Abstract
The purpose of this study was to examine the dietary habits among centenarians residing in community settings (n=105) and in skilled nursing facilities (n=139). The sample was a population-based multi-ethnic sample of adults aged 98 years and older (N=244) from northern Georgia in the US. Compared to centenarians in skilled nursing facilities, those residing in the community were more than twice as likely to be able to eat without help and to receive most of their nourishment from typical foods, but they had a lower frequency of intake of all of the food groups examined, including dairy, meat, poultry and fish, eggs, green vegetables, orange/yellow vegetables, citrus fruit or juice, non-citrus fruit or juice, and oral liquid supplements. A food summary score was created (the sum of the meeting recommendations for five food groups). In multiple regression analyses, the food summary scores were positively associated with residing in a nursing facility and negatively associated with eating without help and receiving most nourishment from typical foods. These data suggest that centenarians residing in communities may have limited access to foods that are known to provide nutrients essential to health and well-being. Also, centenarians who are able to eat without help and/or who eat mainly typical foods may have inadequate intakes of recommended food groups. Given the essential role of foods and nutrition to health and well-being throughout life, these findings require further exploration through the detailed dietary analyses of centenarians living in various settings.
Key words: Dietary habits, centenarian, community-dwelling, nursing home
Introduction
Foods and nutrients play an important role in the health and well-being of older people, even those who are into very advanced ages (Kuczmarski and Weddle 2005; Niedert 2005). Dietary factors that may be important for centenarians include protein, type and quantity of dietary fat, vitamins, minerals, vegetables, and foods rich in antioxidants (Antonini et al. 2005; Akisaka et al. 1996; Chan et al. 1997a, b; Chen 2001; Houston et al. 1994; Mimura et al. 1992; Shibata et al. 1992; Stathakos et al. 2005; Willcox et al. 2001). The dietary patterns of centenarians reflect the country of origin (Antonini et al. 2005; Akisaka et al. 1996; Beregi 1990; Chan et al. 1997a, b; Chen 2001; Houston et al. 1994; Mimura et al. 1992; Shibata et al. 1992) and differ within a country, depending on gender and race/ethnicity (Fischer et al. 1995; Houston et al. 1994; Johnson et al. 1992; Williams et al. 1995). However, to our knowledge, there are no studies currently available that compare the dietary habits of centenarians residing in communities with those residing in skilled nursing facilities. This information is needed to identify dietary preferences and the needs for dietary interventions, and will assist in the design of research tools to explore the dietary patterns of centenarians residing in different living situations. Further, dietary differences could contribute to differences in functional and health status between those living in different living situations. Therefore, the goal of this study was to compare the dietary habits of centenarians residing in community settings and skilled nursing facilities in order to identify food group patterns and quality of food intake, and to make recommendations about dietary assessment instruments for future studies.
Methods
The study participants were part of the second Georgia Centenarian Study (2001–2007), a population-based multidisciplinary study of centenarians conducted in 44 counties in northern Georgia (USA) from 2002 to 2005. The study includes 244 centenarians and near centenarians (age 98 years and older) recruited from the community, personal care homes, and skilled nursing facilities, as previously described (Poon et al. in press). All questionnaires and procedures were approved by the University of Georgia Institutional Review Board on Human Subjects.
The proportion of participants from each age group recruited from skilled nursing facilities was based on the ‘institutionalized’ population of the study area according to the 2000 US Census figures. Thus, 43% of the centenarians resided in skilled nursing facilities (n=105), the remaining community-dwelling participants resided in private residences and personal care homes (n=139), and the total sample size was N=244. Individuals were coded as living in a skilled nursing facility (1) or not (0). Other demographic variables included age (coded in years), gender (1=female, 0=male), and race (1=African-American, 0=white). For functional capacity, the activities of daily living (ADL) were assessed by the Older Adults Resources Scale (Fillenbaum 1988), where the ADL included bathing/showering, dressing, eating, functional mobility, personal hygiene and grooming, and toilet hygiene, and instrumental activities of daily living (IADL) included using a telephone, preparing meals, shopping for groceries or personal items, handling money, housework, and taking medication. The response categories: were completely unable to do (0), able to do with some help (1), or able to do without help (2), and the summary scores were calculated for ADL (range: 0 to 15) and IADL (range: 0 to 14).
