Abstract
Purpose
Although laparoscopic appendectomies (LAs) are performed universally, a controversy still exists whether the LA is an appropriate surgical approach to complicated appendicitis (CA). We retrospectively evaluated the outcomes of laparoscopic versus open appendectomies for CA.
Methods
We retrospectively analyzed 60 consecutive patients who were diagnosed as having CA from July 2009 to January 2011. Outcomes such as operative time, time to soft diet, length of hospital stay, and postoperative complications were analyzed.
Results
There were no statistically significant differences in operative time between the LA and the open appendectomy (OA) groups. Return to soft diet was faster in the LA group (2.1 ± 1.2 vs. 3.5 ± 1.5 days; P = 0.001). Length of hospital stay was shorter for the LA group (4.4 ± 2.3 vs. 5.8 ± 2.9 days; P = 0.045). The overall complication rates showed no statistically significant difference between the two groups. In cases involving a periappendiceal abscess, the LA had a significantly higher incidence of intra-abdominal abscess (IAA) and postoperative ileus (PI; P = 0.028).
Conclusion
The LA showed good results in terms of the time to soft diet, the length of hospital stay, and surgical site infection (SSI) whereas the overall complication rates were similar for the two groups. However, the LA was associated with significantly higher incidence of IAA and PI for the cases with a periappendiceal abscess. Therefore, when using a LA, the surgeon must take great care to minimize the incidence of IAA and PI if a periappendiceal abscess is present.
Keywords: Complicated appendicitis, Laparoscopic appendectomy, Open appendectomy
INTRODUCTION
A laparoscopic appendectomy (LA) was first reported by Semm [1] in 1983. Since then, its advantages, such as the aesthetic appearance of the wound, less postoperative pain, and faster recovery which facilitates early discharge, have been highlighted, and the number of procedures performed has been continuously increasing [2-7]. The LA was performed mostly on uncomplicated appendicitis due to negative opinions about its safety when it was first introduced. However, the application of the procedure has been extended to complicated appendicitis (CA), and it is now considered as an alternative procedure to an open appendectomy (OA) as its safety record has improved [7, 8]. Nevertheless, it is still controversial because there are still concerns about surgical difficulties in managing CA with laparoscopy, overall surgery time, possible post-op complications and conversion to an OA during the surgery [8-10]. Our study aimed to compare the safety and the efficacy between LA and OA for managing CA.
METHODS
Patients who underwent surgery for acute appendicitis at the National Medical Center (Seoul, Korea) between July 2009 and January 2011 were considered for this study. CA in this study was defined as the existence of a secondary intra-abdominal abscess or peritonitis due to the inflammation in the intra-abdominal space, the presence of gangrene or a perforation confirmed by microscopic examination based on the recommendation of the Infectious Disease Society of America [11, 12]. A total of 60 patients were finally enrolled from among 186 patients based on the definition of CA. The severity of appendicitis, the general medical condition of the patients, the advantages and the disadvantages of OA versus LA, the cost, and the possibility of conversion into OA during LA were explained to the patients.
The operation was performed by residents who had experienced more than 20 cases of laparoscopic abdominal surgery and more than 30 cases of OA as the first assistant under the supervision of specialists. The OA was performed by using the traditional method with a McBurney incision. For the LA, a 1-cm incision was made just below the umbilicus, and the abdominal wall was lifted to insert a 10-mm trocar (Safe Pass; BNR Co., Incheon, Korea). A laparoscopic camera was inserted into the intra-abdominal space through a cannula. Carbon dioxide (CO2) was used to inflate the intra-abdominal space with a pressure of 12 mmHg. Patients were positioned at 20 degrees of the Trendelburg position and tilted to the left side about 15 degree. The appendiceal artery was ligated with an Endoclip (Tyco Healthcare, Norwalk, CT, USA) after tissue dissection with a monopolar forcep. The stump of the appendix was ligated with an Endoloop (Ethicon, Somerville, NJ, USA) and was cut by using monopolar scissors. Specimens were retrieved through the cannula in the left lower abdominal quadrant without an endobag. A drain was placed at the discretion of the operating surgeons.
