Abstract
Introduction
The aim of our study was to compare the effects of isobaric and hyperbaric bupivacaine combined with morphine or fentanyl in patients undergoing caesarean section. We assessed quality and spread of analgesia and anaesthesia, postoperative analgesic requirement and side effects.
Material and methods
Hundred patients with American Society of Anesthesiologists physical status (ASA) I-II, age 18 to 40 years, were randomized to 4 groups. The intrathecal solutions were isobaric bupivacaine + morphine (group A), isobaric bupivacaine + fentanyl (group B), heavy bupivacaine + + morphine (group C) and heavy bupivacaine + fentanyl (group D). Mean arterial pressure, heart rate, oxygen saturation, ephedrine consumption, analgesic requirement time and additional analgesic needs were recorded.
Results
The 1st min value of mean arterial pressure was the lowest one in all groups. Heart rate decreased significantly in group A at the 10th min but not in the other groups. The decrease of visual analogue scale (VAS) pain scores began in the groups after the 4th postoperative h (p < 0.05) and the VAS value of group B at the 8th h was significantly higher than the other groups. The first analgesic requirement time in the postoperative period was longer in patients who had intrathecal morphine than those who had fentanyl. The duration of analgesia with isobaric bupivacaine and morphine was the longest one.
Conclusions
We concluded that intrathecal morphine provides a long duration of postoperative analgesia but the duration gets longer when it is combined with plain bupivacaine instead of heavy bupivacaine.
Keywords: opioid, combined spinal, caesarean, analgesia, bupivacaine
Introduction
Combined spinal epidural anaesthesia (CSEA) is nowadays a popular technique in obstetric and gynaecological surgery, including caesarean delivery [1]. Combined spinal epidural anaesthesia involves intentional subarachnoid blockade and epidural catheter placement during the same procedure. Advantages include rapid onset, profound neuraxial block, the ability to titrate or prolong blockade, lower total drug dosages, higher level of patient satisfaction and decreased incidence of accidental dural puncture [2, 3]. Sensorial blockade level is important for successful anaesthesia. The factors that effect the sensorial blockade are baricity, dose, volume and concentration of local anaesthetics, barbotage and demographic properties of patients such as weight, height or age. Baricity is the most important factor for local anaesthetic distribution. According to baricity conception, isobaric solutions remain in the proximity of the injection site and hyperbaric solutions gravitate to dependent areas [4]. The duration of spinal anaesthesia is related to the dose of hyperbaric or isobaric local anaesthetics administered. The relationship between dose, volume, and concentration of intrathecal local anaesthetics and the sensory spread of anaesthesia has been extensively studied using isobaric local anaesthetics [5].
Bupivacaine is an amide local anaesthetic with a moderately rapid onset and long duration of action. Isobaric bupivacaine is formulated using normal saline as a diluent with a specific gravity of 1000 at 37°C. Hyperbaric bupivacaine in 8% glucose has a specific gravity of 1021 at 37°C. Both isobaric and hyperbaric bupivacaine have been used for spinal anaesthesia with good results [6]. Hyperbaric bupivacaine attains higher sensory levels of intrathecal anaesthesia than equal doses of plain bupivacaine. Plain bupivacaine is unpredictable in its behaviour, often spreading to cervical dermatomal levels [7]. The addition of opioids to local anaesthetics for spinal anaesthesia is increasingly common both to enhance anaesthesia and to provide postoperative analgesia [8]. The dose of local anaesthetics can be reduced by adding opioids. On the other hand, the incidence of side effects decreases because of lower doses. Small doses of opioids administered to the central nervous system provide adequate analgesia, reducing the side effects of intravenous analgesic administration. Pruritus, nausea and vomiting or respiratory depression are some examples [9]. This adjuvant analgesic technique is expected to decrease postoperative pain intensity and opioid requirements and to speed up recovery. Intrathecal morphine, which is less hydrophobic than other opioids, has a longer residence time in the cerebrospinal fluid and provides excellent post-operative analgesia [10]. Decades of clinical use demonstrate clear differences between morphine and mu-opioid receptor agonist fentanyl in time course and dermatomal extent of analgesia [11]. According to experimental studies [12], intrathecally administered fentanyl is cleared from cerebrospinal fluid within a relatively short distance, whereas morphine extends to a much greater dermatomal distribution.
