Abstract
PURPOSE
The aim of this retrospective study was to evaluate cumulative survival rate (CSR) of Implantium implants followed for 5 years and association between risk factors and the CSR.
MATERIALS AND METHODS
A total of two hundred forty-nine Implantium Implants System (Dentium, Seoul, Korea) placed in ninety-five patients from 2004 to 2009 were investigated with several identified risk factors (sex, systemic disease, smoking, alchohol, reason of tooth loss, length, arch (maxilla or mandible), replace tooth type (incisor, canine, premolar or molar) Kennedy classification, prosthodontic type, prosthodontic design, opposite dentition, abutment type, occlusal material, occlusal unit, splint to tooth, cantilever, other surgery). Clinical examination (mobility, percussion, screw loosening, discomfort, etc.) and radiographic examination data were collected from patient records including all problems during follow-up period according to protocols described earlier. Life table analysis was undertaken to examine the CSR. Cox regression method was conducted to assess the association between potential risk factors and overall CSR.
RESULTS
Five of 249 implants were failed. Four of these were lost before loading. The 5-year implant cumulative survival rate was 97.37%. Cox regression analysis demonstrated a significant predictive association between overall CSR and systemic disease, smoking, reason of tooth loss, arch, Kennedy classification and prosthodontic design (P<.05). The screw related complication was rare. Two abutment screw fractures were found. Another complications of prosthetic components were porcelain fracture, resin facing fracture and denture fracture (n=19).
CONCLUSION
The 5-year CSR of Implantium implants was 97.37%. Implant survival may be dependent upon systemic disease, smoking reason of tooth loss, arch, Kennedy classification and prosthodontic design (P<.05). The presence of systemic diseases and combination of other surgical procedures may be associated with increased implant failure.
Keywords: Dental implant, Survival rate, Risk factors
INTRODUCTION
A favorable long term result about osseointegrated implant has been reported since first Braånemark system report.1 On the basis of these long term results, treatment of partial and total edentulism with dental implants has become an accepted treatment in dentistry.2-4 Implant that was used in the beginning was mainly external connection type, but internal connection type that is represented by Astra Tech Implant System has been gradually increased. Numerous experimental and clinical studies have shown favorable results for the internal conical type.
The high success rate has been attributed to the formation of a direct bone-implant interface and maintenance of stable bone to implant contact after loading. So, many researchers developed new implant surface and design. Some studies have reported that the microthread configuration offered improved conditions for osseointegration.5-7 And, it has suggested that the rate and degree of osseointegration were superior for the rough surface compared with the turned one.8 However, there are some biologic factors associated with failure of osseointegration except implant design and surface property.9-11 So, implant losses can occur, early or lately. In addition to above representing factors, demographic variables, health-status, tobacco use, and anatomic location are identified as factors that increase the risk for implant losses. However some studies have shown that individual medical problems do not correlate with increased implant failure.12,13 Because of conflicting data from studies, clinicians are unable to provide concrete answer to questions posed by patients seeking dental implant treatment.
When new implant systems are introduced commercially, it is essential that the long-term clinical results added to the animal studies are reported as scientific publications. In South Korea, although the development of dental implant is increased, few clinical studies have demonstrated the clinical performance of dental implants among South Korean population.14-16 Also, in the studies of risk factor relation to implant failure, as the subject of previous studies were different races to Korean, according to arch form, dietary pattern, bone quality and clenching force, the reported results are different. Therefore, this study was aimed to evaluate the long-term clinical outcome of the implants for 5 years, and to determine the risk factors of implant failure in Korean population.
MATERIALS AND METHODS
During the period from 2004 to 2009, a total of 249 Dentium implants (Dentium Co., Seoul, Korea) were placed consecutively in 95 patients at the Korea University Guro Hospital. Data was collected using patient's clinical chart. Implants loaded immediately after Stage I surgery and splinted with other implant system were ruled out as an exclusion criteria.
