Abstract
Aim
The aim of this study is to compare the 24-hour efficacy of dorzolamide/timolol-fixed combination (DTFC) and brimonidine/timolol-fixed combination (BTFC) in primary open-angle glaucoma (POAG).
Methods
One eye each of 77 POAG patients was included in this prospective, observer-masked, crossover comparison. Following a 2-month timolol run-in period, patients had three intraocular pressure (IOP) measurements at 1000, 1200 and 1400 h while on timolol treatment. Patients showing at least a 20% IOP reduction on timolol were randomised to 3 months of therapy with DTFC or BTFC, and then were crossed over to the opposite therapy.
Results
Sixty POAG patients completed the study. The mean 24-hour IOP was significantly reduced with both the fixed combinations compared with the timolol-treated diurnal IOP (P<0.001). When the two fixed combinations were compared directly, DTFC demonstrated a lower mean 24-hour IOP level as compared with BTFC (mean difference: −0.7 mm Hg, 95% confidence interval (CI): (−1.0, −0.3), P<0.001). At two individual time points, DTFC significantly reduced IOP more than BTFC: at 1800 h (−1.0 mm Hg, 95% CI (−1.6,−0.5), P=0.001) and at 0200 (−0.9 mm Hg, 95% CI: (−1.4,−0.5), P=0.001). No significant difference existed for the other time points.
Conclusion
Both the fixed combinations significantly reduce 24-hour IOP in POAG. DTFC provided significantly better 24-hour efficacy.
Keywords: dorzolamide/timolol, brimonidine/timolol, 24-hour IOP, POAG
Introduction
Orally administered fixed-dose combinations have been shown to improve adherence to chronic medical therapy.1, 2, 3, 4 It is known that almost half of the patients with chronic, asymptomatic diseases do not take their medications as prescribed.5, 6, 7, 8 In medicine, a recent meta-analysis showed that non-adherence to medical therapy is reduced by 24–26% with fixed-dose combination regimens compared with unfixed concomitant therapies.3 Fixed combinations of glaucoma medications, in most cases, provide similar intraocular pressure (IOP) reduction to that observed with simultaneous administration of their individual components,1, 9 simplify adjunctive medication regimens,10, 11 reduce the incidence of adverse events,12, 13 and may improve adherence and long-term tolerability.1, 12, 14
The dorzolamide/timolol-fixed combination (DTFC, Cosopt) and the brimonidine/timolol-fixed combination (BTFC, Combigan) are commonly-prescribed fixed combinations for the treatment of glaucoma that have been approved in several countries worldwide.12, 13 Separate diurnal IOP comparisons between fixed and unfixed therapy with DTFC15 and BTFC16 have reported similar efficacy. More recently, a study in which IOP was measured over 24 h17 compared, for the first time, BTFC with the concomitant administration of its individual components and reported similar efficacy between the two regimens. Nevertheless, the mean IOP reduction over 24 h (22%) observed with BTFC was less than anticipated.17 Although this range of pressure reduction is consistent with the evidence obtained from the regulatory trials for BTFC,18, 19 the extent of the 24-h IOP reduction is less than that observed with DTFC.20 Specifically, with DTFC, reported daytime IOP reduction ranges from 27 to 33%21, 22, 23, 24 and the 24-h IOP reduction ranges between 26 and 28%25, 26, 27 in published studies.
At present, there are few data from randomised clinical studies directly comparing these two fixed combinations, and the data that have been reported suggest similar daytime efficacy.28, 29 A more detailed comparison of the efficacy of the two combinations can be made by recording IOP throughout a 24-h period.30
The purpose of the present study is to compare the difference in IOP-lowering efficacy when measured over 24 h, between these two fixed combinations in patients with primary open-angle glaucoma (POAG).
Materials and methods
Informed consent was obtained from all participants before they entered this observer-masked, crossover study.
Patient eligibility
Consecutive adults with newly diagnosed, early-to-moderate POAG (defined as glaucomatous disc damage with vertical disc cupping not exceeding 0.8. and reproducible glaucomatous visual field loss less than 12.0 dB in the study eye with Humphrey 24-2 automated perimetry) were recruited in three academic participating centres: the Glaucoma Unit of the 1st University Department of Ophthalmology, AHEPA Hospital, Thessaloniki, Greece; the Center for the Study of Glaucoma, University of Brescia, Brescia, Italy; and Ophthalmic Consultant Centres, University of Toronto, Mississauga, ON, Canada. All study candidates had to exhibit a typical disc or visual field damage, a mean untreated IOP greater than 25 mm Hg at baseline (two IOP measurements performed at 1000±1 h), and central corneal thickness between 500–600 μm.
All newly diagnosed, previously untreated POAG patients who agreed to participate and met the inclusion and exclusion criteria in the three study centres were enrolled. Inclusion criteria were age between 39 and 85 years; best-corrected distance Snellen visual acuity greater than 0.1 in the study eye; early-to-moderate POAG (defined as patients who exhibit glaucomatous disc damage with disc cupping not exceeding 0.8, and reproducible glaucomatous visual field loss with a mean deviation better than −12.0 dB in the study eye with Humphrey 24-2 SITA standard automated perimetry); patient could safely undergo wash out; open anterior chamber angles; untreated baseline IOP greater than 25 mm Hg, and lower than 40 mm Hg at 1000 (±1 h).