The aim of our study was to compare the effects of the baricity of bupivacaine combined with morphine or fentanyl for spinal anaesthesia in patients undergoing caesarean section. We assessed the quality and spread of analgesia and anaesthesia, postoperative first analgesic requirement time and side effects.
Material and methods
After approval by our local research and the regional ethics committee and informed patient written consent, 100 unpremedicated patients with ASA physical status I-II, aged 18 to 40 years, were included in this randomized, double-blind, prospective study. The patients were scheduled for elective caesarean section under spinal anaesthesia and they also had epidural analgesia after the operation for postoperative analgesia with a CSEA technique. Extremely obese parturients (body mass index – BMI > 40 kg/m2), and patients who refused to join the study, had contraindications for neuraxial block, had cardiovascular or respiratory disorders or had an unsuccessful spinal block were excluded from the study. The anaesthetists who performed the CSEA collected the data and the patients were blinded to the solutions.
Before the spinal block, a peripheral venous cannula was placed and i.v.infusion of 6% hydroxyethyl starch 130/0.4 in 0.9% sodium chloride solution 10 ml/kg was started for fluid loading. No vasopressors were administered before the procedure.
In all patients, using an aseptic technique in the sitting position, 2 ml of 1% lidocaine was infiltrated into the subcutaneous area of the lumbar 4-5 interspace. The epidural space was identified by the loss of resistance technique with 0.9% saline solution using an 18-gauge Tuohy needle. A spinal tap was performed using a 27-gauge Quincke spinal needle which was introduced inside the Tuohy needle. After injection of study drugs, a 20G soft tip epidural catheter with 3 lateral eyes (Perifix®, B Braun Melsungen Ag, D-Melsungen) was introduced 6 cm into the epidural space for postoperative analgesia in all patients.
Patients were randomized to 4 groups according to the intrathecal drugs injected by using computer-generated randomization table as:
group A: intrathecal 0.5% isobaric bupivacaine 9 mg + morphine sulfate 200 µg,
group B: intrathecal 0.5% isobaric bupivacaine 9 mg + fentanyl 25 µg,
group C: intrathecal 0.5% heavy bupivacaine 12.5 mg + morphine sulfate 200 µg,
group D: intrathecal 0.5% heavy bupivacaine 12.5 mg + fentanyl 25 µg.
Sensory blockade was assessed using the cold sensation test on each side of the midclavicular line. The degree of motor blockade was scored from 0 to 3 by the Bromage scale (0 – no motor effects, 1 – a decrease in muscle strength with ability to move the leg against pressure, 2 – inability to move the leg against pressure without complete paralysis, and 3 – unable to move feet or knees) at 1 h, 2 h, 4 h, 8 h, 12 h and 24 h.
Non-invasive mean arterial blood pressure was recorded with 1 min intervals. Heart rate, arterial oxygen saturation by pulse oximetry and respiratory rate were continuously measured. Finally, total ephedrine consumption, the duration of operation, first analgesic requirement time and additional analgesic needs were recorded. Pain scores were assessed by VAS. A score of 0 meant ‘no pain’ and 100 meant ‘the worst possible pain’. The patients who had a postoperative VAS score above 30 were administered a bolus dose of epidural solution in a volume of 9 cc via an epidural catheter. The epidural bolus solution contained 3.6 cc of 0.5% isobaric bupivacaine, 3 mg of morphine sulfate and 2.4 cc of saline. Thereby the concentration of bupivacaine was 0.2%. All patients received at least one time analgesic in the first postoperative 24 h. Then the number of patients who required the epidural analgesic a second time was recorded as additional analgesic need. The additional analgesic need was provided by epidural bolus solution. The epidural catheter was removed at the end of the 24th h. In all patients 75 mg of diclophenac sodium intramuscularly was administered every 12 h.
Maternal hypotension was defined as systolic arterial pressure < 90 mmHg or when decreased more than 25% from the baseline value and was treated by increasing the intravenous infusion rate and, if necessary, administering ephedrine 10 mg i.v. Patients who required fluids and vasopressors were considered to have hypotension. 0.01 mg/kg of i.v. atropine was administered for a heart rate below 45 beats/min.
