Abstract
Background
The recent escalation of US Military suicide deaths to record numbers has been an sentinel for impaired force efficacy and has accelerated the search for reversible risk factors.
Objective
Determine if deficiencies of neuroactive highly unsaturated omega-3 essential fatty acids (n-3 HUFA), in particular docosahexaenoic acid (DHA), are associated with increased risk of suicide death among a large random sample of active duty US military.
Methods
Serum fatty acids were quantified as % of total fatty acids, among US military suicide deaths (n= 800) and controls (n=800) matched for age, date of collection, sex, rank and year of incident. Participants were Active Duty US Military personnel (2002–2008). Outcome measures, included death by suicide, post deployment health assessment questionnaire and ICD-9 mental health diagnosis data.
Results
Risks of suicide death was 14% higher, per standard deviation [SD] lower DHA % (OR =1.14, 95% CI; 1.02–1.27, p<0.03), in adjusted logistic regressions. Among men risk of suicide death was 62% greater with low serum DHA status (adjusted Odds Ratio [OR] =1.62, 95% CI 1.12–2.34, p<0.01, comparing DHA below 1.75% [n=1,389] to above [n=141]). Risk of suicide death was 54% greater in those who reported having seen wounded, dead or killed coalition personnel (OR = 1.54, 95% CI; 1.12–2.12, p< 0.007.)
Conclusion
This US military population had a very low and narrow range of n-3 HUFA status. Although these data suggest that low serum DHA may be a risk factor for suicides, well designed intervention trials are needed to evaluate causality.
Keywords: Suicide, omega-3, docosahexaenoic acid, military, case control
Background
Suicides rates among active duty US Military have increased to record numbers, doubling since the inception of Operation Enduring Freedom (OEF, Afghanistan) and Operation Iraqi Freedom (OIF, Iraq). Army Vice Chief of Staff General Chiarelli described the record suicide rate “horrible” and voiced frustration that “the Army has not yet been able to identify any causal links among the suicide cases” 1.
Deficiencies of nutrients critical for brain function may be a significant contributing risk factor for psychiatric pathology, especially suicide and stress related psychiatric symptoms 2. Highly unsaturated omega-3 polyunsaturated fatty acids (n-3 HUFAs), in particular, docosahexaenoic acid (DHA), are selectively concentrated in neural tissues and required for optimal neural function 3. These fatty acids cannot be made de novo but are available only from dietary sources, with seafood being the richest source. Nutritional deficiencies in n-3 HUFAs may increase vulnerability to combat deployment stress manifesting as psychiatric symptoms including adjustment disorders, major depression, impulsive violence and suicide 4. In civilian populations, observational studies indicate low fish consumption is associated with increased risk of completed suicides 5, 6 and greater suicidal ideation 7. Low DHA status was associated with increased risk of past suicide attempts 8 and future suicide attempts 9. In comparison to placebo, 2 gm/d of n-3 HUFA reduced suicidal thinking, depressive symptoms and reduced the perception of stress, among subjects (n=49) with deliberate self harm 10.
These suggest that low DHA levels may be a contributing factor for adverse psychiatric symptoms. Here, we posited that low DHA status would be associated with increased risk of suicide death among military personnel. Prospectively collected serum and supporting data was available from Armed Forces Health Surveillance Center (AFHSC) for a large number of active duty suicide deaths (n=800) and matched controls (n=800). To our knowledge, this is the largest study of biological factors among suicide deaths.
Methods
Study Design
This case-control study compared total serum fatty acid compositions from among 800 randomly selected active duty US military suicide deaths to 800 matched controls, (2002–2008). The AFHSC is a repository of more than 40 million serum samples with matched health data from US military personnel. Data from service member’s DD Form 2796 (Post-deployment Health Assessment, obtained within 6 months of completion of last deployment) closest to the date of serum sample provided information regarding time and theatre of deployment (if applicable), exposure to stresses during deployment, self report of mental health status and indication for a referral to mental health services demographic data and frozen serum samples were provided by the AFHSC. Mental health and substance abuse related ICD-9CM diagnosis data reports were similarly obtained.
Selection of cases and controls
Suicide deaths were identified among active duty service members from the Army, Navy, Air Force and Marines between 2002 and 2008 for whom data and sera were previously collected and available from the Defense Medical Surveillance System (DMSS) and AFHSC. Cases (n=800) were included only if confirmed by the Armed Forces Institute of Pathology (AFIP) and officially declared a suicide in the Medical Mortality Registry after detailed investigative review. The index sample date was defined as the date of the serum sample closest to the date of death. All cases selected had a serum sample collected within 12 months prior to suicide. Controls (n=800) were randomly selected by the AFHSC and matched by age, gender, rank and availability of a DD Form 2796. Control subjects were selected based on availability of sera drawn within 12 months of the sera drawn from their matched case.
Ethics approval
The institutional review board of The Uniformed Services University (FWA00001628; DOD assurance P60001) approval was granted 08 May 2009 human subjects research protocol HU873B-01.