Exclusion criteria
Exclusion criteria were evidence of concurrent conjunctivitis, keratitis, or uveitis in either eye; history of ocular herpes simplex, or macular oedema; history of inadequate adherence; allergic hypersensitivity, intolerance, or contraindication to either β-blockers, brimonidine, dorzolamide, or benzalconium chloride; intraocular conventional or laser surgery in the study eye; child-bearing potential or lactation; previous history of ocular trauma; use of corticosteroids (within 2 months before the enrolment), severe dry eyes; and use of contact lenses. The demographics of the study patients are shown in Table 1.
Table 1. Baseline characteristics (n=60 completed patients).
| Characteristic | |
|---|---|
| Male, n (%) | 27 (45.0) |
| Female, n (%) | 33 (55.0) |
| Mean age (years)±SD | 65.3±11.9 |
| Range | 31.0, 81.0 |
| Mean morning baseline IOP pressure (mm Hg)±SD | 27.9±2.7 |
| Mean Snellen best-corrected visual acuity±SD | 0.9±0.2 |
| Mean vertical cup/disc ratio±SD | 0.6±0.2 |
| Mean visual field loss mean deviation (dB)±SD | −4.5±3.6 |
Abbreviation: IOP, intraocular pressure.
Procedures
All eligible patients underwent first a timolol 0.5% run-in period for at least 8 weeks before the randomisation to either DTFC or BTFC. Enrolled patients were treated for at least 8 weeks with timolol 0.5% given twice daily (0800 and 2000 h). After this run-in period, they underwent a timolol-treated daytime IOP assessment with three separate IOP measurements performed at 1000, 1200 and 1400 h. Only patients with a mean daytime IOP (average of these three measurements) on timolol monotherapy greater than 18 mm Hg, and a mean reduction of morning IOP (1000±1 h), at least 20%, were randomised for period 1 to either 3 months of chronic therapy with DTFC given twice daily (0800 and 2000 h), or to 3 months with BTFC given twice daily (0800 and 2000 h). At the end of period 1, all study patients underwent a treated 24-h IOP assessment. Patients then were switched for period 2 to the opposite therapy (with either DTFC or BTFC), and at the end of this period, they also underwent a 24-h IOP evaluation.
During the eligibility visit, subjects' ophthalmic and systemic histories were recorded. Slit lamp biomicroscopy, dilated fundoscopy, and automated threshold perimetry were performed, and best-corrected visual acuity and IOP were measured. Enrolled subjects were admitted to hospital and underwent 24-h IOP monitoring at 1000, 1400 1800, 2200, 0200, and 0600 h (±1 h) while sitting upright. Two pressure readings were taken for every time point of the 24-h curve.
The subsequent study phases were observer-masked. Study patients were randomly assigned to receive BTFC drops (Combigan, Allergan Inc., Irvine, CA, USA) twice daily (0800 and 2000 h), or DTFC drops (Cosopt, Merck, Whitehouse Station, NJ, USA) administered twice daily (0800 and 2000 h) for Period 1. At the end of Period 1, all patients were switched to the opposite dosing regimen for Period 2. Patients were instructed regarding correct medication instillation and compliance. A safety visit was carried out 2 weeks after the two treatment periods. At the end of each treatment period, a 24-h IOP curve and a detailed clinical examination were performed. The IOP was always measured by the same investigators who were unaware of the treatment regime, using the same calibrated Goldmann tonometer.
Statistics
The primary efficacy endpoint for this crossover study was the mean 24-h IOP (the mean pressure for the six time points measured). The individual time points, peak, minimum, and 24-h IOP fluctuation were evaluated as secondary endpoints. A generalised estimating equation was used for the crossover repeated measures design to adjust for site differences and baseline, or timolol run-in IOP. A 95% confidence interval (CI) was constructed for the adjusted difference in means. An intention-to-treat approach was adopted, and the subjects were analysed according to their randomised group. The mean IOP of all other patients in the corresponding treatment group was used to impute the missing data for those subjects lost to follow-up. In addition, the per-protocol analysis was performed.
The modified Bonferroni-adjusted P-values were reported to correct the analyses for multiple comparisons with individual time points.31 All other reported P-values were two-tailed, with P<0.05 considered as significant. This 24-h study had at least 85% power to identify a 1.0 mm Hg difference between individual time points and between mean 24-h pressures assuming an SD of 2.5 mm Hg between treatments.
Adverse events were evaluated by McNemar's test for all patients that completed this study.32 Analyses were conducted using SPSS 15.0 (SPSS Inc., Chicago, IL, USA).