Sedation and nausea and vomiting were also recorded postoperatively. The level of sedation was assessed with the Ramsey scale (1 – anxious, agitated, restless, 2 – cooperative, oriented, tranquil, 3 – responds to comments only, 4 – brisk response to light glabellar tap or loud noise, 5 – sluggish response to light glabellar tap or loud noise, 6 – no response). Postoperative nausea and vomiting was assessed with a two-point scale (0 – no episode, 1 – at least one episode).
Statistical analysis
Statistical Package for Social Sciences (SPSS) for Windows 10.0 programme was used for statistical analysis. The main outcome of our study was a 25% increase in the first analgesic requirement time. Group size was selected by using proportions sample size estimates (α: 0.05, β: 0.09). The values were expressed as mean ± SD.
One-way ANOVA parametric test was used for comparisons between groups for normal distributed parameters; the post-hoc test was Tukey Kramer. Kruskal Wallis and Mann-Whitney U statistical tests were used for non-normally distributed parameters; the post-hoc test was Dunn. Qualitative data were compared using the χ2 test (p < 0.05). A p > 0.05 was considered significant.
Results
There were no differences between groups regarding their age, weight, height or duration of surgery (p > 0.05) (Table I). One patient in group B was excluded because of an accidental dural puncture by the Tuohy needle and 1 patient in group D was excluded because of unsuccessful spinal blockade. Another 2 patients were included and a total of 100 patients were analysed.
Table I.
Patient demographics and duration of surgery (mean ± SD)
| Parameters | Group A | Group B | Group C | Group D |
|---|---|---|---|---|
| Age [year] | 26 ±6.06 | 25.92 ±4.22 | 25.92 ±4.68 | 27.92 ±4.58 |
| Weight [kg] | 73.76 ±7.16 | 72.52 ±7.68 | 72.84 ±8.57 | 75 ±8.15 |
| Duration of surgery [min] | 31.56 ±6.69 | 29.52 ±6.38 | 26.96 ±5.41 | 30 ±6.45 |
| Height [cm] | 163.44 ±4.01 | 162.88 ±5.16 | 163.12 ±4.12 | 163.64 ±3.04 |
p > 0.05, group A (n = 25): intrathecal 0.5% isobaric bupivacaine 9 mg + morphine sulfate 200 µg, group B (n = 25): intrathecal 0.5% isobaric bupivacaine 9 mg + fentanyl 25 µg, group C (n = 25): intrathecal 0.5% heavy bupivacaine 12.5 mg + morphine sulfate 200 µg, group D (n = 25): intrathecal 0.5% heavy bupivacaine 12.5 mg + fentanyl 25 µg
The mean arterial pressure decreased significantly at the 1st min in all groups but no statistically significant difference was seen between groups, as shown in Figure 1 (p > 0.05). Heart rate decreased significantly in group A at the 10th min but not in the other groups (p < 0.05) (Figure 2). There was no statistically significant difference between groups according to the incidence of nausea and vomiting or ephedrine requirement (Tables II and III).
Figure 1.
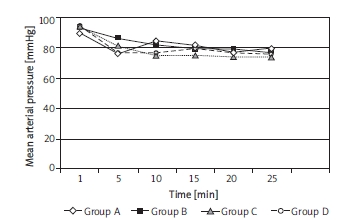
Mean arterial pressure values after spinal blockade
Figure 2.
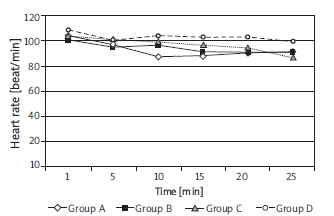
Heart rate values after spinal blockade
Table II.
Nausea and vomiting incidence (%)
| Group A | Group B | Group C | Group D | |
|---|---|---|---|---|
| Yes | 3 (12) | 2 (8) | 2 (8) | 2 (8) |
| No | 22 (88) | 23 (92) | 23 (92) | 23 (92) |
p > 0.05
Table III.