To prevent postoperative infection, an intravenous infusion of second generation cephalosporin was administered for 3 days, followed by oral first generation cephalosporin for 4 days. For patients with a gangrenous appendicitis, metronidazole was added; the same oral antibiotics were prescribed for patients with perforated appendicitis or periappendiceal abscesses.
A surgical site infection (SSI), intra-abdominal abscess (IAA), and postoperative ileus (PI) were assessed as postoperative complications. A SSI is defined as any evidence of infection (e.g., erythema, purulent discharge, induration, etc.) requiring suture removal, antibiotic treatment, or evidence of dehiscence. An IAA is defined as culture-positive purulent drainage from the intra-abdominal fluid collection obtained percutaneously or operatively, and/or radiologically confirmed fluid collection with systemic or localized signs of infection. PI is defined as the condition in which bowel sound is absent and oral intake is limited for more than 4 days due to abdominal distension secondary to carminative failure. Oral intake was initiated once carminative was confirmed. Oral intake was stopped in case of nausea and vomiting; the period, return to soft diet, includes this interval of nothing by mouth.
SPSS ver.12.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. A P < 0.05 was considered as statistically significant when using the chi-square test and the Student t-test.
RESULTS
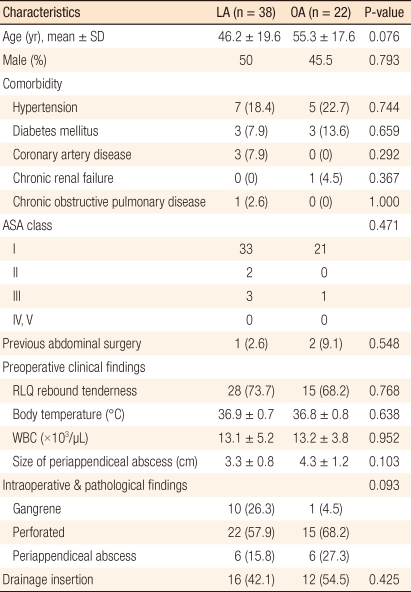
Thirty-eight LAs and 22 OAs were performed on the 60 patients with CA. There were no significant differences in the clinical characteristics and other criteria, such as white blood cell counts, and the size of the abscess on abdominal computed tomography (CT). According to the type of CA, there were 11 cases of gangrenous appendicitis (18.3%), 37 cases of perforated appendicitis (61.7%) and 12 cases of periappendiceal abscess (20.0%), but there were no statistical differences between the LA and the OA groups (Table 1).
Table 1.
Clinicopathologic characteristics in complicated appendicitis
Values are presented as number (%) unless otherwise indicated.
LA, laparoscopic appendectomy; OA, open appendectomy; SD, standard deviation; ASA, American Society of Anesthesiologists; RLQ, right lower quadrant; WBC, white blood cell.
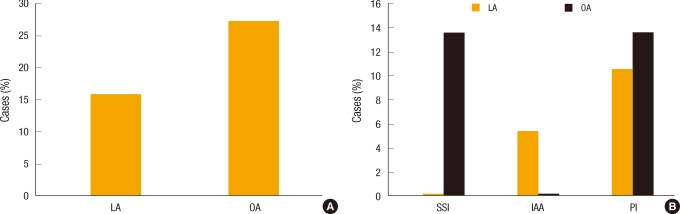
The operative time were 74.9 ± 17.1 minutes in the LA group and 86.3 ± 30.7 minutes in the OA group, but the difference was not statistically significant (P = 0.309). The LA group took 2.1 ± 1.2 days to start soft diet whereas the OA group took 3.5 ± 1.5 days, showing the LA group took less time (P = 0.001). The length of hospital stay was also significantly shorter (P = 0.045) in the LA group (4.4 ± 2.3 days) than in the OA group (5.8 ± 2.9 days) (Fig. 1). Twelve patients experienced postoperative complications: 3 SSIs (5.0%), 2 IAAs (3.3%), and 7 PIs (11.7%).