Results
Patients
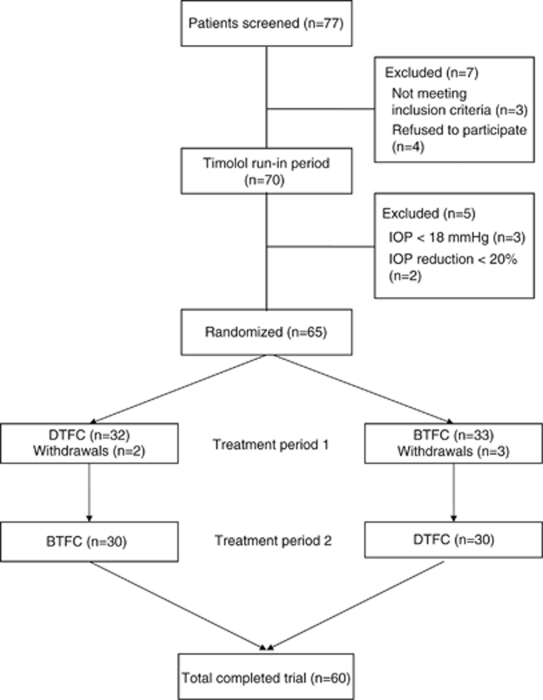
Patient characteristics of those included in this study are shown in Table 1. Sixty patients completed the study out of 77 enrolled. The flow diagram of study participants is presented in Figure 1. Four patients withdrew after randomisation and declined further participation due to difficulties in undergoing repeated IOP monitoring; none of those discontinuations were due to adverse events. Out of the 70 study patients who underwent the timolol diurnal curve, 5 did not meet the study IOP inclusion criterion, and were excluded. From the 65 patients who were randomised to the fixed combination therapies, 5 were withdrawn due to adverse events: 2 in the DTFC period and 3 in the BTFC period. Two patients were discontinued due to intolerance to DTFC; one patient was discontinued from the BTFC group due to systemic hypotension, and two due to intolerance.
Figure 1.
Flow diagram of patients enrolled in study.
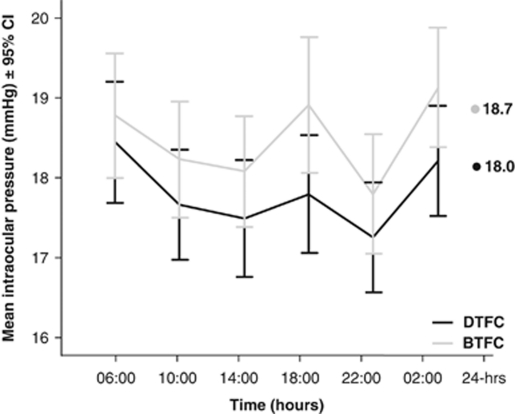
Intraocular pressure
The mean 24-h IOP, and the IOP reductions from untreated baseline and from the mean timolol-treated diurnal IOP are shown in Table 2 and Figure 2. The mean 24-h IOP was significantly reduced from the timolol diurnal IOP baseline for both the fixed combinations (−2.9 mm Hg (13.9%) for DTFC and 2.2 mm Hg (10.5%) for BTFC; P<0.001). When the two fixed combination treatments were compared directly, the DTFC demonstrated a lower absolute IOP level for the 24-h curve, compared with the BTFC (mean difference: −0.7 mm Hg, 95% CI: −1.0, −0.3).
Table 2. Comparison of IOP levels (mm Hg).
| Untreated (95% CI) | Diurnal timolol (95% CI) | 24-h DTFC (95% CI) | 24-h BTFC (95% CI) | |
|---|---|---|---|---|
| Mean | 27.9 (27.2, 28.7)a | 20.9 (20.4, 21.4)b | 18.0 (17.5, 18.6)c | 18.7 (18.1, 19.4)c |
| Mean adjusted difference from untreated | — | −6.9 (−7.4, −6.4)b P<0.001 | −9.9 (−10.6, −9.2)c P<0.001 | −9.2 (−9.9, −8.5)c P<0.001 |
| Mean adjusted difference from diurnal timolol | — | — | −2.9 (−3.4, −2.5)c P<0.001 | −2.2 (−2.8, −1.7)c P<0.001 |
| Mean 24-h adjusted difference | — | — | −0.7 (−1.0, −0.3)c P<0.001 | — |
Abbreviations: BTFC, brimonidine/timolol-fixed combination; CI, confidence interval; DTFC, dorzolamide/timolol-fixed combination.
Adjusted for site.
Adjusted for site and untreated IOP.
Adjusted for site and timolol run-in period.
Figure 2.
The figure shows the mean IOP±95% CI at each individual time point and for the 24-h pressure for DTFC (solid black line) and BTFC (gray line) treatment groups.
In Table 3, the absolute IOP of the individual time points, peak, minimum, and 24-h fluctuation (or range) together with their mean differences are being compared between the two fixed combination treatment groups. At two individual time points (1800 and 0200 h), DTFC reduced IOP significantly more than BTFC (P=0.001 for both comparisons). No statistical differences existed for the other four time points: 0600, 1000, 1400, and 2200 h (P>0.05), and for the 24-h fluctuation (P=0.34). The peak and minimum 24-h IOP were, however, significantly lower with DTFC compared with BTFC (P=0.003 and P=0.033, respectively). These results were similar when the per-protocol analysis was performed.