Sample analysis
Sera were obtained from the Department of Defense Serum Repository which receives and stores ( at -80 F) residual serum specimens from DoD HIV testing and programs related to operational deployments worldwide. Serum samples (n=1,600) were received 21 July 2009 and assayed for total fatty acid composition utilizing a high throughput robotic direct methylation coupled with fast gas-liquid chromatography developed and validated by the Section of Nutritional Neurosciences, Laboratory of Membrane Biochemistry and Biophysics, National Institute of Alcoholism and Alcohol Abuse, National Institutes of Health with interassay variance of <0.5% 11, 12. Laboratory personnel and principle investigators were masked to case status until all fatty acid analyses were completed. Fasting status was determined thus all fatty acids were expressed as percent total fatty acids. Fatty acid degradation in serum samples may have occurred between time of blood draw and freezing. Thus, stability testing was performed by replicating blood draws, serum separation and quantification of degradation of fatty acids at room temperature for 16 time points over 72 hours. The coefficient of variance for DHA was small, 2.1% and showed no evidence of degradation over 72 hours. Fatty acid degradation was expected to occur during prolonged freezer storage. Because case and controls were matched by time of event, the length of storage time for sera was the same and the proportional degradation of fatty acids was similar.
ICD-9 discharge diagnosis data codes were provided from AFHSC, from all available standardized inpatient data reports or ambulatory data reports. A mental health visit counted as any health care visit that included a ICD-9 mental health code (ICD-9 290-219), regardless of the primary visit diagnosis. Visits including substance abuse codes (ICD-9 292-292, 303–305) were similarly counted as substance abuse visits. Post deployment health assessment form DD 2796 data were provided by AFHSC and included mental health screening and stress exposure self report data from previously deployed subjects. However, only 62% of cases had a completed DD Form 2796, in comparison, these data were available on all controls as their selection criteria included having a completed DD Form 2796.
Statistical Methods
We described sample characteristics by age, sex, rank, ethnicity, branch of service, and year of sample. Associations between categorical variable were tested using χ2 tests. There were differences in ethnicity and branch of service comparing suicide cases and controls (table 1) so we adjusted for these factors in subsequent analyses. We assessed the association of DD2796 items to suicide risk in unadjusted and adjusted logistic regression models. Fatty acid data were assessed for normality of distribution and population skewing, no outliers were excluded. Fatty acid data were converted to Z – scores and entered as continuous variables into logistic regression analyses models. Each individual fatty acid was assessed (e.g. increase in Z-score) for suicide risk. Significance for DHA was not corrected for multiple testing as DHA was identified a priori as our primary hypothesis. DHA levels were examined first as quartiles, quintiles, octiles and deciles, then progressive cut-off levels in adjusted logistic regressions. Analyses were conducted using SPSS release 16.0 (SPSS Inc. Chicago, IL).
Table 1.
Demographic characteristics
| Characteristics | Suicide Death | Controls | P Valuea |
|---|---|---|---|
| Mean Age (Range), y | 27.3 (17–59) | 27.3 (18–58) | ns |
|
| |||
| Active Duty, No. (%) | 800 (100%) | 800 (100%) | ns |
|
| |||
| Sex | ns | ||
| Male, No. (%) | 765 (95.6%) | 765 (95.6%) | |
| Female, No. (%) | 35 (4.4%) | 35 (4.4%) | |
|
| |||
| Ethnicity | 0.001 | ||
| Asian, No. (%) | 35 (4.4%) | 33 (4.1%) | |
| African American, No. (%) | 94 (11.8%) | 127 (15.9%) | |
| Hispanic, No. (%) | 66 (8.3%) | 104 (13.0%) | |
| Native American, No. (%) | 22 (2.8%) | 10 (1.3%) | |
| White, No. (%) | 558 (69.8%) | 503 (62.9%) | |
| Unknown/other, No. (%) | 25 (3.1%) | 23 (2.9%) | |
|
| |||
| Rank | ns | ||
| Enlisted, No. (%) | 729 (91.1%) | 729 (91.1%) | |
| Commissioned Officer, No. | |||
| (%) | 62 (7.8%) | 64 (8.0%) | |
| Warrant Officer, No. (%) | 9 (1.1%) | 7 (0.9%) | |
|
| |||
| Service | 0.04 | ||
| Army, No. (%) | 361 (45.1%) | 381 (47.6%) | |
| Air Force, No. (%) | 155 (19.4%) | 147 (18.4%) | |
| Marines, No. (%) | 126 (15.8%) | 153 (19.1%) | |
| Navy, No. (%) | 158 (19.8%) | 119 (14.9%) | |
|
| |||
| Year of suicide death or matched case | ns | ||
| 2002, No. (%) | 78 (9.8%) | 78 (9.8%) | |
| 2003, No. (%) | 85 (10.6%) | 85 (10.6%) | |
| 2004, No. (%) | 103 (12.9%) | 103 (12.9%) | |
| 2005, No. (%) | 102 (12.8%) | 102 (12.8%) | |
| 2006, No. (%) | 128 (16.0%) | 128 (16.0%) | |
| 2007, No. (%) | 144 (18.0%) | 144 (18.0%) | |
| 2008, No. (%) | 160 (20.0%) | 160 (20.0%) | |
|
| |||
| Deployed since 1990 | 0.001 | ||
| Never Deployed, No. (%) | 305 (38.1%) | 7 (0.9%) | |
| Yes Deployed No. (%) | 495 (61.9%) | 793 (99.1%) | |
Chi square comparisons, ns indicates non-significant.