Ephedrine requirement (mean ± SD)
| Group A | Group B | Group C | Group D | |
|---|---|---|---|---|
| Ephedrine requirement [mg] | 10 ±9.57 | 5.2 ±10.84 | 6.8 ±9.45 | 10.8 ±10.37 |
p > 0.05
The main spread of analgesia and anaesthesia was similar between groups (p > 0.05). Patients' assessment of sensory levels after spinal anaesthesia changed within the range of T4 to T12. Bromage scales at the initial period were 3 for all patients; the quality of spinal analgesia was sufficient and no patient required analgesic supplementation during the surgery. None of the patients required additional medication throughout the operation or during data collection. There were no side effects or complications observed due to the procedure. No postdural puncture headache or neurological deficits were observed.
The decrease of VAS scores began in the groups after the postoperative 4th h (p < 0.05) and VAS values of group B at the 8th h were significantly higher than the other groups (Table IV).
Table IV.
Comparison of postoperative pain scores (VAS) (values are means)
| Postoperative time [h] | Group A | Group B | Group C | Group D |
|---|---|---|---|---|
| 1st | 6.8 ±8.52 | 8.4 ±8.50 | 7.6 ±9.25 | 5.6 ±8.20 |
| 2nd | 24.8 ±15.30 | 36 ±23.09 | 27.2 ±14.86 | 27.2 ±16.46 |
| 4th | 25.2 ±20.84 | 24.4 ±24.33 | 20 ±21.99 | 21.6 ±17.70 |
| 8th | 4.4 ±7.68 | 10.8 ±11.87 * | 5.2 ±6.53 | 4.0 ±8.16 |
| 12th | 9.2 ±11.15 | 7.6 ±14.23 | 11.2 ±14.23 | 7.6 ±12.34 |
| 24th | 7.2 ±6.78 | 3.6 ±5.68 | 7.6 ±7.23 | 5.2 ±5.85 |
Between groups p < 0.05
The patients who received heavy bupivacaine and morphine sulfate required more epidural analgesics in the postoperative period. However, this result did not constitute any statistically significant difference (Table V). The number of demands are seen in Table V. None of the patients required epidural analgesic solution more than 2 times. The duration of analgesia by isobaric bupivacaine with morphine was the longest time (Figure 3).
Table V.
Additional analgesic requirement
| Group A | Group B | Group C | Group D | |
|---|---|---|---|---|
| Yes | 1 (4%) | 1 (4%) | 3 (12%) | 2 (8%) |
| No | 24 (96%) | 24 (96%) | 22 (88%) | 23 (92%) |
p > 0.05
Figure 3.
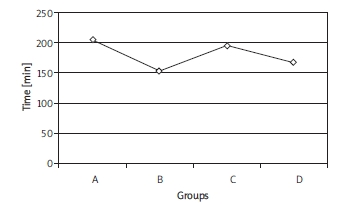
Postoperative first analgesic requirement time
Discussion
Combined spinal epidural anaesthesia has been widely used by obstetric anaesthetists since the 1980s. More than 60% of consultant obstetric anaesthetists in England used the CSEA technique during labour or caesarean section [13]. Combined spinal epidural anaesthesia allows for use of smaller doses of local spinal anaesthetics because the block can be supplemented at any time [14]. Compared to spinal block, the duration of the anaesthesia can be extended by using the CSEA technique. Combined spinal epidural anaesthesia also allows a reduction in the duration of the anaesthesia by the subarachnoid administration of the minimal dose of the local anaesthetic to establish the initial level for the surgery [15].
The duration of spinal anaesthesia depends on the characteristics of the local anaesthetics. Bupivacaine is a potent local anaesthetic with hydrophobic nature [16]. Both bupivacaine and morphine are characterised by a long duration of action. Dosage, volume and concentration of anaesthetic are the major determinants of intrathecally administered solutions [17]. Also the analgesic effect of the additional opioids provides a long postoperative period without pain. As shown in several previous studies, the patients with morphine had a long duration of analgesia [9]. It was not a surprise for us that we had better results with morphine than fentanyl. However, there is always a potential risk of respiratory depression after neuraxial opioids. The incidence of respiratory depression after morphine administration ranges from 0% to 0.9%. Late occurrence might be seen until the postoperative 18th h and can cause permanent brain damage [18]. Our postoperative repeated visits for sedation and respiratory rate monitoring were a precaution for early detection of respiratory depression and provide increased patient satisfaction. None of the patients had a respiratory rate less than 12.
