Abstract
Objectives
The purpose of this study was to retrospectively report the results of patients who completed an exercise-based chiropractic program and its potential to alter the natural progression of adult scoliosis at 24 months after the clinic portion of treatment was concluded.
Methods
A retrospective chart review was conducted at 2 spine clinics in Michigan, USA. Each clinic uses the same chiropractic rehabilitation program to treat patients with adult scoliosis. Multidimensional patient outcomes included radiographic, respiratory, disability, and pain parameters. Outcomes were measured at baseline, at end of active treatment, and at long-term follow-up.
Results
A total of 28 patients fit the inclusion criteria for the study. The average beginning primary Cobb angle was 44° ± 6°. Patients received the same chiropractic rehabilitation program for approximately 6 months. At the end of active treatment, improvements were recorded in Cobb angle, pain scores, spirometry, and disability rating. All radiographic findings were maintained at 24-month follow-up.
Conclusion
This report is among the first to demonstrate sustained radiographic, self-rated, and physiologic benefits after treatment ceased. After completion of a multimodal chiropractic rehabilitation treatment, a retrospective cohort of 28 adult scoliosis patients reported improvements in pain, Cobb angle, and disability immediately following the conclusion of treatment and 24 months later.
Key indexing terms: Chiropractic, Rehabilitation, Scoliosis
Introduction
Approximately 68% of scoliotic curvatures greater than 30° at skeletal maturity tend to progress at a linear rate, regardless of the type of scoliosis curvature pattern.1-3 Asymmetrical gravitational loading on the spine and disk elements leads to asymmetric degeneration.4,5 This cyclic process ultimately causes the adult scoliosis to progress and negatively affect quality of life later.2 Therefore, as other authors have already discussed,6 the only way to improve the asymmetrical degenerative environment is to promote symmetry of the global spine, thus removing asymmetrical gravitational loading.
Exercise-based therapies for scoliosis have not been widely published. A recent review by Everett and Patel6 found only 10 articles in the Medline, PubMed, and CINAHL databases concerning exercise therapy for adult scoliosis. Adding chiropractic AND manipulation to their searches yielded only another 5 studies. Romano and Negrini7 also performed a review to evaluate the effectiveness of manual therapy for scoliosis treatment. Their searches produced only 3 relevant studies, only one of which included an adult population. The purpose of this article is to describe the collection of outcomes following the completion of a multimodal chiropractic rehabilitation program that was ultimately home based. This approach has been reported previously.8,9 However, only atypical cases and/or short-term outcomes were presented. This article outlines the results obtained in a retrospective review of 28 patients who were prescribed the same chiropractic rehabilitation program and presented for a 24-month long-term follow-up. All patients whose data were included completed a Health Insurance Portability and Accountability Act–compliant informed consent to use their nonidentifying information.
Methods
Adult patients with scoliosis who presented to 1 of 2 private medical clinics within the same 2-year period were selected for this study. We only chose patients from these same 2 clinics so that the outcomes measures used would remain homogenous throughout the sample population. Patient files were consecutively selected if they met the following criteria: (1) patients were at least 18 years of age and a Risser 5, (2) patients had a negative history for spinal surgery, (3) the patient completed his/her prescribed treatment program, (4) patients who had returned to the clinic for a 24-month long-term follow-up, (5) patients who gave written informed consent to use their data, and (6) patients who exhibited Cobb angles of at least 30°. Patients were specifically excluded if they had a history of neuromuscular disease or bony anomalies such as a hemivertebra or if they did not present for long-term follow-up. Patients who did not complete all of the outcome assessments were also excluded.
Outcomes measures recorded in these patient charts included spirometry measurements using a Buhl spirometer, a Quadruple Numeric Pain Scale (QNPS) questionnaire, a Functional Rating Index (FRI), and Cobb angle scoliosis measurements. Because of postural collapse in the spine resulting from gravitational loading, all before-and-after radiographs were taken at approximately the same time of day to avoid any normal diurnal changes,10,11 which can range from 5° to 20°. The author removed all identifying information on the radiographs and gave them to another chiropractor for analysis to help avoid examiner bias. Before-and-after films were also shuffled before analysis. The radiographic studies were obtained on 14″×17″ film using a reliable, repeatable method of patient positioning12 to maintain consistency and reduce mensuration error. Radiographs were taken no less than 24 hours after the patient's last treatment, whether at home or at the clinic. Patients were called 2 days before their follow-ups and instructed to not perform their home care the day before.