Results
Demographic characteristics are shown in Table 1. For cases, age at deathranged from 17 to 59 years (mean, 27.3 SD 7.3). Differences were present comparing cases and controls for ethnicity (p<0.001) and branch of military service (p<0.04), thus these factors were included in subsequent analyses. Almost all controls (99.1%) had been deployed vs. 495 of 800 (62%) cases were ever deployed; therefore the relationships of deployment number or duration on suicide risk could not be appropriately assessed and were not added as covariates.
Our primary hypothesis was that lower n-3 HUFA’s, in particular DHA, would be associated with greater risk of suicide. In fact, each standard deviation (SD) lower DHA was associated with a 14% greater risk of suicide (OR =1.14, 95% CI; 1.02–1.27, p<0.03, adjusted for race/ethnicity and service component; see Table 2). We sought to determine if the relationship to suicide risk was uniform across the sample or driven by sub-groups with either very high or very low DHA levels. When examining the subjects by octiles, we found the top octile (n=200) had a wider range in DHA (1.67% to 4.50%) compared to subjects (n=1,200) in the middle six octiles (0.73% to 1.66%) or the lowest octile (n=200) (0.72% to 0.29%). Women had higher DHA% and compared to men (mean 1.48 SD 0.56 vs. mean 1.15 SD 0.45, p<0.0001). However, few women were represented in total sample (n=70, 4.4%); thus, subsequent analyses were also conducted separately by sex. There were no differences in fatty acids comparing women cases and women controls.
Table 2.
Serum fatty acid status and adjusted odds ratios of suicide death
| Suicide Deaths (n=800) | Matched Controls (n=800) | Odds Ratioa | |||
|---|---|---|---|---|---|
| Fatty Acid | Mean (SD) | Mean (SD) | Odds Ratio (95% CI) | P Value | |
| Omega-3 Polyunsaturated Fatty Acids | |||||
| ALAb | 18:3n-3 | 0.54 (0.23) | 0.55 (0.25) | 1.05 (0.95–1.18) | ns |
| EPAb | 20:5n-3 | 0.44 (0.16) | 0.45 (0.17) | 1.10 (0.99–1.23) | 0.08 |
| 22:5n-3 | 0.48 (0.13) | 0.48 (0.13) | 1.03 (0.93–1.15) | ns | |
| DHAb | 22:6n-3 | 1.14 (0.45) | 1.19 (0.47) | 1.14 (1.02–1.27) | 0.03 |
| Omega-6 Polyunsaturated Fatty Acids | |||||
| LAb | 18:2n-6 | 31.19 (4.04) | 31.39 (4.01) | 1.04 (0.94–1.15) | ns |
| 18:3n-6 | 0.40 (0.17) | 0.41 (0.16) | 1.08 (0.97–1.20) | ns | |
| 20:2n-6 | 0.25 (0.05) | 0.26 (0.05) | 1.10 (0.99–1.22) | ns | |
| 20:3n-6 | 1.61 (0.38) | 1.68 (0.37) | 1.18 (1.06–1.32) | 0.001 | |
| AAb | 20:4n-6 | 7.18 (1.87) | 7.29 (1.96) | 1.03 (0.93–1.15) | ns |
| 22:4n-6 | 0.32 (0.08) | 0.32 (0.08) | 1.01 (0.91–1.12) | ns | |
| 22:5n-6 | 0.23 (0.06) | 0.24 (0.07) | 1.03 (0.93–1.15) | ns | |
| Monounsaturated Fatty Acids | |||||
| 16:1n-7 | 1.60 (0.68) | 1.51 (0.61) | 0.89 (0.81–0.99) | 0.04 | |
| 18:1n-9 | 22.95 (3.64) | 22.55 (3.71) | 0.93 (0.84–1.03) | ns | |
| 18:1n-7 | 2.48 (0.52) | 2.41 (0.56) | 0.88 (0.80–0.98) | 0.03 | |
| 20:1n-9 | 0.17 (0.05) | 0.17 (0.05) | 0.95 (0.88–1.05) | ns | |
| 24:1n-9 | 1.16 (0.35) | 1.15 (0.34) | 0.97 (0.88–1.09) | ns | |
| Saturated Fatty Acids | |||||
| 14:0 | 0.38 (0.26) | 0.41 (0.29) | 1.08 (0.97–1.19) | ns | |
| 16:0 | 18.44 (2.76) | 18.29 (2.91) | 0.94 (0.85–1.04) | ns | |
| 18:0 | 6.82 (0.96) | 7.01 (0.93) | 1.18 (1.05–1.30) | 0.003 | |
| 20:0 | 0.33 (0.06) | 0.33 (0.06) | 1.04 (0.94–1.15) | ns | |
| 22:0 | 1.03 (0.26) | 1.05 (0.27) | 1.08 (0.97–1.19) | ns | |
| 24:0 | 0.85 (0.21) | 0.87 (0.22) | 1.06 (0.96–1.18) | ns | |
Odds ratio of suicide death per one standard deviation (SD) for each fatty acid, adjusted for race/ethnicity and service component using multivariate logistic regression. Cases (n=800) and controls (n=800) were matched for sex, age, rank and date of blood draw. Fatty acids expressed as percent total serum fatty acids. ns indicates non-significant.
alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), linoleic acid (LA), arachidonic acid (AA).