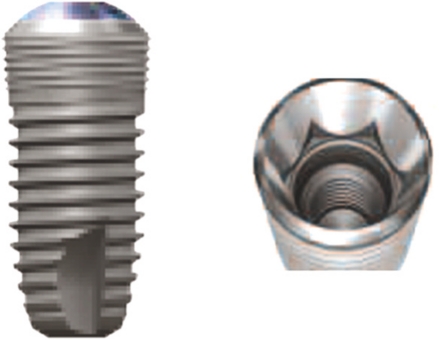
The Dentium implants' interface between abutment and fixture was mediated via a conical seal design that distributes the load to the surrounding cortical bone evenly and prevent screw loosening. The implants had a microthread configuration in the cervical portion, with SLA (Sandblasting with Large grit and Acid etching) surface (Fig. 1).
Fig. 1.
Dentium implant (Dentium Co., Seoul, Korea).
All patients were treated according to the Adell's standard surgical protocol.17 Additional surgical technique (Sinus augmentations, bone regeneration etc.) were used for 80 implants. Patients were seen weekly or biweekly for the first 2 months after implant placement and the monthly for 4 months. Any pressure exerted by the temporary prosthesis was relieved. After 3 - 6 months, the implant was uncovered, healing abutments were placed at least for 1 month, and after that time, the final prosthetic procedure was performed.
Clinical examination (mobility, percussion, screw loosening, discomfort, etc.) and radiographic examination data were collected from patient's record including all problems during follow-up period according to protocols described earlier. The criteria for survival according to Albrektsson and Zarb18 were used to define implant performance. The survival rates were calculated by using a modification of the success criteria suggested by Albrektsson and colleagues.19 So, implant failure, defined as removal and sleeping of the implant was the primary outcome variable. The patients that moved or died were censored. The time between implant placement and the date of the last follow-up or implant failure was used to calculate the duration of implant survival in months.
The risk factors that could affect an implant survival rate were grouped into the following categories12,13:
1. The patient's age at time of implant placement (years) and gender were recorded.
2. Health-status: Whether patients had systemic diseases (diabetes, hypertension, cardiovascular diseases etc), smoking status (non smoker, past smoker or current smoker) and alcohol history were recorded.
3. Implant variables: implant size (length, diameter), implant type and number of implants
4. Anatomic variables: Kennedy classification (tooth borne, distal extension), implant location (maxilla, mandible, anterior, posterior, tooth number)
5. Prosthesis variables: grouped according to prosthesis type, the kind of abutment, prosthetic design (single vs. splinted implants), occlusal materials, opposing dentition, and number of occlusal units in the prosthesis.
6. The reasons of tooth loss were included.
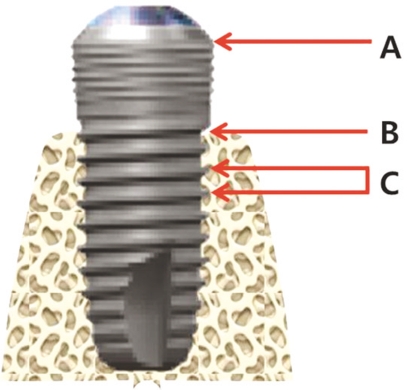
Intraoral periapical radiographs were obtained annually using parallel technique after prosthesis placement. The images were evaluated for peri-implant radiolucency and vertical bone loss. To evaluate the marginal bone level, the distance from a reference point at the implant to the most coronal point (a) where the marginal bone meets the implant (b) was measured in 0.1 mm increments. Measurements were made mesially and distally of each implant. For calibrating magnification, the ratio of real inter-thread width (0.6 mm) to interthread width (c) of radiograph was used (Fig. 2).
Fig. 2.
Reference point for measuring of marginal bone loss. A: junction between implant machined collar bevel and rough surface, B: implant to marginal bone contact level, C: inter-thread distance.
Kaplan-Meier estimate of implant survival was undertaken to examine CSR. Multiple Cox proportional hazards regression and log-rank test was used to assess the influence of potential risk factors on implant survival after adjusting for confounders. The level of statistical significance was set as α=.05.
