Abstract
Studies of many cell types show that level of HIF-1α and HIF-2α is primarily controlled by oxygen-dependent proteasomal degradation, catalyzed by HIF prolyl-hydroxylases (PHDs). However, in hypoxic niche of the intervertebral disc, the mechanism of HIF-α turnover in nucleus pulposus cells is not yet known. We show that in nucleus pulposus cells HIF-1α and HIF-2α degradation was mediated through 26S proteasome irrespective of oxygen tension. Noteworthy, HIF-2α degradation through 26S proteasome was more pronounced in hypoxia. Surprisingly, treatment with DMOG, a PHD inhibitor, shows accumulation of only HIF-1α and induction in activity of its target genes but not of HIF-2α. Loss and gain of function analyses using lentiviral knockdown of PHDs and overexpression of individual PHDs show that in nucleus pulposus cells only PHD2 played a limited role in HIF-1α degradation, again HIF-2α degradation was unaffected. We also demonstrate that the treatment with inhibitors of lysosomal proteolysis results in a strong accumulation of HIF-1α and to a much smaller extent of HIF-2α levels. It is thus evident that in addition to PHD2 catalyzed degradation, HIF-1α turnover in nucleus pulposus cells is primarily regulated by oxygen-independent pathways. Importantly, our data clearly suggests that proteasomal degradation of HIF-2α is not mediated by classical oxygen dependent PHD pathway. These results for the first time provide a rationale for the normoxic stabilization as well as the maintenance of steady state levels of HIF-1α and HIF-2α in nucleus pulposus cells.
Keywords: intervertebral disc, nucleus pulposus, cartilage, hypoxia, HIF, prolyl hydroxylase
INTRODUCTION
The intervertebral disc is a complex tissue that permits a range of motions between adjacent vertebrae and accommodates high biomechanical forces. The outer annulus fibrosus and the cartilagenous endplates enclose a central aggrecan-rich gel-like tissue, the nucleus pulposus that is sparsely populated with cells. One overriding aspect of disc cell biology is that cells of the nucleus pulposus and cells residing in the inner annulus fibrosus are removed from the blood supply. Blood vessels originating in the vertebral body traverse the superficial region of the endplates; none of these vessels infiltrate the nucleus pulposus. With respect to the annulus, Gruber et al pointed out that this tissue is avascular except for small discrete capillary beds in the dorsal and ventral surfaces - in no case does the annulus vasculature enter the nucleus pulposus (1, 2, 3). Thus, the nucleus pulposus cells reside in an avascular, hypoxic tissue niche (4).
Our previous studies have shown that nucleus pulposus cells express Hypoxia Inducible Factor (HIF-1) (5). This molecule is a member of the bHLH–PER-ARNT-SIM (PAS) family of proteins and composed of a constitutively expressed β subunit and an α subunit. The latter subunit is stable under hypoxic conditions, but is rapidly degraded in normoxia (6). It should be added that the other isoform of HIF, HIF-2 is also expressed by the nucleus pulposus cells. Recent evidence suggests that HIF-1α and HIF-2α are not redundant, and that the relative importance of each of the homologues, in response to hypoxia, varies among different cell types (7). Moreover, the target genes are different. For example, unlike HIF-1, HIF-2 regulates expression of a number of unique genes including SOD2, catalase, frataxin and cited2 (8-10). With respect to degradation, these are regulated by prolyl-4-hydroxylase domain (PHD) proteins, members of the 2-oxoglutarate/iron dependent dioxygenase superfamily. These proteins hydroxylate specific prolyl residues in the oxygen-dependent degradation domain (ODD) of HIF-α subunits. The hydroxylated proteins are bound by the ubiquitin ligase, von Hippel-Lindau tumor suppressor protein (pVHL) which targets them for rapid ubiquitination and 26S proteasomal degradation (11). Members of the PHD family that include PHD1, PHD2 and PHD3 are widely expressed in tissues and exhibit a tissue-specific expression pattern (12, 13, 14). Since the activity of PHDs depends on the tissue oxygen tension, these molecules serve as oxygen-sensors that control the cellular abundance of HIF proteins. Noteworthy, their expression and function in mediating HIF homeostasis in the intervertebral disc is unknown.
A considerable number of studies clearly show that in cells of the nucleus pulposus there is robust HIF expression even under normoxic culture conditions. The response is evident across species, it is seen in vivo and in vitro, and more importantly, HIF-1α expression is not induced under hypoxia (5, 15, 16). Accordingly, when compared with most other tissues, there are substantive underlying differences in the HIF status and reactivity of disc cells: HIF-1α expression and activity is always ‘on’. This unusual response suggests that maintenance of steady state levels of HIF-1α in cells of the nucleus pulposus ensures that its transcriptional activity is a major determinant of cell function. Like HIF-1α, protein level of HIF-2α is similar in both hypoxia and normoxia, suggesting that its levels are tightly controlled (17). Whether this unique stabilization of HIF-α subunits in nucleus pulposus cells is achieved through low activity and or expression of one or more of the PHDs is not known (18). Moreover, whether maintenance of constant levels of HIF-1α and HIF-2α in the disc is an adaptive response to an imposed metabolic need, related to the unique embryonic origins of the disc, is a matter of considerable interest. A steady state HIF-1/-2 expression that is oxygen independent is likely to maintain cell metabolism and survival activities even during oxemic shifts that occur when the tissue integrity is breached at an early stage of degeneration or during disc herniation or (19, 20).
The major objective of the study is to determine the mechanisms of HIF-1α and HIF-2α degradation in nucleus pulposus cells and to investigate if PHDs are involved in this process. We show for the first time that in nucleus pulposus cells known to exhibit stabilized expression HIF-1α in normoxia (15, 16), among all PHDs, only PHD2 controls limited HIF-1α degradation in oxygen-dependent manner, while the turnover of HIF-2α is largely independent of PHD activity. Our findings suggest that the cells of nucleus pulposus are functionally adapted to their avascular, hypoxic microenvironment and rely primarily on oxygen independent pathways for precisely controlling HIF-1α and HIF-2α protein levels.
MATERIALS AND METHODS
Plasmids and Reagents
Plasmids were kindly provided by Dr. Greg Semenza, Johns Hopkins University [enolase1 reporter], Dr. Joseph Garcia, Southwestern Medical Center, Dallas [SOD2 and Frataxin reporter] (17), Dr. Nianli Sang [pcDNA3.1-PHD1, -PHD2, -PHD3], Dr. Dorthe Katschinski, Georg-August University, Gottingen [HIF-2α aa 405-568, HIF-2α aa 405-568 P405/531A and pGREx5E1bLuc] (21). Cited2 reporter (-2186/+65) originally constructed by Dr. Shoumo Bhattacharya was provided by Dr. Olga Aprelikova, NIH (17). VEGF reporter (pVEGF-KpnI from –2274/+379) was purchased from ATCC (Manassas, VA) (17). HIF-1α-ODD-LuciferasepcDNA3 (catalog #18965), developed by Dr. William G. Kaelin and psPAX2 (catalog # 12260) and pMD2 (catalog # 12259) by Didier Trono were obtained from Addgene. Lentiviral ShPHD2 and ShPHD3 constructs were from Dr. Kenneth Thirstrup, Sweden (22). As an internal transfection control, vector pRL-TK (Promega) containing Renilla reniformis luciferase gene was used. The amount of transfected plasmid, the pre-transfection period after seeding, and the post-transfection period before harvesting, have been optimized for rat nucleus pulposus cells using pSV β-galactosidase plasmid (Promega) (17).
Isolation of nucleus pulposus cells and treatments of cells
Rat nucleus pulposus cells were isolated using a method reported earlier by Risbud et al. (15). Nucleus pulposus cells and human chondrocytes line T/C28 (kindly provided by Dr. Mary Goldring) were maintained in Dulbeccos Modified Eagles Medium (DMEM) and 10% fetal bovine serum (FBS) supplemented with antibiotics. Several studies have shown that T/C28 line employ identical signaling pathways and respond to environmental stimuli in a similar fashion as primary human chondrocytes and therefore is a good representation of human chondrocytes behavior in vitro (23, 24). Cells were cultured in a Hypoxia Work Station (Invivo2 300, Ruskinn, UK) with a mixture of 1% O2, 5% CO2 and 94% N2 for 8-24 h. In some experiments cells were treated with 10 μM MG132 or 1 mM dimethyl oxalyl glycine (DMOG) or 25 μM BiPS or 50 nM bafilomycin A1 or 50 μM chloroquine for 4-24 h.
Transfections and dual luciferase assay
Cells were transferred to 24-well plates at a density of 4 × 104 cells/well one day before transfection. To investigate the effect of PHD overexpression on HIF-1α-ODD stability or activity of different HRE reporters, cells were cotransfected with 100-300 ng of PHD1-3 or pHsH1-ShPHD2/3 or backbone vector pcDNA3.1 or pHsH1-CMV-EGFP with 400 ng reporter and 300 ng pRL-TK plasmid. For HIF-2α-ODD, cells were cotransfected with 100 ng of HIF-2α aa 405-568 or HIF-2α aa 405-568 P405/531A, 100 ng of pGREx5E1bLuc and 500 ng of pRL-TK plasmid. LipofectAMINE 2000 (Invitrogen) was used as a transfection reagent. For each transfection, plasmids were premixed with the transfection reagent. For measuring the effect of DMOG or MG132 on HIF-1αODD or HRE reporter activity, 24 h after transfection, the cells in some wells were treated with MG132 (10μM) or DMOG (1 mM) or BiPS (25 μM). The next day, the cells were harvested and a Dual-Luciferase™ reporter assay system (Promega) was used for sequential measurements of firefly and Renilla luciferase activities. Quantification of luciferase activities and calculation of relative ratios were carried out using a luminometer (TD-20/20, Turner Designs, CA). At least three independent transfections were performed, and all analyses were carried out in triplicate.
