Abstract
Purpose
To test the hypothesis that posterior approach ptosis surgery, with or without blepharoplasty, can improve the cosmetic appearance of the eyelid.
Methods
In a retrospective, observational, consecutive case cohort study, 261 patients who had posterior approach upper eyelid ptosis surgery with or without concurrent blepharoplasty performed by one surgeon, between 1997 and 2009, were reviewed. Patients were included if they had symmetric eyelid position within 1.5 mm at 3 months after surgery. Outcome measures were subjective grading of eyelid margin contour, millimeters of tarsal platform show (TPS), and millimeters of eyebrow fat span (BFS). Paired preoperative and postoperative standardized photographs were viewed in masked fashion by three experts.
Results
One hundred and forty patients (55 men, 85 women, mean age 70 years, range 20–93) who underwent 233 posterior approach procedures for correction of upper eyelid ptosis had postoperative eyelid symmetry within 1.5 mm. Concurrent blepharoplasty was performed in 67 cases. Eyelid contour scores were significantly improved following surgery (P=.009). Ptosis surgery, without blepharoplasty, decreased the TPS, from 6.1±2.5 mm to 4.8±2.0 mm (P<.001). Patients who underwent concurrent blepharoplasty had a statistically insignificant increase of TPS from 4.0±3.5 mm to 4.3±3.6 mm, had a decrease of BFS from 20.8±6.3 mm to 17.7±6.4 mm (P=.001), and showed similar BFS symmetry postoperatively, compared to patients who had ptosis surgery only.
Conclusions
Posterior approach surgery alone was often successful in controlling TPS: it shortened the TPS. Blepharoplasty combined with posterior approach ptosis surgery tended to lengthen the TPS and shorten the BFS.
INTRODUCTION
Blepharoptosis surgery is designed to elevate the upper eyelid margin, and it has both functional and cosmetic implications. From a functional standpoint, the goal of surgery is to elevate the eyelid margin above the pupillary axis for improvement in superior visual field. From a cosmetic standpoint, the goals of surgery are to achieve a smooth curvature of the eyelid margin (normal contour), symmetry in eyelid margin height, and symmetry in the soft tissues of the eyelid and eyebrow, particularly the amount of tarsal platform show (TPS).
In reported series of blepharoptosis surgery, the commonly reported outcome measure is the position of the eyelid margin (margin reflex distance, or MRD1) relative to the opposite eyelid. Investigators vary in their definition of a successful result, ranging from 0.5 mm to 1.5 mm.1–14 Most investigators have considered eyelid margin position within 1 mm of the desired height (or within 1 mm of symmetry) to represent a successful result. The measurement technique is presumed to be from direct clinical measurements with a ruler, which may have some inherent inaccuracy compared to photographic measurements.
The success of blepharoptosis surgery in elevating the eyelid margin for improvement in vision is good. However, controlling the symmetry, contour, and TPS can be more difficult. Multiple factors come into play, including eyelid and eyebrow compensatory mechanisms, characteristics of the tarsus, volume and contour of the eyebrow fat pad, volume of orbital fat, skin elasticity and thickness, and bony symmetry. For optimal results, surgical decision making should incorporate these multiple factors. However, these factors can be difficult to predict (eg, postoperative resetting of compensatory mechanisms) or difficult to treat (eg, skin quality, volume deflation, bony asymmetry).
Some previous studies have addressed cosmetic outcomes in ptosis, such as eyelid crease position1,8,15–19 or eyelid contour change,20–22 but we are not aware of any studies that analyze the cosmetic outcome of ptosis surgery in detail.
Beyond the basic measurement of eyelid margin position, cosmetic outcomes of blepharoptosis surgery can be further characterized by measurement of eyelid curvature, tarsal show, and eyebrow fat component. The goal of this study was to evaluate the change in these parameters following ptosis surgery, with and without blepharoplasty. We hypothesized that posterior approach ptosis surgery, with or without blepharoplasty, can improve the cosmetic appearance of the eyelid as measured by eyelid contour score, TPS, and eyebrow fat span (BFS). To reduce the impact of eyelid margin position asymmetry, we selected only those cases demonstrating postoperative symmetry of eyelid margin position within 1.5 mm.
METHODS
Approval was received by the University of California Los Angeles Institutional Review Board to perform a retrospective study.
Utilizing cases contained in Oculoplasty Registry, accessed with an electronic medical record (McCann Medical Matrix, St Louis, Missouri), medical records were retrospectively reviewed for consecutive cases of posterior approach conjunctivomullerectomy ptosis surgery. The procedures were performed by a single surgeon, with or without associated blepharoplasty procedures, between 1997 and 2009. The data retrieved included age, gender, type of surgery, previous surgical history, visual acuity, lagophthalmos, and documented surgical complications. For all patients, preoperative and postoperative digital photographs were reviewed. Photographs were taken in primary gaze, with the plane of the face parallel to the plane of the camera back. Lighting was accomplished with a slave-driven studio softbox flash unit. The camera was an Olympus C-5060 with telephoto macro lens set at maximum zoom, 110mm equivalent, at f=11.
Two hundred and sixty-one patients who underwent posterior approach ptosis surgery were identified. Of this group, patients were included in the study if they had adequate 3-month follow-up including photographs, symmetric eyelid position within 1.5 mm, and MRD1 more than 3.5 mm at 3 months after surgery. Some patients have been included in a previous report.20 Patients were excluded if they had previous full-thickness resection or frontalis ptosis surgery, if they had previous eyelid retraction surgery, or if contralateral eyelid retraction correction surgery was performed. After these exclusions, 140 patients who demonstrated acceptable eyelid position and symmetry with at least 3 months follow-up remained.
The amount of tissue resection was planned based on the desired amount of eyelid elevation. A 4-mm resection for each 1 mm of desired elevation was performed. In bilateral cases, surgery was designed to maximize symmetry: if preoperative asymmetry was noted, based on asymmetric ptosis or asymmetric eyebrow compensation, then greater resection was performed on the more ptotic side.