RESULTS
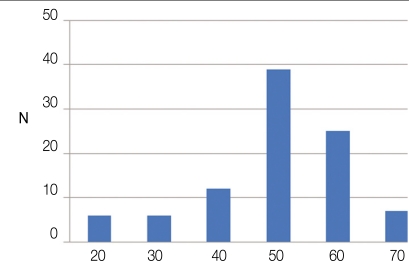
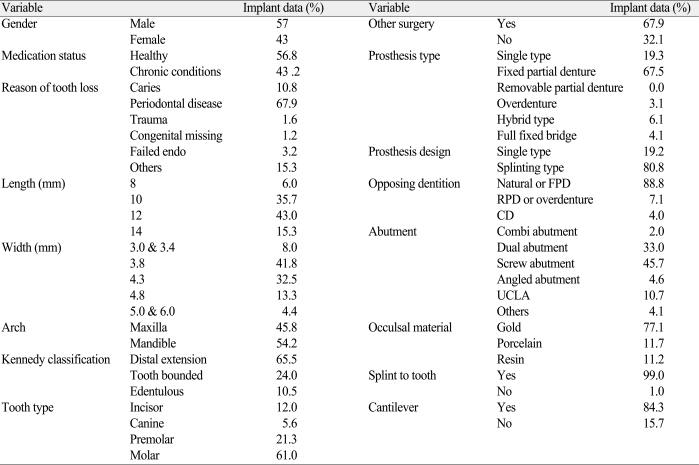
The mean duration of clinical follow-up time of implants was 5.1 years. A total 95 patients were treated using 249 implants to support or retain dental prostheses. Patient ages ranged from 20 to 75 years (mean 56.8 years) (Fig. 3), and 42 patients reported general health problems (43.2%). The descriptive statistics are summarized in Table 1. The most frequently used implants lengths were 12 mm (43.0%) and 10 mm (35.7%). Diameters of the implants were mainly 3.8 mm and 4.3 mm. 135 (54.2%) implants were placed in the mandible and 114 (45.8%) in the maxilla. Regarding the prostheses used, most of the implants supported a fixed partial denture (67.5%) and 38 implants had a single crown (19.3%). The greater part of fixed bridge type was screw retained prosthesis (45.7%). Most implants (174) were opposed to natural teeth or implants (88.8%).
Fig. 3.
Age distribution of the patient at the implant installation.
Table 1.
Distribution of implant according to variables
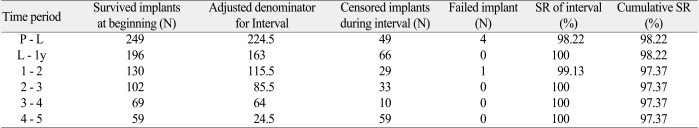
Implant Survival Rates and Loss
Of the 249 implants, 5 implants failed. Four of these were removed between placement and loading. Other one implant was lost after loading for 2 years as a result of a horizontal fixture fracture. Two of 4 failed implants were removed and replaced with new fixtures before loading forces were applied. And one failed implant after loading was replaced with a new one within 3 months. A life table analysis is present in Table 2 showing 97.37% cumulate survival rate after 5 years of follow up (Table 2).
Table 2.
Life table analysis showing cumulative survival rates
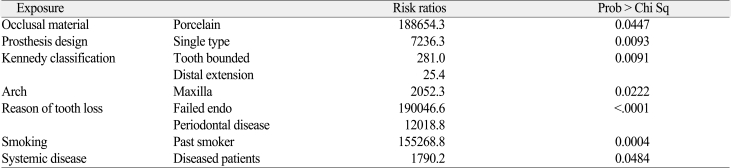
Risk Factors
Occlusal material, prosthesis design, Kennedy classification, arch, the reason of tooth loss, smoking and systemic diseases were statically associated with implant failure (Table 3). The patient who had porcelain occlusal materials, single type prosthesis design, tooth borne case, implant in maxilla site, the tooth loss as a result of failed endodontic treatment, and systemic diseases is more likely to experience implant failure than the other patients. There was no significant association between other risk factors and failure.