Fig. 1.
Outcomes for the variables between laparoscopic appendectomy (LA) and open appendectomy (OA). (A) Time to soft diet (2.1 ± 1.2 vs. 3.5 ± 1.5 days; P = 0.001). (B) Length of hospital stay (4.4 ± 2.3 vs. 5.8 ± 2.9 days; P = 0.045).
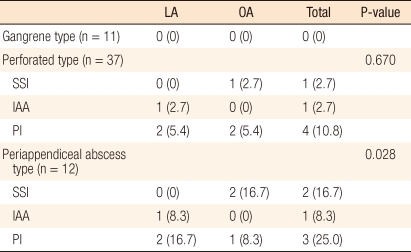
Three cases of SSI in the OA group were treated with suture removal and re-suturing, but additional antibiotics were not used. Two cases of IAA were shown in the LA group, and they were readmitted due to the abdominal pain and fever. Abscesses of 2.5 cm and 3 cm were confirmed by abdominal CT in the area from which the appendix had been removed. The abscesses were treated with intravenous levofloxacin and metronidazole, and the treatment was discontinued when there were no signs of infection on physical examination and blood test. No additional CT scan or ultrasound was performed. Among the 7 cases of PI, 5 were improved with only fasting and intravenous fluids, but the other 2 patients had nasogastric tube insertion. Perforated appendicitis and periappendiceal abscess accounted for 16.2% and 50.0% of complications, respectively, whereas there were no complications in gangrenous appendicitis, indicating that patients with severe and CA had more complications (Table 2).
Table 2.
Complications between LA and OA according to appendicitis types
Values are presented as number (%).
LA, laparoscopic appendectomy; OA, open appendectomy; SSI, surgical site infection; IAA, intra-abdominal abscess; PI, paralytic ileus.
In terms of classifying the postoperative complications according to the operation method, there were 6 cases of complications in the LA group (15.8%) and 6 in the OA group, showing no difference in the postoperative complications between the two groups. However, the characteristic of the postoperative complications was different as there were more IAAs in the LA group, but more SSIs in the OA group (P = 0.042) (Fig. 2). Moreover, the differences in the postoperative complications according to the operation methods were obvious when the inflammation of appendix was more severe (P = 0.028) (Table 2) as there were more cases of PI in the LA group when a periappendiceal abscess was present and there were more cases of SSI in the OA group when a periappendiceal abscess was present, but no significant difference was observed in cases with perforated appendicitis.
Fig. 2.
Postoperative complications comparing patients with laparoscopic appendectomy (LA) versus open appendectomy (OA). (A) Overall complication rate (15.8 vs. 27.3%; P = 0.327). (B) Complication according to procedure (P = 0.042); surgical site infection (SSI; 0 vs. 13.6%), intra-abdominal abscess (IAA; 5.3 vs. 0%), paralytic ileus (PI; 10.5 vs. 13.6%).
DISCUSSION
The LA was started by removing the uncomplicated appendicitis during the obstetrics and gynecology procedures. It was intermittently reported in the 1980's, and comparative research between the LA and the OA was actively conducted during the 1990's. The initial research proved its safety and efficacy for simple appendicitis, but suggested that the LA was not suitable for CA. However, clinical research on LA for CA has continued over the years and it has been performed in more and more cases as surgical techniques and devices have developed [1-10].
The LA is generally agreed to have better aesthetic effects and shorter hospitalization as compared with the OA. On the other hand, the operative time, postoperative complications, and the conversion to OA during LA have been pointed out as potential drawbacks [8, 9]. In terms of operation time, the majority of the research reported that there was no difference between the LA and the OA that the LA took longer than the OA [13-16]. On the other hand, Yau et al. [17] reported that LA group had a shorter operative time (i.e., 55 minutes in the LA group and 70 minutes in the OA group; P < 0.001). Park and Sul [6] reported the same result and explained that the LA had a better surgical filed view that ultimately helped to detect adhesions or abscesses the conventional OA; this might contributed to the shorter operating time and the fewer postoperative complications. During the early period, the LA took more time owing to immature surgical skills among specialists and residents [18-21]. In our study, the OA took longer than the LA, but there was no statistically significance difference between the two. The reason for the result was the mature and skilled surgical techniques of the surgeons that have been accumulated by performing a wide range of laparoscopic surgeries, including laparoscopic cholecystectomies.
