Abstract
Objective
Attempts to treat class II malocclusions without extraction in non-compliant patients have led to utilization of intraoral molar distalizing appliances. The purpose of this study was to investigate dental and skeletal effects of Bonded Molar Distalizer (BMD) which is a simple molar distalizing appliance.
Materials and Methods
Sixteen patients (12 girls, four boys) with bilateral half-cusp class II molar relationship, erupted permanent second molars and normal or vertical growth pattern were selected for bilateral distalization of maxillary molars via BMD. The screws were activated every other day, alternately. Lateral cephalograms and study models were obtained before treatment and after 11 weeks activation of the appliance.
Results
Significant amounts of molar distalization, molar distal tipping and anchorage loss were observed. The mean maxillary first molar distal movement was 1.22±0.936 mm with a distal tipping of 2.97±3.74 degrees in 11 weeks. The rate of distal movement was 0.48 mm per month. Reciprocal mesial movement of the first premolars was 2.26±1.12 mm with a mesial tipping of 4.25±3.12 degrees. Maxillary incisors moved 3.55±1.46 mm and tipped 9.87±5.03 degrees mesially. Lower anterior face height (LAFH) decreased 1.28±1.36 mm.
Conclusion
BMD is appropriate for distalizing maxillary molars, especially in patients with critical LAFH, although significant amounts of anchorage loss occur using this appliance.
Keywords: Malocclusion Angle Class II, Patient Non-Compliance, Bonded Appliance, Screw
INTRODUCTION
Non-extraction treatment of class II malocclusion needs distalization of the upper molars to correct molar relationship and create enough space to resolve increased overjet. Several techniques have been used for molar distalization. Some of these techniques need complete cooperation of the patients (e.g. extra oral force, cetlin plate and class II inter arch elastics) [1–4].
Unfortunately, the patients’ compliance is an unpredictable factor which can widely affect the results of treatment. Therefore, utilization of noncompliant appliances minimizes the need for patient cooperation and prepares a more reliable treatment alternative [5].
Trends for utilizing intramaxillary anchorage for maxillary molar distalization have risen up since the late 1970s [6]. Numerous fixed appliances such as pendulum appliance, jones jig, magnets, coils, distal jet, first class appliance and mini implants have been developed to overcome the limitations of headgear and decrease dependence on the patient’s compliance. Despite less dependence on the patient, most intra oral appliances result in clinically undesirable effects such as tipping of the first molars, loss of anterior anchorage, clockwise rotation of the mandibular plane and increase of the lower anterior facial height [7–16].
Bonded acrylic appliances have been used in orthodontics for rapid palatal expansion [17]. Furthermore, bonded modification of some functional appliances such as twin block and Hamilton activator can be utilized if necessary [18]. In this study we introduce a fixed appliance for distalizing upper molars. This appliance is bonded to the molars and premolars and contains an ordinary orthodontic screw to produce the distalizing force (bonded molar distalizer, BMD). The purpose of this clinical study was to investigate dentoalveolar and skeletal effects of BMD in all three spatial planes while using BMD.
MATERIALS AND METHODS
In order to arrange a historical cohort study, 16 patients (12 male, four female) were selected based on the following criteria:
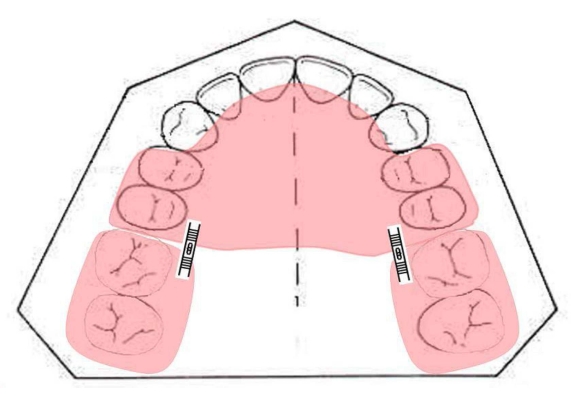
All patients had bilateral half cusp class II molar relationship and were in permanent dentition. Second molars were erupted in all cases. None of the patients had severe incisor protrusion and they had never used any other distalizing appliances. They had a normal or vertical growth pattern. Oral hygiene was appropriate in all cases. They also were medically checked and had no systemic diseases or syndromes. The study was approved by the ethical committee of research center of Tehran University of Medical Sciences and was performed under its observation. After giving comprehensive explanations about the expected advantages and disadvantages of BMD, informed consent was signed by parents before starting treatment. The appliance we used for molar distalization contained two components, the acrylic part and screw parts (Fig 1).