Table 3.
Log-Rank test associated with implant failure
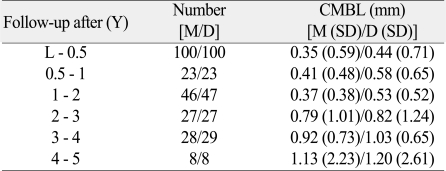
Marginal Bone Level
Implants remaining in the 95 patients at the 5-year revealed no signs of persisting peri-implant radiolucencies. Evaluation of the radiographs showed that an annual average bone loss each mesial and distal side was 0.18 mm and 0.19 mm after loading. The mean value in mm and standard deviations (SD) of the marginal bone changes from baseline up to the 1-year after loading were 0.41 (0.48) / 0.58 (0.65) (Table 4) (Fig. 4).
Table 4.
Cumulative mean marginal bone loss (CMBL)
L: Loading, M: Mesial, D: Distal, SD: Standard Deviation
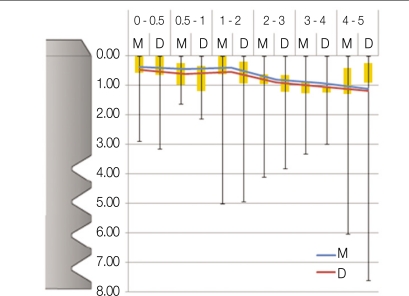
Fig. 4.
Box plot chart with the mean marginal bone level change (blue and red line). A black line shows a difference between the maximum and minimum bone level change.
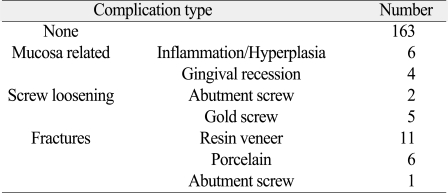
Complications
There were few complications related to peri-implantitis (2%). The most common prosthetic complication encountered was fracture of the resin veneer and porcelain. One abutment screw was fractured in the case using single dual abutment. The other problem related to screw was loosening of gold and abutment screw (Table 5). All complications were easily solved.
Table 5.
Number of complications after loading
DISCUSSION
This study was to document the long-term clinical outcome of the Dentium implants for 5 years, to evaluate this system according to the criteria for survival according to Albrektsson and Zarb18 and to determine the risk factors of implant failure in Korean population. In a total of 249 implants, four implants failed in the early postsurgical healing period. One implant was removed after 2 years in function period due to implant fixture fracture. It would be probably associated with over load. The reasons of early failures of implants could be bone necrosis, infection of bacteria, bone quality, micromovement after placement, early loading and weak initial stability. Meanwhile, the late failure might be affected by a poor oral hygiene, excessive occlusal load, misfit of prosthesis and so on. Esposito et al. suggested that major etiologic factors of late failure was excessive occlusal load related to parafunction such as bruxism and infection. Also patient's immune reaction and implant surface properties could influence a failure.9-11 The overall 5-year cumulated survival rate in this study was reported 97.37%, which was similar to prior reports of TiUnite Implant system and Astra system.20,21 Adell et al. reported that failed rate in each interval was the highest within 1 to 2 years and was decreasing after that due to increasing stability.17
General health problems and past smoking history increased the risk of implant failure. This result was similar to other studies. Moy et al.22 reported that patients over age 60, smoked, had a history of diabetes or postmenopausal, increased implant failure compared with healthy patient. They suggested that smoking caused both systemic and local injury to tissues and is common contributor to decreased tissue oxygenation, which negatively affects wound healing. The diabetes could delay the wound healing response following-implant insertion and may be related to mechanical characteristics of the boneto-implant contact.23
Among the reason of tooth loss, failed endodontic treatment and periodontitis increased risk of implant failures. Remaining infection might be the cause of the failure. There are no previous studies about relationship between failed endodontic treatment and implant survival rate. However, some studies reported about periodontitis patients. The patient who had treated a periodontitis had a lower survival rate with increased marginal bone resorption than a patient in a healthy condition.24-26
All removed implants were initially placed in maxilla, so implants placed in maxilla were also associated with an increased risk for failure compared to implants placed in mandible. There is no significant difference between anterior part and posterior part. Many studies reported similar results. Recent research showed that average cumulative success rate in maxilla was higher than in mandible.22,27 Tolstunov represented about implant location and related success rate. His findings were that implant location seemed to be significant factors in a success-analysis of dental implants.28
In present studies, implant length and width are not associated with risk factor. These results conflict with earlier findings. Some studies reported that implant length influence the implant survival rate.29,30 And some studies discussed that implant diameter affected survival of implant.31-33 These differences may be due to other variables affecting implant survival, including the implant surface, the surgeon's learning curve, bone quality and quantity.