Real time RT-PCR analysis
Total RNA was extracted from rat nucleus pulposus cells or tissues using RNAeasy mini columns (Qiagen). Before elution from the column, RNA was treated with RNase free DNAse I (Qiagen). The purified, DNA-free RNA was converted to cDNA using Superscript III Reverse Transcriptase (Invitrogen). Reactions were set up in triplicate in 96 well plate using 1 μl cDNA with SYBR Green PCR Master Mix (Applied Biosystems) to which gene-specific forward and reverse PCR primers were added (see supplementary Table I, synthesized by Integrated DNA Technologies, Inc.). PCR reactions were performed in a StepOnePlus real time PCR system (Applied Biosystems) according to the manufacturer's instructions. β-actin was used to normalize. Melting curves were analyzed to verify the specificity of the RT-PCR reaction and the absence of primer dimer formation.
Immunofluorescence microscopy
Cells were plated in flat bottom 96 well plates (5 × 103/ well) for 24 h. In some experiments cells were transduced with lentival particles expressing ShPHD2 and ShPHD3 for 72-96 h. After treatment, cells were fixed with 4% paraformaldehyde, permeabilized with 0.2% triton-X 100 in PBS for 10 min, blocked with PBS containing 5% FBS, and imaged using a laser scanning confocal microscope (Olympus Fluoview, Japan).
Protein extraction and Western blotting
Cells were placed on ice immediately following treatment and washed with ice-cold HBSS. Nuclear and cytosolic proteins were prepared using the CellLytic NuCLEAR extraction kit (Sigma-Aldrich, St. Louis). All the wash buffers and final re-suspension buffer included 1X protease inhibitor cocktail (Pierce, IL), NaF (5 mM) and Na3VO4 (200 μM). Nuclear or total cell proteins were resolved on 8-12 % SDS-polyacrylamide gels and transferred by electroblotting to nitrocellulose membranes (Bio-Rad, CA). The membranes were blocked with 5% non-fat dry milk in TBST (50 mM Tris, pH 7.6, 150 mM NaCl, 0.1% tween 20) and incubated overnight at 4 °C in 3% non-fat dry milk in TBST with the anti-HIF-1α or anti-HIF-2α (1:1000, R&D), HIF-1β (1:1000, BD Biosiences), anti-PHD1 or anti-PHD2 or anti-PHD3 antibody (1:1000, Novus), anti-β-tubulin (1:3000, Developmental Studies Hybridoma Bank) and anti-Lamin A/C (1:1000, Cell Signaling). Immunolabeling was detected using the ECL reagent (Amersham Biosciences). Relative expression levels were determined by quantitative densitometric analysis using 1D image analysis software (Quantity One, BIO-RAD).
Lentiviral production and transduction
A lentiviral transfer vector based on pHsCXW that permits co-expression of EGFP and PHD2/3 shRNA under the control of CMV and human H1 promoters respectively was used to knockdown of PHD2 and PHD3 expression in rat nucleus pulposus cells (22). A scrambled sequence cloned in same vector was use as a negative control. Lentiviral particles were produced in HEK293 cells by co-transfecting lentiviral transfer vector with packaging and envelop vectors, psPAX2 and pMD2 using Lipfectamine 2000. To achieve robust knockdown, nucleus pulposus cells plated in 10 cm plate (1×106) were transduced with recombinant viral particles 5 days prior to measurement of protein levels. A transduction efficiency of 80–90% was achieved as determined from the number of GFP positive cells.
Statistical analysis
All measurements were performed in triplicate, data is presented as mean ± S.E. Differences between groups were analyzed by the student t test; *p< 0.05.
RESULTS
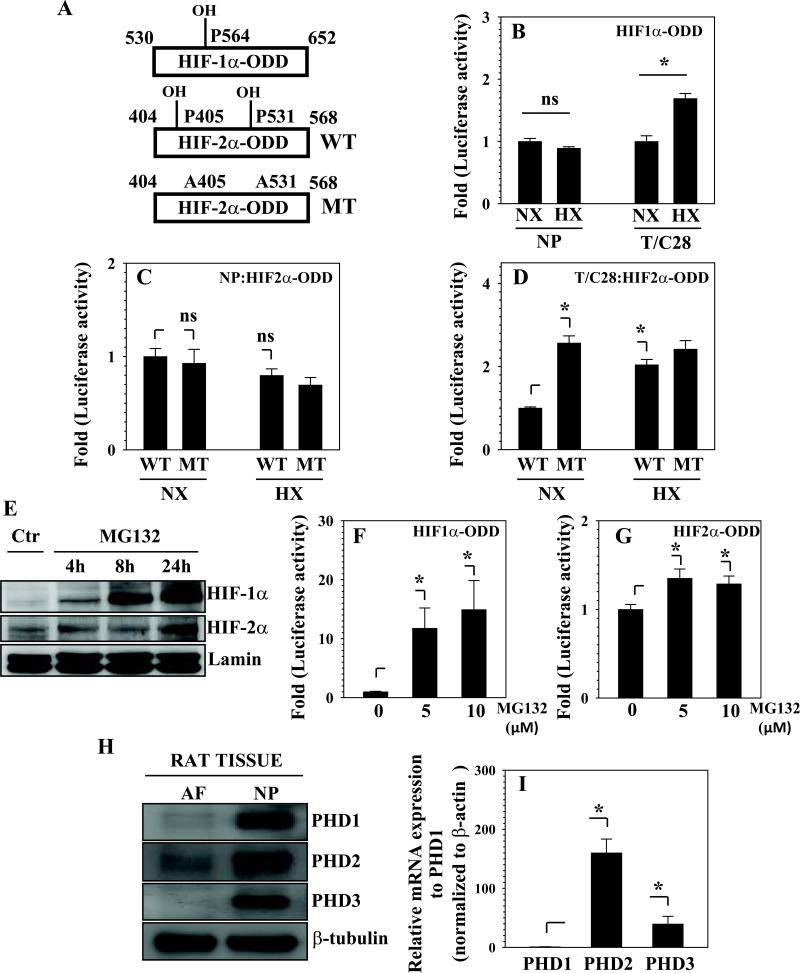
To study the effect of oxygen tension on degradation of HIF-α homologs in nucleus pulposus cells, we measured the stability of transfected HIF-1α-ODD and HIF-2α-ODD. Hydroxylated HIF-1α-ODD on proline residue 564 and HIF-2α-ODD on proline residues 405 and 531 (Fig. 1A) promotes their degradation by 26S proteasome pathway. As expected, in T/C-28 chondrocytes, hypoxia significantly increases stability of HIF-1α-ODD, while in nucleus pulposus cells, there was no difference in ODD stability between normoxic and hypoxic conditions (Fig. 1B). Noteworthy, in nucleus pulposus cells, mutation of both the proline residues (P405 and P531) of HIF-2α-ODD did not result in increased stabilization in normoxia, neither there was a difference between normoxic and hypoxic stability of either wild type or mutant ODD (Fig. 1C). In contrast, in chondrocytes, proline mutations of HIF-2α-ODD resulted in increased stability than the wild type-ODD in normoxia. Moreover, compared to normoxia wild type-ODD was also more stable in hypoxia, while stability of mutant-ODD was similar to its normoxic levels (Fig. 1D). Next, to determine whether the ubiquitin–proteasome pathway plays a role in degradation of HIF-α in nucleus pulposus cells, we evaluated the effect of 26S proteasome inhibitor, MG132 on the accumulation of HIF-1α and HIF-2α. This inhibitor caused a robust accumulation of endogenous HIF-1α as early as 4 h, whereas effect on HIF-2α is much smaller and delayed (Fig. 1E). Furthermore, we assessed the effect of MG132 on the stability of HIF-α-ODD by measuring the levels of HIF-1α- or HIF-2α-ODD. As shown in Fig. 1F, following the treatment with MG132, the stability of HIF-1α-ODD is dramatically increased. On the other hand, HIF-2α-ODD exhibits a much small but significant increase in accumulation in treated cells (Fig. 1G).
Fig. 1.