Ogun et al.[19] found that intrathecal isobaric ropivacaine 0.5% 15 mg with morphine 150 µg provided sufficient anaesthesia for caesarean delivery. The parturients were compared with the bupivacaine group. Time to first complaint of pain was similar in all groups.
In the study of Vercauteren et al. [20], they considered that the incidence of hypotension and ephedrine requirement with isobaric bupivacaine were more common than with heavy bupivacaine. The frequency of ephedrine requirement was similar in all groups in our study. However, the heart rate of patients in group A decreased significantly at the 10th min although the values remained within physiological limits. We thought that this result was coincidental and had no clinical significance because there was no statistically significant difference between groups in sensory levels and spread of anaesthesia and analgesia.
The duration of anaesthesia was shorter with hyperbaric bupivacaine compared with isobaric solution in a study by Malinovsly et al.[21]. We could not find any significant difference in the duration of spinal anaesthesia between groups.
The limitation of our study is that we administered only spinal block for the operation and we used the epidural route only for postoperative analgesia, so the amounts of local anaesthetics and opioids we used were higher than the conventional ones used for the CSEA technique. On the other hand, we primarily aimed to compare the effect of different baricities of bupivacaine with two different opioids and we demonstrated that the postoperative first analgesic requirement time was longer with isobaric bupivacaine than with heavy bupivacaine combined with morphine.
In conclusion, that intrathecal 15 mg isobaric bupivacaine with 200 µg morphine provides longer duration of analgesia, similar haemodynamic effects, ephedrine requirement and side effects when compared to heavy bupivacaine-morphine or bupivacaine-fentanyl combinations during caesarean section. Further studies can be planned with lower doses of morphine with different concentrations of bupivacaine when used with the CSEA technique.
Acknowledgments
The work was conducted in the Central Education and Research Hospital, Erzurum, Turkey.
References
- 1.Velde MV, Teunkens A, Hanssens M. Intrathecal sufentanil and fetal heart rate abnormalities: a double-blind, duble placebo-controlled trial comparing two forms of combined spinal epidural analgesia with epidural analgesia in labor. Anesth Analg. 2004;98:1153–9. doi: 10.1213/01.ANE.0000101980.34587.66. [DOI] [PubMed] [Google Scholar]
- 2.Kamiya Y, Kikuchi T, Inagawa G. Lidocaine concentration in cerebrospinal fluid after epidural administration: a comparison between epidural and combined spinal-epidural anesthesia. Anesthesiology. 2009;110:1127–32. doi: 10.1097/ALN.0b013e31819daf15. [DOI] [PubMed] [Google Scholar]
- 3.Nakamura G, Ganem EM. Effects on mother and fetus of epidural and combined spinal-epidural techniques for labor analgesia. Rev Assoc Med Bras. 2009;55:405–9. doi: 10.1590/s0104-42302009000400014. [DOI] [PubMed] [Google Scholar]
- 4.Akbay KB, Boztepe A, Sezen YG. A comparison of bupivacaine solutions with or without fentanyl intrathecally Türkiye Klinikleri. J Med Sci. 2007;5:118–23. [Google Scholar]
- 5.Malinovsky J, Renaud G, Le Corre P. Influence of volume and baricity of solutions. Anesthesiology. 1999;9:1260. doi: 10.1097/00000542-199911000-00016. [DOI] [PubMed] [Google Scholar]
- 6.Kokki H, Tuovinen K, Hendolin H. Spinal anesthesia for paediatric day-case surgery: a double-blind, randomized, parallel group, prospective comparison of isobaric and hyperbaric bupivacaine. Br J Anaesth. 1998;81:502–6. doi: 10.1093/bja/81.4.502. [DOI] [PubMed] [Google Scholar]