Cumulative marginal bone level alteration adjacent to the fixture has been documented over the 5 years. Changes in marginal bone level between baseline and annual follow-up were calculated. In most implants, the marginal bone level showed very small changes over the follow-up period. The mean difference of bone level changes in each mesial and distal side were 0.41 (0.48) / 0.58 (0.65) in the 1st year and 1.13 (2.23) / 1.20 (2.61) in the 5th year as compared from the base line. An annual average bone loss each mesial and distal side was 0.18 mm and 0.19 mm after loading. It is lower than 0.2 mm per year, which is in accordance with Albrektsson's criteria19, indicating acceptable bone level maintenance around implant. But some patients underwent an aggressive bone resorption. It had to be considered with relation to risk factors. Intraoral radiograph is still one of the most sensitive ways of identifying loss of bone support. In the present study, there are some limitations on accurate information about bone level changes. The parallel intraoral radiograph taking technique was used for projection angle of 90° to fixture axis, but a specially constructed film-holder was not used for this study. And intraoral radiographs disclose bone status from mesial and distal aspects only.
The 5 year CSR of overall implants was 97.37%. However, there are a few limitations in this study. Because of retrospective study, the sampling was limited and the nature and quality of the predictor variables and confounding variables are dependent on the accuracy and quantity of the past record. In addition, the number of patients and implants were not large enough and this study was undertaken in one hospital. However, the results could be accepted for the clinical research, because it is essential to be supported with a minimum of 50 consecutive patients and in at least 5 years.
Further study is necessary to evaluate the relationship between patient oral hygiene and soft tissue reactions. If well-controlled prospective study is perform, more favorable result might be achieved.
CONCLUSION
1. Of the 249 implants, 5 implants were failed and the 5-year CSR of Dentium implant system was 97.22%.
2. Implant survival may depend on systemic disease, smoking, reasons of tooth loss, arch, the edentulous site (by Kennedy classification) and prosthodontic design.
3. An annual average bone loss at each mesial and distal side was 0.18 mm and 0.19 mm.
4. There were few complications related to peri-implantitis and the most common prosthetic complication encountered was fracture of the resin veneer and porcelain.