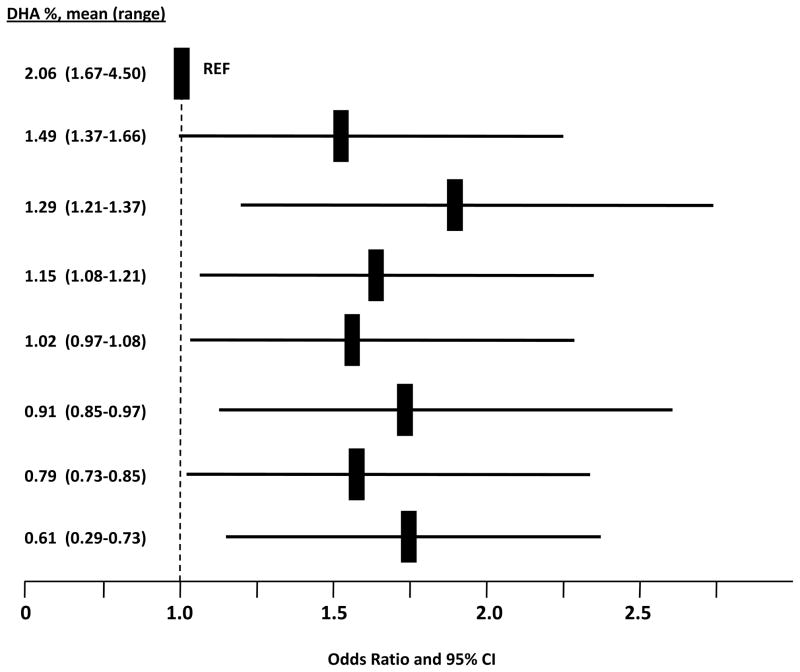
Only subjects with the highest levels of DHA appeared to be protected; compared to the highest octile, risk of suicide death was 62% greater among men with lower serum DHA status (adjusted OR =1.62, 95% CI 1.12–2.34, p<0.01, comparing DHA below 1.75% [n=1,389] to above [n=141]). Compared to the top octile (n=179), the odds of suicide death among males was greater in the octile with the lowest DHA% (n=195), OR=1.75 (95% CI; 1.14–2.68, p< 0.02), the 2nd octile, OR=1.52 (95% CI; 1.00–2.32, p< 0.054) the 3rd octile OR=1.67 (95% CI; 1.09–2.54, p< 0.02), the 4th octile, OR=1.57 (95% CI; 1.03–2.39, p< 0.04), the 5th octile, OR=1.57 (95% CI; 1.02–2.39, p< 0.04), the 6th octile, OR=1.77 (95% CI; 1.16–2.70, p< 0.02), but not the 7th octile, OR=1.48 (95% CI; 0.97–2.26, p< 0.07) (figure 1).
Figure 1. Odds Ratios of Male Suicide Death andOctilesof DHA Status.
Odds ratios and 95% CIs for suicide death are indicted by solid bars and lines respectively. REF indicates reference group, the highest octile of DHA %. Means and ranges of DHA% are indicated for each octile. A statistically significant protective effect was only observed in the highest octile compared to each of the lowest six octiles.
Lower levels of two other fatty acids were associated with increased risk of suicide: 18:0 %, (stearic acid) and 20:3n-6% (di-homogamma linoleic acid, DGLA) (see Table 2). Higher levels of 16:1% (palmitoleic acid) and 18:1n-7 % (cis-vaccenic acid) were associated with lower risks of suicide. Lower levels of both eicosapentaenoic acid (20:5n-3, EPA) and arachidonic acid (20:4n-6, AA) were not significantly associated with suicide risk.
Secondarily, we sought to determine if subjective reports of mental health status were associated with increased risk for suicide among deployed subjects. Data from post deployment health assessment form DD2796 was available for almost all controls (99.1%) had been deployed vs. 495 of 800 (62%) cases were ever deployed. Cases were more likely to endorse “having tried not to think about or avoid situations that reminded them of a frightening, horrible, or upsetting event in the past month” and “seeing coalition soldiers wounded, killed or dead” but less likely to have reported discharging their weapon in direct combat (table 3). No other psychometric responses (e.g., thoughts of being better off dead) were associated with increased risk of suicide. Among all subjects, one greater SD in the number of mental health visits (mean 4.8, SD 12.7) were associated with a greater odds of suicide, OR= 1.17 (95% CI; 1.04–1.31, p<0.009). More inpatient mental health visits (mean 0.15, SD 0.53) were more strongly associated with greater odds of suicide death, OR= 1.47 (95% CI; 1.28–1.70, p<0.0001, per increased SD). History of any visit with substance abuse diagnosis was not associated with suicide, OR= 1.21 (95% CI; 0.90–1.64, ns). Lower DHA status was not related to number of mental health visits or substance abuse diagnoses.
Table 3.