Fig 1.
Bonded Molar Distalizer
Acrylic component: In order to reduce anchorage loss, the palate was covered by acrylic. The acrylic component is extended over the occlusal and facial and lingual surfaces of the premolars and molars up to 1–2 mm before the facial free gingiva. Bonding the appliance to these surfaces creates a posterior bite plate.
Orthodontic screw: Mini expansion screw (dentaurum) with a maximum opening of 6.5 mm was used. 360° opening of this screw produces 0.7 mm distance. Therefore, one turn opening leads to 0.175 mm movement. After impression, the casts were prepared. The first stage in manufacturing the appliance is determination of the location of the screws which are placed close to the molar’s centre of resistance, parallel to the occlusal plane, between the first molars and second premolars. Whereas, the line of action of the force passes through molar’s center of resistance, we expected less tipping in these teeth. Palatal and buccal surfaces of premolars and first molars were etched via 37 percent phosphoric acid for 40 seconds and the appliances were bonded with light cured composite (Fig 2A and B).
Fig 2.
A, Occlusal and B, Lateral intraoral photographs of a 12-year-old boy treated with BMD after bonding BMD; C, Lateral photograph after
In order to have appropriate occlusal contacts and to reduce the probability of debonding, occlusal surfaces of the appliances were adjusted regarding opposite teeth before bonding. Activation of appliance:
Parents were instructed to open the screws in the beginning of the night. Distalizing force was exerted via one turn (90°) opening of the screw of each side, one other day and alternately.
The first patient visit after appliance insertion was 3 days after bonding it. Patients were visited every two weeks till the end of treatment (Fig 2C). The first lateral cephalograms (T1) were taken before starting distalization. Eleven weeks after appliance therapy, force exertion discontinued and final lateral cephalograms (T2) were taken. Study casts were also provided before and after tooth movement to investigate transverse dental relationships.
Cephalometeric analysis
All radiographs were taken in an identical center with an identical radiographic set. They were traced manually using a 0.5 mm pencil. All radiographs were traced twice and the mean value was reported as the final measurement.
Positional changes of the central incisor were measured based on alterations in the position of the incisal edge. In order to investigate the position of the molars and premolars, the centroid point of their crowns which is the midpoint of the line connecting the mesial height of the contour to the distal height of the contour was selected.
The perpendicular bisector of this line was considered as the teeth’s long axis.
The line connecting the apex to the incisal edge was considered as the long axis of the central incisor. The palatal plane was used as the horizontal reference line to determine the vertical positional changes of the teeth while pt-vertical line (PTV), was used to investigate the anteroposterior changes. The angles formed between long axes of the teeth with SN were used to determine the amount of their tipping. Lower anterior facial height (ANS-Me) and Frankfurt mandibular plane angle (FMA) were also measured for each patient to investigate possible skeletal changes.
Analysis of dental casts
Transverse measurements were performed on dental casts between molars mesiobuccal and distobuccal cusp tips, before and after tooth movement.
Mean value, standard deviation, maximum and minimum amounts were calculated for each measurement.
We used digital caliper with 0.01 mm accuracy for linear measurements and protractor with 0.5° accuracy for angular measurements.
Wilcoxon Signed Rank test was used for statistical analysis.
RESULTS
All patients tolerated appliance well and did not reveal pain or mobility of teeth.
There was no evidence of caries or white spots.
Dependant on oral hygiene, some patients showed mild inflammation in the marginal gingiva and interdental papilla in acrylic covered areas at the time of appliance removal.
This inflammation was resolved completely after 3–4 days application of cholorohexidine, oral hygiene care and gingival massage.
Dental changes
Anteroposterior changes
In this study.upper molars tipped 2.97±3.74 degrees distally on the average (p<0.01), while mesial tipping of the first premolars and the upper incisors was 4.25±3.12 (p<0.001) and 9.78±5.04 degrees (p<0.001), respectively which were all statistically significant.
The mean amount of the distal movement of the first molars and second molars was 1.22±0.936 mm (p<0.001) and 1.034±0.854 mm (p<0.01), respectively, which were statistically significant. The first premolars moved 2.26±1.12 (p<0.001) mesially and the upper incisors moved 3.551.46 mm (p<0.001) mesially which were also statistically significant. The mean amount of space opened between the first molar and the first premolar was 3.18±1.03 mm (p<0. 001) which was also significant.