The treatment approach provided to the sample population is centered around the concept of Active Reflex Correction in 3 Dimensions (ARC3D). More specifically, these therapies are collectively used to promote global coronal and sagittal balance, as well as to restore the normal sagittal spinal curves. The primary modality in this treatment is the application of an external ambulatory weighting system developed by Pettibon (patent 6,788,968; Pettibon Weighting System, Pettibon System, Chehalis, WA). It is an external head, torso, and pelvis weighting system designed to cause active reflex adaptations in response to asymmetrically applied external loads. An illustration of this weighting system is shown in Fig 1. These predetermined external loads alter the centers of mass of the head, torso, and pelvis in specific directions to cause neuromuscular recruitment responses that ultimately result in positive global adaptations in the sagittal and coronal dimensions. This weighting system process has been previously tested and described.13,14 All patients in this study were prescribed their own sets of this weighting system for both in-office treatment as well as home use. Each patient came to the author's office for a specified treatment period and then was released from care and followed up 1 to 4 times annually, depending upon the length of care, the severity of the primary scoliosis, and the amount of curve correction obtained. Outcomes were typically taken at 12-month intervals on an ongoing basis. Radiographic examinations were performed annually if the patient consented. For purposes of this retrospective chart review, only patients who received radiographic examination at 24 months were included in the review. Fig 1 provides an illustration of the modalities used by patients in this study. All patients performed these procedures; however, each procedure was customized to the patient depending upon the patient's strength and curvature type/location.
Fig 1.
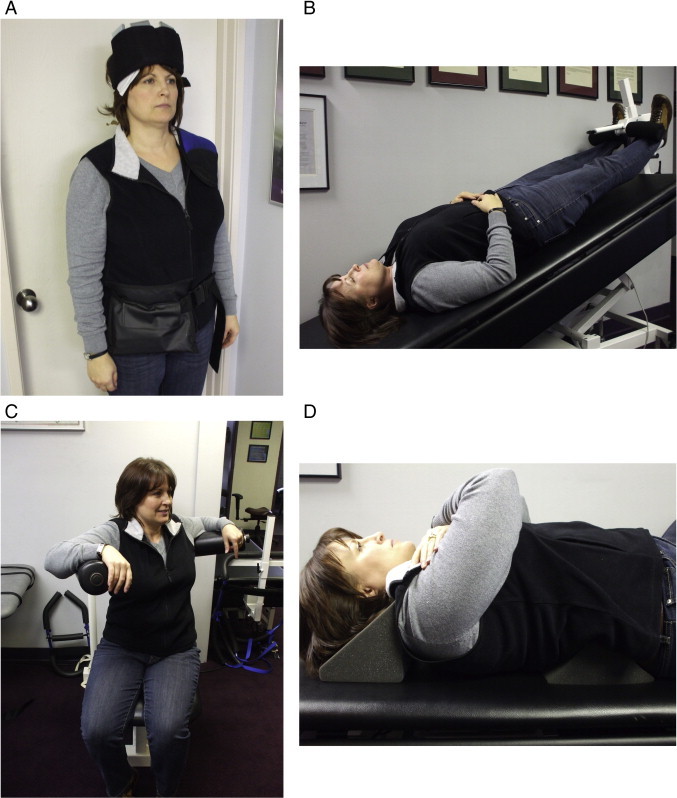
The various clinical and home modalities used for each patient. From top left (clockwise): external weighting system (A), axial distraction (B), rotary torso exercises (C), and spinal molding on foam fulcrum blocks (D).
Results
The average beginning primary Cobb angle was 44° ± 6°. Table 1 shows all of the outcomes of the entire sample. Patients ranged in age between 18 and 54 years old with a median age of 34 years, with 26 women and 2 men. The age range of this cohort of patients is comparable to that included in a 2007 study by Marty-Poumarat et al,1 where the average age of their patients was 37 years (range, 17-60) in a total of 51 patients (female, 48; male, 3). Patients in the present cohort received the same chiropractic rehabilitation program for approximately 6 months. Each radiograph was subcategorized into 1 of 4 groups based on curvature type: thoracic, lumbar, thoracolumbar, and double major. The thoracic group comprised 12 patients, the lumbar group had 5 patients, 5 patients were in the thoracolumbar group, and 6 were in the double major category. Fig 2 illustrates a sample radiographic series throughout the treatment process.
Table 1.