References
- 1.Brånemark PI, Hansson BO, Adell R, Breine U, Lindström J, Hallén O, Ohman A. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl. 1977;16:1–132. [PubMed] [Google Scholar]
- 2.Fugazzotto PA, Gulbransen HJ, Wheeler SL, Lindsay JA. The use of IMZ osseointegrated implants in partially and completely edentulous patients: success and failure rates of 2,023 implant cylinders up to 60+ months in function. Int J Oral Maxillofac Implants. 1993;8:617–621. [PubMed] [Google Scholar]
- 3.Wedgwood D, Jennings KJ, Critchlow HA, Watkinson AC, Shepherd JP, Frame JW, Laird WR, Quayle AA. Experience with ITI osseointegrated implants at five centres in the UK. Br J Oral Maxillofac Surg. 1992;30:377–381. doi: 10.1016/0266-4356(92)90204-v. [DOI] [PubMed] [Google Scholar]
- 4.Leimola-Virtanen R, Peltola J, Oksala E, Helenius H, Happonen RP. ITI titanium plasma-sprayed screw implants in the treatment of edentulous mandibles: a follow-up study of 39 patients. Int J Oral Maxillofac Implants. 1995;10:373–378. [PubMed] [Google Scholar]
- 5.Palmer RM, Palmer PJ, Smith BJ. A 5-year prospective study of Astra single tooth implants. Clin Oral Implants Res. 2000;11:179–182. doi: 10.1111/j.1600-0501.2000.tb00012.x. [DOI] [PubMed] [Google Scholar]
- 6.Wennström JL, Ekestubbe A, Gröndahl K, Karlsson S, Lindhe J. Implant-supported single-tooth restorations: a 5-year prospective study. J Clin Periodontol. 2005;32:567–574. doi: 10.1111/j.1600-051X.2005.00715.x. [DOI] [PubMed] [Google Scholar]
- 7.Abrahamsson I, Berglundh T. Tissue characteristics at microthreaded implants: an experimental study in dogs. Clin Implant Dent Relat Res. 2006;8:107–113. doi: 10.1111/j.1708-8208.2006.00016.x. [DOI] [PubMed] [Google Scholar]
- 8.Abrahamsson I, Berglundh T, Linder E, Lang NP, Lindhe J. Early bone formation adjacent to rough and turned endosseous implant surfaces. An experimental study in the dog. Clin Oral Implants Res. 2004;15:381–392. doi: 10.1111/j.1600-0501.2004.01082.x. [DOI] [PubMed] [Google Scholar]
- 9.Esposito M, Hirsch JM, Lekholm U, Thomsen P. Biological factors contributing to failures of osseointegrated oral implants. (II). Etiopathogenesis. Eur J Oral Sci. 1998;106:721–764. doi: 10.1046/j.0909-8836..t01-6-.x. [DOI] [PubMed] [Google Scholar]
- 10.Esposito M, Hirsch JM, Lekholm U, Thomsen P. Biological factors contributing to failures of osseointegrated oral implants. (I). Success criteria and epidemiology. Eur J Oral Sci. 1998;106:527–551. doi: 10.1046/j.0909-8836..t01-2-.x. [DOI] [PubMed] [Google Scholar]
- 11.Esposito M, Thomsen P, Ericson LE, Sennerby L, Lekholm U. Histopathologic observations on late oral implant failures. Clin Implant Dent Relat Res. 2000;2:18–32. doi: 10.1111/j.1708-8208.2000.tb00103.x. [DOI] [PubMed] [Google Scholar]
- 12.Smith RA, Berger R, Dodson TB. Risk factors associated with dental implants in healthy and medically compromised patients. Int J Oral Maxillofac Implants. 1992;7:367–372. [PubMed] [Google Scholar]
- 13.Matukas VJ. Medical risks associated with dental implants. Int J Oral Implantol. 1988;5:49–50. [PubMed] [Google Scholar]
- 14.Kim SH, Kim S, Lee KW, Han DH. The effects of local factors on the survival of dental implants: A 19 year retrospective study. J Korean Acad Prosthodont. 2010;48:28–40. [Google Scholar]
- 15.Ko SM, Lee JK, Eckert SE, Choi YG. Retrospective multicenter cohort study of the clinical performance of 2-stage implants in South Korean populations. Int J Oral Maxillofac Implants. 2006;21:785–788. [PubMed] [Google Scholar]
- 16.Doh RM, Moon HS, Shin JS, Lee KW. Retrospective study of the implantium(R) implant with a SLA surface and internal connection with microthreads. J Korean Acad Prosthodont. 2009;47:136–147. [Google Scholar]
