
| LV ejection fraction [%] | (N: 59-74) | 27 | 35 | |||
| Right ventricle [mm] | (N < 28) | 29 | 29 | |||
| RVSP [mmHg] | (N < 33) | 33 | 33 | |||
| Haemodynamic measurements: | ||||||
| Aortic VTI [cm] | 17.5 | 22.0 | 22.3 | 22.5 | 21.7 | |
| CO [l/min] | 2.35 | 3.10 | 3.21 | 3.24 | 3.25 | |
| Dyssynchrony assessment: | ||||||
| DFTLV [ms/%RR] | (N > 40%) | 420/47 | 260/31 | 260/31 | 313/38 | 360/45 |
| IAD [ms] | (N < 30) | 50 | Monophasic mitral inflow | 50 | 140 | |
| IVMD [ms] | (N < 20) | 60 | 37 | 20 | 20 | 20 |
| Septo-posterior wall motion delay [ms] | (N < 70) | 250 | 200 | 180 | 180 | 180 |
| Paradoxical motion of the distal IVS | + | – | – | – | – | |
| Paradoxical apical motion (“apical shuffle”) | + | – | – | – | – | |
IVS – interventricular septum, LV – left ventricle, LVEDD/LVESD – LV end-diastolic/end-systolic diameter, LVEDVI – LV end-diastolic volume index, LVEDV/LVESV – LV end-diastolic/end-systolic volume, VTI – velocity time integral, RVSP – right ventricular systolic pressure, DFTLV – LV diastolic filling time (in ms and as percentage of the RR interval), IAD – interatrial delay, IVMD – interventricular mechanical delay, nominal VVD/AVD – simultaneous biventricular pacing/atrio-ventricular delay paced (AVDp) 180 ms/sensed (AVDs) 120 ms, LV+30 – LV pre-excitation of 30 ms
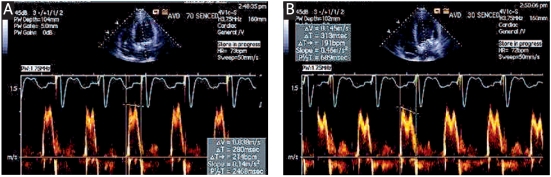
Figure 1.
Atrio-ventricular delay optimization during the atrial-sensed rhythm (70-72 bpm) according to mitral inflow velocity waveforms. A – AVD of 70 ms was too long, as diastolic filling time (DFTLV) was only 280 ms (34% of the RR interval), E and A wave fusion was present. B – with AVD of 30 ms the DFTLV was prolonged to 313 ms (38% of the RR interval)
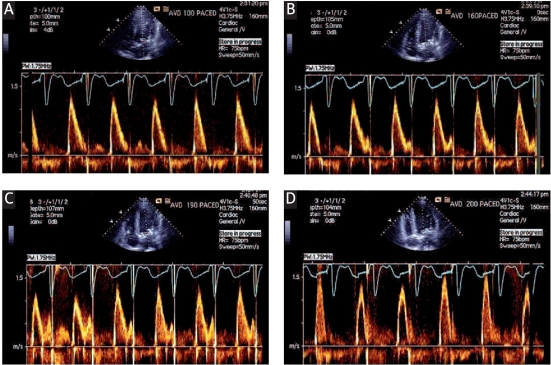
Figure 2.
Atrio-ventricular delay optimization during the atrial-paced rhythm (75 bpm) according to mitral inflow velocity waveforms. A – AVD paced at 100 ms was too short – monophasic mitral inflow was present, B – starting with AVD paced at 160 ms a tiny atrial A-wave appeared, C – AVD paced at 190 ms was optimal since it provided the longest DFTLV without atrial A-wave truncation, D – with AVD paced at 200 ms and longer, truncation of the atrial A-wave was present
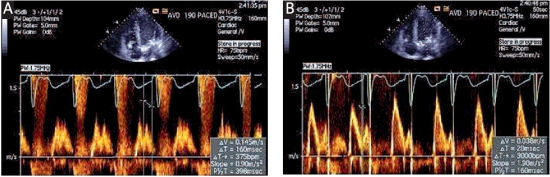
Figure 3.