Vertical changes
The first molars intruded 1.02±0.75 mm (p<0.05). The second molars and incisors also intruded 1.23±1.11 mm (p<0.001) and 1.25±1.25 mm (p<0.001), respectively which were all statistically significant. On the other hand, the first premolars extruded 0.21±1.07 mm (p=0.38), which was not statistically significant.
Transverse changes
Comparison of dental casts before and after treatment revealed 2.68±0.87 mm (p<0.001) increase in the distance between the mesiobuccal cusp tips of the first molars and 3.34±0.95 mm (p<0.001) increase between the distobuccal cusp tips of these teeth which were statistically significant.
Skeletal changes
Anteroposterior skeletal changes were minimal.
Lower anterior facial height (ANS-Me) decreased 1.28±1.36 mm (p<0.001). The mean reduction of the mandibular plane angle (FMA) was 1.03±1.38 degrees (p<0.05) which were both statistically significant.
Pretreatment and post treatment means and standard deviations of the variables under investigation are listed in Table I.
Table I.
Comparison of cephalometric and dental cast measurements before (T1) and after treatment (T2)
| Variable | T1 | T2 | Difference of means | Significance | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | (T2-T1) | SD | P | |
| Cephalometric variables | |||||||
| Skeletal sagittal measurements | |||||||
| SNA (°) | 79.813 | 3.336 | 79.625 | 3.367 | −0.188 | 0.892 | 0.483 |
| SNB (°) | 72.781 | 3.440 | 73.563 | 3.97 | 0.78 | 0.948 | 0.019 |
| ANB (°) | 7.032 | 6.062 | −0.97 | ||||
| Skeletal vertical measurements | |||||||
| ANS-Me | 71.961 | 5.749 | 70.676 | 5.870 | −1.286 | 1.36 | 0.003 |
| FH-mandibular plane (°) | 30.906 | 4.462 | 29.875 | 4.577 | −1.031 | 1.384 | 0.015 |
| Mandibular plan-palatal plane (°) | 28.344 | 5.56 | 26.625 | 5.233 | −1.72 | 1.426 | 1.000 |
| Dentoalveolar angular measurements | |||||||
| SN-6 (°) | 63.969 | 5.575 | 61 | 6.56 | −2.969 | 3.744 | 0.006 |
| SN-7(°) | 56.5 | 7.071 | 53.875 | 7.108 | 2.625 | 0.855 | 0.006 |
| SN-4 (°) | 79.625 | 4.189 | 83.875 | 5.647 | 4.25 | 3.12 | 0.001 |
| SN-1 (°) | 95.094 | 7.647 | 104.969 | 7.475 | 9.875 | 5.0382 | 0.0001 |
| Dentoalveolar linear measurements (sagittal) | |||||||
| PTV-6 centroid (mm) | 21.553 | 3.556 | 20.334 | 3.454 | −0.748 | 0.936 | 0.001 |
| PTV-7centroid (mm) | 12.254 | 2.798 | 11.216 | 2.762 | −1.11 | 0.854 | 0.002 |
| PTV-4 centroid (mm) | 38.362 | 40.204 | 40.625 | 4.504 | 0.21 | 1.117 | 0.0001 |
| PTV-1 (mm) | 53.772 | 3.859 | 57.32 | 4.194 | −1.248 | 1.46 | 0.0001 |
| Dentoalveolar linear measurements (vertical) | |||||||
| Palatal plane-6 centroid (mm) | 18.592 | 1.859 | −0.747 | 1.019 | −1.22 | 1.02 | 0.017 |
| Palatal plane-7 centroid (mm) | 12.81 | 3.61 | −1.11 | 1.23 | −1.043 | 1.23 | 0.004 |
| Palatal plane-4 centroid (mm) | 21.378 | 2.249 | 0.21 | 1.068 | 2.264 | 1.068 | 0.379 |
| Palatal plane-1 (mm) | 27.916 | 2.762 | −1.248 | 1.249 | 3.55 | 1.25 | 0.004 |
| Dental cast variables | |||||||
| 6-MB(mm) | 49.606 | 1.346 | 52.291 | 1.923 | 2.684 | 0.871 | 0.0001 |
| 6-DB (mm) | 52.043 | 1.754 | 55.386 | 2.143 | 3.343 | 0.951 | 0.0001 |
| 4-MB (mm) | 38.918 | 1.995 | 39.197 | 1.984 | 0.28 | 0.39 | 0.016 |
DISCUSSION
In recent years, in order to treat class II malocclusions without extracting teeth and with less dependence to the patient’s cooperation, orthodontists have attempted to distalize upper molars using intraloral appliances. Variable appliances such as magnets, coils, super elastic arch wires, distal jet and pendulum appliances have been used for this purpose.