Questions regarding dietary patterns and related factors were read to each participant (or to his or her caregiver) and the answers were recorded by the interviewer. The questions were adapted from the Mini Nutritional Assessment (Vellas et al. 1999) to assess body weight, food intake, mode of nourishment, and current consumption of food groups, including dairy products (milk, yogurt, and cheese), meat, fish, or poultry, orange/yellow vegetables, green vegetables, citrus fruit and juice, non-citrus fruit and juice, and oral liquid supplements. The total fruit intake was estimated by summing the two fruit categories. Frequency categories were times/week (<1, 1, 2, 3, 4, 5, or 6) or times/day (1 to <2 or 2 or more). We determined that the frequency of intake was more important than the serving sizes for gauging the exposure of this population to these food groups (Thompson and Subar 2001). Therefore, serving sizes were not estimated.
Food groups were selected and analyzed based on the Dietary Guidelines for Americans and epidemiological associations with reduced risks of nutritional deficiencies and chronic disease (USDHHS & USDA 2000, 2005). The intake of these food groups was compared to recommendations for 1,600 calories daily, which would be appropriate for a sedentary older adult (USDHHS & USDA 2005). Participants were considered to have met each of the five selected food group guidelines if they consumed: (1) two or more servings of meat, poultry, or fish daily; (2) two or more servings of dairy foods daily; (3) three or more servings of fruit daily; (4) three or more servings of orange or yellow vegetables weekly; (5) and four or more servings of green vegetables weekly. A food summary score was created by assigning one point for meeting each food group guideline (range: 0 to 5). Some limitations of our approach were that the dietary guidelines recommend foods in specific quantities (e.g., grams, ounces, or cups) and there are specific recommendations for “low-fat milk products,” “dark green vegetables,” and for “orange vegetables,” while our instrument assessed intake in “servings,” as “green vegetables” and as “orange/yellow vegetables,” and we did not assess the fat content of the dairy foods.
The means, standard errors, and/or frequencies were calculated. Differences between centenarians residing in the community and in skilled nursing homes were assessed by chi-square analyses and t tests. Multiple regression analyses were used to identify factors associated with the food summary score. All analyses were conducted with the Statistical Analysis System (SAS Institute, Version 8.0, Cary, NC). The level of significance was set at p<0.05.
Results
The age, gender, race/ethnicity, ADL, and IADL of the participants are shown in Table 1. Compared to centenarians in the community, those in skilled nursing facilities were about 0.8 years older (p<0.01) and had a higher proportion of African-Americans (p<0.05), but the gender distribution was similar (mostly females). Centenarians in the community scored significantly higher than those in skilled nursing facilities in both ADL and IADL, which indicates better functional capacity (p<0.05). Information about dietary habits and body weight was usually provided by the participant in community settings and from the medical chart in skilled nursing facilities (Table 2). The ability to eat without help and the consumption of a typical diet of regular foods was more than twice as likely in community dwellers compared to those in skilled nursing facilities. The use of consistency-modified foods (e.g., blenderized, soft, and mechanically altered) was more common in skilled nursing facilities. The consumption of three meals daily and having no recent decline in food intake was lower in community dwellers compared to those in skilled nursing facilities. The majority of centenarians eat three meals a day, 97% in skilled nursing facilities and 83% among community dwellers. However, 16% of community dwellers eat two meals a day compared to only 2% in skilled nursing facilities. Also, it is noted that 1% of community dwellers eat only one meal a day. The most common weight change category in the community dwellers was ‘no change’ (78%), while those in skilled nursing facilities were less likely to have a stable weight (48%) and more likely to have gained weight (24%) or to have lost weight (28%). The degree of weight loss was not significantly different between the two groups (p<0.06). However, it is noted that more centenarians reported weight loss between 1 and 3 kg in skilled nursing facilities compared to those in the community.
Table 1.
Participant characteristics: the Georgia Centenarian Study.
| Total sample (N=244) | Community (n=139) | Skilled nursing facility (n=105) | p< | |
|---|---|---|---|---|
| Mean±SEM or % | ||||
| Age | 100.6±0.2 | 100.2±0.2 | 101.0±0.2 | 0.01* |
| Gender | ns | |||
| Men | 15 | 17 | 12 | |
| Women | 85 | 83 | 88 | |
| Race/ethnicity | 0.05* | |||
| White | 79 | 83 | 72 | |
| African-American | 21 | 17 | 28 | |
| Functional capacity | ||||
| Activities of daily living | 11.4±0.2 | 12.2±0.2 | 10.2±0.4 | 0.000* |
| Instrumental ADL | 9.2±0.2 | 9.6±0.3 | 8.6±0.5 | 0.048* |
*p<0.05
Table 2.