Table 3. Absolute IOP levels (mm Hg).
| Time points (h) | DTFC Mean (95% CI) | BTFC Mean (95% CI) | Mean adjusted difference (95% CI)a | P-value |
|---|---|---|---|---|
| 0600 | 18.4 (17.7, 19.1) | 18.7 (18.0, 19.5) | −0.3 (−0.9, 0.2) | 0.203b |
| 1000 | 17.7 (17.0, 18.3) | 18.2 (17.5, 18.9) | −0.5 (−1.1 0.1) | 0.070b |
| 1400 | 17.5 (16.9, 18.2) | 18.1 (17.4, 18.7) | −0.5 (−1.1, −0.1) | 0.057b |
| 1800 | 17.9 (17.1, 18.6) | 18.9 (18.1, 19.7) | −1.0 (−1.6, −0.5) | 0.001b |
| 2200 | 17.2 (16.6, 17.9) | 17.8 (17.1, 18.5) | −0.6 (−1.1, 0.1) | 0.068b |
| 0200 | 18.2 (17.6, 18.8) | 19.1 (18.4, 19.8) | −0.9 (−1.4, −0.5) | 0.001b |
| Mean 24 | 18.0 (17.5, 18.6) | 18.7 (18.1, 19.4) | −0.7 (−1.0, −0.3) | <0.001 |
| Maximum | 20.0 (19.3, 20.6) | 20.7 (20.0, 21.4) | −0.7 (−1.2, −0.3) | 0.002 |
| Minimum | 15.8 (15.3, 16.4) | 16.3 (15.7, 17.0) | −0.5 (−0.9, −0.1) | 0.033 |
| Fluctuation | 4.1 (3.6, 4.6) | 4.3 (3.8, 4.9) | −0.2 (−0.7, 0.2) | 0.340 |
Abbreviations: BTFC, brimonidine/timolol-fixed combination; CI, confidence interval; DTFC, dorzolamide/timolol-fixed combination.
Adjusted for site and timolol run-in period.
Modified Bonferroni adjusted P-values.
Adverse events
No serious adverse event concerns were identified during this study. Patients treated with DTFC experienced bitter taste (18.3%) and stinging (16.7%) more often than when treated with BTFC (P=0.001 and P=0.012, respectively). Conversely, more patients experienced conjuctival hyperaemia with BTFC compared with DTFC (16.7 vs 5.0%, P=0.039). There were no significant differences in the other adverse events between the two fixed combination treatment groups (see Table 4).
Table 4. Adverse events recorded in the study (n=60 completed patients).
| Adverse eventa | DTFC, n (%) | BTFC, n (%) | P-value |
|---|---|---|---|
| Bitter taste | 11 (18.3) | 0 (0) | 0.001 |
| Stinging | 10 (16.7) | 1 (1.7) | 0.012 |
| Conjunctival hyperaemia | 3 (5.0) | 10 (16.7) | 0.039 |
| Itchiness | 1 (1.7) | 7 (11.7) | 0.070 |
| Burning | 4 (6.7) | 0 (0) | 0.125 |
| Systemic hypotension | 0 (0) | 4 (6.7) | 0.125 |
| Dry mouth | 0 (0) | 4 (6.7) | 0.125 |
| Foreign body sensation | 0 (0) | 3 (5.0) | 0.250 |
| Dry eye sensation | 1 (1.7) | 3 (5.0) | 0.625 |
| Fatigue | 1 (1.7) | 3 (5.0) | 0.625 |
| Watering | 1 (1.7) | 2 (3.3) | 1.000 |
| SPK | 1 (1.7) | 0 (0) | 1.000 |
| Ocular discharge | 0 (0) | 1 (1.7) | 1.000 |
| Eyelid swelling | 1 (1.7) | 0 (0) | 1.000 |
| Headache | 0 (0) | 1 (1.7) | 1.000 |
| Dizziness | 0 (0) | 1 (1.7) | 1.000 |
| Drowsiness | 0 (0) | 1 (1.7) | 1.000 |
Abbreviations: BTFC, brimonidine/timolol-fixed combination; CI, confidence interval; DTFC: dorzolamide/timolol-fixed combination.
Some patients experienced multiple adverse events.
Discussion
Fixed combination therapy in glaucoma has gained popularity in recent years, presumably because of the perceived benefits of greater patient convenience and adherence.1, 2, 3 At present, DTFC and BTFC are the only fixed combinations approved by the Food and Drug Administration in the United States.12 To date, regulatory approval for fixed combination therapy for glaucoma is based on efficacy and safety comparisons between fixed combinations and the individual components, or the concomitant use of both constituents.1, 9, 12 This approach, solely based on pharmacologic efficacy, is not ideal, as it does not take into account other important clinical benefits such as enhanced adherence, improved convenience, and reduced cost to patients.1 Moreover, there is no uniformity among regulatory trials, and it is generally difficult to compare the efficacy between fixed combinations in the same therapeutic category.