Concurrent blepharoplasty was performed in cases in which eyelid fullness was judged to be excessive or predicted to be excessive following ptosis surgery. As appropriate, based on preoperative assessment, blepharoplasty was designed asymmetrically to address preoperative asymmetry. The tissue excision for blepharoplasty was designed based on the desired amount of TPS. The debulking of skin (and variably of muscle and fat in selected cases) was graded, based on the anticipated eyelid margin and eyebrow position following ptosis surgery. In combined cases the skin or skin-muscle flap was excised, and fat sculpted as indicated, before everting the eyelid to perform the posterior ptosis surgery.
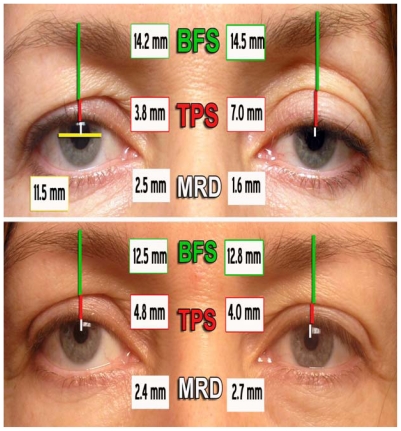
Eyelid measurements were taken from digital photographs, using ImageJ 1.43 (National Institutes of Health, rsbweb.nih.gov/ij/download). The corneal diameter was standardized to 11.5 mm in order to convert pixel measurements to millimeters. In addition to measuring MRD1, we developed two measurements in order to characterize the 3-dimensional relationships of the upper eyelid–eyebrow complex. TPS was measured between the eyelid margin and the fold of skin over the eyelid crease. BFS was calculated as the distance from the skin fold to the top of the eyebrow hairs (Figure 1).
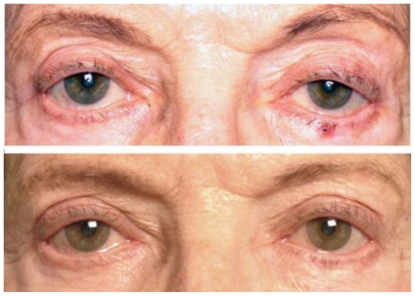
FIGURE 1.
Top, Demonstration of measurement of brow fat span (BFS), tarsal platform show (TPS), and margin reflex distance (MRD1) on standardized photographs (corneal diameter set at 11.5 mm for scale). Bottom, In the same patient, following left ptosis surgery and bilateral asymmetric blepharoplasty, TPS symmetry has improved and BFS has shortened.
Eyelid contour was evaluated using subjective assessment of photographs. Paired preoperative and postoperative standardized photographs were viewed by three experts, who were masked to the specific procedure performed. Interobserver variability was calculated. Observers graded eyelid contour on a subjective scale: 0=poor, 1=fair, and 2=good (Figure 2). Reevaluation of 20 slides confirmed reproducibility of the initial assessment of the eyelid contour scores. Intraobserver reliability was calculated as Cronbach’s alpha of 0.57, and correlation between observer scores was significant with the Pearson correlation test.
FIGURE 2.
Example key utilized for eyelid contour grading. Triangular peaking, medial or lateral displacement of the high point, or flattening of the eyelid contour were assessed in standardized photographs and utilized to grade the eyelid contour as good (2), fair (1), or poor (0).
SURGICAL TECHNIQUE
Local anesthesia was accomplished with 2% lidocaine with epinephrine 1:100,000. The upper eyelid was infiltrated with 2 to 3 mL of anesthetic, including 0.5 mL injected subconjunctivally just superior to the tarsal border.
The patient was then prepared in sterile fashion, allowing time for the epinephrine to take effect and for the fluid volume of anesthetic to dissipate. If concurrent blepharoplasty was to be performed, the skin was marked and the skin muscle flap resected at this time.
Attention was then turned to the posterior ptosis surgery. The eyelid was everted over a Desmarres retractor. The medial and lateral one-third junction of the tarsus was marked at the superior border, and then the conjunctiva was grasped medially and laterally, at a measured point above the tarsus of one-half the desired total resection. The two grasped points were lifted and pulled apart, to avoid clotheslining. As the Desmarres retractor was removed, a Putterman ptosis clamp (Karl Ilg Instruments Inc, St Charles, Illinois) was placed and locked over the grasped conjunctival tissue, flush with the upper tarsal border. A 6-0 mild chromic gut suture was passed from the skin to the conjunctiva and sutured across the base of the clamp (0.5 mm from the clamp edge) in serpentine fashion, three to four passes, then externalized back to the skin. The same suture was then brought back through skin into the conjunctiva and passed back across the base of the clamp, taking bites between the previous suture passes, before externalizing the suture to the skin adjacent to the original starting place. This resulted in two pairs of externalized sutures, which were then tied medially and laterally on the skin surface with adequate tension to eliminate any slack in the suture. The tissues in the clamp, consisting of conjunctiva, Müller’s muscle, and some levator fibers, were excised using a scalpel blade beveled slightly into the clamp to accomplish a flush excision. Bleeding was controlled with pressure. If concurrent blepharoplasty had been performed, the skin incision was closed.
STATISTICAL ANALYSIS
A Wilcoxon signed rank test was used to compare cosmetic eyelid contour scores in all groups of patients (posterior approach with or without blepharoplasty). We assumed that the interval in each point in the 0 to 2 scale is equivalent (that is, change from 0 to 1 is equal to change from 1 to 2). If these assumptions are not met, then the P values are approximate. Statistical analysis was performed with Microsoft Excel (Microsoft Corporation, Redmond, Washington) and SPSS (SPSS, Inc, Chicago, Illinois) programs. Paired samples t tests to evaluate preoperative and postoperative MRD1, TPS, and BFS were performed. A t test was used to evaluate TPS asymmetry and BFS asymmetry by calculating delta values.
