Abstract
Objective
To describe the prevalence and characteristics of pineal cysts found on MRI in children.
Methods
This is a retrospective monocentric study of all brain magnetic resonance imaging (MRI) examinations performed under the same technical conditions for checking the idiopathic nature of short stature (ISS group, n = 116) and for the investigation of central precocious puberty (CPP) over a 3-year period (n = 56). Dimensions, wall and septal thickness, number of locules, signal intensity, and the presence of a solid component were analysed. Ten of 19 cysts were re-evaluated (follow-up interval 4–28 months). The prevalence of the pineal cysts was compared between the two groups using χ2 and Fisher’s exact tests, and a significance threshold of p < 0.05.
Results
The prevalence of cysts was comparable in the two groups, CPP (10.7%) and ISS (11.2%). Cyst characteristics were similar in the two groups and 74% had thin septations. None of the cysts changed on follow-up. None of the children with pineal cysts exhibited neurological signs.
Conclusion
Benign pineal cysts are a common finding in young children. High-resolution MRI demonstrates that these cysts are often septated. This pattern is a normal variant and does not require follow-up MR imaging or IV contrast media.
Keywords: Pineal cyst, Pediatrics, Brain MRI, Precocious puberty
Background
Pineal cysts—also known as benign glial cysts of the pineal gland—are frequently described in adults, both on autopsy (up to 40%) [1, 2] and on MRI (about 10%), where they are often incidental findings [3–7]. Less, however, is known about the prevalence and appearance of pineal cysts in children. Thanks to the high-resolution imaging now possible with MRI, the anatomical details of these cysts can be visualised. Moreover, the finding of an abnormal pineal region in children with central precocious puberty (CPP) is considered possibly causative by many paediatric endocrinologists. The aim of this study is to describe the prevalence and characteristics of pineal cysts found on MRI in children.
Patients and methods
Study populations and inclusion criteria
This is a retrospective study of all brain MRIs performed:
- For the investigation of CPP in the Pediatric Radiology Service from January 2006 to January 2009 (n = 56). CPP was defined as the appearance of signs of puberty before the age of 8 years in girls (thelarche or pubarche) and age 9.5 years in boys (testicular enlargement or pubarche) associated with elevated gonadotropin levels.
- Or for checking the idiopathic nature of short stature (ISS group, n = 116) defined as a height at the time of investigation ranging from −1.8 to −2.75. None of these children was found to have any abnormality following endocrine, karyotypic, and general investigations (digestive, cardiac, renal, pulmonary).
MRIs showing a pituitary gland abnormality were excluded from the study (n = 3).
Methods
Exam protocol
Pituitary MRIs were performed on two 1.5-T devices—the Avanto (Siemens, Erlangen, Germany) and the GE Signa (General Electric, Healthcare technologies, Milwaukee, WI).
The standardised MR protocol consisted of 3-mm sagittal and coronal T1-weighted spin-echo slices (TR = 400 ms, TE = 115 ms, matrix size = 512 × 512) centred on the pituitary region, 3-mm axial T2-weighted fast spin-echo slices (TR = 5,040 ms, TE = 115 ms, matrix size = 512 × 512 ) of the entire head, and 1-mm sagittal T2-weighted 3D gradient-echo slices (Siemens CISS 3D with TR = 11 ms and TE = 5 ms, or GE FIESTA with TR = 5 ms and TE = 1.80 ms, matrix size = 512 × 512 and FOV = 240 × 240) centred on the midline. The total acquisition time was about 15 min.
In accordance with the protocol and patient safety principles, gadolinium contrast agent was not routinely used, with the exception of follow-up studies for two children with cysts.
Definitions
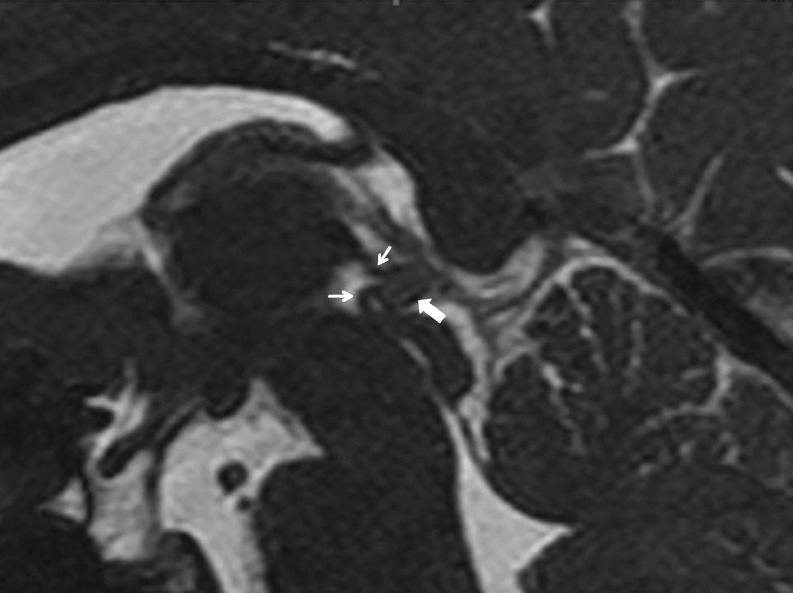
The normal pineal gland is an ovoid structure, less than a centimetre in size along its major axis. In the absence of fluid, its signal intensity on T1- and T2-weighted images is close to that of grey matter (Fig. 1).