Involvement of 26S proteasomal pathway in HIF-1α and HIF-2α degradation in nucleus pulposus (NP) cells. (A) Schematic of HIF-1α-ODD and HIF-2α-ODD reporters used for transfections. Hydroxylation of specific proline residues in ODD promotes degradation. Change from proline to alanine (P405/531A: MT) abolishes hydroxylation and blocks degradation. Evaluation of HIF-1α-ODD (B) and HIF-2α-ODD (C, D) stabilization in NP and T/C28 chondrocytes cultured under normoxia and hypoxia. The activity of both HIF-1α-ODD and HIF-2α-ODD was induced by hypoxia in T/C28 cells, but remained constant in NP cells. In NP cells, stability of MT-HIF-2α-ODD was similar to WT-ODD in normoxia, while in chondrocytes, MTODD was more stable in normoxia. (E) Western blot analysis of nuclear proteins of NP cells treated with MG132 for 4-24 h. MG132 treatment resulted in a robust accumulation of HIF-1α, much smaller effect on HIF-2α was seen. (F, G) Effect of the proteosome inhibitor, MG132 on HIF-α-ODD stabilization. (F) Following treatment with the inhibitor, a dose dependent increase in HIF-1α-ODD stability is seen. (G) A small but significant increase in stability of HIF-2α-ODD was also observed. (H) Western blot analysis of PHDs in annulus fibrosus (AF) and NP tissues. All PHD isoforms were expressed at a higher level in NP tissue. (I) Real-time RT-PCR analysis of PHDs in NP tissue. Note that PHD2 had the highest relative expression, while PHD1 expression was the least. Data is represented as mean ± SE of three independent experiments performed in triplicate (n=3); *p< 0.05; ns, not significant.
We then evaluated if PHD isoforms that control HIF-α hydroxylation and subsequent degradation are expressed by the nucleus pulposus cells. Western blot analysis of the rat nucleus pulposus and annulus fibrosus tissues indicate that the expression of PHD1, PHD2 and PHD3 is greater in nucleus pulposus than in annulus fibrosus tissue (Fig. 1H). Moreover, real time RT-PCR analysis indicates that PHD2 is the most predominant isoform in nucleus pulposus tissue. In contrast, baseline expression of PHD1 is very low (Fig. 1I).
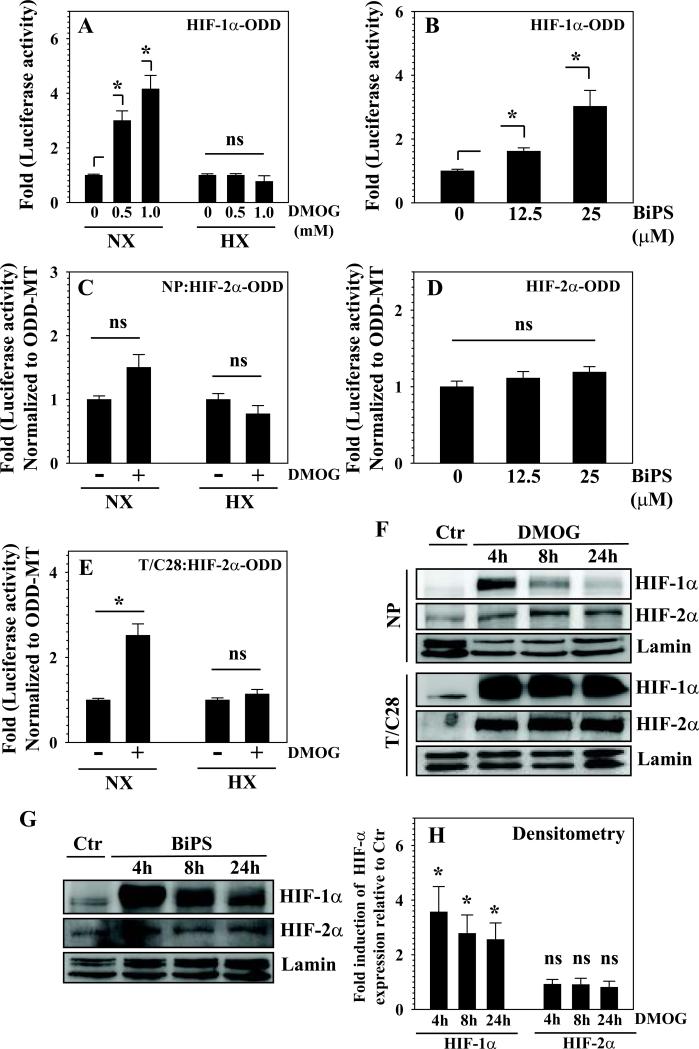
To investigate the role of PHDs in HIF degradation in nucleus pulposus cells, we evaluated the effect of dimethyl-2-oxoglutarate (DMOG) and BiPS, prolyl-hydroxylase inhibitors on the stability of HIF-α-ODD. Figure 2A and B show that the stability of HIF-1α-ODD is significantly increased by treatment with both DMOG and BiPS in a dose-dependent manner. Importantly, positive effect of DMOG on stability of HIF-1α-ODD was absent in hypoxia (Fig. 2A). A similar response to DMOG treatment is observed in chondrocytes (not shown). To validate the effect of these inhibitors on HIF-2α stability and requirement of proline hydroxylation for degradation, we measured effect of DMOG and BiPS on the stability of wild type and mutant HIF-2α-ODD. In contrast to HIF-1α-ODD, in nucleus pulposus cells these inhibitors have no effect on the stability of HIF-2α-ODD under normoxic conditions (Fig. 2C, D). Noteworthy, chondrocytes show increased stability of HIF-2α-ODD following DMOG treatment in normoxia (Fig. 2E). Figure 2F and G shows the effect of these inhibitors on the stability of HIF-1α and HIF-2α subunits by Western blot. There is a rapid accumulation of HIF-1α following treatment with both DMOG and BiPs, levels remained high till 24 h. On the other hand, there is no significant increase in accumulation of HIF-2α following the treatment with both DMOG and BiPS. As expected, chondrocytes exhibit robust accumulation of both HIF-1α and HIF-2α by DMOG (Fig. 2F). Densitometric analysis of multiple Western blots confirmed that in nucleus pulposus cells, the accumulation of HIF-1α is significantly increased by DMOG, while HIF-2α is unaffected (Fig. 2H).
Fig. 2.
Effect of PHD inhibition on the HIF-1α and HIF-2α degradation in NP cells and B) NP cells were transfected with HIF-1α-ODD reporter, and luciferase activity was measured 24 h following treatment with PHD inhibitors DMOG (A) and BiPS (B). Both inhibitors show a significant stabilization of HIF-1α-ODD in a dose dependent manner. (C and D) Effect of DMOG (C) and BiPs (D) on NP cells transfected with a wild type (WT) or a mutant (P405/531A; MT) HIF-2α-ODD reporter. There is no change in stability of either WT-ODD or MT-ODD following the treatment with DMOG and BiPS in normoxia and hypoxia. (E) T/C28 chondrocytes show increased stability of WT-ODD after DMOG treatment, effect on stability is lost in hypoxia. (F) Western blot analysis of NP and chondrocytes treated with DMOG. In NP, treatment resulted in a robust accumulation of HIF-1α while HIF-2α levels were unaffected. Chondrocytes showed a much higher accumulation in both HIF-1α and HIF-2α. (G) Western blot analysis of NP cells treated with BiPS showed a robust accumulation of HIF-1α as early as 4 h. HIF-2α levels were unaffected by the inhibitor treatment. (H) Multiple blots were quantified by densitometric analysis. Lamin A/C expression was used as a loading control and to calculate relative expression levels. DMOG treatment significantly increased HIF-1α accumulation, while HIF-2α levels remained constant. Data is represented as mean ± SE of three independent experiments performed in triplicate (n=3); *p< 0.05; ns, not significant.