RESULTS
Of 140 patients, 55 were men and 85 women; their mean age was 70.3±14.3 years, ranging from 20 to 93 years. Nintey-three patients had ptosis surgery on both sides, and 47 had unilateral surgery. Concurrent blepharoplasty was performed in 67 cases. The mean preoperative MRD1 was 1.7±1.1 mm in the group with ptosis surgery alone and 1.9±1.7 mm in the group with concurrent blepharoplasty; these values were not significantly different (P>.05).
EYELID CONTOUR SCORE
One of the chief advantages of posterior approach conjunctivomullerectomy surgery is that it has minimal tendency to worsen the eyelid contour. In fact, we noted a significant improvement in eyelid contour score following ptosis surgery (P<.009).
TARSAL PLATFORM SHOW
The amount of TPS decreased following surgery in the isolated ptosis surgery group and was unchanged following surgery in the concurrent blepharoplasty group. Ptosis surgery alone, without blepharoplasty, decreased the TPS from 6.1±2.5 mm preoperatively to 4.8±2.0 mm postoperatively (P<.001). Patients who underwent concurrent blepharoplasty manifested no decrease in TPS: 4.0±3.5 mm preoperatively, compared to 4.3±3.6 mm postoperatively (P>.05) (Table).
TABLE.
EYELID MEASUREMENTS OF 166 ISOLATED PTOSIS AND 67 COMBINED BLEPHAROPLASTY CASES, BEFORE AND AFTER SURGERY
| CHARACTERISTIC | PREOPERATIVE | POSTOPERATIVE | p VALUE |
|---|---|---|---|
| TPS | |||
| Ptosis alone (mm±SD) | 6.1±2.5 | 4.8±2.0 | <.001 |
| With bleph (mm±SD) | 4.0±3.5 | 4.3±3.6 | >.05 |
| BFS | |||
| Ptosis alone (mm±SD) | 17.1±5.1 | 16.3±4.4 | <.001 |
| With bleph (mm±SD) | 20.8±6.3 | 17.7±6.4 | <.001 |
| TPS asymmetry* | |||
| Ptosis alone (mm±SD) | 1.5±1.4 | 0.9±0.8 | <.01 |
| With bleph (mm±SD) | 1.4±1.2 | 1.1±0.8 | <.01 |
| BFS asymmetry* | |||
| Ptosis alone (mm±SD) | 2.2±1.7 | 1.9±1.6 | <.01 |
| With bleph (mm±SD) | 1.5±1.1 | 1.4±0.9 | <.01 |
BFS, eyebrow fat span; TPS, tarsal platform show.
Measured as the delta of longer minus the shorter side.
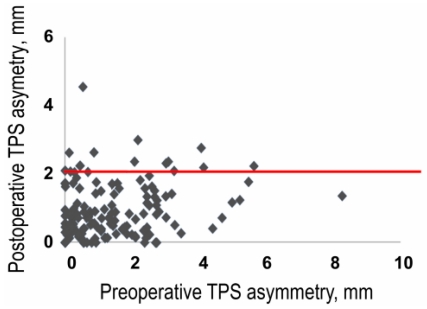
To evaluate preoperative and postoperative symmetry, we calculated TPS asymmetry as the delta, or smaller subtracted from larger TPS. Preoperative TPS asymmetry measured 1.5±1.4 mm, and it decreased to 0.9±0.8 mm postoperatively (P<.01). The asymmetry of TPS improved more in the ptosis surgery alone group than in the concurrent blepharoplasty group, from 1.4±1.2 mm to 1.1±0.8 mm (Table). One hundred eighteen patients (84%) had postoperative TPS asymmetry less than 2 mm (Figure 3). Although TPS symmetry increased on average, Figure 3 clearly demonstrates the unpredictable nature of blepharoplasty and ptosis surgery in controlling the TPS; some patients were even more asymmetric after surgery than before surgery.
FIGURE 3.
Scatterplot showing worsened postoperative tarsal platform show (TPS) symmetry in some patients; most patients had postoperative asymmetry less than 2 mm (horizontal red line).
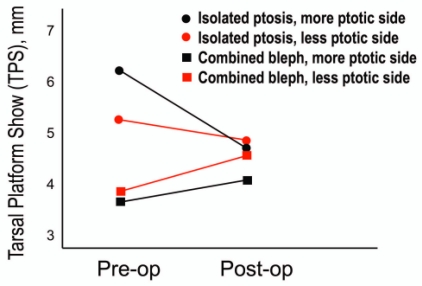
Figure 4 illustrates the change in TPS differentially in the more ptotic and less ptotic eyelid. One of the hallmarks of levator dehiscence is elevation of the eyelid crease, and as expected, we found that the preoperative TPS was longer on the more ptotic eyelid. Isolated ptosis surgery was successful in decreasing the asymmetry of TPS. In the concurrent blepharoplasty group, the preoperative TPS was shorter (as we would expect in this group of patients with eyelid fullness as an indication for blepharoplasty). As we would anticipate, blepharoplasty surgery caused lengthening of the TPS. The concurrent blepharoplasty group of patients showed minimal TPS asymmetry before surgery and remained symmetric after surgery. Although not statistically significant, there may be a tendency to undercorrect the long TPS characterizing the more ptotic eyelid.
FIGURE 4.
Change of bilateral tarsal platform show (TPS) following posterior approach ptosis surgery. In the isolated ptosis surgery group (circles), TPS decreased postoperatively. TPS was longer preoperatively in the more ptotic eyelid, and the asymmetry (vertical distance between the circles) decreased postoperatively. In the combined blepharoplasty patients (squares), TPS increased postoperatively and there was a trend toward less postoperative symmetry of TPS.
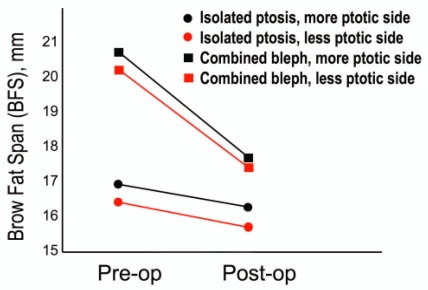
BROW FAT SPAN
As predicted, patients who underwent concurrent blepharoplasty had more significant decrease of BFS, from 20.8±6.3 mm preoperatively to 17.7±6.4 mm postoperatively (P<.001), than those who had ptosis surgery alone, from 17.1±5.1 mm preoperatively to 16.3±4.4 mm postoperatively (P<.001) (Table).