Fig. 1.
Normal MRI appearance of the pineal region in a 9-year-old girl. T2-weighted 3D sagittal slice. Normal pineal gland (large arrow), upper and lower roots of the pineal gland (small arrows)
We defined a cyst as any well-demarcated, smooth-edged, fluid-filled formation within the pineal gland that was greater than or equal to 5 mm in size in at least one dimension.
Reading method
The following parameters were analysed (VLB, CA) for each cyst: dimensions (anteroposterior, transverse, and craniocaudal) in millimetres; wall thickness (thin if less than 2 mm); wall regularity; number of locules (uni-, bi-, or multilocular); septal thickness for bi- and multilocular cysts (thin if less than 2 mm); T1- and T2-weighted signal intensity of the cyst contents relative to CSF; the presence of a solid component in the form of a nodule in the cyst wall or within the septa.
Cyst follow-up (clinical, MRI)
Each child with a cyst was examined clinically by a paediatric neurologist. None had neurological signs or headaches.
All of the children identified as having a pineal cyst were contacted by mail for a follow-up MRI of the pineal region.
In the CPP group, two pineal cysts were rechecked after an interval ranging from 4 months to 1 year. In addition to the usual sequences, the follow-up MRI protocol included gadolinium-enhanced sagittal and coronal T1-weighted slices.
In the ISS group, eight pineal cysts were rechecked after an interval ranging from 4 to 28 months. The MRI protocol was unchanged, except for the addition of a coronal T2-weighted FSE sequence in three cases.
Statistical analysis
The prevalence and appearance of the pineal cysts found were compared between the two groups, using chi-square and Fisher’s exact tests, and a significance threshold of p < 0.05.
The characteristics of the patient groups are expressed as mean ± standard deviation.
Results
Precocious puberty group