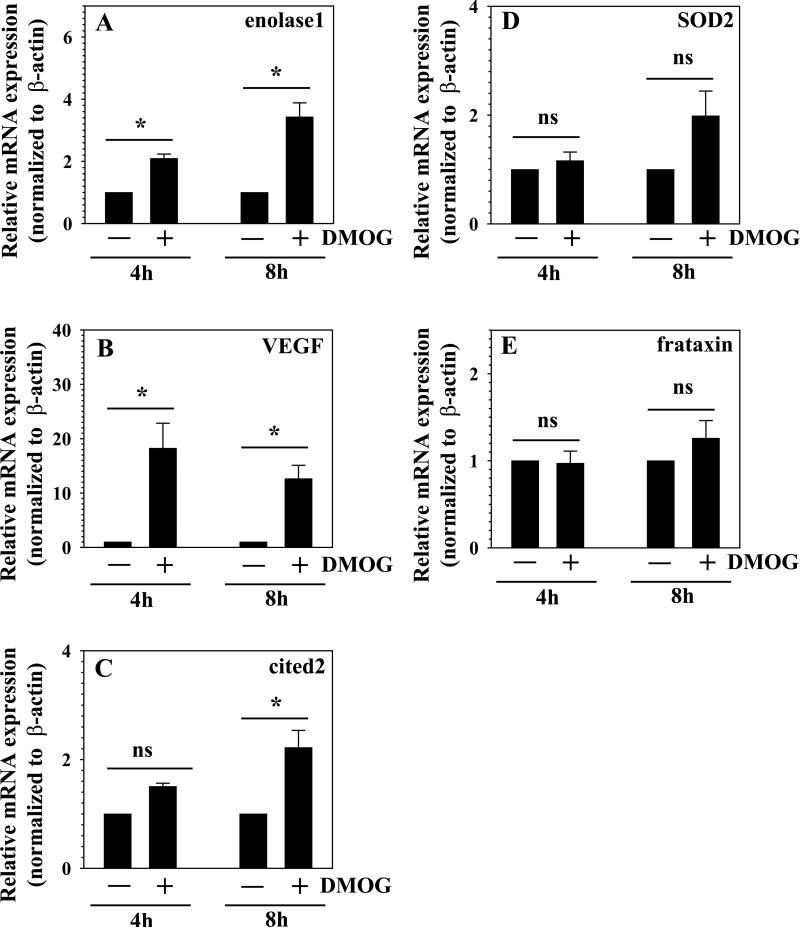
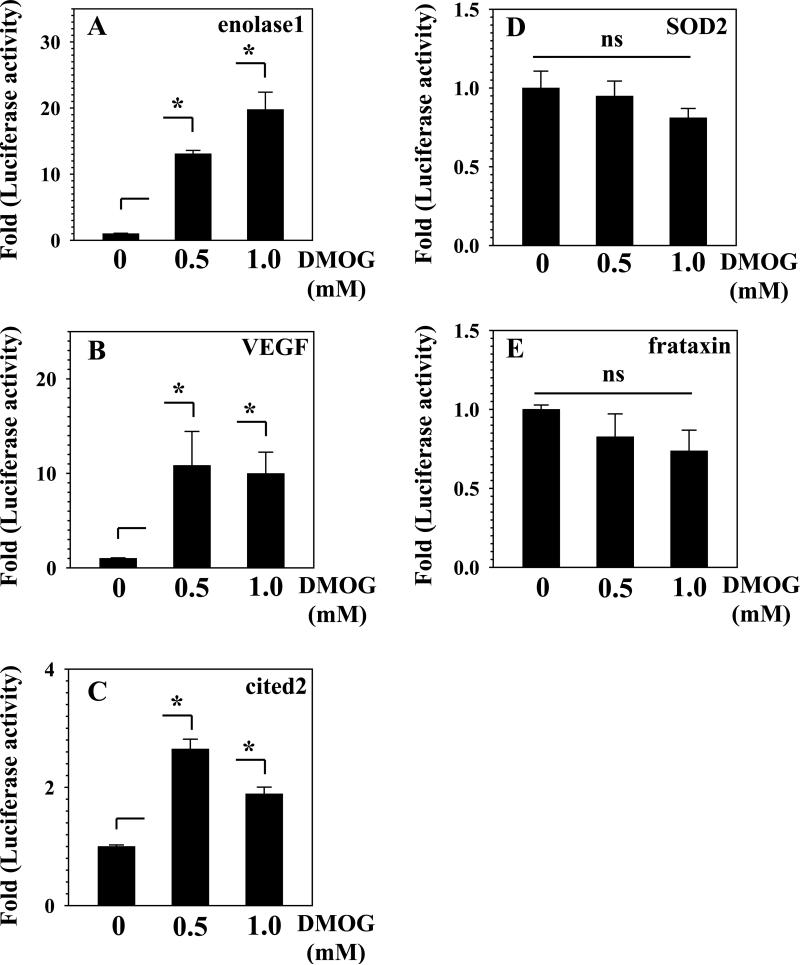
To further evaluate the transcriptional activity of HIF-1 and HIF-2, we examined the effect of DMOG treatment on mRNA expression of HIF-1 and HIF-2 target genes. Figure 3A, B shows that the mRNA expression of enolase1, VEGF is strongly induced by the treatment with DMOG. Induction in enolase-1 and VEGF is more pronounced than cited2, which shows increase in expression only after 8 h of treatment (Fig. 3C). Unlike HIF-1 target genes, the mRNA expression of HIF-2 target genes, SOD2 and frataxin is not significantly affected after DMOG treatment (Fig. 3D and E). In addition to mRNA expression analysis, we measured the effect of DMOG on the promoter activities of the respective target genes. As expected, the reporter activity of enolase1 (Fig. 4A) and VEGF (Fig. 4B) is strongly induced (about 10-20 fold), while cited2 elicits a 2-3 fold induction (Fig. 4C). In contrast, the promoter activities of both SOD2 (Fig. 4D) and frataxin (Fig. 4E), classical HIF-2 target genes, are not induced by DMOG treatment.
Fig. 3.
The effect of PHD inhibition on mRNA expression of HIF target genes in NP cells. Real-time RT-PCR analysis of HIF-1 and HIF-2 target genes, (A) enolase1, (B) VEGF, (C) cited2, (D) SOD2 and (E) frataxin in NP cells treated with DMOG. Expression of enolase1 and VEGF is robustly induced by DMOG treatment at all the time points, induction in cited2 expression is delayed and begins at 8 h. SOD2 and frataxin expression is not affected following treatment with DMOG. Data represent mean ± SE of three independent experiments performed in triplicate (n=3); *p< 0.05; ns, not significant.
Fig. 4.
The effect of PHD inhibition on promoter activity of HIF target genes in NP cells. Reporter plasmids of HIF-1 target genes (A) enolase1, (B) VEGF, (C) cited2, (D) SOD2 and (E) frataxin were transfected into NP cells and luciferase activity was measured following 24 h treatment with DMOG. Note that the reporter activity of enolase1, VEGF and cited2 was increased by the treatment with DMOG. In contrast, SOD2 and frataxin promoter activities were not influenced by the treatment. Data is represented as mean ± SE of three independent experiments performed in triplicate (n=3); *p< 0.05; ns, not significant.
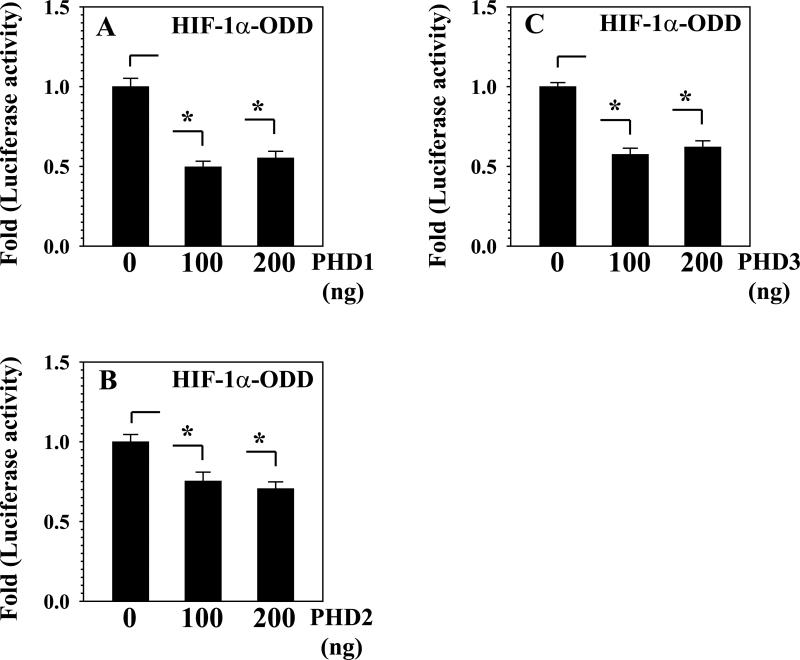
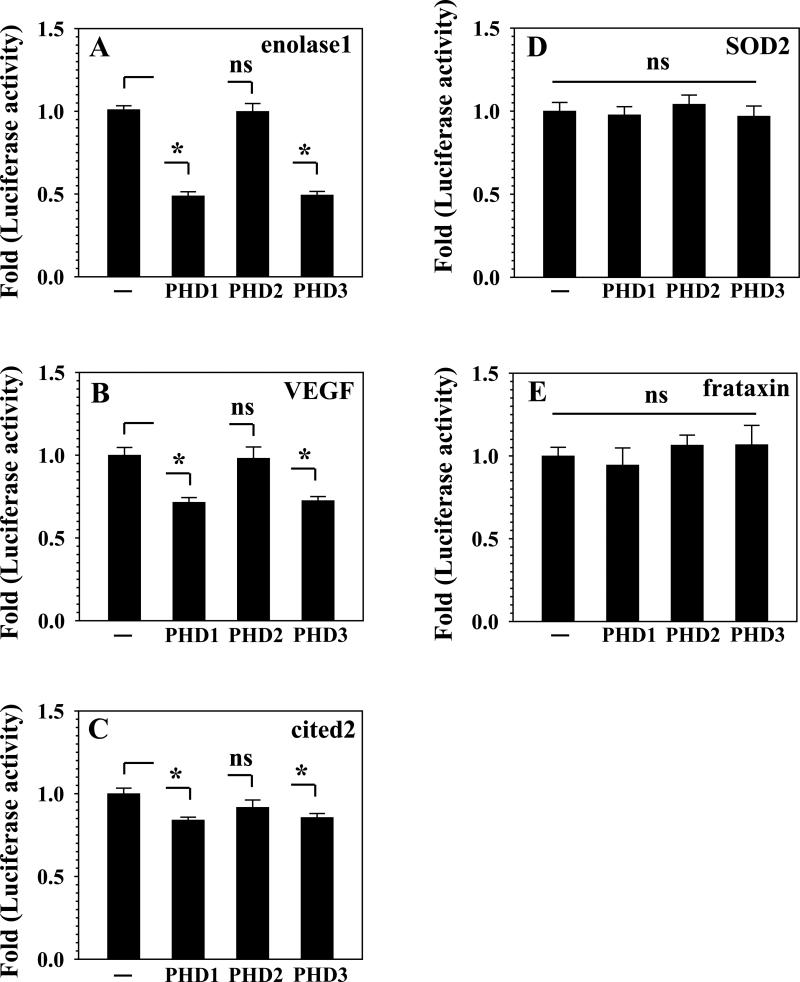
To investigate if PHD function is limited by substrate and co-factor availability in the nucleus pulposus cells, we transfected cells with plasmids encoding PHD1 (Fig. 5A), PHD2 (Fig. 5B) and PHD3 (Fig. 5C) and measured the stability of HIF-1α-ODD. Figure 5 shows that all the PHD isoforms promote the degradation of HIF-1α-ODD. We further evaluated the effect of individual PHD overexpression on the transcriptional activity of endogenous HIF-1α and HIF-2α protein in nucleus pulposus cells. The promoter activities of enolase1 (Fig. 6A), VEGF (Fig. 6B) and cited2 (Fig. 6C) are significantly suppressed by PHD1 and PHD3 overexpression. However, surprisingly, PHD2 overexpression did not affect the activity of any of the HIF-1 target gene promoters (Fig. 6A-C). Next, we evaluated the effect of individual PHD on HIF-2α responsive reporter activity. Again, the promoter activities of either SOD2 (Fig. 6D) or frataxin (Fig. 6E) are not affected by PHD overexpression.