In this study, we investigated dental and skeletal effects of BMD on 16 patients.
Dental changes
Anteroposterior changes
In the current study, the first molars and second molars moved 1.22±0.936 mm and 1.034±0.854 mm distally, respectively in about 11.25±3.44 weeks. Table II compares these results with some other studies using intraoral distalizing appliances [10, 11, 13, 19–33]. At the first glance, it seems that the amount of distal molar movement via BMD is less than other appliances.
Table II.
Comparison of alterations after treatment with some noncompliance distalization appliances
| Appliance | Duration of treatment (months) | Molar distal movement (mm) | Rate of distalization | Molar distal tipping (degrees) | Premolar mesial movement (mm) | Premolar mesial tipping (degrees) | Incisor mesial movement (mm) | Incisor mesial tipping (degrees) | Mandibular plan angle | Lower anterior facial height | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Ghosh Nanada11 | Pendulum | 6.21 m | 3.37 | 0.54 | 8.36 | 2.5 | 1.3 | N.A | 2.40 | +2.97 | |
| Bussik19 | Pendulum | 7 m | 5.7 | 0.81 | 10.60 | 1.8 | 1.5 | 1.4 | 3.60 | +1 | +2.2 |
| Toroglu20 | Pendulum | 5 m | 4.1 | 0.82 | 13.4 | 6.6 | 5.9 | 4.1 | 8.7 | +1.8*/+1.4** | +2.1*/+3.8** |
| Chaques21 | Pendulum | 6.5 m | 5.3 | 0.81 | 13.06 | 2.2 | 4.8 | 2.1 | 5.14 | ||
| Chiue22 | Pendulum | 7 m | 6.1 | 0.87 | 10.7 | 1.4 | −1.7 | 1.1 | 3.10 | 1.3 | +2.5 |
| Bondermak10 | Magnet | 16 m | 4.2 | 1.1 | 8.00 | N.A | N.A | 1.8 | 5.80 | ||
| Bondermak23 | Magnet | 6 m | 2.2 | 0.36 | 1.00 | N.A | N.A | 1.9 | 4.04 | 1.1 | |
| Bondermark23 | Super coil | 6 m | 3.2 | 0.53 | 1.00 | N.A | N.A | 1.9 | 4.04 | 1.1 | |
| Bondermak24 | Magnet | 5.8 m | 2.6 | 0.37 | 8.80 | 1.8 | 6.7 | 1.9 | 5.5 | 0.5 | +1.1 |
| Bondermark24 | Niti coil | 5.8 m | 2.5 | 0.43 | 2.20 | 1.2 | 2.1 | 1.5 | 4.7 | 0.6 | +1.3 |
| Runge25 | Jones jig | 6.3 m | 2.2 | 0.35 | 4.0 | 2.2 | 9.5 | 2.00 | −0.08 | +1 | |
| Brick man13 | Jones jig | 6.35 m | 2.5 | 0.39 | 7.53 | 2.0 | 4.8 | N.A | 2.4 | −0.06 | +1.46 |
| Haydar26 | Jones jig | 2.5 m | 2.8 | 1.12 | 7.85 | 3.3 | 6.0 | 0.55 | 1.00 | 0.65 | N.A |
| Papadopoulos27 | Modified jig | 3.8 m | 1.4 | 0.37 | 6.80 | 2.6 | 8.1 | 2.3 | 4.80 | ||
| Marvopolous28 | Modified jig | 4.1m | 2.8 | 0.68 | 6.8 | 3.3 | 7.5 | 1.8 | 5.16 | ||
| Ngantung29 | Distal jet | 6.7 m | 2.12 | 0.31 | 3.26 | 2.6 | 4.3 | N.A | 12.16 | +2.4 | |
| Bolla30 | Distal jet | 5 m | 3.2 | 0.64 | 3.10 | 1.3 | 2.8 | N.A | 0.6 | −0.3 | +0.9 |
| Nishii et al31 | Distal jet | 6.4 m | 2.4 | 0.37 | 1.8 | 1.4 | 1.5 | 4.5 | |||
| Chiue22 | Distal jet | 10 m | 2.8 | 0.28 | 5.0 | 2.6 | 0.3 | 3.7 | 13.7 | 0.7 | +2.4 |
| Fortini32 | First class | 2.4 m | 4 | 1.6 | 4.60 | 1.7 | 2.2 | 1.3 | 2.6 | 0.5 | N.A |
| Papadopoulos33 | First class | 4 m | 4 | 1 | 8.6 | 1.9 | 1.9 | 1.6 | 2.00 | N.A | N.A |
| Current study | BMD | 2.5 m | 1.22 | 0.48 | 2.97 | 2.26 | 4.25 | 3.55 | 9.87 | −1.03 | −1.28 |
for low angle group and
for high angle group
More careful investigation of this table reveals that less distal movement in this study might simply be arised from the shorter duration of treatment with BMD.