This group included 43 girls (76.7%) and 13 boys (23.3%), with a sex ratio of 0.30 reflecting the female predominance of CPP. The mean age was 8.5 ± 3.25 years at the time of the MRI (range: 1.08–15.25 years).
Cysts were found in six children (10.7%). All six were girls, whose mean age was 7 ± 3.25 years (range: 1.08–10.25 years). None of them presented clinical signs other than thelarche before the age of 8 years.
The cyst characteristics are depicted in Table 1. Cysts were unilocular (n = 1), bilocular (n = 2), or multilocular (n = 3). Their walls and septa were all less than 1 mm thick and regular. The T1-weighted signal was hypointense and the T2-weighted signal was slightly hypointense relative to the cerebro-spinal fluid (CSF).
Table 1.
Characteristics of cysts in the precocious puberty group (6/56 or 10.7%)
| Patient | Sex | Age (years) (months) | Dimensions (mm) anteroposterior × craniocaudal × transverse | Wall thickness (mm) | Locules | Septal thickness (mm) | Signal intensity T1/T2 |
|---|---|---|---|---|---|---|---|
| 1 | F | 6 | 8.5 × 7 × 7 | <1 | Multilocular | < 1 | Hypo/hyper |
| 8 | |||||||
| 2 | F | 8 | 12 × 9 × 11 | <1 | Multilocular | < 1 | Hypo/hyper |
| 4 | |||||||
| 3 | F | 10 | 7.5 × 5 × 6.5 | <1 | Unilocular | - | Hypo/hyper |
| 3 | |||||||
| 4 | F | 1 | 6 × 6 × 5.5 | <1 | Multilocular | < 1 | Hypo/hyper |
| 1 | |||||||
| 5 | F | 8 | 9 × 5 × 6 | <1 | Bilocular | < 1 | Hypo/hyper |
| 11 | |||||||
| 6 | F | 5 | 7 × 4 × 6 | <1 | Bilocular | < 1 | Hypo/hyper |
| 9 |
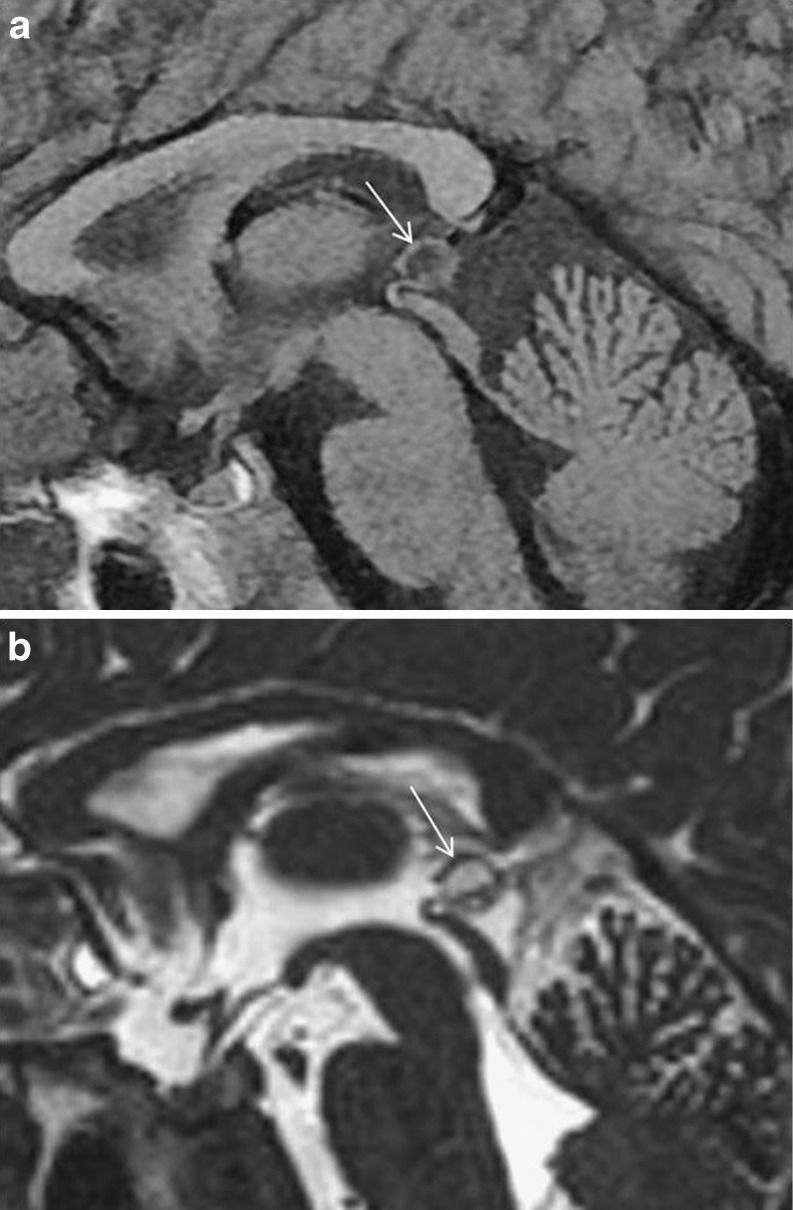
The pineal cysts that were rechecked (n = 2) were multilocular and showed thin gadolinium enhancement of the wall and septa, with no visible nodules (Figs. 2 and 3).
Fig. 2.
Patient 1. Initial MRI: (a) sagittal T1-weighted image and (b) sagittal T2-weighted 3D image. Multilocular cyst (arrows) with thin (sub-millimetre) wall and septa
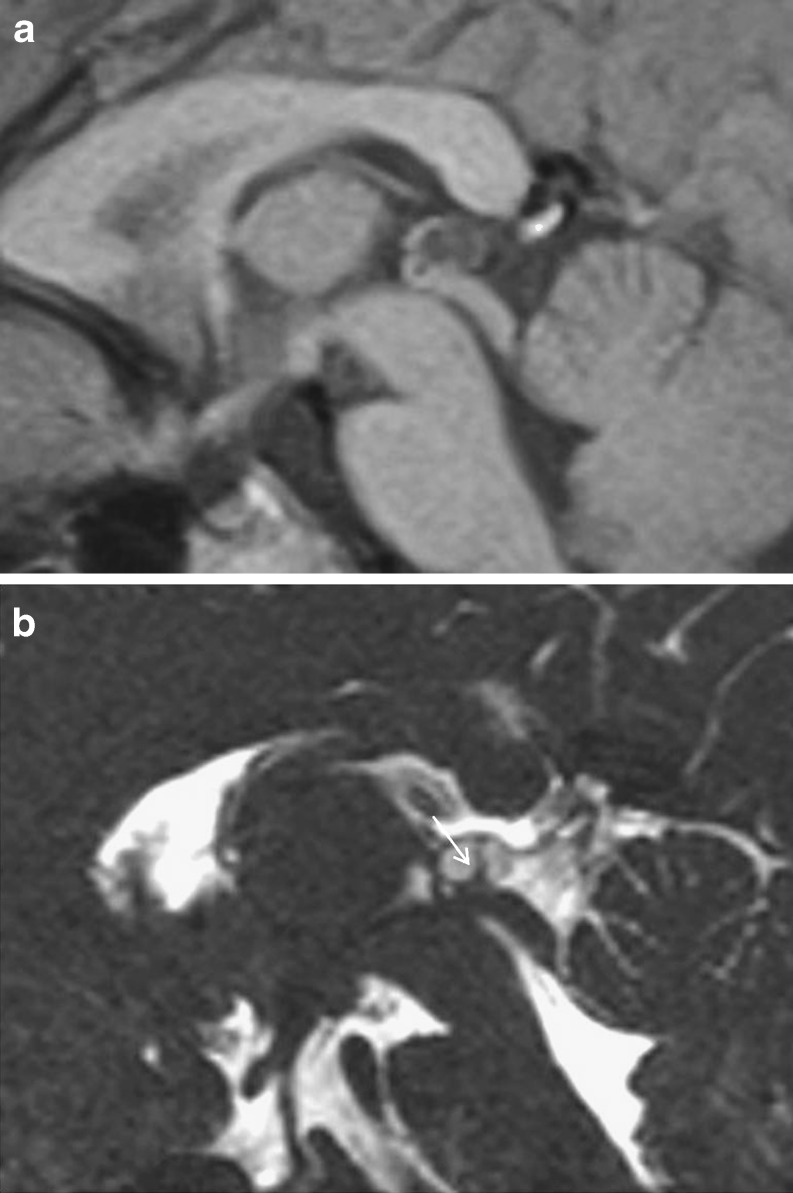
Fig. 3.