Outcomes of the entire sample
| Curve type | Cobb1 | Cobb2 | Cobb3 | QNPS1 | QNPS2 | QNPS3 | FRI1 | FRI2 | FRI3 | Buhl1 | Buhl2 | Buhl3 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Thoracic | ||||||||||||
| Mean | 44.0 | 32.5 | 33.9 | 52.6 | 32.7 | 26.7 | 25.1 | 11.8 | 8.8 | 2479.2 | 2654.2 | 2700.0 |
| N | 12.0 | 12.0 | 12.0 | 12.0 | 12.0 | 12.0 | 12.0 | 12.0 | 12.0 | 12.0 | 12.0 | 12.0 |
| SD | 5.6 | 7.5 | 7.2 | 14.1 | 14.9 | 12.3 | 6.8 | 5.5 | 6.0 | 477.9 | 414.8 | 405.6 |
| Lumbar | ||||||||||||
| Mean | 44.6 | 34.0 | 35.0 | 59.4 | 36.8 | 26.0 | 26.8 | 12.6 | 8.2 | 2450.0 | 2610.0 | 2570.0 |
| N | 5.0 | 5.0 | 5.0 | 5.0 | 5.0 | 5.0 | 5.0 | 5.0 | 5.0 | 5.0 | 5.0 | 5.0 |
| SD | 2.5 | 10.3 | 11.8 | 16.5 | 19.4 | 10.9 | 6.5 | 6.9 | 5.2 | 885.3 | 709.2 | 601.7 |
| Thoracolumbar | ||||||||||||
| Mean | 39.2 | 22.0 | 22.0 | 61.2 | 26.2 | 28.2 | 21.6 | 12.0 | 2.8 | 2260.0 | 2660.0 | 2810.0 |
| N | 5.0 | 5.0 | 5.0 | 5.0 | 5.0 | 5.0 | 5.0 | 5.0 | 5.0 | 5.0 | 5.0 | 5.0 |
| SD | 7.7 | 8.6 | 6.8 | 20.4 | 9.1 | 5.2 | 7.9 | 7.2 | 3.0 | 258.4 | 373.2 | 427.8 |
| Double major | ||||||||||||
| Mean | 46.7 | 44.8 | 45.0 | 46.0 | 34.5 | 22.2 | 20.3 | 11.0 | 6.8 | 2416.7 | 2408.3 | 2425.0 |
| N | 6.0 | 6.0 | 6.0 | 6.0 | 6.0 | 6.0 | 6.0 | 6.0 | 6.0 | 6.0 | 6.0 | 6.0 |
| SD | 6.3 | 8.5 | 8.6 | 18.2 | 16.5 | 6.3 | 5.2 | 2.8 | 6.9 | 606.4 | 566.1 | 461.2 |
| Total | ||||||||||||
| Mean | 43.8 | 33.5 | 34.4 | 53.9 | 32.6 | 25.9 | 23.8 | 11.8 | 7.2 | 2421.4 | 2594.6 | 2637.5 |
| N | 28.0 | 28.0 | 28.0 | 28.0 | 28.0 | 28.0 | 28.0 | 28.0 | 28.0 | 28.0 | 28.0 | 28.0 |
| SD | 6.0 | 10.8 | 10.8 | 16.6 | 14.9 | 9.7 | 6.7 | 5.4 | 5.8 | 541.8 | 484.5 | 453.1 |
Cobb1, initial Cobb angle; Cobb2, after 6 months of active treatment; Cobb3, long-term follow-up; QNPS1, initial QNPS score; QNPS2, after 6 months of active treatment; QNPS3, long-term follow-up; FRI1, initial FRI disability score; FRI2, after 6 months of active treatment; FRI3, long-term follow-up; Buhl1, initial spirometry measurement; Buhl2, after 6 months of active treatment; Buhl3, long-term follow-up.
Fig 2.
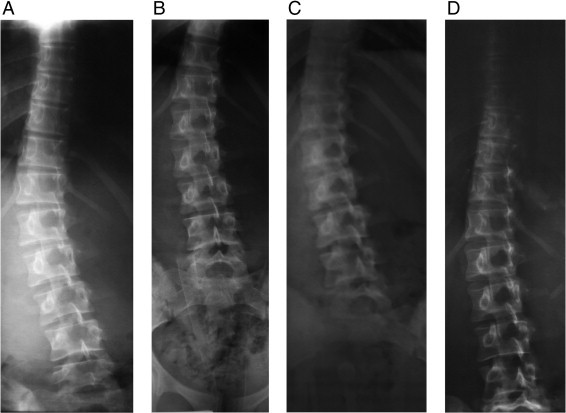
A sample time line of a patient's progress during treatment. From left, the initial radiograph (A), stress radiograph (taken while wearing external weighting system to evaluate potential) (B), 6 months (C), and 24 months (D).