To evaluate preoperative and postoperative symmetry, we calculated BFS asymmetry as the delta, or smaller subtracted from larger BFS. BFS asymmetry decreased more in the ptosis surgery alone group, 2.2±1.7 mm to 1.9±1.6 mm postoperatively, than in the concurrent blepharoplasty group, 1.5±1.1 mm to 1.4±0.9 mm. Figure 5 demonstrates the BFS change and also BFS asymmetry comparing the more ptotic and less ptotic eyelid. Preoperatively more than postoperatively, the BFS was longer in the more ptotic eyelid (presumably related to eyebrow compensation and frontalis drive).
FIGURE 5.
Change of eyebrow fat span (BFS) following posterior approach ptosis surgery. In the combined blepharoplasty group (squares), BFS decreased postoperatively. The BFS in the isolated ptosis surgery group (circles) started lower and showed a statistically insignificant decrease. In all groups, there was a trend for longer BFS on the side of the more ptotic eyelid, before and after surgery.
DISCUSSION
The outcomes of blepharoptosis surgery have been defined primarily by change in the eyelid margin position relative to the cornea, with success defined as eyelid position or symmetry within 0.5,1–3 1.0,5–14 or 1.5 mm.4 Certainly, the primary goal of blepharoptosis surgery is to elevate a ptotic eyelid, so that measuring the change in eyelid position is a logical and appropriate outcome measure. Furthermore, eyelid symmetry is an important aspect of facial appearance, and measuring the symmetry of the eyelid margin following ptosis surgery provides a measure of the cosmetic result.
However, assessing only the eyelid margin position fails to address other important determinants of the cosmetic result of blepharoptosis surgery. The eyelid margin position is only one aspect of the cosmetic appearance of the eyelid. To achieve optimal cosmetic results of ptosis surgery, it is important to control—as much is possible—not only eyelid margin position and symmetry, but also eyelid contour, eyelid crease (TPS), and eyebrow position.
Most cases of acquired ptosis relate to stretching or dehiscence of the levator aponeurosis, in the setting of normal levator function. When levator function is adequate, ptosis surgery is designed to shorten the elongated levator aponeurosis, restoring normal length relative to the levator muscle and the tarsus. The levator aponeurosis can be accessed anteriorly through an eyelid crease incision,3,6,14,19,23–28 nonincisionally,29 or through a posterior approach.30–32 The conjunctivomullerectomy procedure described by Putterman4,33,34 and modified by others35–40 is a simplified posterior approach ptosis surgery that predictably shortens the levator aponeurosis.37
We prefer posterior approach conjunctivomullerectomy ptosis surgery in most cases, because the predictability for eyelid margin position and contour is superior, in our experience, compared to the anterior levator approach.20 Eyelid margin contour (curvature) is affected by the characteristics and stability of the tarsus. For example, in older patients, in chronic inflammation, in congenital variations such as floppy eyelid syndrome, and in postoperative cases in which the tarsus has been removed, the tarsus may be unstable and prone to develop peaking or other contour abnormalities. This is particularly true with anterior ptosis surgery and is the reason that we prefer the posterior approach in most cases. As long as the contour is acceptable before surgery, it will almost always be acceptable after surgery, when the posterior approach is used. In the current study, eyelid contour scores increased slightly in both the isolated ptosis and the combined blepharoplasty groups.
Tarsal platform show is a complicated relationship. It is primarily affected by the combination of eyelid margin position (in other words, long or short eyelid), combined with the fullness of the septal fat pannus, subcutaneous fat, and eyebrow fat pad that form the anterior contour of the upper eyelid soft tissue. Eyebrow compensation is very important here: as the eyebrow goes up and down, it controls the position of these soft tissues.41,42 When the eyebrow is up, for example, because of compensatory drive triggered by eyelid margin ptosis, the soft tissues are elevated off the tarsal platform and the visible length of the tarsal platform increases. In contrast, when the eyebrow comes down, for example, due to release of compensatory drive following ptosis surgery, the tarsal platform will become shorter. The amount and symmetry of TPS are critical determinants of eyelid appearance.
In fact, symmetry of TPS may be more important than symmetry of MRD1 in the perception of facial appearance (unpublished data, Robert Goldberg MD, et al, oral presentation, American Society of Ophthalmic Plastic and Reconstructive Surgery Annual Scientific Meeting, Chicago Illinois, October 13, 2010). To optimize the cosmetic result of ptosis surgery, we must optimally predict and control the postoperative TPS.
A number of investigators have measured relationships of the eyebrow, eyelid, and eyelid margin position in order to establish population norms or to assess symmetry. 43–46 Recently, Flynn and colleagues21 utilized computer measurements to characterize the eyelid margin contour, although in their study the goal was to assess medial or lateral shift of the peak, but not flattening, triangular peaking, or other cosmetic disturbances of normal eyelid margin curvature. We are currently studying application of computer modeled quadrant curves to characterize and assess normal and abnormal eyelid margin curvature (unpublished data, Ronald Mancini, MD, et al, poster presentation, American Society of Ophthalmic Plastic Reconstructive Surgery Annual Scientific Meeting, Chicago, Illinois, October 13, 2010).
Although TPS has not been measured in previous reported series of blepharoptosis surgery, it is commonly recognized that as a component of ptosis surgery, the eyelid crease should be controlled. Discussing crease considerations in blepharoptosis surgery, Baylis and Cies15 noted the following: “Production of an eyelid fold at the time of an initial blepharoptosis procedure should be a primary goal. Lack of a distinct symmetrical upper eyelid fold constituted a cosmetic blemish and necessitated revision.” Putterman and Urist17 reviewed options for surgical manipulation of the crease and the overlying fold of skin. Shore and associates16 noted that “revision of the eyelid crease and fold can be accomplished by trimming more skin, fixating the skin at a lower or higher position on the aponeurosis, or placing full-thickness eyelid sutures.” Kim and associates18 discussed controlling the eyelid crease in the Oriental vs Occidental eyelid configuration.