Dietary habits and weight changes in community and skilled nursing facilities: the Georgia Centenarian Study.
| Community | Skilled nursing facility | p< | |
|---|---|---|---|
| Information primarily provided by | 0.0001* | ||
| n | 139 | 104 | |
| Participant (%) | 74 | 11 | |
| Family member (%) | 19 | 7 | |
| Other proxy (%) | 4 | 1 | |
| Medical chart (%) | 4 | 82 | |
| At meal times, how does this individual usually eat? | 0.0001* | ||
| n | 139 | 105 | |
| Completely unable to feed self (%) | 5 | 12 | |
| Can eat with some help (%) | 9 | 49 | |
| Is able to eat without help (%) | 86 | 39 | |
| How does this individual receive most of his/her nourishment? (Choose one category) | 0.0001* | ||
| n | 139 | 104 | |
| Refusing nourishment (%) | 0 | 0 | |
| Partial or total parenteral nutrition (%) | 0 | 0 | |
| Nasogastric or gastronomy tube (%) | 1 | 2 | |
| Oral liquid supplements (%) | 0 | 0 | |
| Blenderized or pureed liquid diet (%) | 3 | 24 | |
| Soft diet (%) | 2 | 9 | |
| Mechanically altered diet (%) | 2 | 30 | |
| Typical diet of regular foods (%) | 92 | 36 | |
| How many meals does this individual usually consume each day? | 0.003* | ||
| n | 138 | 104 | |
| Generally does not consume meals (%) | 1 | 1 | |
| One meal daily (%) | 1 | 0 | |
| Two meals daily (%) | 16 | 2 | |
| Three meals daily (%) | 83 | 97 | |
| Has food intake declined over the past three months due to loss of appetite, digestive problems, or chewing or swallowing difficulties? | 0.02* | ||
| n | 139 | 100 | |
| Severe (%) | 2 | 0 | |
| Moderate (%) | 14 | 5 | |
| No (%) | 83 | 95 | |
| Has the individual had a change in body weight in the past three months? | 0.0001* | ||
| n | 135 | 100 | |
| No (%) | 78 | 48 | |
| Yes, gained weight (%) | 6 | 24 | |
| Yes, lost weight (%) | 16 | 28 | |
| Weight loss during the last three months? | 0.06 | ||
| n | 135 | 101 | |
| Weight loss greater than 3 kg (6.6 pounds) | 5 | 7 | |
| Weight loss between 1 and 3 kg (2.2 and 6.6 pounds) | 11 | 22 | |
| No weight loss (or loss <1 kg) | 84 | 71 | |
| Information about body weight is from | 0.0001* | ||
| n | 139 | 104 | |
| Participant (%) | 71 | 11 | |
| Family member (%) | 23 | 11 | |
| Other proxy (%) | 5 | 2 | |
| Medical chart (%) | 1 | 77 |
*p<0.05. Percentages may not add up to 100% because of rounding.
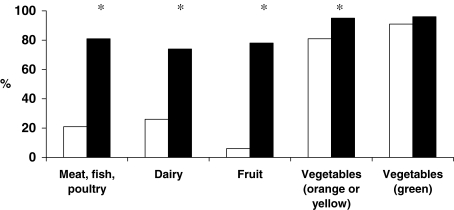
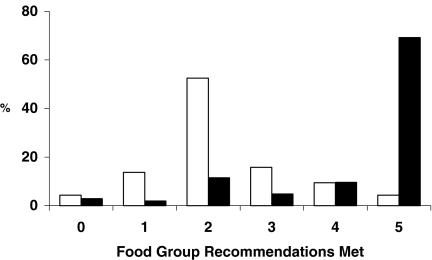
Compared to centenarians in the community, those in the skilled nursing facilities had a significantly higher frequency of intake of all nine food groups (Table 3). Those in skilled nursing facilities also were significantly more likely to meet the recommended frequencies of intake for meat, fish, and poultry (4:1), dairy (3:1), fruit (10:1), and orange/yellow vegetables (1.2:1.0), but not green vegetables (Figure 1). They also had a significantly higher food summary score (mean±SEM: 4.2±0.1 vs. 2.3±0.1, p<0.0001, Figure 2) compared with the community-dwelling centenarians.