Adjusted odds ratios of suicide death by post deployment questionnaire items
| Item | Odds Ratioa (95% CI) | P Value |
|---|---|---|
| Interested in mental help? | 1.47 (0.80–2.67) | ns |
| Feel detached? | 1.81 (0.99–3.30) | 0.05 |
| Intrusive nightmares? | 1.43 (0.89–2.29) | ns |
| Do you avoid situations? | 1.76 (1.03–3.00) | 0.04 |
| Are you on guard? | 1.06 (0.68–1.66) | ns |
| Avoid conflicts? | 1.41 (0.71–2.78) | ns |
| Do you lose control? | 0.81 (0.32–2.06) | ns |
| See any civilians killed? | 1.41 (1.00–1.98) | 0.05 |
| See any enemy killed? | 1.22 (0.89–1.69) | ns |
| See any coalition killed? | 1.52 (1.11–2.09) | 0.01 |
| Discharge weapon? | 1.46 (1.03–2.06) | 0.04 |
| Feel in danger of being killed? | 0.96 (0.71–1.29) | ns |
| Item | “A Lot” | “Some” | ||
|---|---|---|---|---|
| Odds Ratioa (95 % CI) | P Value | Odds Ratioa (95 % CI) | P Value | |
| Feeling down? | 2.10 (0.94–4.70) | ns | 1.67 (0.69–4.69) | ns |
| Little interest? | 1.35 (0.75–2.43) | ns | 1.19 (0.62–2.28) | ns |
| Want to hurt yourself? | 0.99 (0.00–0.00) | ns | 0.99 (0.00–0.00) | ns |
Odds ratios by logistic regression for risk of suicide death in comparison to a negative response adjusted for race/ethnicity age, sex, grade and service. Post deployment form DD2796 data were compared among deployed cases (n=307) and controls (n=793). ns indicates non-significant.
Discussion
Here we found that low DHA status is a significant risk factor for suicide death among active duty US military. Nearly all US military personnel had low n-3 HUFA status in comparison to North American 13, Australasian 14, Mediterranean 15 and Asian 8 populations. The low amounts and narrow range of DHA in this US Military population in comparison to world and US diversity, made detection of an association difficult and impaired the evaluation of risk relationships among people with higher n-3 HUFA status. For example, the lowest DHA status in a population of suicide attempters in China appeared to be higher than nearly all the US military personnel reported here 8. Chinese subjects in the lowest quartile of DHA status in erythrocytes (mean 2.72% range 0.56–3.72) had a higher odds of a suicide attempt (OR =4.76, 95%CI, 1.67–14.28, p<0.0003) compared to the highest quartile (mean 6.9%, range 6.15–8.94) 8. When compared across these two populations, the lowest DHA status may be associated with a 5–6 fold increased risk of suicidal behaviors compared to the highest status. The maximal benefit may not have been assessed in this sample of US military personnel.
Increased risk for suicide is likely due to multiple social, psychiatric and environmental risk factors underscoring the complexity of psychological health issues among service members. The relative impact of low DHA status on increased suicide risk (62%) can be put into perspective in comparison to the relative impact of severe combat stress or prior mental health problems on increased suicide risk. Personnel with a positive response to “Did you see wounded, killed or dead coalition during deployment?” had an increased risk of suicide death by 54%. The strength of the relationship between more numerous prior mental health visits and increased risk of suicide death was also similar to that of low DHA status.
Some of the limitations inherent in this retrospective analysis were inability to characterize neuropsychiatric symptoms, stress exposure, traumatic brain injury, alcohol use or other potential risk factors and assessment of reverse causality. We noted that an effect of storage time was found for DHA%; mean (SD): 1.32 (0.53) in 2008 and 1.03 (0.40) in 2002, p<0.0001, however the time of storage was matched for cases and controls. Although unlikely, it is possible that DHA was selectively degraded among cases as compared to controls. Although we would have preferred to use multiple serum samples over time the use of a baseline single serum sample robustly PUFA status over serial samples over 12 months duration 16.
As this is a case control study, we must consider the possibility that the presence of a mental illness or substance misuse has changed dietary habits or tissue status and lowered DHA status. However here we found no differences in fatty acid status comparing personnel with and without mental health and substance abuse diagnoses and was thus unlikely to suggest reverse causality for suicides. In addition, reverse causality for depression and n-3 HUFA deficiencies is unlikely as meta-analyses of randomized placebo controlled trials have reported robust treatment efficacy.
We caution that causality for higher n-3 HUFA status in preventing or treating suicide cannot be inferred from this study alone, however this interpretation is supported by a randomized placebo controlled trial of 2 g/d of EPA and DHA finding a 45 % reduction in suicidal thinking and a 30% reduction in depression among patients with recurrent self harm 10. Large treatment effect sizes for n-3 HUFAs among subjects with severe depressive symptoms have been reported in several meta-analyses of randomized placebo controlled trials 17, 18, 19. Severe depressive symptoms are a risk factor for suicidal thinking 20. Epidemiologic data also indicate that low fish consumption is associated with increased risk for suicide. In a 17-yr follow-up of 256,118 Japanese subjects 5, subjects eating fish less than every day had a higher risk of suicide compared to subjects ate fish daily. Among 1,767 Finnish subjects, consuming fish less than twice per week was associated with higher risk of depressive symptoms and suicidal thinking 7. Low DHA status also predicted a 3.4 fold greater risk of a new suicide attempt over more than 800 days 9. These future suicide attempters had greater activity in the anterior cingulate and limbic forebrain in resting PET scans quantifying regional glucose uptake, 21 consistent with the suspected pathophysiology of severe depression and post traumatic stress disorder. Over a 10-fold range of DHA status (0.7 – 7.1% DHA in phospholipid) lower DHA status robustly predicted this regional hyperactivity indicating that low DHA status is may potentially be associated with greater limbic system activity 21. Mann et al 22 have linked suicidal and aggressive behaviors and impulsivity to reduced prefrontal cortical activity on positron emission tomography (PET). DHA supplementation increases prefrontal activity during sustained attention in a dose responsive manner 23.