Therefore, it seems logical to compare distal molar movements per month (rates of distalization) instead of comparing pure molar movements.
This method eliminates the duration of treatment as an interfering factor.
Referring table I, rate of distalization for BMD is generally more than distal jet and magnets and equals with coils and jigs.
Although the amount of distal molar movement via BMD is less than pendulum and first class appliances, the molar tipping was significantly less instead.
BMD have succeeded to move molars more bodily.
In spite of this, less molar tipping may also be the result of less distal movement and less duration of treatment, and if molars were distalized as much as other studies, they might have tipped more.
Existence of the second molars and their bodily movement simultaneous with the first molars may be another possible reason for less distal movement.
Nevertheless, there is controversy about the effects of eruption of the second molar on the amount of distal movement of the first molar.
Nanda and Ghosh used pendulum appliance and did not find any significant difference in the amount of the first molars distal movement among patients with erupted second molars and the group in which second molars had not erupted yet [11].
Josef also achieved the same result [34]. In spite of their result, Gianelly and Kinzinger revealed that presence of the second molars increases the duration of treatment. Kinzinger also pointed out that presence of the second molar increases the trend of tipping of the first molar during distalization [35,36]. Since the second molars in all patients had erupted in our study, such comparison was impossible.
Nevertheless, if the second molars could affect the rate of distalization reversely, it might be another reason for less distal movement via BMD.
Alterations of the anchorage unit are calculated based on the mesial movement of the first premolars and incisors.
In this research, necessary anchorage for molars distalization was provided by the first and second premolars and their supporting bone, the anterior base of the maxilla, and the incisors’ supporting alveolar bone.
Using BMD for 11.25±3.44 weeks, the premolars moved 2.26±1.12 mm mesially and tipped 4.25±3.12 mm mesially, while the incisors moved 3.55±1.46 mm and tipped 9.87± 5.03 mm mesially.
Our results revealed that anchorage loss by premolar mesial movement was less than the-reports by Ghosh and Nanda
et al (pendulum), Haydar et al (jones jig), Ngantung et al (distal jet), Chiu et al (distal jet), Papadopoulos et al (Modified Jig) and Marvopoulos et al (Modified Jig) [11,20,26–29] while it was more than the other reports. Similar situation is observed for the mesial movement of the incisors and premolar mesial tipping.
Incisor mesial tipping was more than the majority of past records.
Regarding these comparisons we may result that the amount of anchorage loss in this research was intermediate to great.
Despite other appliances, BMD does not contain the Nance button in the anchorage unit which seems has led to more movement of the anchorage unit.
Furthermore, BMD exerts direct force to the incisors. Considering mesial tipping of the incisors, it seems that BMD might be a good choice for patients with class II molar relationship combined with retrusion of the incisors.
Greater amounts of anchorage loss, especially incisor mesial tipping may also be the result of direct application of force to the anchorage unit.
Although the screws of the left and right side were opened alternately, the anchorage unit had always been under the interrupted force arising from screw opening.
Despite the fact that we used palatal anchorage and covered premolars, since bodily movement requires stronger anchorage, more bodily movement of the molars in this study may be one of the reasons of more anchorage loss.
Another reason for anchorage loss in this research may be the existence of second molars.
Effective biologic movement of one molar requires 180g force and simultaneous movement of two molars needs 300–350g force [23, 37]. In this study, all the second molars had erupted and were moved with the first molar which may affect anchorage loss. It is revealed that if pendulum appliance is utilized before eruption of the second molars, the result will be 2/3 distal molar movement and 1/3 anchorage loss 9). Otherwise, if treatment begins after second molar eruption has completed, the result would converse. Gianelly suggests distalizing the first molar before eruption of the second molar. He also suggests that for cases in which second molars have erupted, at first attain distalizing second molars and after stabilization of their position, start distalization of the first molars. This method has been suggested to result in less anchorage loss; however, it increases the duration of treatment up to at least 6 mounts [36].