Table 3.
Intake of selected food groups in community dwelling and skilled nursing facilities: the Georgia Centenarian Study.
| Food group | Frequency of intake | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | <1/wk | 1/wk | 2/wk | 3/wk | 4/wk | 5/wk | 6/wk | 1/d to <2/d | 2 or more/d | |
| Oral liquid supplement* | ||||||||||
| Community (%) | 108 | 66 | 2 | 3 | 1 | 3 | 4 | 3 | 12 | 7 |
| Skilled nursing facility (%) | 89 | 33 | 1 | 0 | 0 | 0 | 0 | 7 | 10 | 49 |
| Milk, yogurt, and cheese* | ||||||||||
| Community (%) | 138 | 4 | 3 | 4 | 5 | 4 | 7 | 16 | 32 | 26 |
| Skilled nursing facility (%) | 104 | 2 | 0 | 0 | 4 | 3 | 1 | 4 | 12 | 74 |
| Meat, fish, or poultry* | ||||||||||
| Community (%) | 139 | 2 | 1 | 1 | 4 | 4 | 0 | 21 | 46 | 21 |
| Skilled nursing facility (%) | 104 | 3 | 0 | 1 | 1 | 0 | 1 | 4 | 10 | 81 |
| Eggs* | ||||||||||
| Community (%) | 137 | 13 | 7 | 19 | 18 | 8 | 8 | 12 | 15 | 1 |
| Skilled nursing facility (%) | 104 | 5 | 1 | 4 | 6 | 2 | 67 | 7 | 8 | 1 |
| Green vegetables* | ||||||||||
| Community (%) | 139 | 1 | 1 | 1 | 5 | 11 | 6 | 18 | 42 | 14 |
| Skilled nursing facility (%) | 104 | 2 | 0 | 0 | 2 | 0 | 1 | 2 | 8 | 86 |
| Orange/yellow vegetables* | ||||||||||
| Community (%) | 139 | 3 | 6 | 11 | 25 | 12 | 6 | 7 | 27 | 3 |
| Skilled nursing facility (%) | 104 | 2 | 1 | 2 | 2 | 4 | 1 | 1 | 74 | 13 |
| Citrus fruit or citrus juice* | ||||||||||
| Community (%) | 139 | 11 | 1 | 6 | 4 | 6 | 2 | 23 | 44 | 3 |
| Skilled nursing facility (%) | 104 | 2 | 1 | 2 | 1 | 4 | 0 | 7 | 71 | 12 |
| Non-citrus fruit or juice* | ||||||||||
| Community (%) | 139 | 2 | 3 | 8 | 14 | 9 | 3 | 13 | 41 | 7 |
| Skilled nursing facility (%) | 104 | 1 | 0 | 3 | 3 | 4 | 0 | 3 | 11 | 76 |
| Total fruit* | ||||||||||
| Community (%) | 139 | 1 | 1 | 1 | 4 | 3 | 0 | 4 | 50 | 37 |
| Skilled nursing facility (%) | 104 | 1 | 0 | 0 | 0 | 1 | 0 | 3 | 11 | 85 |
*p<0.0001. Percentages may not add up to 100% because of rounding.
Figure 1.
Compared to centenarians residing in the community (open bars), those residing in skilled nursing facilities (filled bars) were significantly (*p<0.001) more likely to consume two or more servings of meat, poultry, or fish daily, two or more servings of dairy foods daily, three or more servings of fruit daily, and three or more servings of orange or yellow vegetables weekly. There was no difference between the two groups in consuming four or more servings of green vegetables weekly. These food categories were modeled after the Dietary Guidelines for Americans (USDHHS & USDA 2005) for a 1,600-calorie meal pattern
Figure 2.