Fig. 5.
PHD function in NP cells is not limited by substrate availability. (A, B and C) NP cells were co-transfected with HIF-1α-ODD reporter along with expression vectors of (A) PHD1 or (B) PHD2, or (C) PHD3 and/or empty backbone vector pcDNA3.1. Note that exogenously expressed PHDs can hydroxylate and decrease the stability of HIF-1α-ODD. Data represent mean ± SE of three independent experiments performed in triplicate (n=3); *p< 0.05; ns, not significant.
Fig. 6.
Effect of individual PHDs on the promoter activity of HIF target genes in NP cells. NP cells were co-transfected with (A) enolase1, (B) VEGF, (C) cited2, (D) SOD2 and (E) frataxin promoter constructs along with expression vectors for PHD1, PHD2 and PHD3 and/or empty backbone vector. Note that the activity of enolase1, VEGF and cited2 promoter was significantly suppressed by overexpression of PHD1 and PHD3, but not PHD2. Promoter activity of SOD2 and frataxin was not unaffected by the overexpression of PHD1, PHD2 and PHD3. Data represent mean ± SE of three independent experiments performed in triplicate (n=3); *p< 0.05; ns, not significant.
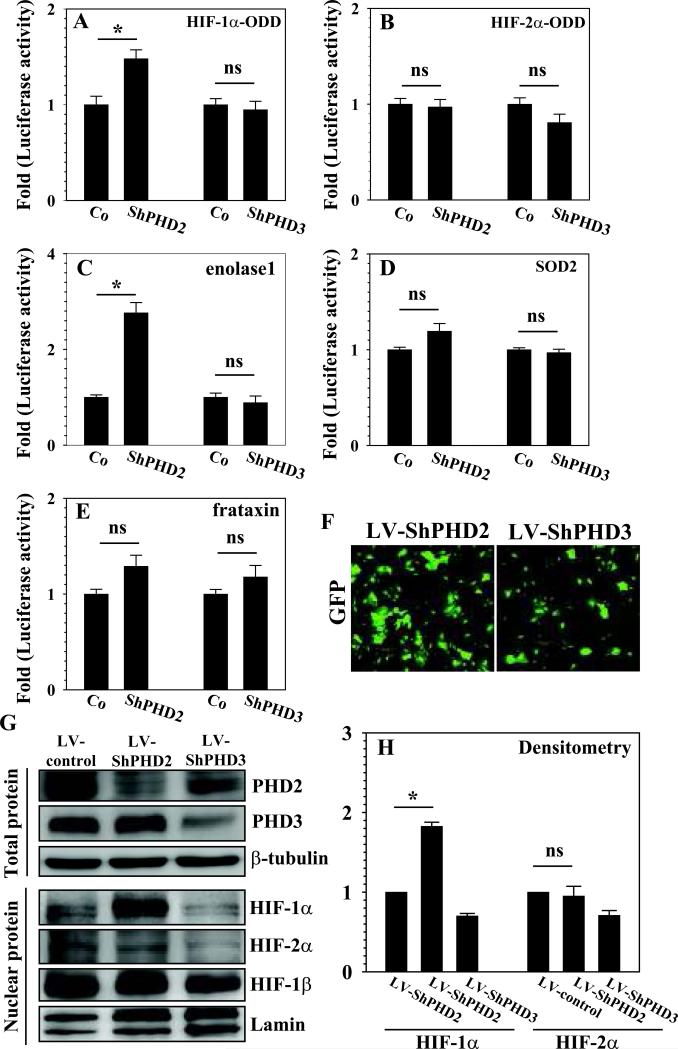
To further evaluate the role of PHD2 and PHD3 in degradation HIF in nucleus pulposus cells, we suppressed the expression of PHD2 and PHD3 using shRNAs under normoxic conditions. Nucleus pulposus cells transfected with shPHD2 exhibit a small, but significant increase in stabilization of HIF-1α-ODD, whereas its stability is not affected by suppression of PHD3 (Fig. 7A). On the other hand, the stability of HIF-2α-ODD is not significantly affected by silencing of either PHD2 or PHD3 (Fig. 7B). Nucleus pulposus cells transfected with ShPHD2 but not ShPHD3 also evidence induction in enolase1 promoter activity (Fig. 7C). To assess the effect of silencing of PHD2 and PHD3 on HIF-2α transcriptional activity, we measured the promoter activity of target genes, SOD2 and frataxin in silenced nucleus pulposus cells. Neither SOD2 nor frataxin promoter activities are not significantly changed by silencing either PHD2 or PHD3 (Fig. 7D and E).
Fig. 7.
Effect of PHD2 and PHD3 silencing on the stability of HIF-1α and HIF-2α in NP cells. Cells were co-transfected with plasmids encoding ShPHD2 or ShPHD3 or their respective control shRNA (Co) along with (A) HIF-1α-ODD or (B) HIF-2α-ODD or the reporters (C) enolase1, or (D) SOD2 or (E) frataxin. Silencing of PHD2 resulted in a significant increase in stability of HIF-1α-ODD. Silencing of PHD3 had no effect on the HIF-1α-ODD stability. (B) The stability of HIF-2α-ODD was not affected by silencing of either PHD2 or PHD3. (C-E) The promoter activity of (C) enolase1 but not (D) SOD2 or (E) frataxin was significantly induced by silencing of PHD2. PHD3 silencing had no effect on activity of any of the reporters. (F) Immunofluorescence analysis of GFP in NP cells transduced with lentivirus co-expressing GFP and shRNA of either PHD2 (LV-ShPHD2) or PHD3 (LV-ShPHD3) shows high transduction efficiency. Magnification X20. (G) Western blot analysis of cells transduced with LVShPHD2/3. The expression of PHD2 or PHD3 was suppressed by respective ShRNAs compared with cells transduced with control lentivirus (LV-control). Note that accumulation of HIF-1α was seen in PHD2, but not PHD3 silenced cells. Accumulation of HIF-2α was not affected by silencing of either PHD2 or PHD3. (H) Densitometric analysis of multiple blots from experiment described in G above. Relative HIF-1α level compared to LV-control was significantly increased with LV-ShPHD2, but not LV-ShPHD3. Relative HIF-2α level was not affected by either LV-ShPHD2 and LV-ShPHD3. Data is represented as mean ± SE of three independent experiments performed in triplicate (n=3); *p< 0.05; ns, not significant.
To measure the effect of stable silencing of PHD2 and PHD3 on HIF-1α and HIF-2α protein levels, we used lentivirus mediated shRNA transduction of nucleus pulposus cells. Assessment of GFP positive cells, confirmed that the transduction efficiency was more than 80% (Fig. 7F). Western blot analysis confirms that the shRNAs suppress the expression of PHD2 or PHD3 respectively. Figure 7G shows that silencing of PHD2, but not PHD3, results in increased accumulation of HIF-1α, while HIF-2α stability is unaffected by either PHD2 or PHD3 suppression (Fig. 7G). Densitometric analysis confirms that silencing of PHD2, but not PHD3, significantly increases the accumulation of HIF-1α, while the accumulation HIF-2α is not affected by silencing of both PHD2 and PHD3 (Fig. 7H).