Interatrial delay assessment during the atrial-paced rhythm (75 bpm). Registration of the tricuspid (A) and mitral (B) inflow during apnoea and the difference between the beginning of the right and left atrial A-wave was calculated: 160 ms – 20 ms = 140 ms
Discussion
Cardiac resynchronization therapy is an effective treatment in heart failure patients, especially if significant mechanical dyssynchrony is present [4]. Unfortunately, one-third of these patients do not derive clinical benefit from CRT. Atrial conduction abnormalities and suboptimal device programming are factors which determine the final outcome [5].
After un upgrade to CRT the patient’s functional class, mechanical synchrony and LV ejection fraction improved significantly. However, optimization of the AVD during atrial sensed and paced rhythm revealed a huge difference between these two settings. The nominal value for atrial sensed-paced offset in the Cognis 100-D device is 60 ms. Previous studies [6] have underlined that even greater offset could be haemodynamically beneficial in CRT patients, but it varies widely among patients. The RAA is the standard site for atrial lead implantation, but pacing from this region may induce and/or aggravate pre-existing interatrial conduction disturbances. Physiological mechanical IAD determined by echocardiography is less than 30 ms [7]. In our patient the native IAD, determined during atrial sensed-rhythm, was prolonged to 50 ms and it was further elongated to 140 ms during atrial-paced rhythm. It resulted in a 160 ms time difference between the optimal paced and sensed AVD, which was impossible to program. In our patient, apart from the atrial pacing site, left atrial enlargement in the course of mitral insufficiency could have been a factor of the IAD prolongation. Atrial lead placement in the interatrial septum (preferentially in the Bachmann’s bundle region) could have obviated the huge sensed-paced AVD offset [7].
Acknowledgments
The authors declare no conflict of interests.
References
- 1.Bristow MR, Saxon LA, Boehmer J, et al. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med. 2004;350:2140–50. doi: 10.1056/NEJMoa032423. [DOI] [PubMed] [Google Scholar]
- 2.Bhan A, Kapetanakis S, Monaghan MJ. Optimization of cardiac resynchronization therapy. Echocardiography. 2008;25:1031–9. doi: 10.1111/j.1540-8175.2008.00789.x. [DOI] [PubMed] [Google Scholar]
- 3.Adelstein E, Saba S. Right atrial pacing and the risk of postimplant atrial fibrillation in cardiac resynchronization therapy recipients. Am Heart J. 2008;155:94–9. doi: 10.1016/j.ahj.2007.08.030. [DOI] [PubMed] [Google Scholar]
- 4.Shen X, Aronow WS, Anand K, et al. Clinical research evaluation of left ventricular dyssynchrony using combined pulsed wave and tissue Doppler imaging. Arch Med Sci. 2010;6:519–25. doi: 10.5114/aoms.2010.14462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Piotrowski G, Szymanski P, Banach M, et al. Left atrial and left atrial appendage systolic function in patients with post-myocardial distal blocks. Arch Med Sci. 2010;6:892–9. doi: 10.5114/aoms.2010.19298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gold MR, Niazi I, Giudici M, et al. Acute hemodynamic effects of atrial pacing with cardiac resynchronization therapy. J Cardiovasc Electrophysiol. 2009;20:894–900. doi: 10.1111/j.1540-8167.2009.01460.x. [DOI] [PubMed] [Google Scholar]
- 7.Dabrowska-Kugacka A, Lewicka-Nowak E, Rucinski P, Kozlowski D, Raczak G, Kutarski A. Single-site Bachmann’s bundle pacing is beneficial while coronary sinus pacing results in echocardiographic right heart pacemaker syndrome in brady-tachycardia patients. Circulation J. 2010;74:1308–15. doi: 10.1253/circj.cj-09-0846. [DOI] [PubMed] [Google Scholar]