Compared to centenarians residing in the community (open bars), those residing in skilled nursing facilities (filled bars) had significantly higher food group scores (p<0.0001). The food group score ranged from 0 to 5 and one point was given for each of the following five food groups: two or more servings of meat, poultry, or fish daily, two or more servings of dairy foods daily, three or more servings of fruit daily, three or more servings of orange or yellow vegetables weekly, and four or more servings of green vegetables weekly. These food categories were modeled after the Dietary Guidelines for Americans (USDHHS & USDA 2005) for a 1,600-calorie meal pattern
Predictors of the food summary score were identified by multiple regression analyses (Table 4). The food summary score was positively associated with living in a skilled nursing facility (p<0.0001) and negatively associated with eating without help (p<0.02) and consuming a typical diet of regular foods (p<0.002). The trend for food summary scores to be lower in women compared to men approached statistical significance (p<0.06).
Table 4.
Predictors of the food summary score: the Georgia Centenarian Study.
| Parameter estimate | Standard error | p< | |
|---|---|---|---|
| Skilled nursing facility (vs. community) | 1.45 | 0.21 | 0.0001* |
| Age (years) | −0.05 | 0.04 | 0.24 |
| Female (vs. male) | −0.41 | 0.21 | 0.06 |
| African-American (vs. white) | −0.09 | 0.19 | 0.63 |
| Eat without help (vs. some help or unable) | −0.60 | 0.19 | 0.002* |
| Typical diet of regular foods (vs. other) | −0.52 | 0.20 | 0.02* |
| Eat three meals daily (vs. <three) | 0.06 | 0.26 | 0.81 |
| No loss of appetite (vs. moderate loss or severe loss) | 0.16 | 0.24 | 0.50 |
| Severe weight loss of >3 kg in past 3 months (vs. <3 kg) | 0.24 | 0.32 | 0.46 |
*p<0.05. Variables were coded skilled nursing facility (1) vs. community dwelling (0); age in years; female (1) vs. male (0); African-American (1) vs. white (0); able eat without help (1) vs. some help or unable (0); typical diet of regular foods (1) vs. other (0); eat three meals daily (1) vs. one or two meals (0); no loss of appetite (1) vs. some loss or severe loss of appetite (0); severe weight loss of >3 kg in past 3 months (1) vs. <3 kg in past 3 months.
Discussion
Centenarians consumed foods from several food groups, as has been observed by other studies throughout the world (Antonini et al. 2005; Akisaka et al. 1996; Beregi 1990; Chan et al. 1997a, b; Chen 2001; Houston et al. 1994; Mimura et al. 1992; Shibata et al. 1992; Willcox et al. 2001). These studies have not differentiated dietary patterns as a function of living situations, perhaps because many of these studies did not include a large percentage of persons residing in skilled nursing facilities. We have found that living situations can contribute significantly to food patterns. Compared to community-dwelling centenarians, those residing in skilled nursing facilities had a higher frequency of intake of most food groups, received most of their nourishment from foods with modified consistency (e.g., blenderized or mechanically altered), were more likely to use oral liquid supplements, and were more likely to have maintained their food intake during the past three months. Possible reasons for these influences include dietary regulations in skilled nursing facilities, and differences in caregivers and in health care management.
Differences in the frequency of intake of the various food groups were striking between these two subgroups of centenarians. However, our methodology may have overestimated or underestimated food intake to varying degrees in both groups, since we did not determine serving sizes or distinguish between food that was served and food that was eaten. Skilled nursing facilities are required to serve meals that meet dietary guidelines and other federal nutrition policies (Castellanos 2004; Wellman and Kamp 2004), so it is likely that these facilities did indeed serve a nutritionally adequate diet with all of the recommended food groups. Those in skilled nursing facilities frequently used consistency-modified foods (63% as the main source of nourishment) and oral liquid supplements (59%, one or more daily), which can help maintain and/or improve food intake, nutrient intake, and body weight in frail elders (Castellanos 2004; Kuczmarski and Weddle 2005). We previously reported that community-dwelling centenarians had a high prevalence of illnesses that interfere with eating (22%) and who had trouble biting and chewing (48%) (Nickols-Richardson et al. 1996), so the use of consistency-modified foods and oral liquid supplements would be appropriate. Weight gain was reported more often in centenarians from skilled nursing facilities than from the community. Weight loss is common in frail older adults (Callahan and Jensen 2004; Johnson and Fischer 2004; Johnson and Park in press). Perhaps some centenarians entered the skilled nursing facility after a loss of body weight and the nutritional support of the facility was able to restore some of this weight loss. It is also possible that changes in body weight were reported somewhat more accurately in the skilled nursing facility (where such records are required) than in the community setting.