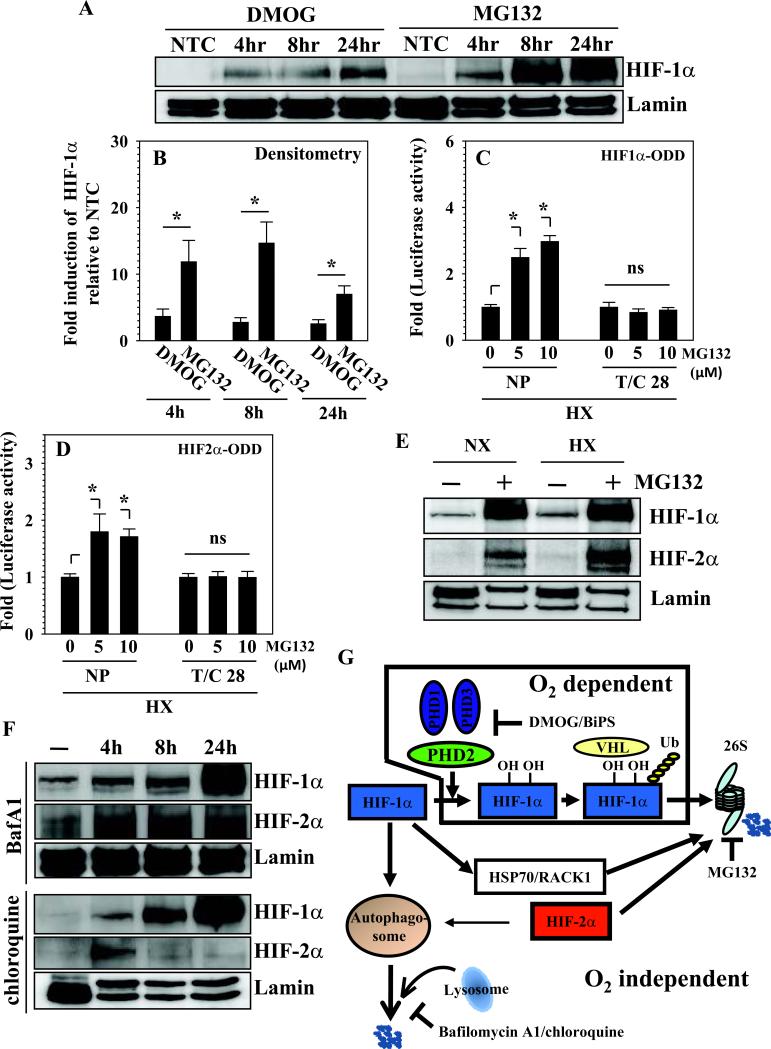
To investigate if proteasomal degradation of HIF-1α was predominantly through an oxygen-dependent PHD pathway, we compared accumulation in HIF-1α protein levels following treatment with DMOG and MG132. The concentrations of inhibitors were chosen such that they result in complete inhibition of the respective pathways. Following treatment with both inhibitors, equivalent amounts of protein were loaded on the same gel and Western blot analysis for HIF-1α was performed. Figure 8A and B shows that the accumulation of HIF-1α by MG132 is significantly higher than cells treated with DMOG. Moreover, to evaluate if 26S proteasome also mediates HIF-α degradation under hypoxic conditions, we treated nucleus pulposus cells maintained at 1% O2 with MG132 and measured stability of HIF-1α- and HIF-2α-ODD. Figure 8C and D clearly shows that even under hypoxia, MG132 increased stability of both HIF-1α and HIF-2α-ODD. In contrast, under hypoxic conditions in chondrocytes, stability of both HIF-α homologues remained unaffected. Western blot analysis showed a robust accumulation of HIF-1αin MG132 treated cells even in hypoxia, accumulation of HIF-2α was also pronounced (Fig. 8E). To determine if ubiquitin independent mechanisms of HIF-α degradation were active in nucleus pulposus cells, we treated cells with bafilomycin A1 and chloroquine, inhibitors of protein degradation through the lysosomal pathway. Figure 8F shows that treatment with bafilomycin A1 and chloroquine results accumulation of HIF-1α as early as 4 h. By 24 h a substantial accumulation of HIF-1α is seen in these inhibitor-treated nucleus pulposus cells. Compared to HIF-1α, accumulation of HIF-2α in inhibitor treated nucleus pulposus cells was less pronounced.
Fig. 8.
HIF-1/2α degradation is controlled by oxygen-independent proteasomal and lysosomal pathways in NP cells. (A) Simultaneous analysis of HIF-1α levels in NP cells treated with DMOG or MG132 at a concentration that completely inhibits PHD or 26S proteasome function respectively. Note that HIF-1α accumulation is higher in MG132 than DMOG treated cells. (B) Densitometric analysis of multiple blots from the experiment described in (A) above. Fold accumulation of HIF-1α was significantly higher in MG132 compared to DMOG treated cells. Data represent mean ± SE of three independent experiments (n=3); *p< 0.05; ns, not significant. (C, D) Effect of the proteosome inhibitor, MG132 on HIF-α-ODD stability in hypoxia. (C) Unlike chondrocytes, following treatment with the inhibitor, a dose dependent increase in HIF-1α-ODD stability is seen in NP. (D) A significant increase in hypoxic stability of HIF-2α-ODD was also observed only in NP cells. (E) Western blot analysis of HIF-1α and HIF-2α expression in NP cells treated with MG132 under hypoxia. Similar to normoxic group, MG132 treatment in hypoxia also resulted in a robust accumulation of HIF-1α as well as HIF-2α. (F) Western blot analysis of HIF-1α and HIF-2α in NP cells treated with bafilomycin A1 (BafA1) and chloroquine for 4-24 h. BafA1 and chloroquine treated cells showed accumulation of HIF-1α as early as 4 h, a robust accumulation was seen 24 h following the treatment. HIF-2α also showed increased accumulation in treated cells. (G) A schematic model of the unique regulation of HIF-1α and HIF-2α degradation in NP cells. PHD2 controls a limited oxygen dependent degradation of HIF-1α through 26S proteasome pathway. Oxygen-independent mechanisms through 26S proteasome as well as lysosomal pathway are active in HIF-1α turnover. In contrast, HIF-2α is unresponsive to oxidative degradation and is also turned over though 26S and lysosomal pathway.
DISCUSSION
The mechanisms by which the cells of the nucleus pulposus survive in the hypoxic environment of the intervertebral disc are not fully understood. We previously reported that HIF-1α and HIF-2α are expressed in nucleus pulposus cells and played an important role in regulating energy metabolism and matrix synthesis (15-17). Importantly, unlike most other cell types, both homologs were stabilized under normoxic condition as well as maintained a steady state level that was independent of oxemic tension (15-17). In supporting these previous observations, our results clearly showed that in nucleus pulposus cells, stability of HIF-1α-ODD and HIF-2α-ODD is independent of oxemic tension. Moreover, absence of increased stability of HIF-2α-ODD containing proline to alanine at positions 405 and 531 suggests that hydroxylation reaction may not control HIF-2α degradation in these cells (21). Again these findings are different than T/C28 cells and human primary articular chondrocytes that exhibit responsiveness of HIF-2α degradation to PHD function in vitro suggesting a cell type specific response (25). In light of these observations, it was important to understand how HIF-α levels were maintained in the nucleus pulposus cells. We found that both HIF-1α and HIF-2α were degraded through the 26S proteasome pathway. Since all PHDs mediate proteasomal HIF-α degradation but differ in their ability to hydroxylate HIF-1α in vivo, we investigated their individual role in HIF-α turnover in nucleus pulposus cells (26, 27). The high relative expression of PHD2 in nucleus pulposus tissue suggests that this isoform may play an important role in HIF-α turnover. However, surprisingly our results indicate that PHD2 controls to a limited extent HIF-1α degradation and thus not a major regulator of HIF-1α turnover. Moreover, results suggest that HIF-1α levels are regulated primarily by oxygen-independent proteasomal and lysosomal pathways. In contrast to HIF-1α, the turnover of HIF-2α through 26S proteasome is largely independent of PHD function, there is also a limited involvement of lysosomal pathway. These findings strongly suggest that nucleus pulposus cells are functionally adapted to their avascular, hypoxic microenvironment and rely mostly on oxygen independent pathways for controlling HIF-1α and HIF-2α levels. Our results provides a rationale for normoxic stabilization and maintenance of steady state levels of these proteins in the nucleus pulposus.
Noteworthy, the higher expression of PHDs in nucleus pulposus compared to annulus fibrosus may reflect the different embryological origins of these cells and their function. Moreover, since PHD2 and PHD3 expression is known to be sensitive to hypoxia, in nucleus pulposus tissue, their expression would be expected to be enhanced in comparison to the annulus fibrosus (28, 29). Studies aimed at determining the function of PHDs in nucleus pulposus cells revealed a unique pattern of HIF-α regulation. When PHD function was inhibited by DMOG, HIF-1α protein levels were modestly increased suggesting that the PHDs participated in HIF-1α turnover. In contrast, lack of HIF-2α accumulation indicated that the PHDs played a very limited role in the turnover of this homologue. The differences are striking when compared to DMOG dependent HIF-1/2α accumulation in chondrocytes. Measurement of the stability of HIF-α-ODD in cells validated these results again indicating lack of PHD involvement in controlling HIF-2α turnover in nucleus pulposus. Moreover, the notion that in nucleus pulposus cells the PHD dependent hydroxylation of proline resides 405 and 531 in HIF-2α-ODD was not required for degradation was further strengthened by studies of mutant-ODD. Lack of induction of SOD2 and frataxin mRNA and activity of promoters that contain HIF-2 responsive HRE motif/s by DMOG suggested that PHDs played very limited role in controlling HIF-2 transcriptional activity. With respect to HIF-1, a strong induction in expression of the target genes enolase1 and VEGF lend support to the role of PHDs in HIF-1α stabilization. Concerning cited2, our previous work has showed that unlike other cell types, this gene was sensitive to both HIF-1α and HIF-2α in nucleus pulposus cells (17). Accordingly, our results suggest that DMOG dependent induction in cited2 expression was primarily driven by HIF-1α accumulation. Since cited2 mRNA expression is induced after 8 h of DMOG treatment, it would not be unreasonable to assume that immediate early transcriptional activation requires HIF-2, while HIF-1 subsequently induces and sustains transcription.