Vertical changes
Although in our study the molars were intruded, the amount of intrusion was not remarkable in comparison with distal movement. Intrusion of the molars may be related to the posterior bite plate as masticatory forces and pressure of muscles in rest facilitate intrusion of the molars or at least prevent their extrusion. Incisors’ intrusion may be related to great amounts of their mesial tipping because increase in labial inclination leads to relative upward movement of incisal edges leading to relative intrusion of these teeth which helps opening the bite.
Transverse changes
Measurements of dental casts revealed an increase in inter molar width which was 2.68±0.78 mm between mesiobuccal cusp tips of the first molars and 3.34±0.95 mm between their distobuccal cusp tips. Increase in the inter molar width might be a reason of posterior buccal cross bite following molar distalization. Since axes of the screws were parallel to the line of occlusion and there was no acrylic to connect the two molars, molar movement would be distal and buccal. Greater increase in the distance between distobuccal cusps in comparison to mesiobuccal cusps may also denote distobuccal rotation of the molars as was expected since force exertion was lingual to molars’ center of resistance. It was reported that using pendulum appliance, the distance between mesiobuccal cusp tips increased 1.4 mm, while the distance between distobuccual cusp tips did not change significantly which was indicative of mesiobuccul rotation of the first molars [11]. We observed buccal cross bite in the premolar area after treatment with BMD. Since the transverse distance between the first premolars did not increase significantly as was expected because of the rigidity of acrylic, manifestation of buccal cross bite in the premolar region might be related to loss of anchorage and mesial movement of these teeth.
Skeletal effects
Considering our results, anteroposterior positional changes of the maxilla and mandible based on SNA and SNB were minimal. In spite of this, indicators of the lower anterior facial height such as FMA and linear measurement of ANS-Me revealed significant reduction (p<0.01). FMA decreased 1.03±1.38 degrees (p<0.05).
Significant reduction of the lower anterior facial height might be related to intrusion of the molars.
Decrease in over bite despite reduction of the lower anterior facial height may be the result of upper incisor protrusion.
None of the studies stated above revealed decrease in the anterior facial height. Therefore, from this point of view BMD is a unique appliance. Regarding the aforementioned results, it can be concluded that presence of posterior bite plane in BMD was effective on prevention of molar extrusion and mandibular downward rotation.
This feature is especially important in patients with increased lower anterior facial height and vertical growth pattern. Prevention of increase in facial height which occurs via other distalizing appliances is critical in this group of patients. Using BMD, the facial height not only does not increase, but also decreases which is desirable for long face patients. Therefore, distalization of maxillary molars in vertical growing patients might be a special clinical application for BMD.
CONCLUSION
Distalization of upper molars with BMD is coincident with less distal tipping and more bodily movement of the molars.
Relatively great amounts of anchorage loss occur. Furthermore, bonded acrylic appliances have the disadvantages of difficulty in chewing and compromised hygiene. The exclusive feature of BMD is that it decreases lower anterior facial height which possibly makes it a suitable choice for patients with a long face problem and a vertical growth pattern.
ACKNOWLEDGMENTS
The authors would like to thank Dr Soheil Saadat for statistical analyzing and valuable comments on the manuscript.