The low percentage of centenarians in community settings consuming the recommended number of servings of meat, fish, and poultry (21%, two servings daily), dairy foods (26%, two servings daily), and fruit (6%, three servings daily) raises concerns about their access to foods that promote health and well-being. Animal foods (eggs, meat, fish, poultry, and dairy foods) are the primary sources of protein and vitamin B12 in the US diet (IOM 1998, 2002; Johnson 2004). Protein is essential for the maintenance of the immune system, muscle, and other organ systems (IOM 2002), while vitamin B12 is important for red blood cell synthesis, the nervous system, and cognition (IOM 1998). Dairy foods are the primary dietary sources of calcium and vitamin D, which are essential for bone health, muscle function, and the nervous system (IOM 1997). Fruit provides essential nutrients, such as potassium, vitamin C, vitamin A, and folate, and is a rich source of antioxidant nutrients (IOM 1998, 2000, 2001). Thus, it is possible that community-dwelling centenarians may be at risk of suboptimal intakes of several key nutrients and health-promoting foods.
Higher food summary scores were significantly and positively associated with living in a skilled nursing facility (vs. the community) when controlled for other demographic and nutrition-related factors. Given the requirements that skilled nursing facilities must provide nutritious meals (Castellanos 2004), it is not surprising that this contributed to higher food pattern scores. The reason for the lower food summary scores among those which ate without help and who consumed most of their nourishment from a diet of typical foods (e.g., without consistency modifications) raises several concerns. Perhaps those who eat without help actually may need help, may be refusing help with eating, or may be eliminating or avoiding nutritious foods that are difficult to prepare and/or eat. Similarly, it is possible that those who consume mainly typical foods may actually be able to improve their food intake by accepting some foods with consistency modifications or by accepting some help with eating. Consistency-modified foods help those with swallowing difficulties or other problems to maintain food and nutrient intake. Providing assistance with eating and consistency-modified foods may be difficult for some older people or their families and caregivers to accept or to implement (Castellanos 2004).
There are some limitations to this study in that the findings may not be generalizable to other populations of centenarians. Dietary habits and criteria for and frequency of nursing home placement vary among countries and cultures. Although the results are reported separately for centenarians residing in communities and those residing in skilled nursing facilities, there may be other variables associated in unknown ways with differential probability of selection into our sample, such as race or gender. Prior history of chronic diseases, the degree of satisfaction concerning the foods served in the skilled nursing facilities, and follow-up data of morbidity are not available for the participants. Further, the characteristics of a Georgia sample may differ from the characteristics of centenarians in other geographic regions.
In summary, centenarians face different food-related challenges depending on their living situation. To explore these challenges, future studies should include detailed dietary assessments (e.g., multiple daily dietary records and/or observations of food intake), and obtain detailed information about consistency-modified foods, oral liquid supplements, other dietary supplements, and barriers to food access (Kuczmarski and Weddle 2005; Niedert 2005). Community-dwelling centenarians may not have access to the wholesome foods that they need. Contributory factors, which could be further explored in the centenarians and their caregivers, include physical or mental problems that contribute to problems with biting, chewing, and swallowing, impaired ability to shop or cook, and a lack of knowledge about the food and nutritional needs of older adults (Kuczmarski and Weddle 2005; Niedert 2005). Caregivers in both the community and in skilled nursing facilities must be prepared to address a variety of food- and nutrition-related concerns of these elders, including the need for foods from all of the recommended food groups, interventions for declining food intake and body weight, and the appropriate use of consistency-modified foods and oral liquid supplements.
Acknowledgments
The Georgia Centenarian Study (Leonard W. Poon, PI) is funded by 1P01-AG17553 from the National Institute on Aging, a collaboration among the University of Georgia, Louisiana State University, Louisiana State University Health Sciences Center, Boston University, University of Kentucky, Emory University, Duke University, Rosalind Franklin University of Medicine and Science, Iowa State University, and the University of Michigan. The authors acknowledge the valuable recruitment and data acquisition effort from M. Burgess, K. Grier, E. Jackson, E. McCarthy, K. Shaw, L. Strong, and S. Reynolds, data acquisition team manager; S. Anderson, E. Cassidy, M. Janke, and T. Savla, data management; M. Durden for project fiscal management.