Since PHD2 and to a lesser extent PHD3 were expressed at a higher level than PHD1 we chose to silence these two PHDs to investigate their role in HIF-α degradation. That PHD2 but not PHD3 silencing increased HIF-1α accumulation suggested that PHD2 selectively controlled the turnover of HIF-1α. Moreover, in line with the DMOG experiments, lack of induction of HIF-2α in PHD2 as well as PHD3 silenced cells supported the notion that these proteins have a minor or no role to play in degradation of this isoform. Based on recent reports that PHD3 was necessary for ATF4 degradation (21) while PHD1 regulated NF-κB signaling through hydroxylation of IKKβ (30), experiments are in progress to determine if PHD isoforms preferentially degrade substrates other than HIF-α in nucleus pulposus cells. Gain of function experiments provided further insights into the relationship between PHDs and HIF-α. Noteworthy, despite the ability of all exogenously expressed PHD homologs to degrade HIF-1α-ODD, PHD2 overexpression failed to decrease the endogenous HIF-1α transcriptional activity. These results indicate that the enzymatic activity of PHDs is not limited by the availability of co-factors such as α-ketoglutarate, Fe2+ and ascorbate. Importantly, it is apparent that in nucleus pulposus cells, once a certain threshold of PHD2 activity is achieved it becomes critical to sustain steady state levels of HIF-1α for maintenance of cell function and survival. To achieve this either cells may increase the rate of HIF-1α synthesis and/or HIF-1α may become resistant to further degradation. Noteworthy, this phenomenon seems to be triggered only by PHD2 overexpression implying physiological role of PHD2 in HIF-1α turnover. Again, the exact mechanism of this unique adaptation is not known and is currently under investigation. A parallel experiment examining the effect of PHD overexpression on HIF-2 target gene expression confirmed that none of the PHDs significantly mediate endogenous HIF-2α turnover.
Studies that compared accumulation of HIF-1α using maximally inhibitory concentrations of DMOG and MG132, suggested that in addition to oxygen dependent PHD pathway, HIF-1α underwent proteasomal degradation that was independent of prolyl hydroxylation. This observation was strengthened by the observation that even under hypoxia, MG132 induced a robust stabilization of HIF-α–ODDs and accumulation of endogenous HIF-1α and to a lesser extent HIF-2α. Again this response was unique to nucleus pulposus cells. Thus this oxygen independent pathway appeared to play a dominant role in HIF-1α turnover in nucleus pulposus cells. This relative oxemic insensitivity of HIF-1α degradation explains why there is normoxic stabilization of this subunit in nucleus pulposus cells. Relevant to this discussion if the observation that RACK1 and HSP70 control oxygen-independent degradation of HIF-1α through the proteasomal pathway (31, 32). While HIF-1α turnover by RACK1 is through 26S proteasome, turnover by HSP70 is mediated by either 20S and/or 26S proteasome (33). Whether this oxygen independent turnover of HIF-α in nucleus pulposus cells needs RACK1 and/or HSP70 is to be determined.
Two major pathways promote proteolysis in mammalian cells: proteasomal and lysosomal. We evaluated the effect of inhibitors bafilomycin A1, an agent that prevents proteolysis by blocking the fusion between autophagosomes and lysosomes and chloroquine that block lysosomal acidification on the accumulation of HIF-α (34, 35). Cargo accumulation in the presence of these inhibitors suggested that the lysosomal pathway was involved with both HIF-1α and HIF-2α turnover. These results are in line with finding that similar to HIF-1α, the expression of HIF-2α in hypoxic chondrocytes regulated the induction of autophagy suggesting a feedback between HIF-2 and autophagic pathway (36, 37). Since, HIF-2α is refractory to oxygen dependent proteasomal degradation and that the recent observation that NF-κB pathway transcriptionally regulate HIF-2α expression in chondrocytes (38), it may not be unreasonable to assume that in nucleus pulposus cells, the level of this isoform is regulated in a unique manner. This may occur possibly both at the transcript level as well as by the evolutionary conserved autophagosomal pathway in an oxygen independent fashion. From this perspective, in nucleus pulposus cells, the regulatory system is more complex than has hitherto been considered.
Supplementary Material
ACKNOWLEDGEMENTS
This work was supported by grants from the National Institutes of Health R01-AR050087 and R01-AR055655. Study design: MVR, IMS, Study conduct: NF, Data collection: NF, Date analysis: NF, MVR, Data interpretation: NF, KC, IMS, MVR, Drafting manuscript: NF, KC, IMS, MVR. MVR takes responsibility for the integrity of the data analysis.
Footnotes
DISCLOSURES
All authors state that they have no conflicts of interest.
REFERNCES
- 1.Gruber HE, Ashraf N, Kilburn J, Williams C, Norton HJ, Gordon BE, Hanley EN. Vertebral endplate architecture and vascularization: application of micro-computerized tomography, a vascular tracer, and immunocytochemistry in analyses of disc degeneration in the aging sand rat. Spine. 2005;30:2593–2600. doi: 10.1097/01.brs.0000187877.30149.83. [DOI] [PubMed] [Google Scholar]
- 2.Hassler O. The human intervertebral disc: A micro-angiographical study on its vascular supply at various ages. Acta Orthop Scand. 1969;40:765–772. doi: 10.3109/17453676908989540. [DOI] [PubMed] [Google Scholar]
- 3.Rudert M, Tillmann B. Lymph and blood supply of the human intervertebral disc: cadaver study of correlations to discitis. Acta Orthop Scand. 1993;64:37–40. doi: 10.3109/17453679308994524. [DOI] [PubMed] [Google Scholar]
- 4.Bartels EM, Fairbank JC, Winlove CP, Urban JP. Oxygen and lactate concentrations measured in vivo in the intervertebral discs of patients with scoliosis and back pain. Spine. 1998;23:1–7. doi: 10.1097/00007632-199801010-00001. [DOI] [PubMed] [Google Scholar]
- 5.Rajpurohit R, Risbud MV, Ducheyne P, Vresilovic EJ, Shapiro IM. Phenotypic characteristics of the nucleus pulposus: expression of hypoxia inducing factor-1, glucose transporter-1 and MMP-2. Cell Tissue Res. 2002;308:401–407. doi: 10.1007/s00441-002-0563-6. [DOI] [PubMed] [Google Scholar]
- 6.Semenza GL, Roth PH, Fang HM, Wang GL. Transcriptional regulation of genes encoding glycolytic enzymes by hypoxia-inducible factor 1. J Biol Chem. 1994;269:23757–23763. [PubMed] [Google Scholar]
- 7.Sowter HM, Raval RR, Moore JW, Ratcliffe PJ, Harris AL. Predominant role of hypoxia-inducible transcription factor (Hif)-1 alpha versus Hif-2 alpha in regulation of the transcriptional response to hypoxia. Cancer Res. 2003;63:6130–6134. [PubMed] [Google Scholar]
- 8.Scortegagna M, Ding K, Oktay Y, Gaur A, Thurmond F, Yan LJ, Marck BT, Matsumoto AM, Shelton JM, Richardson JA, Bennett MJ, Garcia JA. Multiple organ pathology, metabolic abnormalities and impaired homeostasis of reactive oxygen species in Epas1-/- mice. Nat Genet. 2003;35:331–340. doi: 10.1038/ng1266. [DOI] [PubMed] [Google Scholar]
- 9.Oktay Y, Dioum E, Matsuzaki S, Ding K, Yan LJ, Haller RG, Szweda LI, Garcia JA. Hypoxia-inducible factor 2 alpha regulates expression of the mitochondrial aconitase chaperone protein frataxin. J Biol Chem. 2007;282:11750–11756. doi: 10.1074/jbc.M611133200. [DOI] [PubMed] [Google Scholar]
- 10.Aprelikova O, Wood M, Tackett S, Chandramouli GV, Barrett JC. Role of ETS transcription factors in the hypoxia-inducible factor-2 target gene selection. Cancer Res. 2006;66:5641–5647. doi: 10.1158/0008-5472.CAN-05-3345. [DOI] [PubMed] [Google Scholar]
- 11.Maxwell PH, Wiesener MS, Chang GW, Clifford SC, Vaux EC, Cockman ME, Wykoff CC, Pugh CW, Maher ER, Ratcliffe PJ. The tumour suppressor protein VHL targets hypoxia-inducible factors for oxygen-dependent proteolysis. Nature. 1999;399:271–275. doi: 10.1038/20459. [DOI] [PubMed] [Google Scholar]