The concept of fixating the skin through a cutaneous incision, in order to form the eyelid crease, has been suggested as a reason to choose anterior approach blepharoptosis surgery, in order to be able to control the crease by attaching skin to deep structures.16,19,47–50 However, the surgically created eyelid crease is not the sole determinant of aesthetic eyelid contours. The 3-dimensional appearance of the eyelid is determined not only by the crease, but by the tissues that fill the upper eyelid space, including eyebrow fat, subcutaneous fat, orbital fat, skin, and orbicularis muscle. Surgical procedures designed to control or change the eyelid appearance cannot rely on the eyelid crease alone, and conversely, TPS can be manipulated without any eyelid crease incision, by elevating or lowering the eyelid margin. Controlling the upper orbital volume and TPS potentially requires manipulation of the eyebrow fat, orbital fat, eyelid margin position, and skin. The interaction of blepharoptosis and cosmetic eyelid appearance is important in that regard: elevating the eyelid margin position shortens the eyelid directly and also can reset eyebrow compensation.41,51 Operating on the eyelid crease alone may be neither necessary nor adequate to modulate the eyelid volume and complex compensatory mechanisms that control TPS.
To optimize the cosmetic result of ptosis surgery, preoperative planning should take into account factors that could impact the symmetry of the eyelid margin position and symmetry of the TPS. This might include assessment of eyebrow position and compensation and bony asymmetry. TPS and BFS can be helpful in characterizing these relationships.
If the tarsal platform is longer on the side of the more ptotic eyelid, and particularly if there is eyebrow compensation (eyebrow elevated), ptosis surgery alone can improve symmetry of tarsal show. This improvement is a result of the shortening of eyelid, and also relaxation of eyebrow compensation, which allows the eyebrow to descend and recruits skin, muscle, and subbrow fat to the eyelid space, decreasing TPS (Figure 6). Unfortunately, the degree of postoperative eyebrow descent, like the degree of contralateral eyelid descent, is somewhat unpredictable, even with preoperative neosynephrine testing to predict the degree of eyebrow and contralateral eyelid descent.52–55
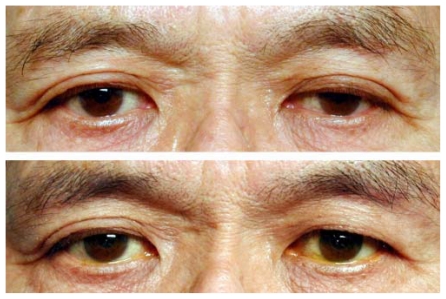
FIGURE 6.
Top, Bilateral upper eyelid ptosis, left more than right, with asymmetric long tarsal platform show (TPS) preoperatively. Bottom, Following isolated ptosis surgery, left more than right. The eyelid is shortened and eyebrow compensation relaxed, resulting in shortening and improved symmetry of TPS, without any skin surgery or surgical crease formation.
In contrast, if the patient starts out with asymmetric or unilateral ptosis, but symmetric TPS, then ptosis surgery alone will likely worsen TPS symmetry. This might decrease the cosmetic success of the surgery even if the eyelid margin position ends up satisfactory and symmetric. If the eyebrow is compensating on the more ptotic side, the postoperative asymmetry will be amplified, as the eyebrow relaxation after surgery will cause even more exaggerated asymmetric shortening of the TPS (Figure 7).
FIGURE 7.
Top, Left upper eyelid ptosis with symmetric tarsal platform show (TPS) preoperatively. The eyebrow is compensating on left side. Bottom, Following isolated ptosis surgery on the left, the eyelid is shortened, eyebrow compensation relaxes, and the TPS decreases, resulting in TPS asymmetry.
Normally, the TPS is longer on the more ptotic side. A TPS that is symmetric or even shorter on the more ptotic side should raise the specter of bony asymmetry, soft tissue asymmetry, or ocular dominance on the opposite side. Bony asymmetry is another important aspect of ptosis surgery planning. Most patients have a small side and a large side of their face.56,57 The small side is characterized by crowding and by a shorter tarsal platform, and in our experience the smaller side is often the more ptotic side. When the preoperative tarsal platform is shorter on the ptotic side, this is an important observation that suggests either lack of compensatory drive (neurologic or ocular dominance) or bony and soft tissue asymmetry. In either case, the tarsal platform will not improve following ptosis surgery alone. To improve postoperative symmetry in these cases, ptosis surgery might be better combined with asymmetric blepharoplasty surgery to decrease soft tissue fullness and expose more of the TPS, and if there is bony asymmetry with a crowded eyebrow, forehead lift might also be considered in order to increase the BFS (Figure 8).
FIGURE 8.
Top, Left upper eyelid ptosis with symmetric tarsal platform show (TPS) preoperatively. Bottom, Following left ptosis surgery, combined with bilateral asymmetric blepharoplasty (left more than right). Slight residual left upper eyelid ptosis may be driving subtle eyebrow compensation, and TPS symmetry is maintained postoperatively.
We measured the TPS and BFS in the central eyelid. This was chosen to simplify the analysis, but a richer interpretation of the cosmetic result of ptosis surgery would include the actual contour of the TPS and BFS. For example, in Figure 8, the central TPS measures symmetric, but there is clearly asymmetry of the nasal third of the TPS. Modern computer imaging software is powerful in detecting and characterizing these types of contours, and many aspects of the complex contours of the periorbital area will be amenable to objective analysis in future studies. Of course, the mathematical definitions of beauty will always fall short in tackling a complex topic with so many subjective, cultural, and emotional overlays. That should not discourage us from striving to generate more rigorous analyses of the cosmetic outcomes of our periorbital surgeries.