To the best of our knowledge, this is the first study comparing the 24-h efficacy of these two fixed combinations. Although both BTFC and DTFC dose timolol 0.5% twice daily, the pharmacologic difference in the second component of these fixed combinations (brimonidine vs dorzolamide) may account for the relative differences in 24-h IOP efficacy observed in the present study. Brimonidine is a relatively short-acting medication, and when instilled twice daily, may have a relatively weak IOP-lowering effect at trough and during the night.33, 34, 35 In the study by Orzalesi et al,34 brimonidine monotherapy dosed twice daily did not significantly reduce IOP from untreated baseline at 1800 and 0300 time points. These time points closely mirror the two time points in our study (1800 and 0200) in which DTFC provided significantly better IOP control than BTFC. Further, a recent 24-h study by Liu et al36 demonstrated the absence of measurable nocturnal efficacy for brimonidine even with three times per day dosing. It is worthwhile noting that in that 24-h study, there was no statistically significant change in IOP under brimonidine therapy compared with baseline untreated IOP during the nocturnal period, but there was a significant lowering of IOP during the daytime diurnal period in both supine and sitting positions.36 In contrast, dorzolamide monotherapy has demonstrated significant nocturnal IOP-lowering efficacy.20, 35, 37 In two separate 24-h studies,35, 37 the nocturnal efficacy of dorzolamide was equivalent to that of latanoprost. A recent meta-analysis of 24-h studies demonstrated that mean reduction of night time points (1800, 2200, and 0200 h) was statistically lower than that of day time points for timolol and brimonidine, but not for dorzolamide.20 This meta analysis is again consistent with the 1800 and 0200 h time points in this study, when BTFC was statistically inferior to DTFC.
Our study enrolled newly diagnosed, previously untreated POAG patients with a relatively high-untreated IOP to ensure uniformity of the study cohort and to enhance the power of study, to detect any differences between the two medications if present. The study design employed three relatively stringent inclusion criteria of (1) baseline untreated IOP >25 mm Hg, (2) initial response to timolol 0.5 >20%, and (3) timolol-treated IOP >18 mm Hg. These strict inclusion criteria ensured that both timolol non-responders and patients who had already reached a reasonable target IOP with timolol monotherapy were both excluded from the study. Timolol dosed twice daily reduced untreated IOP in our cohort by 25.1%. The efficacy comparison between timolol run-in and the treatment periods with the two medications under investigation indicate that both fixed combinations significantly reduced mean 24-h IOP compared with timolol monotherapy.
The comparison between the two fixed combinations in this study demonstrated that DTFC was superior to BTFC at two individual time points (1800 and 0200 h), as well as the mean, maximum, and minimum 24-h pressure. However, mean 24-h IOP fluctuation was similar between DTFC and BTFC. Our results demonstrated a significant difference between DTFC and BTFC (−0.7 mm Hg over a 24-h period), unlike the findings of the two previous daytime studies in which no significant difference was detected.28, 29 Significant differences in this study design compared with those previous studies include: (1) crossover design vs parallel arm, (2) inclusion of only POAG patients, (3) a higher baseline untreated IOP, (4) exclusion of patients adequately responding to timolol monotherapy, and (5) a more complete 24-h IOP evaluation of the two fixed combinations. All of the above factors contributed to a greater power in this study to detect small but significant differences between the two fixed combinations.
Although most previously published daytime studies28, 29 have demonstrated similar IOP-lowering efficacy for BTFC over DTFC, a recent 3-month parallel-arm study by Nixon et al38 reported a greater IOP reduction with BTFC monotherapy (−7.7 mm Hg) compared with DTFC monotherapy (−6.7 mm Hg). The study by Nixon et al38 pooled data from two separate trials: a single site pilot study with 40 patients, and a multi-centre trial with 140 patients. Out of the total of 180 patients, 101 were treated with BTFC or DTFC as monotherapy (30 from the pilot study, 71 from the multi-centre trial), whereas 79 patients were treated as an adjunct to prostaglandin therapy.38 The methodology of that study was critically differed from the protocol utilised in the present study in several ways. First, the Nixon study38 measured IOP at a single time point (1000) at 2 h post dose. This time point would be near the peak efficacy for brimonidine, which tends to have a rapid onset of action.12, 18, 19, 20, 39 The current study measures IOP every 4 h over a 24-h time period. Although no differences between the two fixed combinations were observed at the two corresponding time points 2 h post-dose (1000 and 2200 h), we did observe significant differences in favour of DTFC at 1800 h (near the trough efficacy of brimonidine) and at 0200 (during the overnight period where brimonidine has previously been shown to have a weaker effect). The different findings when comparing a single time point study to a 24-h study highlight again the importance of measuring IOP over 24 h to properly assess the efficacy of glaucoma medications.30 Second, the Nixon study.38 was a parallel-arm design, whereas the current study had a crossover design. Parallel arm studies tend to require much larger patient numbers to achieve the same statistical power compared with crossover studies. The Nixon study showed a weakly significant superiority (P=0.04) in favour of BTFC at a single time point, whereas the current study showed a stronger statistical significance in favour of DTFC (P<0.001) over 24 h. Third, the Nixon paper required the pooling of data from two separate trials to achieve a weak statistical signficance, whereas the current 24-h study is reporting results from a single trial. Finally, all of the patients in this study were naive to treatment before the run-in with timolol 0.5% bid, whereas in the Nixon study, only 28% of the patients treated with BTFC, and 34% with DTFC were naive to treatment. Inclusion bias due to known poor response to one or more of the pharmacologic agents in BTFC or DTFC could have affected the findings.