Looking at the Cobb angle measurements, a mean of 10° ± 9° of reduction was observed across all curvature groups. The QNPS scores improved by 39% after 6 months and further improved by another 21% at 24-month follow-up. Disability scores on the FRI improve from a baseline of 60% disability to 30% disability at 6 months and 18% disability at 24 months. Spirometry measures also increased by 7% and were maintained at 24 months.
When considering the individual curvature type, differences in the outcomes were recorded. The thoracic scoliosis group recorded an average Cobb angle reduction of 11.5° ± 8.9°, with a sustained reduction of 10° ± 9° at 24 months. The thoracic curvature group mirrored the results of the entire sample, likely because of the fact that they comprised the largest portion of the group. The lumbar group achieved similar results to the thoracic group, with a 10.6° ± 8.8° reduction at 6 months and a sustained improvement of 9.6° ± 9.9°. The lumbar group showed slight improvement in spirometry at 6 months, but this decreased at 24 months. The thoracolumbar group was significant in that it averaged the highest baseline QNPS score and the lowest baseline spirometry measurement. Patients in this group also had the lowest average baseline Cobb angle and achieved the largest Cobb angle reduction of 17.2° ± 4.2° at 6 months. This reduction was maintained at 24 months (17.2° ± 4.0°). The QNPS score for this group also demonstrated the biggest drop (57%) at 6 months, but slightly regressed at 24 months (increased 8%). The FRI disability rating improved from 54% at baseline to 30% at 6 months and further improved to 7% at 24 months. Spirometry measurements increased by 400 mL at 6 months and another 150 mL at 24 months. Finally, the chiropractic rehabilitation program did not seem to positively or negatively affect the magnitude of the Cobb angles in the double major group. From baseline to 6 months and to 24 months, the QNPS scores decreased from 46 to 35 to 22. Respective FRI scores improved as well: 51%, 28%, and 17%. Spirometry scores were essentially unchanged throughout the study period for this group.
Discussion
There are very little published data showing the ability of a nonsurgical, nonbracing, exercise-based therapy to provide a corrective benefit for scoliosis patients, especially in the long term. These data are among the first to demonstrate a sustained radiographic benefit well after clinic treatment had been ceased. All of these patients were skeletally mature at the time of treatment. Although patients in the double major group likely received no Cobb angle benefit, positive outcomes in pain rating and disability scores were recorded following treatment, which were the main reasons all patients in this entire sample initially presented.
Two patients in this study (1 in the double major group, 1 in the lumbar group) progressed following the 6 months of clinic treatment. It is unknown why these 2 patients continued to progress. Compliance monitoring, incorrect weighting configurations, or incidental disregard for other unforeseen factors may be responsible for treatment failure in these 2 instances.
It is important to note that all of these patients were instructed, upon release from care, to continue to perform home maintenance exercises. This study failed to collect this information. This may have shown which patients were the most compliant, thus demonstrating how the sustained performance of home care may have affected the collective and individual results. Future studies by this author will include home journals for patients to record their compliance levels, which can then be statistically analyzed. Furthermore, because these patient charts were pulled from 2 clinics by the author, the study design cannot exclude examiner bias in the selection process. However, care was taken to select patients based upon demographic data and inclusion criteria only, so that as many files could be included as possible.
This appears to be the first study in which chiropractic rehabilitation methods were used to reduce the severity of scoliosis, as well as its effect on pain, activities of daily living, and respiratory function. It is also the first chiropractic study to evaluate these results 24 months after clinic treatment was concluded.
Limitations
As a retrospective design, this case study has inherent flaws. Patients who failed treatment were included, and another chiropractor analyzed the radiographs. Because of the retrospective study design, only patients who presented for a 24-month follow-up were included, which may bias the findings. Some cases were not usable because they did not complete a final examination at 24 months. Several modalities were used by the patients in this study, so it is unknown which of the specific modalities within this program had the most significant impact on the patients' outcomes. Because the patients in this cohort did not report for treatment until they were adults, it is unknown how many of them had their scoliosis as juveniles or adolescents, thereby contributing to a more progressive nature of the curvature. It is possible that at least some of these patients were not at a high risk for further progression; and therefore, their natural history of the scoliosis could not be fully predicted. However, the pain and functional improvements recorded in this study support the potential ability of chiropractic rehabilitation to positively impact adult patients with scoliosis.