- 7.Hallworth SP, Fernando R, Columb MO. The effect of posture and baricity on the spread of intrathecal bupivacaine for elective cesarean delivery. Anesth Analg. 2005;100:1159–65. doi: 10.1213/01.ANE.0000149548.88029.A2. [DOI] [PubMed] [Google Scholar]
- 8.Parlow JL, Money P, Chan P. Addition of opioids alters the density and spread of intrathecal local anesthetics? An in vitro study. Can J Anesth. 1999;46:66–70. doi: 10.1007/BF03012518. [DOI] [PubMed] [Google Scholar]
- 9.Santos LM, Santos VCJ. Intrathecal morphine plus general anesthesia in cardiac surgery: effects on pulmonary function, postoperative analgesia and plasma morphine concentration. Clinics. 2009;64:279–85. doi: 10.1590/S1807-59322009000400003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Andrieu G, Roth B, Ousmane L. The efficacy of intrathecal morphine with or without clonidine for postoperative analgesia after radical prostatectomy. Anesth Analg. 2009;108:1954–7. doi: 10.1213/ane.0b013e3181a30182. [DOI] [PubMed] [Google Scholar]
- 11.Channaiah VB, Chary K, Vlk JL, Wang Y, Chandra SBC. Low-dose fentanyl: hemodynamic response to endotracheal intubation in normotensive patients. Arch Med Sci. 2008;4:293–9. [Google Scholar]
- 12.Eisenach J, Hood D, Curry R. Cephalad movement of morphine and fentanyl in humans after intrathecal injection. Anesthesiology. 2003;99:166–173. doi: 10.1097/00000542-200307000-00027. [DOI] [PubMed] [Google Scholar]
- 13.Ingelmo PM, Somaini M. Optimal epidural volume expansion during combined spinal-epidural anesthesia: one question, one answer. Minerva Anesthesiol. 2010;76:334–9. [PubMed] [Google Scholar]
- 14.Nakamura G, Ganem EM. Effects on mother and fetus of epidural and combined spinal-epidural techniques for labor analgesia. Rev Assoc Med Bras. 2009;55:405–9. doi: 10.1590/s0104-42302009000400014. [DOI] [PubMed] [Google Scholar]
- 15.Imbelloni LE, Fornasari M. Combined spinal epidural anesthesia during colon surgery in a high-risk patient. Case report. Rev Bras Anestesiol. 2009;59:41–5. doi: 10.1016/s0034-7094(09)70099-6. [DOI] [PubMed] [Google Scholar]
- 16.Raddi P, Nagalingaswamy VP, Khatib F, Wang Y, Chandra SBC. A comparison of interpleural bupivacaine and intravenous pethidine for postoperative pain relief following open cholecystectomy. Arch Med Sci. 2009;5:57–62. [Google Scholar]
- 17.Kuusniemi KS, Pihlajamäki KK, Pitkänen MT. Low dose bupivacaine: a comparison of hypobaric and near isobaric solutions for arthroscopic surgery of the knee. Anaesthesia. 1999;54:540–5. doi: 10.1046/j.1365-2044.1999.00855.x. [DOI] [PubMed] [Google Scholar]
- 18.Carvalho B. Respiratory depression after neuraxial opioids in the obstetric setting. Anesth Analg. 2008;107:956–61. doi: 10.1213/ane.0b013e318168b443. [DOI] [PubMed] [Google Scholar]
- 19.Ogun CO, Kirgiz EN, Duman A. Comparison of intrathecal isobaric bupivacaine-morphine and ropivacaine-morphine for caesarean delivery. Br J Anaesth. 2003;90:659–64. doi: 10.1093/bja/aeg123. [DOI] [PubMed] [Google Scholar]
- 20.Vercauteren MP, Coppejans HC, Hoffmann VL. Small-dose hyperbaric versus plain bupivacaine during spinal anesthesia for cesarean section. Anesth Analg. 1998;86:989–93. doi: 10.1097/00000539-199805000-00014. [DOI] [PubMed] [Google Scholar]
- 21.Malinovsky JM, Géraldine R, Pascal LC. Intrathecal bupivacaine in humans: influence of volume and baricity of solutions. Anesthesiology. 1999;91:1260. doi: 10.1097/00000542-199911000-00016. [DOI] [PubMed] [Google Scholar]