In this crossover trial, there were no serious adverse events. Both DTFC and BTFC were generally well tolerated by the study patients. The ocular side effects were mild and similar for both fixed combinations, except for greater hyperaemia with BTFC, and greater stinging and bitter taste with DTFC.
Unfortunately, to date, there is limited published information evaluating the commonly used fixed combinations vs monotherapies, or unfixed therapy, beyond 2–3 time points in the daytime. It is important to assess the therapeutic equivalence of fixed combinations vs unfixed therapy, and between them throughout the 24-h period. This study compared for the first time the 24-h IOP efficacy with BTFC vs DTFC after a run-in period of 2 months with timolol. In a comparative efficacy study involving combined therapy with timolol, it is important to include a run-in period with timolol to exclude timolol non-responders, as well as those that achieved adequate IOP control on timolol monotherapy. The study's crossover design may have facilitated the determination of the real efficacy of the two fixed combinations. The results herein may explain for the first time why the 24-h IOP reduction provided by BTFC may be less than might be anticipated. Considering the previously documented 24-h efficacy of brimonidine and BTFC,17, 33, 35 it is conceivable that the reason for the reduced efficacy with BTFC may be the shorter duration of action of brimonidine, when instilled twice daily, whereas dorzolamide may have a longer duration of action and better night-time efficacy.20, 37
We observed the mean IOP, when six time-points over 24-h are averaged, to be significantly better with DTFC than with BTFC. However, the 0.7 mm Hg difference over 24 h is small, and the longer-term significance of this difference is uncertain. It must also be emphasised that our results apply to POAG with mild-to-moderate glaucoma and may not apply to other types of glaucoma. This study did not investigate the long-term 24-hour IOP-lowering efficacy of BTFC compared with DTFC. Further research should elucidate the long-term 24-h efficacy of these medications in glaucoma.
Dr Konstas is a consultant and has received research funding from Alcon, Allergan, MSD, and Pfizer. Dr Quaranta is a consultant at Alcon and MSD. Dr Yan is a consultant at Alcon, Allergan, and MSD. Dr Mikropoulos is a consultant at Alcon and Allergan. Dr Riva is a consultant at Allergan and MSD. Mr Barton is a consultant at Alcon, Aquesys, and MSD. Drs Gill and Haidich declare no conflict of interest. This study was not supported by any public or private body.
Footnotes
Ethical approval
The research protocol was approved by the Bioethics Committee of the Medical School of the Aristotle University of Thessaloniki and the study was registered at ClinicalTrials.gov (identifier NCT00972257). The study procedures were in accordance with the ethical standards of the Helsinki Declaration of 1975 (as revised in 1983).
References
- Konstas AGP, Mikropoulos D, Stewart WC.Fixed combination therapy in glaucomaIn: Shaarawy T, Hitchings R, Sherwood M, Crowston J (eds).Glaucoma Elsevier, USA; 2009565–75. [Google Scholar]
- Connor J, Rafter N, Rodgers A. Do fixed-dose combination pills or unit-of-use packaging improve adherence? A systematic review. Bull World Health Organ. 2004;82:935–939. [PMC free article] [PubMed] [Google Scholar]
- Bangalore S, Kamalakkannan G, Parkar S, Messerli FH. Fixed-dose combinations improve medication compliance: a meta-analysis. Am J Med. 2007;120:713–719. doi: 10.1016/j.amjmed.2006.08.033. [DOI] [PubMed] [Google Scholar]
- Petrilla AA, Benner JS, Battleman DS, Tierce JC, Hazard EH. Evidence-based interventions to improve patient compliance with antihypertensive and lipid-lowering medications. Int J Clin Pract. 2005;59:1441–1451. doi: 10.1111/j.1368-5031.2005.00704.x. [DOI] [PubMed] [Google Scholar]
- Olthoff CM, Schouten JSAG, Borne van der BW, Webers CA. Noncompliance with ocular hypotensive treatment in patients with glaucoma or ocular hypertension. Ophthalmology. 2005;112:953–961. doi: 10.1016/j.ophtha.2004.12.035. [DOI] [PubMed] [Google Scholar]
- Schwartz GF. Compliance and persistency in glaucoma follow-up treatment. Curr Opin Ophthalmol. 2005;16:114–121. doi: 10.1097/01.icu.0000156139.05323.26. [DOI] [PubMed] [Google Scholar]