Footnotes
Additional authors include S. M. Jazwinski, R. C. Green, M. Gearing, W. R. Markesbery, J. L. Woodard, J. S. Tenover, I. C. Siegler, P. Martin, M. MacDonald, C. Rott, W. L. Rodgers, and J. Arnold.
References
- Akisaka M, Asato L, Chan YC, Suzuki M, Uezato T, Yamamoto S. Energy and nutrient intakes of Okinawan centenarians. J Nutr Sci Vitaminol (Tokyo) 1996;42(3):241–248. doi: 10.3177/jnsv.42.241. [DOI] [PubMed] [Google Scholar]
- Antonini FM, Petruzzi E, Pinzani P, Orlando C, Petruzzi I, Pazzagli M, Masotti G. Effect of diet and red wine consumption on serum total antioxidant capacity (TAC), dehydroepiandrosterone-sulphate (DHEAS) and insulin-like growth factor-1 (IGF-1) in Italian centenarians. Arch Gerontol Geriatr. 2005;41(2):151–157. doi: 10.1016/j.archger.2005.01.003. [DOI] [PubMed] [Google Scholar]
- Beregi E (ed) (1990) Interdisciplinary topics in gerontology, vol 27. Centenarians in Hungary: a sociomedical and demographic study. Karger, Basel, Switzerland, pp 53–64
- Callahan E, Jensen GL. Weight issues in later years. Generations. 2004;28(3):39–44. [Google Scholar]
- Hammer Castellanos V. Food and nutrition in nursing homes. Generations. 2004;28(3):65–71. [Google Scholar]
- Chan YC, Suzuki M, Yamamoto S. Dietary, anthropometric, hematological and biochemical assessment of the nutritional status of centenarians and elderly people in Okinawa, Japan. J Am Coll Nutr. 1997;16(3):229–235. doi: 10.1080/07315724.1997.10718679. [DOI] [PubMed] [Google Scholar]
- Chan YC, Suzuki M, Yamamoto S. Nutritional status of centenarians assessed by activity and anthropometric, hematological and biochemical characteristics. J Nutr Sci Vitaminol (Tokyo) 1997;43(1):73–81. doi: 10.3177/jnsv.43.73. [DOI] [PubMed] [Google Scholar]
- Chen C. A survey of the dietary nutritional composition of centenarians. Chin Med J (Engl) 2001;114(10):1095–1097. [PubMed] [Google Scholar]
- Fillenbaum G. The OARS assessment methodology: multidimensional functional assessment questionnaire. 2. Durham, North Carolina: Duke University Center for the Study of Aging and Human Development; 1988. [Google Scholar]
- Fischer JG, Johnson MA, Poon LW, Martin P. Dairy product intake of the oldest old. J Am Diet Assoc. 1995;95(8):918–921. doi: 10.1016/S0002-8223(95)00254-5. [DOI] [PubMed] [Google Scholar]
- Houston DK, Johnson MA, Poon LW, Clayton GM. Individual foods and food group patterns of the oldest old. J Nutr Elder. 1994;13(4):5–23. doi: 10.1300/J052v13n04_03. [DOI] [PubMed] [Google Scholar]
- Dietary reference intakes for calcium, phosphorous, magnesium, vitamin D, and fluoride. Washington, DC: National Academy Press; 1997. [PubMed] [Google Scholar]
- Dietary reference intakes for thiamin, riboflavin, niacin, vitamin B6, folate, vitamin B12, panthothenic acid, biotin, and choline. Washington, DC: National Academy Press; 1998. [PubMed] [Google Scholar]
- Dietary reference intakes for vitamin C, vitamin E, selenium, and carotenoids. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- Dietary reference intakes for vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium, and zinc. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. Washington, DC: National Academy Press; 2002. [DOI] [PubMed] [Google Scholar]
- Johnson MA. Hype and hope about foods and supplements for healthy aging. Generations. 2004;28(3):45–53. [Google Scholar]
- Johnson MA, Fischer JG. Eating and appetite: common problems and practical remedies. Generations. 2004;28(3):11–17. [Google Scholar]