REFERENCES
- 1.Nanda R. Biomechanics and esthetic strategies in clinical orthodontics. St Louis, Missouri: Elsevier; 2005. pp. 178–83. [Google Scholar]
- 2.Klein PL. An evaluation of cervical traction on the maxilla and the upper first permanent molar. Angle Orthod. 1957;27:61–8. [Google Scholar]
- 3.Kloehn SJ. Evaluation of cervical anchorage force in treatment. Angle Orthod. 1961;31:91–104. [Google Scholar]
- 4.Cetlin NM, Ten Hoeve A. Nonextraction treatment. J ClinOrthod. 1983 Jun;17(6):396–413. [PubMed] [Google Scholar]
- 5.Papadopoulos MA. Non-compliance distalization: a monograph on the clinical management and effectiveness of a jig assembly in Class II malocclusion orthodontic treatment. Thessaloniki, Greece: Phototypotiki; 2005. [Google Scholar]
- 6.Kinzinger GS, Eren M, Diedrich PR. Treatment effects of intraoral appliances with conventional anchorage designs for non-compliance maxillary molar distalization: a literature review. Eur J Orthod. 2008 Dec;30(6):558–71. doi: 10.1093/ejo/cjn047. [DOI] [PubMed] [Google Scholar]
- 7.Gianelly AA, Bednar J, Dietz VS. Japanese NiTi coils used to move molars distally. Am J OrthodDentofacialOrthop. 1991 Jun;99(6):564–6. doi: 10.1016/S0889-5406(05)81633-6. [DOI] [PubMed] [Google Scholar]
- 8.Jones RD, White JM. Rapid Class II molar correction with an open-coil jig. J ClinOrthod. 1992 Oct;26(10):661–4. [PubMed] [Google Scholar]
- 9.Hilgers JJ. The pendulum appliance for Class II non-compliance therapy. J ClinOrthod. 1992 Nov;26(11):706–14. [PubMed] [Google Scholar]
- 10.Bondemark L, Kurol J. Distalization of maxillary first and second molars simultaneously with repelling magnets. Eur J Orthod. 1992 Aug;14(4):264–72. doi: 10.1093/ejo/14.4.264. [DOI] [PubMed] [Google Scholar]
- 11.Ghosh J, Nanda RS. Evaluation of an intraoral maxillary molar distalization technique. Am J OrthodDentofacialOrthop. 1996 Dec;110(6):639–46. doi: 10.1016/s0889-5406(96)80041-2. [DOI] [PubMed] [Google Scholar]
- 12.Carano A, Testa M. The distal jet for upper molar distalization. J ClinOrthod. 1996 Jul;30(7):374–80. [PubMed] [Google Scholar]
- 13.Brickman CD, Sinha PK, Nanda RS. Evaluation of the Jones jig appliance for distal molar movement. Am J OrthodDentofacialOrthop. 2000 Nov;118(5):526–34. doi: 10.1067/mod.2000.110332. [DOI] [PubMed] [Google Scholar]
- 14.Kinzinger G, Fuhrmann R, Gross U, Diedrich P. Modified pendulum appliance including distal screw and uprighting activation for non-compliance therapy of Class II malocclusion in children and adolescents. J OrofacOrthop. 2000;61(3):175–90. doi: 10.1007/s000560050003. [DOI] [PubMed] [Google Scholar]
- 15.McSherry PF, Bradley H. Class II correction-reducing patient compliance: a review of the available techniques. J Orthod. 2000 Sep;27(3):219–25. doi: 10.1179/ortho.27.3.219. [DOI] [PubMed] [Google Scholar]
- 16.Papadopoulos MA. Clinical efficacy of the non-compliance appliances used for Class II orthodontic correction. In: Papadopoulos MA, editor. Orthodontic treatment for the Class II non-compliant patient: current principles and techniques. Edinburgh, United Kingdom: Elsevier, Mosby; 2006. pp. 367–87. [Google Scholar]
- 17.Wendling LK, McNamara JA, Jr, Franchi L, Baccetti T. A prospective study of the short-term treatment effects of the acrylic-splint rapid maxillary expander combined with the lower Schwarz appliance. AngleOrthod. 2005 Jan;75(1):7–14. doi: 10.1043/0003-3219(2005)075<0007:APSOTS>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 18.Graber TM. Functional appliances. In: Graber TM, Vanarsdall RL, Katherine WL, editors. Orthodontics current principles and techniques. St Louis: Elsevier Mosby; 2005. p. 515. [Google Scholar]
- 19.Bussick TJ, McNamara JA., Jr Dentoalveolar and skeletal changes associated with the pendulum appliance. Am J OrthodDentofacialOrthop. 2000 Mar;117(3):333–43. doi: 10.1016/s0889-5406(00)70238-1. [DOI] [PubMed] [Google Scholar]
- 20.Toroglu MS, Uzel I, Cam OY, Hancioglu ZB. Cephalometric evaluation of the effects of pendulum appliance on various vertical growth patterns and of the changes during short-term stabilization. ClinOrthod Res. 2001 Feb;4(1):15–27. doi: 10.1034/j.1600-0544.2001.040103.x. [DOI] [PubMed] [Google Scholar]