Patient 1. Follow-up MRI at 4 months. (a) Sagittal T1-weighted image and (b) sagittal gadolinium-enhanced T1-weighted image. Thin enhancement of the cyst wall and the main internal septum (arrow)
Idiopathic short stature group
The mean age was 8.0 ± 5.5 years (range: 6 months to 15.5 years). The group included 54 girls (46.5%) and 62 boys (53.5%), for a sex ratio of 1.14.
Pineal cysts were found in 13 children (11.2%). These were 7 boys and 6 girls (sex ratio 1.16). The mean age of these 13 children was 6.5 ± 5.25 years (range: 6 months to 15.5 years).
None of the children with cysts presented any symptoms. The characteristics of their cysts are described in Table 2. The largest diameter ranged from 6 to 12 mm. They showed a hypointense signal on T1-weighted images that was slightly hyperintense relative to CSF, and a hyperintense signal on T2-weighted images that was either isointense or slightly hypointense relative to CSF. They had walls that were thin (less than 1 mm in 11 cases, and between 1 and 2 mm in 2 cases) and regular.
Table 2.
Characteristics of cysts in the growth delay group (13/116 or 11.2)
| Patient | Sex | Age (years) (months) | Dimensions (mm) anteroposterior × craniocaudal × transverse | Wall thickness (mm) | Locules | Septal thickness (mm) | Signal intensity T1/T2 | Interval between MRI1 and MRIs | Appearance and size of cyst MRI/MRI2 |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Female | 12 | 10 × 6.5 × 7.5 | < 1 | Multilocular | < 1 | Hypo/hyper | ||
| 8 | |||||||||
| 2* | Male | - | 8 × 6.5 × 7 | 1 to 2 | Unilocular | - | Hypo/hyper | 12 | Unchanged |