- 12.Ivan M, Kondo K, Yang H, Kim W, Valiando J, Ohh M, Salic A, Asara JM, Lane WS, Kaelin WG. HIFα targeted for VHL-mediated destruction by proline hydroxylation: implications for O2 sensing. Science. 2001;292:464–468. doi: 10.1126/science.1059817. [DOI] [PubMed] [Google Scholar]
- 13.Jaakkola P, Mole DR, Tian YM, Wilson MI, Gielbert J, Gaskell SJ, Kriegsheim Av, Hebestreit HF, Mukherji M, Schofield CJ, Maxwell PH, Pugh CW, Ratcliffe PJ. Targeting of HIF-α to the von Hippel-Lindau ubiquitylation complex by O2-regulated prolyl hydroxylation. Science. 2001;292:468–472. doi: 10.1126/science.1059796. [DOI] [PubMed] [Google Scholar]
- 14.Lieb ME, Menzies K, Moschella MC, Ni R, Taubman MB. Mammalian EGLN genes have distinct patterns of mRNA expression and regulation. Biochem Cell Biol. 2002;80:421–426. doi: 10.1139/o02-115. [DOI] [PubMed] [Google Scholar]
- 15.Risbud MV, Guttapalli A, Stokes DG, Hawkins D, Danielson KG, Schaer TP, Albert T, Shapiro IM. Nucleus pulposus cells express HIF-1alpha under normoxic culture conditions: a metabolic adaptation to the intervertebral disc microenvironment. J Cell Biochem. 2006;98:152–159. doi: 10.1002/jcb.20765. [DOI] [PubMed] [Google Scholar]
- 16.Agrawal A, Guttapalli A, Narayan S, Albert TJ, Shapiro IM, Risbud MV. Normoxic stabilization of HIF-1alpha drives glycolytic metabolism and regulates aggrecan gene expression in nucleus pulposus cells of the rat intervertebral disk. Am J Physiol Cell Physiol. 2007;293:C621–631. doi: 10.1152/ajpcell.00538.2006. [DOI] [PubMed] [Google Scholar]
- 17.Agrawal A, Gajghate S, Smith H, Anderson DG, Albert TJ, Shapiro IM, Risbud MV. Cited2 modulates hypoxia-inducible factor-dependent expression of vascular endothelial growth factor in nucleus pulposus cells of the rat intervertebral disc. Arthritis Rheum. 2008;58:3798–3808. doi: 10.1002/art.24073. [DOI] [PubMed] [Google Scholar]
- 18.Appelhoff RJ, Tian YM, Raval RR, Turley H, Harris AL, Pugh CW, Ratcliffe PJ, Gleadle JM. Differential function of the prolyl hydroxylases PHD1: PHD1, and PHD3 in the regulation of hypoxia-inducible factor. J Biol Chem. 2004;279:38458–38465. doi: 10.1074/jbc.M406026200. [DOI] [PubMed] [Google Scholar]
- 19.Ha KY, Koh IJ, Kirpalani PA, Kim YY, Cho YK, Khang GS, Han CW. The expression of hypoxia inducible factor-1alpha and apoptosis in herniated discs. Spine. 2006;31:1309–1313. doi: 10.1097/01.brs.0000219493.76081.d6. [DOI] [PubMed] [Google Scholar]
- 20.Roberts S, Evans H, Trivedi J, Menage J. Histology and pathology of the human intervertebral disc. J Bone Joint Surg Am. 2006;88:10–14. doi: 10.2106/JBJS.F.00019. [DOI] [PubMed] [Google Scholar]
- 21.Köditz J, Nesper J, Wottawa M, Stiehl DP, Camenisch G, Franke C, Myllyharju J, Wenger RH, Katschinski DM. Oxygen-dependent ATF-4 stability is mediated by the PHD3 oxygen sensor. Blood. 2007;110:3610–3617. doi: 10.1182/blood-2007-06-094441. [DOI] [PubMed] [Google Scholar]
- 22.Johansen JL, Sager TN, Lotharius J, Witten L, Mørk A, Egebjerg J, Thirstrup K. HIF prolyl hydroxylase inhibition increases cell viability and potentiates dopamine release in dopaminergic cells. J Neurochem. 2010;115:209–219. doi: 10.1111/j.1471-4159.2010.06917.x. [DOI] [PubMed] [Google Scholar]
- 23.Parker WL, Finnson KW, Soe-Lin H, Knaus P, Philip A. Expression and function of TbetaRII-B, a variant of the type II TGF-beta receptor, in human chondrocytes. Osteoarthritis Cartilage. 2007;15:442–453. doi: 10.1016/j.joca.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 24.Lago R, Gomez R, Otero M, Lago F, Gallego R, Dieguez C, Gomez-Reino JJ, Gualillo O. A new player in cartilage homeostasis: adiponectin induces nitric oxide synthase type II and pro-inflammatory cytokines in chondrocytes. Osteoarthritis Cartilage. 2008;16:1101–1109. doi: 10.1016/j.joca.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 25.Thoms BL, Murphy CL. Inhibition of hypoxia-inducible factor-targeting prolyl hydroxylase domain-containing protein 2 (PHD2) enhances matrix synthesis by human chondrocytes. J Biol Chem. 2010;285:20472–20480. doi: 10.1074/jbc.M110.115238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Minamishima YA, Moslehi J, Bardeesy N, Cullen D, Bronson RT, Kaelin WG. Somatic inactivation of the PHD2 prolyl hydroxylase causes polycythemia and congestive heart failure. Blood. 2008;111:3236–3244. doi: 10.1182/blood-2007-10-117812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Takeda K, Ho VC, Takeda H, Duan LJ, Nagy A, Fong GH. Placental but not heart defects are associated with elevated hypoxia-inducible factor alpha levels in mice lacking prolyl hydroxylase domain protein 2. Mol Cell Biol. 2006;26:8336–8346. doi: 10.1128/MCB.00425-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Metzen E, Stiehl DP, Doege K, Marxsen JH, Hellwig-Bürgel T, Jelkmann W. Regulation of the prolyl hydroxylase domain protein 2 (phd2/egln-1) gene: identification of a functional hypoxia-responsive element. Biochem J. 2005;387:711–717. doi: 10.1042/BJ20041736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pescador N, Cuevas Y, Naranjo S, Alcaide M, Villar D, Landázuri MO, Del Peso L. Identification of a functional hypoxia-responsive element that regulates the expression of the egl nine homologue 3 (egln3/phd3) gene. Biochem J. 2005;390:189–197. doi: 10.1042/BJ20042121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cummins EP, Berra E, Comerford KM, Ginouves A, Fitzgerald KT, Seeballuck F, Godson C, Nielsen JE, Moynagh P, Pouyssegur J, Taylor CT. Prolyl hydroxylase-1 negatively regulates IkappaB kinase-beta, giving insight into hypoxia-induced NFkappaB activity. Proc Natl Acad Sci U S A. 2006;103:18154–18159. doi: 10.1073/pnas.0602235103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu YV, Baek JH, Zhang H, Diez R, Cole RN, Semenza GL. RACK1 competes with HSP90 for binding to HIF-1alpha and is required for O(2)-independent and HSP90 inhibitor-induced degradation of HIF-1alpha. Mol Cell. 2007;25:207–217. doi: 10.1016/j.molcel.2007.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Luo W, Zhong J, Chang R, Hu H, Pandey A, Semenza GL. Hsp70 and CHIP selectively mediate ubiquitination and degradation of hypoxia-inducible factor (HIF)-1alpha but Not HIF-2alpha. J Biol Chem. 2010;285:3651–3663. doi: 10.1074/jbc.M109.068577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van de Sluis B, Groot AJ, Vermeulen J, van der Wall E, van Diest PJ, Wijmenga C, Klomp LW, Vooijs M. COMMD1 Promotes pVHL and O2-Independent Proteolysis of HIF-1alpha via HSP90/70. PLoS One. 2009;4:e7332. doi: 10.1371/journal.pone.0007332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yamamoto A, Tagawa Y, Yoshimori T, Moriyama Y, Masaki R, Tashiro Y. Bafilomycin A1 prevents maturation of autophagic vacuoles by inhibiting fusion between autophagosomes and lysosomes in rat hepatoma cell line, H-4-II-E cells. Cell Struct Funct. 1998;23:33–42. doi: 10.1247/csf.23.33. [DOI] [PubMed] [Google Scholar]
- 35.Rubinsztein DC, Gestwicki JE, Murphy LO, Klionsky DJ. Potential therapeutic applications of autophagy. Nat Rev Drug Discov. 2007;6:304–312. doi: 10.1038/nrd2272. [DOI] [PubMed] [Google Scholar]
- 36.Zhang H, Bosch-Marce M, Shimoda LA, Tan YS, Baek JH, Wesley JB, Gonzalez FJ, Semenza GL. Mitochondrial autophagy is an HIF-1-dependent adaptive metabolic response to hypoxia. J Biol Chem. 2008;283:10892–10903. doi: 10.1074/jbc.M800102200. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 37.Bohensky J, Terkhorn SP, Freeman TA, Adams CS, Garcia JA, Shapiro IM, Srinivas V. Regulation of autophagy in human and murine cartilage: hypoxia-inducible factor 2 suppresses chondrocyte autophagy. Arthritis Rheum. 2009;60:1406–1415. doi: 10.1002/art.24444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Saito T, Fukai A, Mabuchi A, Ikeda T, Yano F, Ohba S, Nishida N, Akune T, Yoshimura N, Nakagawa T, Nakamura K, Tokunaga K, Chung UI, Kawaguchi H. Transcriptional regulation of endochondral ossification by HIF-2alpha during skeletal growth and osteoarthritis development. Nat Med. 2010;16:678–686. doi: 10.1038/nm.2146. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.