- Sica DA. Rationale for fixed-dose combinations in the treatment of hypertension: the cycle repeats. Drugs. 2002;62:443–462. doi: 10.2165/00003495-200262030-00003. [DOI] [PubMed] [Google Scholar]
- Melikian C, White TJ, Vanderplas A, Dezii CM, Chang E. Adherence to oral antidiabetic therapy in a managed care organization: a comparison of monotherapy, combination therapy, and fixed-dose combination therapy. Clin Ther. 2002;24:460–467. doi: 10.1016/s0149-2918(02)85047-0. [DOI] [PubMed] [Google Scholar]
- Cox JA, Mollan SP, Bankart J, Robinson R. Efficacy of antiglaucoma fixed combination therapy vs unfixed components in reducing intraocular pressure: a systematic review. Br J Ophthalmol. 2008;92:729–734. doi: 10.1136/bjo.2008.139329. [DOI] [PubMed] [Google Scholar]
- Sleath B, Robin AL, Covert D, Byrd JE, Tudor G, Svarstad B. Patient-reported behavior and problems in using glaucoma medications. Ophthalmology. 2006;113:431–436. doi: 10.1016/j.ophtha.2005.10.034. [DOI] [PubMed] [Google Scholar]
- European Glaucoma Society Terminology and Guidelines for Glaucoma3rd ed.DOGMA S.r.l., Savona; 2008 [Google Scholar]
- Higginbotham EJ. Considerations in glaucoma therapy: fixed combinations vs their component medications. Clin Ophthalmol. 2010;4:1–9. [PMC free article] [PubMed] [Google Scholar]
- Razeghinejad MR, Sawchyn AK, Katz LJ. Fixed combinations of dorzolamide-timolol and brimonidine-timolol in the management of glaucoma. Expert Opin Pharmacother. 2010;11:959–968. doi: 10.1517/14656561003667540. [DOI] [PubMed] [Google Scholar]
- Tabet R, Stewart WC, Feldman R, Konstas AGP. A review of additivity to prostaglandin analogs: fixed and unfixed combinations. Surv Ophthalmol. 2008;53 (Suppl 1:S85–S92. doi: 10.1016/j.survophthal.2008.08.011. [DOI] [PubMed] [Google Scholar]
- Hutzelmann J, Owens S, Shedden A, Adamsons I, Vargas E. Comparison of the safety and efficacy of the fixed combination of dorzolamide/timolol and the concomitant administration of dorzolamide and timolol: a clinical equivalence study. Br J Ophthalmol. 1998;82:1249–1253. doi: 10.1136/bjo.82.11.1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goni FJ, Brimonidine/Timolol Fixed Combination Study Group 12-week study comparing the fixed combination of brimonidine and timolol with concomitant use of the individual components in patients with glaucoma and ocular hypertension. Eur J Ophthalmol. 2005;15:581–590. [PubMed] [Google Scholar]
- Konstas AGP, Katsimpris IE, Kaltsos K, Georgiadou I, Kordelou A, Nelson LA, et al. Twenty-four-hour efficacy of the brimonidine/timolol fixed combination vs therapy with the unfixed components. Eye. 2008;22:1391–1397. doi: 10.1038/sj.eye.6702906. [DOI] [PubMed] [Google Scholar]
- Craven ER, Walters TR, Williams R, Chou C, Cheetham JK, Schiffman R, et al. Brimonidine and timolol fixed-combination therapy vs monotherapy: a 3-month randomized trial in patients with glaucoma or ocular hypertension. J Ocul Pharmacol Ther. 2005;21:337–348. doi: 10.1089/jop.2005.21.337. [DOI] [PubMed] [Google Scholar]
- Sherwood MB, Craven ER, Chou C, DuBiner HB, Batoosingh AL, Schiffman RM, et al. Twice-daily 0.2% brimonidine-0.5% timolol fixed-combination therapy vs monotherapy with timolol or brimonidine in patients with glaucoma or ocular hypertension: a 12-month randomized trial. Arch Ophthalmol. 2006;124:1230–1238. doi: 10.1001/archopht.124.9.1230. [DOI] [PubMed] [Google Scholar]
- Stewart WC, Konstas AGP, Nelson LA, Kruft B. Meta-analysis of 24-hour intraocular pressure studies evaluating efficacy of glaucoma medicines. Ophthalmology. 2008;115:1117–1122. doi: 10.1016/j.ophtha.2007.10.004. [DOI] [PubMed] [Google Scholar]
- Boyle JE, Ghosh K, Gieser DK, Adamsons IA. A randomized trial comparing the dorzolamide-timolol combination given twice daily to monotherapy with timolol or dorzolamide. Ophthalmology. 1999;106:10–16. [PubMed] [Google Scholar]
- Fechtner RD, Airaksinen PJ, Getson AJ, Lines CR, Adamsons IA. Efficacy and tolerability of the dorzolamide 2%/timolol 0.5% combination (Cosopt) vs 0.005% (Xalatan) in the treatment of ocular hypertension or glaucoma: results from two randomized clinical trials. Acta Ophthalmol Scand. 2004;82:42–48. doi: 10.1046/j.1600-0420.2004.0205.x. [DOI] [PubMed] [Google Scholar]
- Shin DH, Feldman RM, Sheu WP. Efficacy and safety of the fixed combinations latanoprost/timolol vs dorzolamide/timolol in patients with elevated intraocular pressure. Ophthalmology. 2004;111:276–282. doi: 10.1016/j.ophtha.2003.05.019. [DOI] [PubMed] [Google Scholar]