| 7 | |||||||||
| 3 | Female | 1 | 6.5 × 4.5 × 8 | <1 | Multilocular | <1 | Hypo/hyper | ||
| 6 | |||||||||
| 4* | Male | 15 | 8 × 4.5 × 7.5 | 1 to 2 | Multilocular | <1 | Hypo/hyper | 17 | Unchanged |
| 6 | |||||||||
| 5* | Female | 9 | 12 × 7 × 8 | <1 | Multilocular | <1 | Hypo/hyper | 4 | Unchanged |
| 11 | |||||||||
| 6 | Male | 4 | 11 × 7 × 6.5 | <1 | Multilocular | <1 | Hypo/hyper | ||
| 4 | |||||||||
| 7 | Male | 1 | 9.5 × 4 × 6.5 | <1 | Bilocular | <1 | Hypo/hyper | ||
| 10 | |||||||||
| 8* | Female | 3 | 12 × 7 × 10 | <1 | Multilocular | <1 | Hypo/hyper | 14 | Unchanged |
| 8 | |||||||||
| 9 | Female | 1 | 6.5 × 4.5 × 4 | <1 | Unilocular | - | Hypo/hyper | ||
| 11 | |||||||||
| 10* | Male | 4 | 10.5 × 6.5 × 8 | <1 | Multilocular | <1 | Hypo/hyper | 28 | Unchanged |
| 6 | |||||||||
| 11* | Male | 12 | 10 × 7 × 8 | <1 | Multilocular | <1 | Hypo/hyper | 13 | Unchanged |
| 4 | |||||||||
| 12* | Female | 2 | 6 × 5.5 × 6 | <1 | Unilocular | - | Hypo/hyper | 6 | Unchanged |
| 1 | |||||||||
| 13* | Male | 2 | 10 × 6.5 × 6 | <1 | Unilocular | - | Hypo/hyper | 23 | Unchanged |
| 4 |
*Patients who received follow-up MRI. The size and appearance of the cyst were unchanged
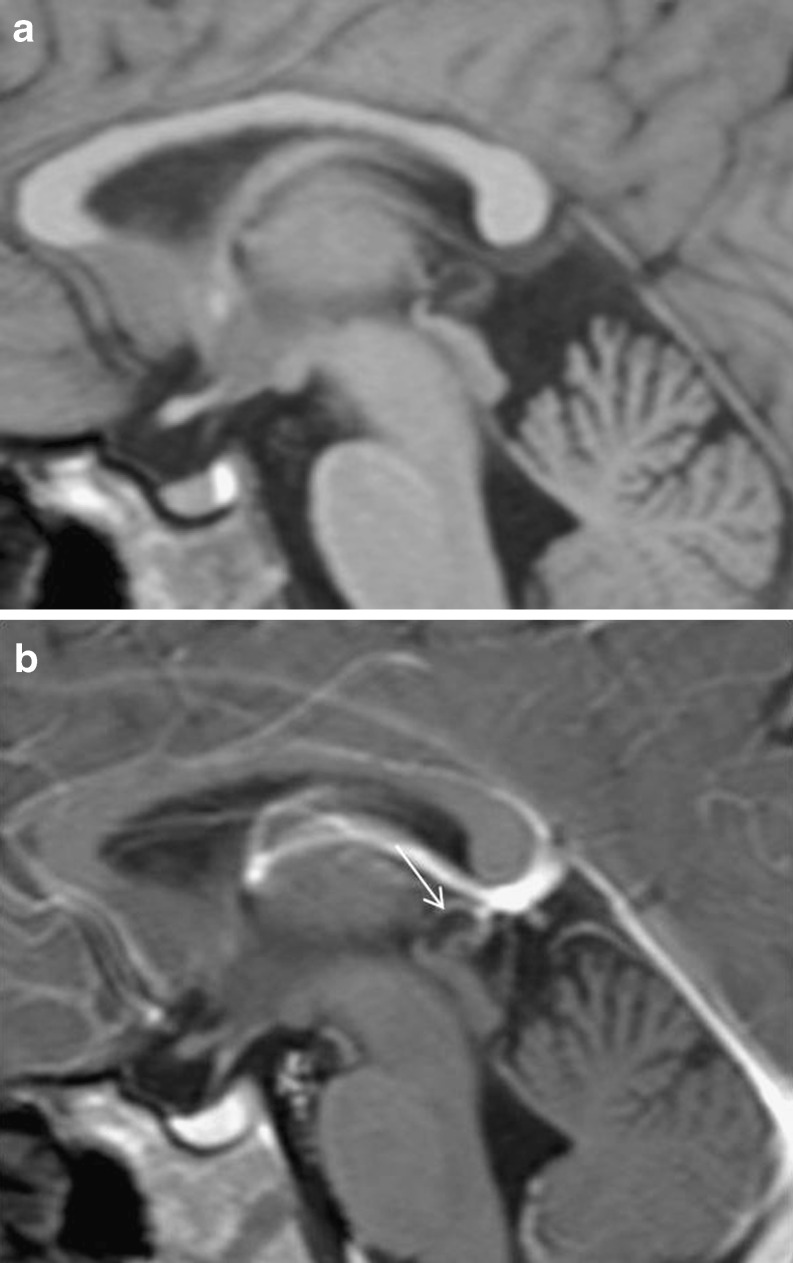
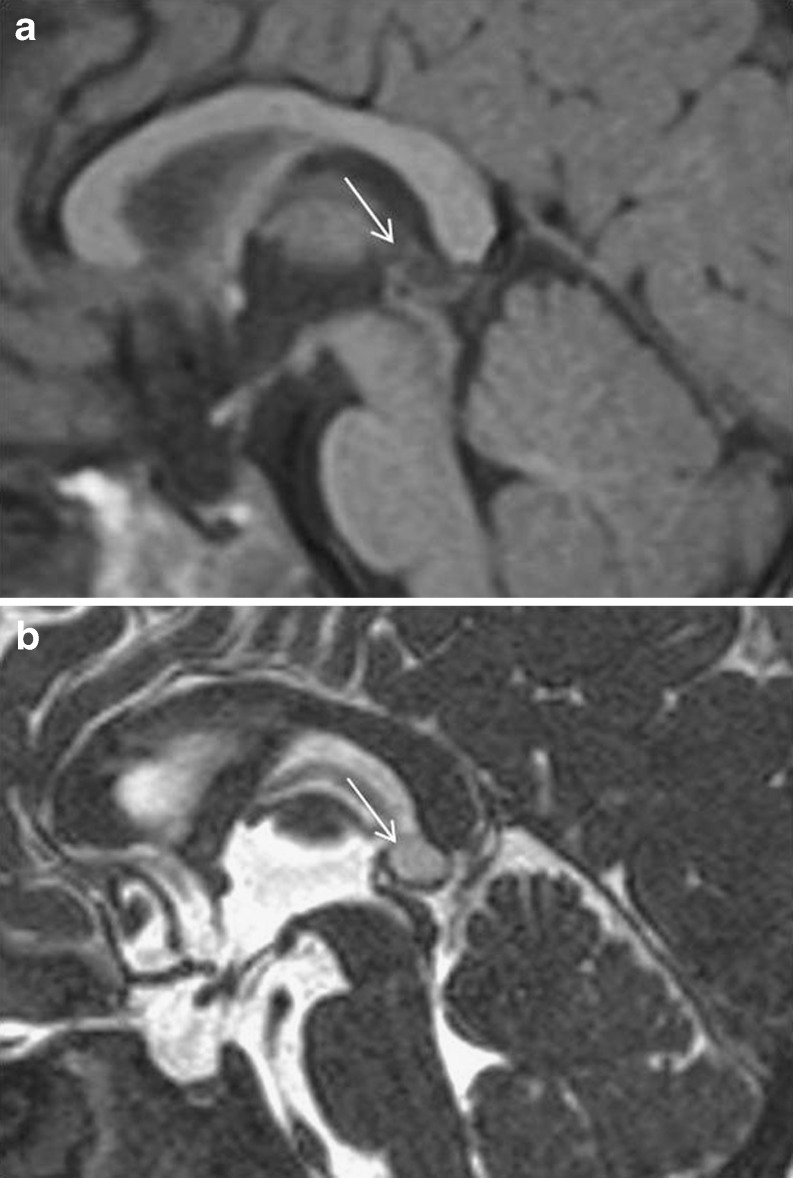
Four cysts were unilocular (Fig. 4) and nine were bi- or multilocular with thin, regular septa (Fig. 5). None of the cysts had walls or septa with solid portions or nodular thickening. The multilocularity and presence of septa were particularly well visualised in the sagittal T2-weighted 3D gradient-echo images.