The periods to start oral intake were 2.7 days and 3.9 days post for the LA group and 3.9 days and 4.6 days post for the OA group in the study of Katsuno et al. [15] and So et al. [21], respectively, showing that it took less time in the LA group. Tuggle et al. [22] analyzed National Surgical Quality Improvement Program (NSQIP) to evaluate the length of hospital stay, and it showed statistical significance (4.0 days in the LA group and 5.1 days in the OA group). Khiria et al. [23] evaluated the length of hospital stay for CA and reported a statistical difference between the two groups (5 days in the LA group and 9 days in the OA group). The initiation of soft diet in this study occurred sooner for the LA group (2.1 days in the LA group and 3.5 days in the OA group) and the length of hospital stay was shorter with statistical significance.
The postoperative complications in this study did not show significant differences between the two groups, but their characteristics were different. Especially, SSIs occurred in the OA group and IAAs occurred in the LA group. The prevalence of SSIs tends to be less in LA according to the literature [13, 15-17, 21-24]. Kang et al. [25] subdivided CA and compared the postoperative complications. As a result, SSIs occurred in 5 cases with gangrenous appendicitis (8.9%), in 4 cases with perforated appendicitis (7.3%), and 1 case with a periappendiceal abscess in the OA group, but there were no SSIs in the LA group. On the other hand, there was no significant difference between the groups in terms of the onset of the IAA despite the fact that the LA group showed a rather poor result [13-17, 26]. Especially, the incidence of IAAs in the LA group in a cohort study with pediatric patients conducted by Krisher et al. [10] was significantly worse with figures of 24.0% in the LA group and 4.2% in the OA group. They explained that this result was due to the leakage of infected substances, the appendiceal stump not being inverted and the resection side being exposed in the intra-abdominal space during the removal process of the appendix in the LA. Some literature mentioned that the leakage of infected substances and the breakdown of the appendiceal stump could be avoided by using an Endo-GIA stapler; the use of an endobag minimized intra-abdominal infection and reduced postoperative complications [27-29].
Frazee et al. [9] also subdivided CA into 2 types (i.e., gangrenous and perforated) and compared the postoperative complications after the LA. There were 1 case of IAA (7%) in gangrenous appendicitis and 5 cases in perforated appendicitis (26%). The onset of IAA was reported to be increased when the pre-operative inflammation was more severe in the study of Krisher et al. [10]; IAA did not occur in gangrenous appendicitis, but abscesses occurred in 7 cases from the LA group (24%) and 6 cases from the OA group (4.3%). Our study showed similar results that there was significant difference in the incidence of the complications with periappendiceal abscess in the two groups whereas no difference was observed in the parameter of gangrene or perforated appendicitis. Especially, the incidence of IAA and ileus was higher when a periappendiceal abscess was managed with the LA. Therefore, careful management is required and the use of an Endo-GIA and an endobag should be considered since a high incidence of IAA and ileus has been reported when appendicitis with severe inflammation is treated with a LA.