The improvement in TPS symmetry in our patients suggests that we were able to control this parameter in some patients. However, many patients were asymmetric after surgery, occasionally more asymmetric than before surgery. Postoperative TPS asymmetry was more pronounced in the concurrent blepharoplasty group, compared to ptosis surgery alone. Clearly there was ascertainment bias in patients who were selected for ptosis surgery, compared to patients who were treated with ptosis surgery combined with blepharoplasty. This limits the conclusions that can be made comparing the groups. However, the decision to add blepharoplasty to the ptosis surgery was based on the surgeon’s determination that the cosmetic result would be better if the eyelid tissues were debulked. The determination of performing symmetric or asymmetric ptosis surgery, and symmetric or asymmetric blepharoplasty surgery, was based on preoperative evaluation, designed to maximize postoperative symmetry. Even if the difference between the groups reflects more the increased complexity of patients chosen for concurrent blepharoplasty than it does the inherent ability of ptosis surgery or blepharoplasty to control eyelid symmetry, it does suggest that even in experienced hands, it is not always possible to achieve the goal of symmetric TPS.
CONCLUSION
Eyelid margin position and symmetry (MRD1) is an obvious characteristic to describe the result of blepharoptosis surgery, but it is not the only important outcome measurement. The cosmetic outcome of ptosis surgery is also affected by the eyelid margin contour and by the characteristics and symmetry of TPS and BFS. By shortening the eyelid, and inducing relaxation of eyebrow compensatory drive, posterior approach surgery alone can control eyelid contours and TPS. Depending on factors such as bony asymmetry, eyebrow position and compensation, eyebrow fat pad shape and size, and eyelid tissue fullness, cosmetic blepharoplasty and/or eyebrow repositioning can be incorporated in an effort to additionally control the TPS and BFS symmetry. We found that isolated ptosis surgery resulted in shortening of the TPS and slight contraction of BFS, whereas ptosis surgery combined with blepharoplasty resulted in unchanged TPS and decreased BFS. Although TPS symmetry improved statistically in this series following ptosis surgery with or without blepharoplasty, some patients were asymmetric after surgery: we were not always able to predict and control the effect of these multiple factors on final surgical outcome.
ACKNOWLEDGMENTS
Funding/Support: None.
Financial Disclosures: None.
Author Contributions: Design and conduct of the study (R.A.G., H.L.); Collection, management, analysis (R.A.G., H.L.), and interpretation (R.A.G.) of the data; Preparation, review, and approval of manuscript (R.A.G.).
Conformity With Author Information: The University of California Los Angeles Institutional Review Board approved this study (Oculoplastic Registry IRB# 01-12-048. Last renewed and approved 07/25/2011).
REFERENCES
- 1.Johnson CC. Blepharoptosis. Arch Ophthalmol. 1962;67(11):48–54. doi: 10.1001/archopht.1962.00960020020005. [DOI] [PubMed] [Google Scholar]
- 2.Lake S, Mohammad-Ali FH, Khooshabeh R. Open sky Muller’s muscle-conjunctiva resection for ptosis surgery. Eye. 2003;17(9):1008–1012. doi: 10.1038/sj.eye.6700623. [DOI] [PubMed] [Google Scholar]
- 3.Frueh BR, Musch DC, McDonald H. Efficacy and efficiency of a new involutional ptosis correction procedure compared to a traditional aponeurotic approach. Trans Am Ophthalmol Soc. 2004;102:199–206. discussion 206–207. [PMC free article] [PubMed] [Google Scholar]
- 4.Putterman AM, Fett DR. Müller’s muscle in the treatment of upper eyelid ptosis: a ten-year study. Ophthalmic Surg. 1986;17(6):354–360. [PubMed] [Google Scholar]
- 5.Cates CA, Tyers AG. Outcomes of anterior levator resection in congenital blepharoptosis. Eye. 2001;15(Pt 6):770–773. doi: 10.1038/eye.2001.247. [DOI] [PubMed] [Google Scholar]
- 6.Doxanas MT. Simplified aponeurotic ptosis surgery. Ophthalmic Surg. 1992;23(8):512–515. [PubMed] [Google Scholar]
- 7.Liu D. Ptosis repair by single suture aponeurotic tuck. Surgical technique and long-term results. Ophthalmology. 1993;100(2):251–259. doi: 10.1016/s0161-6420(93)31662-3. [DOI] [PubMed] [Google Scholar]
- 8.Berlin AJ, Vestal KP. Levator aponeurosis surgery. A retrospective review. Ophthalmology. 1989;96(7):1033–1036. discussion 1037. [PubMed] [Google Scholar]
- 9.Anderson RL, Dixon RS. Aponeurotic ptosis surgery. Arch Ophthalmol. 1979;97(6):1123. doi: 10.1001/archopht.1979.01020010577015. [DOI] [PubMed] [Google Scholar]
- 10.McCulley TJ, Kersten RC, Kulwin DR, Feuer WJ. Outcome and influencing factors of external levator palpebrae superioris aponeurosis advancement for blepharoptosis. Ophthal Plast Reconstr Surg. 2003;19(5):388–393. doi: 10.1097/01.IOP.0000087071.78407.9A. [DOI] [PubMed] [Google Scholar]