Fig. 4.
A 7-month-old boy (patient 2). (a) Sagittal T1-weighted image and (b) sagittal T2-weighted 3D image: unilocular cyst (arrows)
Fig. 5.
Pineal cyst in a 4½-year-old boy (patient 10). Unilocular appearance on (a) sagittal T1-weighted image turns out to be multilocular on (b) sagittal T2-weighted 3D image (arrow)
In the 8 children who had a follow-up MRI (4 months to 1 year), the cysts were found to be perfectly stable.
The prevalence of cysts was comparable in the two groups of children, CPP and ISS (Table 3).
Table 3.
Comparison of the two groups
| Precocious puberty group n = 56 | Growth delay groupn = 116 | χ2 test | |
|---|---|---|---|
| Age | 8.5 ± 3.3 years (range: 1.08–15.25 years) | 8.0 ± 5.5 years (range: 6 months to 15.5 years | / |
| Sex | 43 girls (76.7%), 13 boys (23.3%) Sex ratio = 0.30 | 54 girls (46.5%), 62 boys (53.5%) Sex ratio = 1.14 | / |
| Number of cysts | 6 (10.7%) | 13 (11.2%) | NS (p = 0.87) |
| Sex of children with cysts | 6 girls (13.9%) | 6 girls (11.1%), | / |
| 0 boys (0%) | 7 boys (11.3%) | ||
| Fisher’s exact test NS (p = 0.32) | χ2 test NS (p = 0.79) | ||
| Unilocular | 1 | 4 | / |
| Bilocular or > | 5 | 9 | / |
| Major axis | 6 to 12 mm | 6 to 12 mm | / |
| Stability | 100% of cases (n = 2) | 100% of cases (n = 8) | / |
There was no significant difference in the prevalence of cysts between the sexes within the CPP (0% for boys, 11.1% for girls, p = 0.32) or ISS group (11.3% for boys, 11.1% for girls, p = 0.79).
Discussion
In adults, the frequency of pineal cysts found on routine autopsy varies between 20 and 40% [1, 2], but these figures include all cystic transformations of 2 and 5 mm in size. This explains the high prevalence found in autopsy studies compared with imaging studies, which—except in a few reports [8, 9]—use a minimum size of 5 mm. Histologically, the wall of a benign cyst of the pineal gland is ≤2 mm thick and has three distinct layers from the periphery to the centre: an outer fibrocollagenous layer (capsule), a middle pineal cell layer that sometimes contains calcifications, and an inner glial tissue layer [2, 6, 10, 11]. Hypotheses proposed to explain the genesis of a cyst include physiological involution of the pineal gland, the persistence of a pineal diverticulum arising from the pineal recess of the third ventricle, and ischaemic degeneration of an intrapineal glial plaque followed by necrosis and cavitation [2, 10, 12].
It is generally agreed that on MRI the normal pineal gland appears as a solid nodule of tissue in only about 52% of cases [8, 12], and that its appearance can be more crescent-like (26%) or ring-like (22%), a change believed to be a cystic transformation with no pathological significance, provided its largest diameter is less than or equal to 5 mm. Our study took these criteria into account, as only lesions with at least one diameter ≥5 mm were considered to be cysts. Under these conditions, we found a prevalence of 10–11% in both groups.
In MRI studies, the reported frequency of pineal cysts, all age groups combined, is somewhere between 1.2 and 10.8%, depending on both the technical parameters—and thus on the date of the study [6–8, 11, 13, 14]—and the minimum cyst size used, which ranges from 2 to 5 mm [6]. Most of the MRI studies carried out in children involve patients investigated for headaches and/or various neurological disorders (seizures, vertigo, visual problems, mental retardation, etc.) [5, 7, 8], contrary to our study, which only included patients with no neurological signs. Yet we found pineal cysts in very young children—six of the patients were under 3 years old and one of these was under 1 year—in accordance with some previous reports [15].