- Johnson MA, Park S. Nutrition in the later years. In: Berdanier CD, Feldman E, editors. Handbook of nutrition and food. 2. Boca Raton, Florida: CRC Press; in press. [Google Scholar]
- Johnson MA, Brown MA, Poon LW, Martin P, Clayton GM. Nutritional patterns of centenarians. Int J Aging Hum Dev. 1992;34(1):57–76. doi: 10.2190/AMKL-8CT9-5C6F-358F. [DOI] [PubMed] [Google Scholar]
- Kuczmarski MF, Weddle DO, American Diertetic Association Position paper of the American Dietetic Association: nutrition across the spectrum of aging. J Am Diet Assoc. 2005;105(4):616–633. doi: 10.1016/j.jada.2005.02.026. [DOI] [PubMed] [Google Scholar]
- Mimura G, Murakami K, Gushiken M. Nutritional factors for longevity in Okinawa—present and future. Nutr Health. 1992;8(2–3):159–163. doi: 10.1177/026010609200800311. [DOI] [PubMed] [Google Scholar]
- Nickols-Richardson SM, Johnson MA, Poon LW, Martin P. Mental health and number of illnesses are predictors of nutritional risk in elderly persons. Exp Aging Res. 1996;22(2):141–154. doi: 10.1080/03610739608254003. [DOI] [PubMed] [Google Scholar]
- Niedert KC, American Diertetic Association Position of the American Dietetic Association: liberalization of the diet prescription improves quality of life for older adults in long-term care. J Am Diet Assoc. 2005;105(12):1955–1965. doi: 10.1016/j.jada.2005.10.004. [DOI] [PubMed] [Google Scholar]
- Poon LW, Jazwinski SM, Green RC, Woodard JL, Martin P, Rodgers WL, Johnson MA, Hausman D, Arnold J, Davey A, Batzer MA, Markesbery WR, Gearing M, Siegler IC, Tenover JS, Cress E, Miller LS, MacDonald M, MacDonald Rott, Reynolds S, Dai J. Contributors of longevity and adaptation: findings and new directions from the Georgia Centenarian Studies. In: Perls T, editor. Exceptional longevity. Baltimore, Maryland: Johns Hopkins University Press; 2006. [Google Scholar]
- Shibata H, Nagai H, Haga H, Yasumura S, Suzuki T, Suyama Y. Nutrition for the Japanese elderly. Nutr Health. 1992;8(2–3):165–175. doi: 10.1177/026010609200800312. [DOI] [PubMed] [Google Scholar]
- Stathakos D, Pratsinis H, Zachos I, Vlahaki I, Gianakopoulou A, Zianni D, Kletsas D. Greek centenarians: assessment of functional health status and life-style characteristics. Exp Gerontol. 2005;40(6):512–518. doi: 10.1016/j.exger.2005.03.008. [DOI] [PubMed] [Google Scholar]
- Thompson FE, Subar AF. Dietary assessment methodology. In: Coulston AM, Rock CL, Monsen ER, editors. Nutrition in the prevention and treatment of disease. San Diego, California: Academic Press; 2001. pp. 3–30. [Google Scholar]
- US Department of Health and Human Services and US Department of Agriculture (2000) Nutrition and Your Health: Dietary Guidelines for Americans. Available online at http://www.health.gov/DietaryGuidelines/dga2000/DIETGD.PDF
- US Department of Health and Human Services and US Department of Agriculture (2005) Dietary Guidelines for Americans 2005. Available online at http://www.health.gov/dietaryguidelines/dga2005/document/pdf/DGA2005.pdf
- Vellas B, Guigoz Y, Garry PJ, Nourhashemi F, Bennahum D, Lauque S, Albarede JL. The Mini Nutritional Assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition. 1999;15(2):116–122. doi: 10.1016/S0899-9007(98)00171-3. [DOI] [PubMed] [Google Scholar]
- Wellman NS, Kamp B. Federal food and nutrition assistance programs for older people. Generations. 2004;28(3):78–85. [Google Scholar]
- Willcox BJ, Willcox DC, Suzuki M. The Okinawa program. New York: Clarkson Potter; 2001. [Google Scholar]
- Williams LA, Johnson MA, Poon LW, Martin P. Oral health and demographic risk factors for poor nutrient intake in the elderly. Age Nutr. 1995;6(1):4–9. [Google Scholar]