While this current study could not assess neurobiological mechanisms, several are plausible. Serotinergic, dopaminergic and noradrenergic deficits and overactive stress responses of the hypothalamic-pituitary-adrenal (HPA) axis are implicated in the neurobiology of suicidal behavior 22. In piglets, dietary deficiencies of DHA and AA for 18 days decreased serotonin, dopamine and their metabolite levels in frontal cortex by 50% 24. In mice, chronic stress induced a 40–65% decrease in serotonin and norepinepherine levels in frontal cortex25. These were completely reversed by EPA and DHA supplementation. Deficits in synaptoneogenesis and neural plasticity caused by DHA deficiencies may underlie these observations 26. Observational studies in humans are consistent with these animal studies: lower plasma DHA levels correlated with lower cerebrospinal fluid (CSF) levels of the serotonin metabolite 5-hydroxyindolacetic acid among healthy controls 27 and lower levels of CSF-corticotrophin releasing factor in perpetrators of domestic violence 28.
Unexpectedly we found that higher DGLA status was associated with lower risk of suicide death. In contrast, Virkkunen et al reported that higher phospholipid DGLA levels were associated with a greater likelihood of suicide attempts and violent homicide 29 and higher DGLA in adipose has been associated with greater depressive symptoms 30. Additionally we found that lower levels of stearic acid (18:0) were associated with greater risk of suicide, and that higher levels of palitolenic (16:1) and cis-vaccenic acids (18:1n-7) were associated with lower risk of suicide, the implication of these findings are not clear as psychotropic effects of saturated and monounsaturated fatty acids have not been reported to our knowledge.
Rapidly rising suicide rates are a sentinel for increased impairment of fighting force efficacy due to mental illness 31. The greatest cause of inpatient bed utilization in the US Military is mood disorders, primarily major depression with suicidal risk and adjustment disorders 32. In response, the US Army has initiated a $50 million observation study of enrolling 120,000 subjects per year for five years 33 with the primary purpose of identifying “modifiable risk and protective factors related to mental health and suicide.” Our identification of low DHA serum status as a significant risk factor for suicide deaths can complement this effort. The low n-3 HUFA status is likely due to a combination of several factors including excess omega-6 linoleic acid consumption and deficits in seafood consumption from both foods consumed at US military dining facilities, from available restaurants and choices made at home 34.
Low DHA status can be readily reversed using low cost dietary interventions14 that are likely to have multiple beneficial health effects 35. The American Psychiatric Association already recommends consumption of at least 1 gm per day of n-3 HUFAs for all patients with psychiatric disorders 19. The FDA has determined that up to 3 gm of n-3 HUFAs is generally recognized as safe. The evaluation of efficacy of these levels of n-3 HUFAs in the primary prevention of suicide attempts, or as treatment following suicidal behaviors, merits consideration the US military.
Acknowledgments
Supported by a grant from the Defense Advanced Research Projects Agency and by the Division of Intramural Basic and Clinical Research, NIAAA, NIH. M.D.L. and J.R.H. conceived and designed the study, acquired funding, analyzed the data and wrote primary manuscript drafts. J.E.J assembled data for analysis and contributed to interpretation and writing. Y. L., D.Y.K., and J.L conducted the laboratory analyses and contributed to the writing. Supported by a grant from the Defense Advanced Research Projects Agency and by the Division of Intramural Basic and Clinical Research, NIAAA, NIH. We are indebted to Drs. Angie Eick and Mark Rubertone, (Armed Forces Health Surveillance Center, Silver Spring MD, for data assembly and sample access and to Dr. Ann Scher (Uniformed Services Health Sciences University, Bethesda, MD), Tammy Crowder (Defense and Veterans Brain Injury Center, Rockville MD) for their editorial comments and CDR John C. Umhau, M.D, NIAAA, NIH for his contributions. None of these acknowledged persons have any known conflicts of interest.
Footnotes
The authors have no potential conflicts of interest, financial or otherwise.
Source Information
From the Department of Preventive Medicine and Biometrics, Uniformed Services University, Bethesda, MD (M.D.L., J.E.J.) and the Section of Nutritional Neurosciences, Laboratory of Membrane Biochemistry and Biophysics, National Institute of Alcoholism and Alcohol Abuse, National Institutes of Health (J.R.H., Y. L., D.Y.K., and J.L.). The views expressed in this article are those of the authors and do not reflect official policy or position of the Uniformed Services University, the Department of Defense, the National Institutes of Health, the U.S. Government, or any of the institutional affiliations listed.
Contributor Information
Michael D. Lewis, Email: mlewis@usuhs.mil.
Joseph R. Hibbeln, Email: jhibbeln@mail.nih.gov.
Jeremiah E. Johnson, Email: JEREMIAH.JOHNSON-01@travis.af.mil.
Yu Hong Lin, Email: yulin@mail.nih.gov.
Duk Y. Hyun, Email: ngc2243@hotmail.com.
James D. Loewke, Email: jloewke@mail.nih.gov.