The 3D gradient-echo sequences (so called CISS or FIESTA)—which have also been used in other series [9]—allows acquisition of very high contrast resolution images (liquid/solid). It is a sequence well-adapted to the analysis of fluid structures, thanks to its heavy T2-weighting. The well-circumscribed appearance, regular contours, wall thickness less than 2 mm, and especially the lack of nodules that characterise these cysts fit the usual criteria for benign, probably glial, cysts [12]. While the multilocular appearance and internal septa are described in some histopathological studies [16], the multiple septations found in 74% of the cases in our series have rarely been reported in MRI studies, most of which describe cysts as unilocular [6, 10, 16]. One exception is the recent series by Pastel et al. [17] who, using a similar sequence, demonstrated the presence of intracystic septa in six patients.
The signal intensity of the cysts in our series is consistent with previous data [6, 10, 13, 18], i.e., a fluid signal subtly hyperintense relative to CSF on T1-weighted images and slightly hypointense relative to CSF on T2-weighted images. We found no haemorrhagic changes, which are still reported only in adults [12, 19]. Some authors have described cysts that are very hyperintense—and hyperintense to CSF—on T2-weighted images [18, 20]. This could be due to the cysts having a higher protein content than the LCR or to the stagnant nature of the cyst fluid [18, 20]. The FLAIR (fluid-attenuated inversion recovery) sequence could have demonstrated the lack of fluid suppression for these cysts, which unlike CSF remain moderately hyperintense [12].
Several MRI studies in large young adult cohorts have shown a higher frequency of pineal cysts in women in their 3rd decade [7, 13, 14]—as high as 5.8%. More recently, Al-Holou [15] studied MRIs from a population of children and young adults, and found a significantly higher prevalence among female subjects. The current report did not show any significant sex difference in the prevalence of cysts, but may lack the necessary statistical power (i.e., a larger cohort) to discern it.
We did not use contrast material routinely to explore ISS or precocious puberty in children if unenhanced studies did not disclose pituitary abnormalities, as the additional risk could not be justified by its diagnostic value. However, pineal cysts frequently show thin peripheral contrast enhancement [6, 11, 13, 21–23], sometimes associated with enhancement of the cystic cavity by diffusion of the contrast agent on late images (30 min post-injection). Stability over time—which also argues in favour of a benign cyst [2, 3, 6, 13]—can be appreciated on the heavily T2-weighted 3D GE sequences. Simple cysts can however show atypical features on MRI as enhancing septa or haemorrhagic signal [21, 24].
Precocious puberty may be associated with some malignant tumours of the pineal region (choriocarcinoma and germinoma), and very rarely, if ever, with pineal parenchymal tumours such as pineocytoma or pineoblastomas, which represent two distinct patterns of tumours, well- and non-differentiated [12, 24–26]. Most pineocytomas are described in middle-aged adults [16, 26], but can also be found in children. They are often small (less than 3 cm), and they may show some cystic areas, a purely cystic form being rare [12].
In conclusion, pineal cysts are a commonplace and incidental finding (11%) in children with no neurological signs. The frequent presence of septations with high-resolution MRI (74%) should be recognised to avoid superfluous controls or IV contrast media.
Acknowledgements
The authors wish to thank the technicians Pr Dominique Musset and Pascale Zerbini for performing the MRIs and for preparing the manuscript.
References
- 1.Hasegawa A, Ohtsubo K, Mori W. Pineal gland in old age; quantitative and qualitative morphological study of 168 human autopsy cases. Brain Res. 1987;409:343–349. doi: 10.1016/0006-8993(87)90720-7. [DOI] [PubMed] [Google Scholar]
- 2.Al-Holou WN, Maher CO, Muraszko KM, et al. The natural history of the pineal cysts in children and young adults. J Neurosurg Pediatr. 2010;5:162–166. doi: 10.3171/2009.9.PEDS09297. [DOI] [PubMed] [Google Scholar]
- 3.Barboriak DP, Lee L, Provenzale JM. Serial MR imaging of pineal cysts: implications for natural history and follow-up. AJR Am J Roentgenol. 2001;176:737–743. doi: 10.2214/ajr.176.3.1760737. [DOI] [PubMed] [Google Scholar]