- 11.Dortzbach RK, Kronish JW. Early revision in the office for adults after unsatisfactory blepharoptosis correction. Am J Ophthalmol. 1993;115(1):68–75. doi: 10.1016/s0002-9394(14)73527-5. [DOI] [PubMed] [Google Scholar]
- 12.Older J. Levator aponeurosis surgery for the correction of acquired ptosis: analysis of 113 procedures. Ophthalmology. 1983;90:1056–1059. doi: 10.1016/s0161-6420(83)80047-5. [DOI] [PubMed] [Google Scholar]
- 13.Bartley GB, Lowry JC, Hodge DO. Results of levator-advancement blepharoptosis repair using a standard protocol: effect of epinephrine-induced eyelid position change. Trans Am Ophthalmol Soc. 1996;94:165–73. discussion 174–177. [PMC free article] [PubMed] [Google Scholar]
- 14.Lucarelli MJ, Lemke BN. Small incision external levator repair: technique and early results. Am J Ophthalmol. 1999;127(6):637–644. doi: 10.1016/s0002-9394(99)00064-1. [DOI] [PubMed] [Google Scholar]
- 15.Baylis HI, Cies WA. Surgical revision of the upper eyelid fold. Am J Ophthalmol. 1975;80(6):1019–1023. doi: 10.1016/0002-9394(75)90331-1. [DOI] [PubMed] [Google Scholar]
- 16.Shore JW, Bergin DJ, Garrett SN. Results of blepharoptosis surgery with early postoperative adjustment. Ophthalmology. 1990;97(11):1502–1511. doi: 10.1016/s0161-6420(90)32384-9. [DOI] [PubMed] [Google Scholar]
- 17.Putterman AM, Urist MJ. Reconstruction of the upper eyelid crease and fold. Arch Ophthalmol. 1976;94(11):1941–1954. doi: 10.1001/archopht.1976.03910040647013. [DOI] [PubMed] [Google Scholar]
- 18.Kim MK, Rathbun JE, Aguilar GL, Seiff SR. Ptosis surgery in the Asian eyelid. Ophthal Plast Reconstr Surg. 1989;5(2):118–126. doi: 10.1097/00002341-198906000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Hornblass A. Correction of eyelid ptosis. Plast Reconstr Surg. 1988;81(6):988. doi: 10.1097/00006534-198806000-00043. [DOI] [PubMed] [Google Scholar]
- 20.Ben Simon GJ, Lee S, Schwarcz RM, McCann JD, Goldberg RA. External levator advancement versus Müller’s muscle-conjunctival resection for correction of upper eyelid involutional ptosis. Am J Ophthalmol. 2005;140(3):426–432. doi: 10.1016/j.ajo.2005.03.033. [DOI] [PubMed] [Google Scholar]
- 21.Flynn TH, Rose GE, Shah-Desai SD. Digital image analysis to characterize the upper lid marginal peak after levator aponeurosis repair. Ophthal Plast Reconstr Surg. 2011;27:12–14. doi: 10.1097/IOP.0b013e3181eea2e3. [DOI] [PubMed] [Google Scholar]
- 22.Baylis H, Axelrod R, Rosen N. Full thickness eyelid resection for the treatment of undercorrected blepharoptosis and eyelid contour defects. Adv Ophthal Plast Reconstr Surg. 1982;1:205–212. [Google Scholar]
- 23.Blaskovicz L. Treatment of ptosis. The formation of a fold in the eyelid and resection of the levator and tarsus. Arch Ophthalmol. 1929;58:672–680. [Google Scholar]
- 24.Berke R. A simplified Blasovics operation for blepharoptosis; results in ninety-one operations. Arch Ophthalmol. 1952;48:460–495. doi: 10.1001/archopht.1952.00920010469011. [DOI] [PubMed] [Google Scholar]
- 25.Jones LT, Quickert MH, Wobig JL. The cure of ptosis by aponeurotic repair. Arch Ophthalmol. 1975;93(8):629–634. doi: 10.1001/archopht.1975.01010020601008. [DOI] [PubMed] [Google Scholar]
- 26.Fox SA. Levator tucking. Ann Ophthalmol. 1979;11:453–456. [PubMed] [Google Scholar]
- 27.Harris W, Dortzbach R. Levator tuck: a simplified blepharoptosis procedure. Ann Ophthalmol. 1975:873–878. [PubMed] [Google Scholar]
- 28.Wilkins RB, Patipa M. The recognition of acquired ptosis in patients considered for upper-eyelid blepharoplasty. Plast Reconstruct Surg. 1982;70(4):431–434. doi: 10.1097/00006534-198210000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Shimizu Y, Nagasao T, Asou T. A new non-incisional correction method for blepharoptosis. J Plast Reconstr Aesthet Surg. 2010;63(12):2004–2012. doi: 10.1016/j.bjps.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 30.Collin JR. A ptosis repair of aponeurotic defects by the posterior approach. Br J Ophthalmol. 1979;63(8):586–590. doi: 10.1136/bjo.63.8.586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ichinose A, Tahara S. Transconjunctival levator aponeurotic repair without resection of Müller’s muscle. Aesthetic Plast Surg. 2007;31(3):279–284. doi: 10.1007/s00266-006-0202-9. [DOI] [PubMed] [Google Scholar]
- 32.Patel V, Salam A, Malhotra R. Posterior approach white line advancement ptosis repair: the evolving posterior approach to ptosis surgery. Br J Ophthalmol. 2010;94(11):1513–1518. doi: 10.1136/bjo.2009.172353. [DOI] [PubMed] [Google Scholar]
- 33.Putterman AM. A clamp for strengthening Müller’s muscle in the treatment of ptosis. Modification, theory, and clamp for the Fasanella-Servat ptosis operation. Arch Ophthalmol. 1972;87(6):665–667. doi: 10.1001/archopht.1972.01000020667010. [DOI] [PubMed] [Google Scholar]
- 34.Putterman AM, Urist MJ. Müller muscle-conjunctiva resection. Technique for treatment of blepharoptosis. Arch Ophthalmol. 1975;93(8):619–623. doi: 10.1001/archopht.1975.01010020595007. [DOI] [PubMed] [Google Scholar]