- Miglior S, Grunden JW, Kwok K. Efficacy and safety of fixed combinations of latanoprost/timolol and dorzolamide/timolol in open-angle glaucoma or ocular hypertension. Eye. 2010;24:1234–1242. doi: 10.1038/eye.2009.307. [DOI] [PubMed] [Google Scholar]
- Konstas AGP, Papapanos P, Tersis I, Houliara D, Stewart WC. Twenty-four- hour diurnal curve comparison of commercially available latanoprost 0.005% vs timolol and dorzolamide fixed combination. Ophthalmology. 2003;110:1357–1360. doi: 10.1016/S0161-6420(03)00404-4. [DOI] [PubMed] [Google Scholar]
- Konstas AGP, Kozobolis VP, Tsironi S, Makridaki I, Efremova R, Stewart WC. Comparison of the 24-hour intraocular pressure-lowering effects of latanoprost and dorzolamide/timolol fixed combination after 2 and 6 months of treatment. Ophthalmology. 2008;115:99–103. doi: 10.1016/j.ophtha.2007.03.007. [DOI] [PubMed] [Google Scholar]
- Quaranta L, Miglior S, Floriani I, Pizzolante T, Konstas AGP. Effects of the timolol-dorzolamide fixed combination and latanoprost on circadian diastolic ocular perfusion pressure in glaucoma. Invest Ophthalmol Vis Sci. 2008;49:4226–4231. doi: 10.1167/iovs.08-1744. [DOI] [PubMed] [Google Scholar]
- Arcieri ES, Arcieri RS, Pereira AC, Andreo EG, Finotti IG, Sá Filho WF. Comparing the fixed combination brimonidine-timolol vs fixed combination dorzolamide-timolol in patients with elevated intraocular pressure. Curr Med Res Opin. 2007;23:683–689. doi: 10.1185/030079907x178694. [DOI] [PubMed] [Google Scholar]
- Hatanaka M, Grigera DE, Barbosa WL, Jordao M, Susanna R. An eight-week multicentric, randomized, interventional, open-label, Phase 4, parallel comparison of the efficacy and tolerability of the fixed combination of timolol maleate 0.5%/brimonidine tartrate 0.2% vs fixed combination of timolol maleate 0.5%/dorzolamide 2% in patients with elevated intraocular pressure. J Glaucoma. 2008;17:674–679. doi: 10.1097/IJG.0b013e318168f008. [DOI] [PubMed] [Google Scholar]
- Konstas AGP, Quaranta L, Miglior S, Mikropoulos DG, Bozkurt B.Twenty-four hour intraocular pressure monitoring in glaucoma Expert Rev Ophthalmol 2011(in press).
- Simes RJ. An improved Bonferroni procedure for multiple tests of significance. Biometrika. 1986;73:751–754. [Google Scholar]
- Siegel S. Nonparametric Statistics for the Behavioral Sciences. McGraw Hill: New York; 1956. pp. 63–67. [Google Scholar]
- Konstas AGP, Stewart WC, Topouzis F, Tersis I, Holmes KT, Stangos N. Brimonidine 0.2% given two or three times daily vs timolol maleate 0.5% in primary open-angle glaucoma. Am J Ophthalmol. 2001;131:729–733. doi: 10.1016/s0002-9394(01)00834-0. [DOI] [PubMed] [Google Scholar]
- Orzalesi N, Rossetti L, Bottoli A. The effect of latanoprost, brimonidine, and a fixed combination of timolol and dorzolamide on circadian intraocular pressure in patients with glaucoma or ocular hypertension. Arch Ophthalmol. 2003;121:453–457. doi: 10.1001/archopht.121.4.453. [DOI] [PubMed] [Google Scholar]
- Quaranta L, Gandolfo F, Turano R, Rovida F, Pizzolante D, Musig A, et al. Effects of topical hypotensive drugs on circadian IOP, blood pressure, and calculated diastolic ocular perfusion pressure in patients with glaucoma. Invest Ophthalmol Vis Sci. 2006;47:2917–2923. doi: 10.1167/iovs.05-1253. [DOI] [PubMed] [Google Scholar]
- Liu JHK, Medeiros FA, Slight JR, Weinreb RN. Diurnal and nocturnal effects of brimonidine monotherapy on intraocular pressure. Ophthalmology. 2010;117:2075–2079. doi: 10.1016/j.ophtha.2010.03.026. [DOI] [PubMed] [Google Scholar]
- Orzalesi N, Rossetti L, Invernizzi T, Bottoli A, Autelitano A. Effect of timolol, latanoprost, and dorzolamide on circadian IOP in glaucoma or ocular hypertension. Invest Ophthalmol Vis Sci. 2000;41:2566–2573. [PubMed] [Google Scholar]
- Nixon DR, Yan DB, Chartrand JP, Piemontesi RL, Simonyi S, Hollander DA. Three-month, randomized, parallel-group comparison of brimonidine-timolol vs dorzolamide-timolol fixed combination therapy. Curr Med Res Opin. 2009;25:1645–1653. doi: 10.1185/03007990902994041. [DOI] [PubMed] [Google Scholar]
- Yuksel N, Karbas L, Altintas O, Yildrim Y, Caglar Y. A comparison of the short-term hypotensive effects and side effects of unilateral brimonidine and apraclonidine in patients with elevated intraocular pressure. Ophthalmologica. 2002;216:45–49. doi: 10.1159/000048296. [DOI] [PubMed] [Google Scholar]