References
- 1.Tyson AS. Washington Post 2009. Nov Wednesday, 18, 2009. Army’s record suicide rate ‘horrible,’ general says Despite high total, awareness campaign shows signs of helping. [Google Scholar]
- 2.Hibbeln JR, Davis JM. Considerations regarding neuropsychiatric nutritional requirements for intakes of omega-3 highly unsaturated fatty acids. Prostaglandins Leukot Essent Fatty Acids. 2009 Aug-Sep;81(2–3):179–186. doi: 10.1016/j.plefa.2009.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McNamara RK, Carlson SE. Role of omega-3 fatty acids in brain development and function: potential implications for the pathogenesis and prevention of psychopathology. Prostaglandins Leukot Essent Fatty Acids. 2006 Oct-Nov;75(4–5):329–349. doi: 10.1016/j.plefa.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 4.Hibbeln JR. Depression, suicide and deficiencies of omega-3 essential fatty acids in modern diets. World Rev Nutr Diet. 2009;99:17–30. doi: 10.1159/000192992. [DOI] [PubMed] [Google Scholar]
- 5.Hirayama T. Life style and mortality. A large scale census-based cohort study in Japan. New York: Karger; 1990. [Google Scholar]
- 6.De Vriese SR, Christophe AB, Maes M. In humans, the seasonal variation in poly-unsaturated fatty acids is related to the seasonal variation in violent suicide and serotonergic markers of violent suicide. Prostaglandins Leukot Essent Fatty Acids. 2004 Jul;71(1):13–18. doi: 10.1016/j.plefa.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 7.Tanskanen A, Hibbeln JR, Hintikka J, Haatainen K, Honkalampi K, Viinamaki H. Fish consumption, depression, and suicidality in a general population. Arch Gen Psychiatry. 2001 May;58(5):512–513. doi: 10.1001/archpsyc.58.5.512. [DOI] [PubMed] [Google Scholar]
- 8.Huan M, Hamazaki K, Sun Y, et al. Suicide attempt and n-3 fatty acid levels in red blood cells: a case control study in China. Biol Psychiatry. 2004 Oct 1;56(7):490–496. doi: 10.1016/j.biopsych.2004.06.028. [DOI] [PubMed] [Google Scholar]
- 9.Sublette ME, Hibbeln JR, Galfalvy H, Oquendo MA, Mann JJ. Omega-3 polyunsaturated essential fatty acid status as a predictor of future suicide risk. Am J Psychiatry. 2006 Jun;163(6):1100–1102. doi: 10.1176/ajp.2006.163.6.1100. [DOI] [PubMed] [Google Scholar]
- 10.Hallahan B, Hibbeln JR, Davis JM, Garland MR. Omega-3 fatty acid supplementation in patients with recurrent self-harm. Single-centre double-blind randomised controlled trial. Br J Psychiatry. 2007 Feb;190:118–122. doi: 10.1192/bjp.bp.106.022707. [DOI] [PubMed] [Google Scholar]
- 11.Masood MA, Salem N., Jr High-throughput analysis of plasma fatty acid methyl esters employing robotic transesterification and fast gas chromatography. Lipids. 2008 Feb;43(2):171–180. doi: 10.1007/s11745-007-3130-9. [DOI] [PubMed] [Google Scholar]
- 12.Masood A, Stark KD, Salem N., Jr A simplified and efficient method for the analysis of fatty acid methyl esters suitable for large clinical studies. J Lipid Res. 2005 Oct;46(10):2299–2305. doi: 10.1194/jlr.D500022-JLR200. [DOI] [PubMed] [Google Scholar]
- 13.Holub BJ, Wlodek M, Rowe W, Piekarski J. Correlation of omega-3 levels in serum phospholipid from 2053 human blood samples with key fatty acid ratios. Nutr J. 2009;8:58. doi: 10.1186/1475-2891-8-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Milte CM, Coates AM, Buckley JD, Hill AM, Howe PR. Dose-dependent effects of docosahexaenoic acid-rich fish oil on erythrocyte docosahexaenoic acid and blood lipid levels. Br J Nutr. 2008 May;99(5):1083–1088. doi: 10.1017/S000711450785344X. [DOI] [PubMed] [Google Scholar]
- 15.Olveira G, Dorado A, Olveira C, et al. Serum phospholipid fatty acid profile and dietary intake in an adult Mediterranean population with cystic fibrosis. Br J Nutr. 2006 Aug;96(2):343–349. doi: 10.1079/bjn20051655. [DOI] [PubMed] [Google Scholar]
- 16.Buydens-Branchey L, Branchey M, Hibbeln JR. Low plasma levels of docosahexaenoic acid are associated with an increased relapse vulnerability in substance abusers. Am J Addict. 2009 Jan-Feb;18(1):73–80. doi: 10.1080/10550490802544003. [DOI] [PubMed] [Google Scholar]
- 17.Appleton KM, Gunnell D, Peters TJ, Ness AR, Kessler D, Rogers PJ. No clear evidence of an association between plasma concentrations of n-3 long-chain polyunsaturated fatty acids and depressed mood in a non-clinical population. Prostaglandins Leukot Essent Fatty Acids. 2008 Jun;78(6):337–342. doi: 10.1016/j.plefa.2008.04.009. [DOI] [PubMed] [Google Scholar]
- 18.Lin PY, Su KP. A meta-analytic review of double-blind, placebo-controlled trials of antidepressant efficacy of omega-3 fatty acids. J Clin Psychiatry. 2007 Jul;68(7):1056–1061. doi: 10.4088/jcp.v68n0712. [DOI] [PubMed] [Google Scholar]