Conclusion
This retrospective case series analyzed the long-term results of 28 patients treated for adult scoliosis. Of these patients, Cobb angle reductions were recorded in 22 of the 28 patients, with the remaining 6 patients (double major group) receiving no apparent Cobb angle benefit. Improvements in pain scores and disability ratings were recorded among all curvature types at 6 and 24 months. The thoracic, lumbar, and thoracolumbar groups demonstrated improvement in spirometry, which did not change in the double major group.
Funding sources and potential conflicts of interest
No funding sources were reported for this study. The author is Director of Research for the Pettibon Institute.
References
- 1.Marty-Poumarat C., Scattin L., Marpeau M., Garreau de Loubresse C., Aegerter P. Natural history of progressive adult scoliosis. Spine. 2007;32:1227–1234. doi: 10.1097/01.brs.0000263328.89135.a6. [DOI] [PubMed] [Google Scholar]
- 2.Weinstein S.L., Dolan L.A., Spratt K.F., Peterson K.K., Spoonamore M.J., Ponseti I.V. Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA. 2003;289:559–567. doi: 10.1001/jama.289.5.559. [DOI] [PubMed] [Google Scholar]
- 3.Weinstein S.L. Natural history. Spine. 1999;24:2592–2600. doi: 10.1097/00007632-199912150-00006. [DOI] [PubMed] [Google Scholar]
- 4.Aebi M. The adult scoliosis. Eur Spine J. 2005;14:925–948. doi: 10.1007/s00586-005-1053-9. [DOI] [PubMed] [Google Scholar]
- 5.Hawes M.C., O'Brien J.P. The transformation of spinal curvature into spinal deformity: pathological processes and implications for treatment. Scoliosis. 2006;1:3. doi: 10.1186/1748-7161-1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Everett C.R., Patel R.K. A systematic literature review of nonsurgical treatment in adult scoliosis. Spine. 2007;32:S130–S134. doi: 10.1097/BRS.0b013e318134ea88. [DOI] [PubMed] [Google Scholar]
- 7.Romano M., Negrini S. Manual therapy as a conservative treatment for adolescent idiopathic scoliosis: a systematic review. Scoliosis. 2008;3:2. doi: 10.1186/1748-7161-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morningstar M.W., Woggon D., Lawrence G. Scoliosis treatment using a combination of manipulative and rehabilitative therapy: a retrospective case series. BMC Musculoskelet Disord. 2004;5:32. doi: 10.1186/1471-2474-5-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morningstar M.W., Joy T. Scoliosis treatment using spinal manipulation and the Pettibon Weighting System: a summary of 3 atypical presentations. Chiropr Osteopat. 2006;14:1. doi: 10.1186/1746-1340-14-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beauchamp M., Labelle H., Grimand G., Stanciu C., Poitras B., Dansereau J. Diurnal variation of Cobb angle measurement in adolescent idiopathic scoliosis. Spine. 1993;18:1581. doi: 10.1097/00007632-199309000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Zetterberg C., Hansson T., Lindstrom J., Irstam L., Andersson G.B. Postural and time-dependent effects on body height and scoliosis angle in adolescent idiopathic scoliosis. Acta Orthop Scand. 1983;54:836. doi: 10.3109/17453678308992918. [DOI] [PubMed] [Google Scholar]
- 12.Harrison D.E., Harrison D.D., Colloca C.J., Betz J., Janik T.J., Holland B. Repeatability over time of posture, radiograph positioning, radiograph line drawing: an analysis of six control groups. J Manipulative Physiol Ther. 2003;26:87–98. doi: 10.1067/mmt.2003.15. [DOI] [PubMed] [Google Scholar]
- 13.Saunders E.S., Woggon D., Cohen C. Improvement of cervical lordosis and reduction of forward head posture with anterior head weighting and proprioceptive balancing protocols. J Vertebral Subluxation Res. 2003 [Google Scholar]
- 14.Morningstar M.W., Strauchman M.N., Weeks D.A. Spinal manipulation and anterior headweighting for the correction of forward head posture and cervical hypolordosis: a pilot study. J Chiropr Med. 2003;2:51–54. doi: 10.1016/S0899-3467(07)60042-1. [DOI] [PMC free article] [PubMed] [Google Scholar]


