Abstract
Objective
The purpose of this case study is to describe the clinical presentation of a patient with a chief complaint of low back and leg pain with no prior diagnosis of lung cancer.
Clinical Features
A 48-year-old man with a history of back pain presented to a chiropractic office with a complaint of low back and left leg pain.
Intervention and Outcome
Abnormal examination and radiographic findings were discovered. The patient was immediately referred to the pulmonologist for co-management. Through the use of advanced imaging and biopsy, stage 4 lung cancer was diagnosed.
Conclusion
Low back pain recurrence in an established patient should constitute a reevaluation of the problem. The cause cannot be assumed to be musculoskeletal in origin even though this may have been the case with the initial complaint. Metastatic disease should be considered with any type of recurrent low back pain.
Key indexing terms: Carcinoma, Non–small cell lung, Radiculopathy, Chiropractic, Metastasis
Introduction
For the United States in 2006, 106 374 men and 90 080 women were diagnosed with lung cancer.1 In 2009, lung cancer was estimated to cause 28% of all cancer-related deaths in the United States.2 Cigarette smoking is the leading cause of lung cancer, but 15% of patients with the disease have never smoked.3,4
There are 2 categories of lung cancer: small cell (oat cell) carcinoma and non–small cell carcinoma. Thirteen percent to 15% of all lung cancers worldwide are small cell carcinomas.5 This type of cancer is aggressive, is usually central in location, and is associated with mediastinal involvement, early metastasis, and paraneoplastic syndromes.6
This case study describes the management of an established patient returning from an absence of care with a complaint of low back pain. Despite a similar presentation in this patient's history, the recognition of a potentially different etiology led to the clinical decision to perform a reexamination, a step frequently omitted in the course of chiropractic treatment. Small cell lung carcinoma with metastasis was eventually diagnosed as the result of this examination.
Case report
A 48-year-old white man presented to a chiropractic office with signs and symptoms of low back pain and pain in the lower left leg. This patient had been under intermittent care for neck and back pain for over 13 years. Each episode of neck or back pain was treated with conservative care and responded favorably. Upon walking into the room on this occasion, a noticeable decrease in weight was noted; and the patient appeared anxious and fatigued. Upon being asked about the weight loss, the patient said that he had been “inspired by The Biggest Loser,” was watching his diet, and began exercising 8 months ago. When asked about fatigue and anxiousness, he said that he was a “little tired” and “didn't like doctors.”
History revealed a complaint of left lower extremity weakness, numbness, and pain that began approximately 1 month prior. He could not recall any trauma or precipitating event that could have initiated the symptoms. The pain was described as “dull and aching” and localized in nature. At rest, the patient rated his functional impairment as 3/10 and, with activity, as 7/10. The symptoms were reported to be constant throughout the day. He had difficulty walking and numbness in the whole left leg. Upon having the patient walk, a slappage gait was observed on the left side. Right and left patellar and Achilles reflex had a finding of clonus and a positive Babinski reflex on the left, which would indicate an upper motor neuron lesion. Upper extremity reflexes were tested and found to have no abnormalities. Motor tests revealed a 0-1 motor test on the left foot with dorsiflexion supination. Severe left side hyperesthesia, severely diminished vibratory sensation, severely diminished 2-point discrimination, and diminished sharp-dull sensation were present on left, lower medial ankle and foot. Left cheek hypoesthesia, left hand hypoesthesia, and diminished left-sided grip strength were also found. Upon further observation, the patient was wheezing and sweating. When asked about how he was feeling, he said that he was trying to quit smoking and he would get this way after not having one for a while. His fingers and toes were observed to have clubbing. When asked how long he had smoked, he said 1 to 2 packs a day for the last 22 years, which meant that he started smoking at age 26 years. Vitals were abnormal with elevated blood pressure, respiration, and pulse. These are specifically listed along with patient demographics in Table 1.
Table 1.