- 19.Freeman MP, Hibbeln JR, Wisner KL, et al. Omega-3 fatty acids: evidence basis for treatment and future research in psychiatry. J Clin Psychiatry. 2006 Dec;67(12):1954–1967. doi: 10.4088/jcp.v67n1217. [DOI] [PubMed] [Google Scholar]
- 20.Pietrzak RH, Goldstein MB, Malley JC, Rivers AJ, Johnson DC, Southwick SM. Risk and protective factors associated with suicidal ideation in veterans of Operations Enduring Freedom and Iraqi Freedom. J Affect Disord. 2009 Oct 9; doi: 10.1016/j.jad.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 21.Sublette ME, Milak MS, Hibbeln JR, et al. Plasma polyunsaturated fatty acids and regional cerebral glucose metabolism in major depression. Prostaglandins Leukot Essent Fatty Acids. 2009 Jan;80(1):57–64. doi: 10.1016/j.plefa.2008.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mann JJ. Neurobiology of suicidal behaviour. Nat Rev Neurosci. 2003 Oct;4(10):819–828. doi: 10.1038/nrn1220. [DOI] [PubMed] [Google Scholar]
- 23.McNamara RK, Able J, Jandacek R, et al. Docosahexaenoic acid supplementation increases prefrontal cortex activation during sustained attention in healthy boys: a placebo-controlled, dose-ranging, functional magnetic resonance imaging study. Am J Clin Nutr. Feb 3; doi: 10.3945/ajcn.2009.28549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de la Presa Owens S, Innis SM. Docosahexaenoic and arachidonic acid prevent a decrease in dopaminergic and serotoninergic neurotransmitters in frontal cortex caused by a linoleic and alpha-linolenic acid deficient diet in formula-fed piglets. J Nutr. 1999 Nov;129(11):2088–2093. doi: 10.1093/jn/129.11.2088. [DOI] [PubMed] [Google Scholar]
- 25.Vancassel S, Leman S, Hanonick L, et al. n-3 polyunsaturated fatty acid supplementation reverses stress-induced modifications on brain monoamine levels in mice. J Lipid Res. 2008 Feb;49(2):340–348. doi: 10.1194/jlr.M700328-JLR200. [DOI] [PubMed] [Google Scholar]
- 26.Cao D, Kevala K, Kim J, et al. Docosahexaenoic acid promotes hippocampal neuronal development and synaptic function. J Neurochem. 2009 Oct;111(2):510–521. doi: 10.1111/j.1471-4159.2009.06335.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hibbeln JR, Linnoila M, Umhau JC, Rawlings R, George DT, Salem N., Jr Essential fatty acids predict metabolites of serotonin and dopamine in cerebrospinal fluid among healthy control subjects, and early- and late-onset alcoholics. Biol Psychiatry. 1998 Aug 15;44(4):235–242. doi: 10.1016/s0006-3223(98)00141-3. [DOI] [PubMed] [Google Scholar]
- 28.Hibbeln JR, Bissette G, Umhau JC, George DT. Omega-3 status and cerebrospinal fluid corticotrophin releasing hormone in perpetrators of domestic violence. Biol Psychiatry. 2004 Dec 1;56(11):895–897. doi: 10.1016/j.biopsych.2004.08.021. [DOI] [PubMed] [Google Scholar]
- 29.Virkkunen ME, Horrobin DF, Jenkins DK, Manku MS. Plasma phospholipid essential fatty acids and prostaglandins in alcoholic, habitually violent, and impulsive offenders. Biol Psychiatry. 1987 Sep;22(9):1087–1096. doi: 10.1016/0006-3223(87)90051-5. [DOI] [PubMed] [Google Scholar]
- 30.Mamalakis G, Kiriakakis M, Tsibinos G, et al. Depression and serum adiponectin and adipose omega-3 and omega-6 fatty acids in adolescents. Pharmacol Biochem Behav. 2006 Oct;85(2):474–479. doi: 10.1016/j.pbb.2006.10.008. [DOI] [PubMed] [Google Scholar]
- 31.Tanielian T, Jaycox LH. Invisible Wounds of War. Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Arlington, VA: The Rand Corporation; 2008. [Google Scholar]
- 32.AFHSC. Medical Survelliance Monthly Report. 2007 Annual Summary Issue. 3 Vol. 15. Silver Spring, MD: U.S. Army Center for Health Promotion and Preventive Medicine, Armed Forces Health Surveillance Center (AFHSC); 2008. [Google Scholar]
- 33.National Institute on Mental Health. Army Study to Assess Risk and Resilience in Service Members (Army STARRS) 2010 [cited; Available from: http://www.nimh.nih.gov/health/topics/suicide-prevention/suicide-prevention-studies/army-study-to-assess-risk-and-resilience-in-service-members-army-starrs.shtml.
- 34.Marriott BP, Varadarajan S, JR, Majchrzak HS, Johnson JG. What, When and Where do Soldiers Eat When Not Deployed and How Could Select Changes impact Omega-3 Fatty Acid Intake? Nutritional Armor for the Warfighter: Can Omega-3 Fatty Acids Enhance Stress Resilience, Wellness, and Military Performance? 2009 http://videocastnihgov/Summaryasp?File=15353.
- 35.National Institutes of Health. Nutritional Armor for the Warfighter: Can Omega-3 Fatty Acids Enhance Stress Resilience, Wellness, and Military Performance? 2009 October 13-14; [cited 05 March 2010]; Available from: Day 1 < http://videocast.nih.gov/Summary.asp?File=15352> Day 2 < http://videocast.nih.gov/Summary.asp?File=15353>.