- 35.Weinstein GS, Buerger GF., Jr Modification of the Müller’s muscle-conjunctival resection operation for blepharoptosis. Am J Ophthalmol. 1982;93(5):647–651. doi: 10.1016/s0002-9394(14)77383-0. [DOI] [PubMed] [Google Scholar]
- 36.Perry JD, Kadakia A, Foster JA. A new algorithm for ptosis repair using conjunctival Müllerectomy with or without tarsectomy. Ophthalmic Plast Reconstr Surg. 2002;18(6):426–429. doi: 10.1097/00002341-200211000-00007. [DOI] [PubMed] [Google Scholar]
- 37.Dresner SC. Further modifications of the Müller’s muscle-conjunctival resection procedure for blepharoptosis. Ophthalmic Plast Reconstr Surg. 1991;7(2):114–122. doi: 10.1097/00002341-199106000-00005. [DOI] [PubMed] [Google Scholar]
- 38.Ben Simon GJ, Lee S, Schwarcz RM, McCann JD, Goldberg RA. Muller’s muscle-conjunctival resection for correction of upper eyelid ptosis: relationship between phenylephrine testing and the amount of tissue resected with final eyelid position. Arch Facial Plast Surg. 2007;9(6):413–417. doi: 10.1001/archfaci.9.6.413. [DOI] [PubMed] [Google Scholar]
- 39.Michels KS, Vagefi MR, Steele E, et al. Müller muscle-conjunctiva resection to correct ptosis in high-risk patients. Ophthal Plast Reconstr Surg. 2007;23(5):363–366. doi: 10.1097/IOP.0b013e31814a6415. [DOI] [PubMed] [Google Scholar]
- 40.Mercandetti M, Putterman AM, Cohen ME, Mirante JP, Cohen AJ. Internal levator advancement by Müller’s muscle-conjunctival resection: technique and review. Arch Facial Plast Surg. 2001;3(2):104–110. doi: 10.1001/archfaci.3.2.104. [DOI] [PubMed] [Google Scholar]
- 41.Fagien S. Eyebrow analysis after blepharoplasty in patients with brow ptosis. Ophthal Plast Reconstr Surg. 1992;8(3):210–214. doi: 10.1097/00002341-199209000-00009. [DOI] [PubMed] [Google Scholar]
- 42.Putterman AM, Fagien S. Putterman’s Cosmetic Oculoplastic Surgery. 4th ed. cha 11 New York: Saunders Elsevier; 2008. Müller’s muscle-conjunctival resection-ptosis procedure combined with upper blepharoplasty. [Google Scholar]
- 43.Cartwright MJ, Kurumety UR, Nelson CC, Frueh BR, Musch DC. Measurements of upper eyelid and eyebrow dimensions in healthy white individuals. AJO. 1994;117(2):231–234. doi: 10.1016/s0002-9394(14)73081-8. [DOI] [PubMed] [Google Scholar]
- 44.Coombes AG, Sethi CS, Kirkpatrick WN, et al. A standardized digital photography system with computerized eyelid measurement analysis. Plast Reconstr Surg. 2007;120(3):647–656. doi: 10.1097/01.prs.0000270315.53241.10. [DOI] [PubMed] [Google Scholar]
- 45.Price KM, Gupta PK, Woodward JA, Stinnett SS, Murchison AP. Eyebrow and eyelid dimensions: an anthropometric analysis of African Americans and Caucasians. Plast Reconstr Surg. 2009;124(2):615–623. doi: 10.1097/PRS.0b013e3181addc98. [DOI] [PubMed] [Google Scholar]
- 46.Cole EA, Winn BJ, Putterman AM. Measurement of eyebrow position from inferior corneal limbus to brow: a new technique. Ophthal Plast Reconstr Surg. 2010;26(6):443–447. doi: 10.1097/IOP.0b013e3181d3dd22. [DOI] [PubMed] [Google Scholar]
- 47.Leone CR. Management of the blepharoplasty patient with ptosis. Ophthalmic Surg. 1988;19(7):515–522. [PubMed] [Google Scholar]
- 48.Carraway JH, Vincent MP. Levator advancement technique for eyelid ptosis. Plast Reconstr Surg. 1986;77(3):394–403. doi: 10.1097/00006534-198603000-00008. [DOI] [PubMed] [Google Scholar]
- 49.Crum AV, Bernardino CR. Preventing and managing post-surgical ptosis. Rev Ophthalmol. 2010;17(10):116–119. [Google Scholar]
- 50.Older JJ. Ptosis repair and blepharoplasty in the adult. Ophthalmic Surg. 1995;26(4):304–308. [PubMed] [Google Scholar]
- 51.Teske SA, Kersten RC, Devoto MH, Kulwin DR. Hering’s law and eyebrow position. Ophthal Plast Reconstr Surg. 1998;14(2):105–106. doi: 10.1097/00002341-199803000-00006. [DOI] [PubMed] [Google Scholar]
- 52.Erb MH, Kersten RC, Yip C-C, et al. Effect of unilateral blepharoptosis repair on contralateral eyelid position. Ophthal Plast Reconstr Surg. 2004;20(6):418–422. doi: 10.1097/01.iop.0000143714.10858.d4. [DOI] [PubMed] [Google Scholar]
- 53.Bodian M. Lip droop following contralateral ptosis repair. Arch Ophthalmol. 1982;100(7):1122–1124. doi: 10.1001/archopht.1982.01030040100018. [DOI] [PubMed] [Google Scholar]
- 54.Wladis EJ, Gausas RE. Transient descent of the contralateral eyelid in unilateral ptosis surgery. Ophthal Plast Reconstr Surg. 2008;24(5):348–351. doi: 10.1097/IOP.0b013e3181831f40. [DOI] [PubMed] [Google Scholar]
- 55.Lyon DB, Gonnering RS, Dortzbach RK, Lemke BN. Unilateral ptosis and eye dominance. Ophthal Plast Reconstr Surg. 1993;9(4):237. doi: 10.1097/00002341-199312000-00002. [DOI] [PubMed] [Google Scholar]
- 56.Ing E, Safarpour A, Ing T, Ing S. Ocular adnexal asymmetry in models: a magazine photograph analysis. Can J Ophthalmol. 2006;41(2):175–182. doi: 10.1139/I06-005. [DOI] [PubMed] [Google Scholar]
- 57.Katsumata A, Fujishita M, Maeda M, Ariji Y, Ariji E, Langhis RP. 3D-CT evaluation of facial asymmetry. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99(2):212–220. doi: 10.1016/j.tripleo.2004.06.072. [DOI] [PubMed] [Google Scholar]