- 21.Chaqués-Asensi J, Kalra V. Effects of the pendulum appliance on the dentofacial complex. J ClinOrthod. 2001 Apr;35(4):254–7. [PubMed] [Google Scholar]
- 22.Chiu PP, McNamara JA, Jr, Franchi L. A comparison of two intraoral molar distalization appliances: distal jet versus pendulum. Am J OrthodDentofacialOrthop. 2005 Sep;128(3):353–65. doi: 10.1016/j.ajodo.2004.04.031. [DOI] [PubMed] [Google Scholar]
- 23.Bondemark L, Kurol J, Bernhold M. Repelling magnets versus superelastic nickel-titanium coils in simultaneous distal movement of maxillary first and second molars. Angle Orthod. 1994;64(3):189–98. doi: 10.1043/0003-3219(1994)064<0189:RMVSNC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 24.Bondemark L. A comparative analysis of distal maxillary molar movement produced by a new lingual intra-arch Ni-Ti coil appliance and a magnetic appliance. Eur J Orthod. 2000 Dec;22(6):683–95. doi: 10.1093/ejo/22.6.683. [DOI] [PubMed] [Google Scholar]
- 25.Runge ME, Martin JT, Bukai F. Analysis of rapid molar distal movement without patient cooperation. Am J OrthodDentofacialOrthop. 1999 Feb;115:153–7. doi: 10.1016/S0889-5406(99)70343-4. [DOI] [PubMed] [Google Scholar]
- 26.Haydar S, Uner O. Comparison of Jones jig molar distalization appliance with extraoral traction. Am J Orthod Dentofacial Orthop. 2000 Jan;(11791):49–53. doi: 10.1016/s0889-5406(00)70247-2. [DOI] [PubMed] [Google Scholar]
- 27.Papadopoulos MA, Mavropoulos A, Karamouzos A. Cephalometric changes following simultaneous first and second maxillary molar distalization using a non-compliance intraoral appliance. J OrofacOrthop. 2004 Mar;65(2):123–36. doi: 10.1007/s00056-004-0317-z. [DOI] [PubMed] [Google Scholar]
- 28.Mavropoulos A, Sayinsu K, Allaf F, Kiliaridis S, Papadopoulos MA, Keles AO. Non-compliance unilateral maxillary molar distalization: a three-dimensional tooth movement analysis. Angle Orthod. 2006 May;76(3):382–7. doi: 10.1043/0003-3219(2006)076[0382:NUMMD]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 29.Ngantung V, Nanda RS, Bowman SJ. Post-treatment evaluation of the distal jet appliance. Am J OrthodDentofacialOrthop. 2001 Aug;120(2):178–85. doi: 10.1067/mod.2001.114645. [DOI] [PubMed] [Google Scholar]
- 30.Bolla E, Muratore F, Carano A, Bowman SJ. Evaluation of maxillary molar distalization with the distal jet: a comparison with other contemporary methods. Angle Orthod. 2002 Oct;72(5):481–94. doi: 10.1043/0003-3219(2002)072<0481:EOMMDW>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 31.Nishii Y, Katada H, Yamaguchi H. Three-dimensional evaluation of the distal jet appliance. World J Orthod. 2002;3:321–7. [Google Scholar]
- 32.Fortini A, Lupoli M, Giuntoli F, Franchi L. Dentoskeletal effects induced by rapid molar distalization with the first class appliance. Am J OrthodDentofacialOrthop. 2004 Jun;125(6):697–705. doi: 10.1016/j.ajodo.2003.06.006. [DOI] [PubMed] [Google Scholar]
- 33.Papadopoulos MA, Melkos AB, Athanasiou AE. Noncompliance maxillary molar distalization with the first class appliance: a randomized controlled trial. Am J OrthodDentofacialOrthop. 2010 May;137(5):586–7. doi: 10.1016/j.ajodo.2009.10.033. [DOI] [PubMed] [Google Scholar]
- 34.Joseph AA, Butchart CJ. An evaluation of the pendulum distalization appliance. SeminOrthod. 2000;6:129–35. [Google Scholar]
- 35.Kinzinger GS, Fritz UB, Sander FG, Diedrich PR. Efficiency of a pendulum appliance for molar distalization related to second and third molar eruption stage. Am J OrthodDentofacialOrthop. 2004 Jan;125(1):8–23. doi: 10.1016/j.ajodo.2003.02.002. [DOI] [PubMed] [Google Scholar]
- 36.Gianelly AA. Distal movement of the maxillary molars. Am J OrthodDentofacialOrthop. 1998 Jul;114(1):66–72. doi: 10.1016/s0889-5406(98)70240-9. [DOI] [PubMed] [Google Scholar]
- 37.Bench R, Gugino C, Hilgers J. Bioprogressive Therapy Part 6: Forces used in bioprogressive Therapy. J ClinOrthod. 1978 Feb;12(2):123–39. [PubMed] [Google Scholar]