- 17.Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10:387–416. doi: 10.1016/s0300-9785(81)80077-4. [DOI] [PubMed] [Google Scholar]
- 18.Albrektsson T, Zarb GA. Current interpretations of the osseointegrated response: clinical significance. Int J Prosthodont. 1993;6:95–105. [PubMed] [Google Scholar]
- 19.Roos J, Sennerby L, Lekholm U, Jemt T, Gröndahl K, Albrektsson T. A qualitative and quantitative method for evaluating implant success: a 5-year retrospective analysis of the Brånemark implant. Int J Oral Maxillofac Implants. 1997;12:504–514. [PubMed] [Google Scholar]
- 20.Glauser R, Lundgren AK, Gottlow J, Sennerby L, Portmann M, Ruhstaller P, Hämmerle CH. Immediate occlusal loading of Brånemark TiUnite implants placed predominantly in soft bone: 1-year results of a prospective clinical study. Clin Implant Dent Relat Res. 2003;5:47–56. doi: 10.1111/j.1708-8208.2003.tb00015.x. [DOI] [PubMed] [Google Scholar]
- 21.Rasmusson L, Roos J, Bystedt H. A 10-year follow-up study of titanium dioxide-blasted implants. Clin Implant Dent Relat Res. 2005;7:36–42. doi: 10.1111/j.1708-8208.2005.tb00045.x. [DOI] [PubMed] [Google Scholar]
- 22.Moy PK, Medina D, Shetty V, Aghaloo TL. Dental implant failure rates and associated risk factors. Int J Oral Maxillofac Implants. 2005;20:569–577. [PubMed] [Google Scholar]
- 23.Fiorellini JP, Nevins ML, Sekler J, Chung A, Oringer RJ. Correlation of peri-implant health and aspartate aminotransferase levels: a cross-sectional clinical study. Int J Oral Maxillofac Implants. 2000;15:500–504. [PubMed] [Google Scholar]
- 24.Stanford C. Dental implant outcomes may vary in patients with a history of periodontal disease. J Evid Based Dent Pract. 2010;10:46–48. doi: 10.1016/j.jebdp.2009.11.016. [DOI] [PubMed] [Google Scholar]
- 25.Schou S, Holmstrup P, Worthington HV, Esposito M. Outcome of implant therapy in patients with previous tooth loss due to periodontitis. Clin Oral Implants Res. 2006;17:104–123. doi: 10.1111/j.1600-0501.2006.01347.x. [DOI] [PubMed] [Google Scholar]
- 26.Ong CT, Ivanovski S, Needleman IG, Retzepi M, Moles DR, Tonetti MS, Donos N. Systematic review of implant outcomes in treated periodontitis subjects. J Clin Periodontol. 2008;35:438–462. doi: 10.1111/j.1600-051X.2008.01207.x. [DOI] [PubMed] [Google Scholar]
- 27.Bass SL, Triplett RG. The effects of preoperative resorption and jaw anatomy on implant success. A report of 303 cases. Clin Oral Implants Res. 1991;2:193–198. doi: 10.1034/j.1600-0501.1991.020406.x. [DOI] [PubMed] [Google Scholar]
- 28.Tolstunov L. Implant zones of the jaws: implant location and related success rate. J Oral Implantol. 2007;33:211–220. doi: 10.1563/1548-1336(2007)33[211:IZOTJI]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 29.Wyatt CC, Zarb GA. Treatment outcomes of patients with implant-supported fixed partial prostheses. Int J Oral Maxillofac Implants. 1998;13:204–211. [PubMed] [Google Scholar]
- 30.Jemt T, Lekholm U. Implant treatment in edentulous maxillae: a 5-year follow-up report on patients with different degrees of jaw resorption. Int J Oral Maxillofac Implants. 1995;10:303–311. [PubMed] [Google Scholar]
- 31.Shin SW, Bryant SR, Zarb GA. A retrospective study on the treatment outcome of wide-bodied implants. Int J Prosthodont. 2004;17:52–58. [PubMed] [Google Scholar]
- 32.Eckert SE, Meraw SJ, Weaver AL, Lohse CM. Early experience with Wide-Platform Mk II implants. Part I: Implant survival. Part II: Evaluation of risk factors involving implant survival. Int J Oral Maxillofac Implants. 2001;16:208–216. [PubMed] [Google Scholar]
- 33.Attard NJ, Zarb GA. Implant prosthodontic management of partially edentulous patients missing posterior teeth: the Toronto experience. J Prosthet Dent. 2003;89:352–359. doi: 10.1067/mpr.2003.91. [DOI] [PubMed] [Google Scholar]