A LA to manage CA showed good results in terms of the time to oral intake and the length of hospital stay as compared with an OA, but there was no significant difference in the total numbers of postoperative complications between the LA and the OA groups. However, in the LA group, higher incidences of IAA and PI were observed in CA cases involving a periappendiceal abscess. Therefore, when using a LA, the surgeon must take great care to minimize the incidence of IAA and PI if a periappendiceal abscess is present.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Semm K. Endoscopic appendectomy. Endoscopy. 1983;15:59–64. doi: 10.1055/s-2007-1021466. [DOI] [PubMed] [Google Scholar]
- 2.Frazee RC, Roberts JW, Symmonds RE, Snyder SK, Hendricks JC, Smith RW, et al. A prospective randomized trial comparing open versus laparoscopic appendectomy. Ann Surg. 1994;219:725–728. doi: 10.1097/00000658-199406000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guller U, Hervey S, Purves H, Muhlbaier LH, Peterson ED, Eubanks S, et al. Laparoscopic versus open appendectomy: outcomes comparison based on a large administrative database. Ann Surg. 2004;239:43–52. doi: 10.1097/01.sla.0000103071.35986.c1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ortega AE, Hunter JG, Peters JH, Swanstrom LL, Schirmer B Laparoscopic Appendectomy Study Group. A prospective, randomized comparison of laparoscopic appendectomy with open appendectomy. Am J Surg. 1995;169:208–212. doi: 10.1016/s0002-9610(99)80138-x. [DOI] [PubMed] [Google Scholar]
- 5.Hellberg A, Rudberg C, Kullman E, Enochsson L, Fenyo G, Graffner H, et al. Prospective randomized multicentre study of laparoscopic versus open appendicectomy. Br J Surg. 1999;86:48–53. doi: 10.1046/j.1365-2168.1999.00971.x. [DOI] [PubMed] [Google Scholar]
- 6.Park JB, Sul JY. Laparoscopic appendectomy: a safe primary procedure for complicated appendicitis. J Korean Surg Soc. 2007;72:51–56. [Google Scholar]
- 7.Lee MH, Song BJ, Choi SY, Park SH, Kim CS. Clinical evaluation of laparoscopic appendectomy. J Korean Soc Coloproctol. 1998;14:551–560. [Google Scholar]
- 8.Bonanni F, Reed J, 3rd, Hartzell G, Trostle D, Boorse R, Gittleman M, et al. Laparoscopic versus conventional appendectomy. J Am Coll Surg. 1994;179:273–278. [PubMed] [Google Scholar]
- 9.Frazee RC, Bohannon WT. Laparoscopic appendectomy for complicated appendicitis. Arch Surg. 1996;131:509–511. doi: 10.1001/archsurg.1996.01430170055010. [DOI] [PubMed] [Google Scholar]
- 10.Krisher SL, Browne A, Dibbins A, Tkacz N, Curci M. Intra-abdominal abscess after laparoscopic appendectomy for perforated appendicitis. Arch Surg. 2001;136:438–441. doi: 10.1001/archsurg.136.4.438. [DOI] [PubMed] [Google Scholar]
- 11.Solomkin JS, Mazuski JE, Baron EJ, Sawyer RG, Nathens AB, DiPiro JT, et al. Guidelines for the selection of anti-infective agents for complicated intra-abdominal infections. Clin Infect Dis. 2003;37:997–1005. doi: 10.1086/378702. [DOI] [PubMed] [Google Scholar]
- 12.Rivera-Chavez FA, Peters-Hybki DL, Barber RC, Lindberg GM, Jialal I, Munford RS, et al. Innate immunity genes influence the severity of acute appendicitis. Ann Surg. 2004;240:269–277. doi: 10.1097/01.sla.0000133184.10676.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fukami Y, Hasegawa H, Sakamoto E, Komatsu S, Hiromatsu T. Value of laparoscopic appendectomy in perforated appendicitis. World J Surg. 2007;31:93–97. doi: 10.1007/s00268-006-0065-x. [DOI] [PubMed] [Google Scholar]