- 4.Cauley KA, Linell GJ, Braff SP, et al. Serial follow-up MRI of indeterminate cystic lesions of the pineal region: experience of a rural tertiary care referral center. AJR Am J Roentgenol. 2009;193:533–537. doi: 10.2214/AJR.08.1906. [DOI] [PubMed] [Google Scholar]
- 5.Mandera M, Marcol W, Bierzynska-Macyszyn G, et al. Pineal cysts in childhood. Childs Nerv Syst. 2003;19:750–755. doi: 10.1007/s00381-003-0813-2. [DOI] [PubMed] [Google Scholar]
- 6.Petitcolin V, Garcier JM, Mohammedi R, et al. Prévalence et morphologie des kystes épiphysaires : à propos de 1844 IRM hypophysaires. J Radiol. 2002;83:141–145. [PubMed] [Google Scholar]
- 7.Sawamura Y, Ikeda J, Ozawa M, et al. Magnetic resonance images reveal a high incidence of asymptomatic pineal cysts in young women. Neurosurgery. 1995;37:11–15. doi: 10.1227/00006123-199507000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Sener RN. The pineal gland: a comparative MR imaging study in children and adults with respect to normal anatomical variations and pineal cysts. Pediatr Radiol. 1995;25:245–248. doi: 10.1007/BF02011087. [DOI] [PubMed] [Google Scholar]
- 9.Pu Y, Mahankali S, Hou J, et al. High prevalence of pineal cysts in healthy adults demonstrated by high-resolution, non contrast brain MR imaging. AJNR Am J Neuroradiol. 2007;28:1706–1709. doi: 10.3174/ajnr.A0656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barkovich AJ. Pediatric Neuroimaging. 4. Philadelphia: Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 11.Jinkins JR, Xiong L, Reiter RJ. The midline pineal “eye”: MR and CT characteristics of the pineal gland with and without benign cyst formation. J Pineal Res. 1995;19:64–71. doi: 10.1111/j.1600-079X.1995.tb00172.x. [DOI] [PubMed] [Google Scholar]
- 12.Osborn AG. Diagnostic imaging: brain. Salt Lake City: Amirsys; 2004. pp. 132–135. [Google Scholar]
- 13.Golzarian J, Baleriaux D, Bank WO, et al. Pineal cyst: normal or pathological? Neuroradiology. 1993;35:251–253. doi: 10.1007/BF00602604. [DOI] [PubMed] [Google Scholar]
- 14.Lee DH, Norman D, Newton TH. MR imaging of pineal cyst. J Comput Assist Tomogr. 1987;11:586–590. doi: 10.1097/00004728-198707000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Al-Holou WN, Hugh JL, Muraszko KM, et al. Prevalence of pineal cysts in children and young adults. J Neurosurg Pediatr. 2009;4:230–236. doi: 10.3171/2009.4.PEDS0951. [DOI] [PubMed] [Google Scholar]
- 16.Osborn AG, Preece MT. Intracranial cysts: radiologic-pathologic correlation and imaging approach. Radiology. 2006;239:650–664. doi: 10.1148/radiol.2393050823. [DOI] [PubMed] [Google Scholar]
- 17.Pastel DA, Mamourian AC, Duhaime AC. Internal structure in pineal cysts on high-resolution magnetic resonance imaging: not a sign of malignancy. J Neurosurg Pediatr. 2009;4:81–84. doi: 10.3171/2008.5.17681. [DOI] [PubMed] [Google Scholar]
- 18.Inoue Y, Saiwai S, Miyamoto T, et al. Enhanced high-resolution sagittal MRI of normal pineal glands. J Comput Assist Tomogr. 1994;18:182–186. doi: 10.1097/00004728-199403000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Patel AJ, Fuller GN, Wildrick DM, et al. Pineal cyst apoplexy: case report and review of the literature. Neurosurgery. 2005;57:1066. doi: 10.1227/01.NEU.0000179990.46401.66. [DOI] [PubMed] [Google Scholar]
- 20.Kjos BO, Brant-Zawadzki M, Kucharczyk W, et al. Cystic intracranial lesions: magnetic resonance imaging. Radiology. 1985;155:363–369. doi: 10.1148/radiology.155.2.3983386. [DOI] [PubMed] [Google Scholar]
- 21.Fleege MA, Miller GM, Fletcher GP, et al. Benign glial cysts of the pineal gland: unusual imaging characteristics with histologic correlation. AJNR Am J Neuroradiol. 1994;15:161–166. [PMC free article] [PubMed] [Google Scholar]
- 22.Mamourian AC, Yarnell T. Enhancement of pineal cysts on MR images. AJNR Am J Neuroradiol. 1991;12:773–774. [PMC free article] [PubMed] [Google Scholar]
- 23.Fain JS, Tomlinson FH, Scheithauer BW, et al. Symptomatic glial cysts of the pineal gland. J Neurosurg. 1994;80:454–460. doi: 10.3171/jns.1994.80.3.0454. [DOI] [PubMed] [Google Scholar]
- 24.Korogi Y, Takahashi M, Ushio Y. MRI of pineal region tumors. J Neurooncol. 2001;54:251–261. doi: 10.1023/A:1012773727022. [DOI] [PubMed] [Google Scholar]
- 25.Fakhran S, Escott EJ. Pineocytoma mimicking a pineal cyst on imaging: true diagnostic dilemma or a case of incomplete imaging? AJNR Am J Neuroradiol. 2008;29:159–163. doi: 10.3174/ajnr.A0750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim BS, Kim DK, Park SH. Pineal parenchymal tumor of intermediate differentiation showing malignant progression at relapse. Neuropathology. 2009;29:602–608. doi: 10.1111/j.1440-1789.2008.00994.x. [DOI] [PubMed] [Google Scholar]