Demographics and vitals as measured on the initial visit in the chiropractic office
| Vital signs | Patient findings |
|---|---|
| Height | 175 cm |
| Weight | 155 lb |
| BMI | 22.9 |
| Blood pressure, right arm, sitting | 160/105 mm Hg |
| Blood pressure, left arm, sitting | 160/103 mm Hg |
| Pulse | 112 beats/min |
| Respirations | 28 breaths/min |
Respiratory examination revealed increased respiratory effort, moderate right side, percussive dullness posteromedially and posterolaterally. Palpation revealed severely decreased tactile fremitus on the right lower lateral and lower medial chest wall and moderately decreased breath sounds on the right posterolateral and posteromedial chest wall. No lymphadenopathy was noted. A mildly abnormal finger to nose test result was also present. Radiographic images were ordered and displayed evidence of a lung mass (Fig 1). The patient was informed of the findings and was immediately referred for a computed tomography (CT) of the lungs and to see a pulmonary specialist. The CT confirmed a right upper lobe mass (Figs 2 and 3). The patient was subsequently under the care of the pulmonary specialist and oncologist. Magnetic resonance imaging of the head and whole-body positron emission tomographic scans were ordered along with a biopsy taken by the pulmonary specialist.
Fig 1.

Lateral chest radiograph showing upper lobe mass.
Fig 2.

An axial CT of the thorax revealing an anteriorly situated right lung mass.
Fig 3.
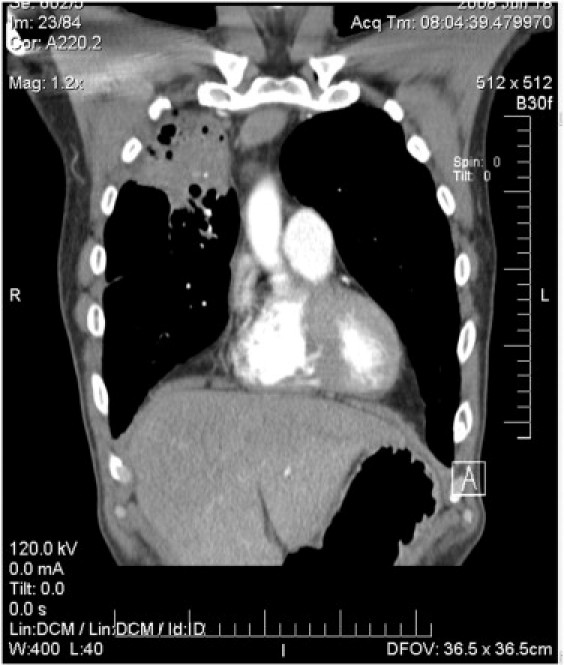
Coronal CT with upper right lobe mass.
The final diagnosis was non–small cell carcinoma with liver metastasis. An interesting finding in this case is that there was no evidence of neurological metastasis, which could explain the findings of the upper motor lesions found during the examination. The patient received chemotherapy and radiation therapy for the carcinoma. He sought chiropractic care for palliative relief during the treatment of his cancer. The chiropractor was also used to explain the medical tests and what they meant, because “he trusted” the chiropractor. The patient died within 1 year of diagnosis.
Discussion
This case is an example of the “red flags” that are sometimes not acknowledged, especially on the patient that one has had a working relationship with and presents with a recurrence of the same symptoms. The “red flags” in this patient were considerable weight loss in a short time, sweating, and fatigue; yet the patient stated he was attempting to lose weight. The anxious feeling around doctors can and do cause abnormal findings (white coat syndrome). The patient came in with slappage gait indicative of a lower motor neuron lesion; yet upon examination, all upper motor neuron lesions were found. However, an intracranial and cervical, thoracic, and lumbar spine magnetic resonance revealed no central nervous system lesions.
A full-body positron emission tomographic scan revealed hypermetabolic activity in the vertebral bodies of the spine, yet no metastasis was confirmed on CT. Vertebral metastasis may grow to compress the spinal cord in which neurological symptoms such as pain, numbness, or weakness may be reported especially in the lower extremities.6 A series of disk protrusions were identified in the cervical and lumbar spine but did not correlate the symptoms to possible adjacent nerve root radiculopathy. Interestingly, all the neurological findings were left-sided, contralateral to the right upper lobe lung malignancy.