- 14.Kirshtein B, Bayme M, Domchik S, Mizrahi S, Lantsberg L. Complicated appendicitis: laparoscopic or conventional surgery? World J Surg. 2007;31:744–749. doi: 10.1007/s00268-006-0467-9. [DOI] [PubMed] [Google Scholar]
- 15.Katsuno G, Nagakari K, Yoshikawa S, Sugiyama K, Fukunaga M. Laparoscopic appendectomy for complicated appendicitis: a comparison with open appendectomy. World J Surg. 2009;33:208–214. doi: 10.1007/s00268-008-9843-y. [DOI] [PubMed] [Google Scholar]
- 16.Lin HF, Wu JM, Tseng LM, Chen KH, Huang SH, Lai IR. Laparoscopic versus open appendectomy for perforated appendicitis. J Gastrointest Surg. 2006;10:906–910. doi: 10.1016/j.gassur.2005.12.012. [DOI] [PubMed] [Google Scholar]
- 17.Yau KK, Siu WT, Tang CN, Yang GP, Li MK. Laparoscopic versus open appendectomy for complicated appendicitis. J Am Coll Surg. 2007;205:60–65. doi: 10.1016/j.jamcollsurg.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 18.Joo KH, Son BH, Kim HO, Hwang SI, Kim H, Han WK. Efficacy of a laparoscopic appendectomy when performed by surgeons early in their laparoscopic training courses. J Korean Soc Coloproctol. 2010;26:17–21. [Google Scholar]
- 19.Seo K, Choi Y, Choi J, Yoon K. Laparoscopic appendectomy is feasible for inexperienced surgeons in the early days of individual laparoscopic training courses. J Korean Surg Soc. 2009;76:23–27. [Google Scholar]
- 20.Kim SY, Hong SG, Roh HR, Park SB, Kim YH, Chae GB. Learning curve for a laparoscopic appendectomy by a surgical trainee. J Korean Soc Coloproctol. 2010;26:324–328. doi: 10.3393/jksc.2010.26.5.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.So JB, Chiong EC, Chiong E, Cheah WK, Lomanto D, Goh P, et al. Laparoscopic appendectomy for perforated appendicitis. World J Surg. 2002;26:1485–1488. doi: 10.1007/s00268-002-6457-7. [DOI] [PubMed] [Google Scholar]
- 22.Tuggle KR, Ortega G, Bolorunduro OB, Oyetunji TA, Alexander R, Turner PL, et al. Laparoscopic versus open appendectomy in complicated appendicitis: a review of the NSQIP database. J Surg Res. 2010;163:225–228. doi: 10.1016/j.jss.2010.03.071. [DOI] [PubMed] [Google Scholar]
- 23.Khiria LS, Ardhnari R, Mohan N, Kumar P, Nambiar R. Laparoscopic appendicectomy for complicated appendicitis: is it safe and justified? A retrospective analysis. Surg Laparosc Endosc Percutan Tech. 2011;21:142–145. doi: 10.1097/SLE.0b013e31821ad770. [DOI] [PubMed] [Google Scholar]
- 24.Garg CP, Vaidya BB, Chengalath MM. Efficacy of laparoscopy in complicated appendicitis. Int J Surg. 2009;7:250–252. doi: 10.1016/j.ijsu.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 25.Kang DW, Kim MK, Kim JH, Kim BS, Chun HJ, Sun BH. Laparoscopic versus open for complicated appendicitis. J Korean Surg Soc. 1999;56:570–578. [Google Scholar]
- 26.Pokala N, Sadhasivam S, Kiran RP, Parithivel V. Complicated appendicitis--is the laparoscopic approach appropriate? A comparative study with the open approach: outcome in a community hospital setting. Am Surg. 2007;73:737–741. [PubMed] [Google Scholar]
- 27.Piskun G, Kozik D, Rajpal S, Shaftan G, Fogler R. Comparison of laparoscopic, open, and converted appendectomy for perforated appendicitis. Surg Endosc. 2001;15:660–662. doi: 10.1007/s004640020072. [DOI] [PubMed] [Google Scholar]
- 28.Katkhouda N, Friedlander MH, Grant SW, Achanta KK, Essani R, Paik P, et al. Intraabdominal abscess rate after laparoscopic appendectomy. Am J Surg. 2000;180:456–459. doi: 10.1016/s0002-9610(00)00504-3. [DOI] [PubMed] [Google Scholar]
- 29.Stoltzing H, Thon K. Perforated appendicitis: is laparoscopic operation advisable? Dig Surg. 2000;17:610–616. doi: 10.1159/000051970. [DOI] [PubMed] [Google Scholar]