From 2003 to 2007, the median age at diagnosis for cancer of the lung and bronchus was 71 years of age7; approximately 8.8% were diagnosed in those between the ages of 45 and 54 years.8 A 5-year relative survival rate for distant metastasis at the time of diagnosis is 3.5%. 8 In this case, the patient was 48 years of age but reported smoking 2 packs per day for 22 years. With a low 5-year survival rate for stage 4 non–small cell carcinoma, death within 1 year of diagnosis was not abnormal. He was treated with radiation, chemotherapy, and antiemetics. This was within the usual treatment regimen for stage 4 non–small cell carcinoma: cisplatin-based chemotherapy and surgical resection if there is a solitary metastatic lesion and a resectable primary tumor.6 Non–small cell carcinoma consists of 3 main subtypes: adenocarcinoma, squamous, and large cell. Each histological subtype has similar treatment regimens but has different clinical presentations and characteristics. The types and percentages of lung cancer are shown in Table 2. Adenocarcinoma usually arises from peripheral mucosal glands, whereas squamous cell carcinoma is usually a proximal bronchus morphological change in the type of epithelium; and large cell usually appears as a large mass in the periphery with atypical cells containing focal necrosis.9
Table 2.
Types of lung cancer with percentage of cancer cases
| Cancer type | % Cases |
|---|---|
| Non–small cell | 75-80 |
| • Adenocarcinoma | 30-35 |
| • Squamous cell carcinoma | 30-35 |
| • Large cell carcinoma | 10-20 |
| Small cell carcinoma | 20-25 |
Lung cancers usually present with symptoms resulting from the primary tumor or metastatic disease, or as the effects of unusual hormone production with symptoms depending on the location of the disease. In stage 4 non–small cell carcinoma of the right upper lobe as found in this case after biopsy, the clinical presentation due to the primary tumor might include signs of respiratory distress, superior vena cava obstruction, recurrent laryngeal nerve palsy, and phrenic nerve palsy.8 The 4 most common sites of metastasis from a primary lung malignancy are the bone, brain, liver, and adrenal glands.10 In this case, neurologic findings indicative of an upper motor neuron lesion were present; but no evidence of neurological metastasis was discovered.
Conclusion
This case shares the findings that presented to a chiropractic practice and encourages clinicians specializing in musculoskeletal disease to consider visceral sources of pathology in returning cases especially if findings are not consistent with musculoskeletal findings. Low back pain recurrence in an established patient should constitute a reevaluation of the problem. The cause cannot be assumed to be musculoskeletal in origin even though this may have been the case with the initial complaint. Metastatic disease should be considered with any type of recurrent low back pain.
Funding sources and potential conflicts of interest
No funding sources or conflicts of interest were reported for this study.
References
- 1.United States cancer statistics: 1999-2006 incidence and mortality web-based report. 2010. http://www.cdc.gov/uscs Available at: Accessed April 23, 2010.
- 2.What are the key statistics about lung cancer? 2010. http://www.cancer.org/acs/groups/content/@nho/documents/document/500809webpdf.pdf Available from: Accessed April 28, 2010.
- 3.Subramanian J., Govindan R. Lung cancer in never smokers: a review. J Clin Oncol. 2007;25(5):561–570. doi: 10.1200/JCO.2006.06.8015. [DOI] [PubMed] [Google Scholar]
- 4.Hong W.K., Tsao A.S. Merck Sharp and Dohme Corporation; Whitehouse Station (NJ): 2009. Merck manual. [Google Scholar]
- 5.Garcia M., Jernal A., Ward E.M., Center M.M., Hao Y., Siegel R.I. Global cancer facts and figures, 2007. American Cancer Society; Atlanta: 2007. p. 13. [Google Scholar]
- 6.Rost G.I., Bevilacqua G., Bidoli P., Portalone L., Santo A., Genestreti G. Small cell lung cancer. Ann Oncol. 2006;17(2) doi: 10.1093/annonc/mdj910. [DOI] [PubMed] [Google Scholar]
- 7.Altekruse S.F., Kosary C.L., Krapcho M., Nayman N., Aminou R., Waldron W. SEER cancer statistics review: 1975-2007. 2010. http://seer.cancer.gov/csr/1975_2007 Available from: Accessed April 21, 2010.
- 8.Johnston M.R. Curable lung cancer: how to find it and treat it. Postgrad Med. 1997;101(3):155–165. doi: 10.3810/pgm.1997.03.178. [DOI] [PubMed] [Google Scholar]
- 9.Collins L.G., Haines C., Perkel R., Enck R.E. Lung cancer: diagnosis and management. Am Fam Physician. 2007;75(1):56–63. [PubMed] [Google Scholar]
- 10.Huq S., Maghfoor I., Perry M. Lung cancer non small cell. eMedicine. Oncology. 2010 [Google Scholar]


