Abstract
Transcutaneous DNA immunization is an attractive immunization approach. Previously, we reported that transcutaneous immunization by applying plasmid DNA onto a skin area wherein the hair follicles had been induced into growth stage by ‘cold’ waxing-based hair plucking significantly enhanced the resultant immune responses. In the present study, using a plasmid that encodes the Bacillus anthracis protective antigen (PA63) gene fragment, it was shown that the anti-PA63 antibody responses induced by applying the plasmid onto a skin area where the hair was plucked by ‘warm’ waxing were significantly stronger than by ‘cold’ waxing, very likely because the ‘warm’ waxing-based hair depilation significantly i) enhanced the uptake (or retention) of the plasmid in the application area and ii) enhanced the expression of the transfected gene in the follicular and interfollicular epidermis in the skin. The antibody response induced by transcutaneous DNA immunization was hair cycle dependent, because the plasmid needed to be applied within 5 days after the hair plucking to induce a strong antibody response. The antibody responses were not affected by whether the expressed PA63 protein, as an antigen, was secreted or cell surface bound. Finally, this strategy of enhancing the immune responses induced by transcutaneous DNA immunization following ‘warm’ waxing-based hair depilation was not limited to the PA63 as an antigen, because immunization with a plasmid that encodes the HIV-1 env gp160 gene induced a strong anti-gp160 response as well. Transcutaneous DNA immunization by modifying the hair follicle cycle may hold a great promise in inducing strong and functional immune responses.
Keywords: Antibody, hair follicles, HIV-1 gp160, protective antigen
1. INTRODUCTION
Transcutaneous immunization onto the skin has become a favorable route for vaccine administration over the traditional use of needles and syringes. The feasibility of transcutaneous immunization using plasmid DNA was proven in the 1990’s, but the resultant immune responses were generally weak [1, 2]. Several approaches have been taken to enhance the immune responses from transcutaneous DNA immunization, including physical or chemical disruption of the stratum corneum [3, 4], the use of vaccine adjuvants or skin permeation enhancers [5, 6], or formulating the plasmid into carrier systems such as nanoparticles or emulsions [7, 8]. However, all these approaches have had only limited success at enhancing the immune responses.
Data from several studies have shown that the main portals of entry for plasmid DNA applied onto the skin are the hair follicles, and the transfected gene expression was mainly confined to the hair follicles [9–13]. The penetration or uptake of substances applied onto the skin via the hair follicles is reported to be dependent on whether the hair follicles are in growing or resting stages [14]. Hair follicles are open for penetration by foreign objects when in the growth (or anagen) stage, and closed when in the resting (or telogen) stage [14]. Domashenko et al. (2000) reported that the stage of the hair follicle cycle at the time of DNA application is critical for the expression of transfected genes [10]; the highest expression occurred when the plasmid was applied during the anagen stage when cells in the hair follicle are proliferating [10]. Fan et al. (1999) reported that functional hair follicles were required for a topically applied DNA vaccine to induce immune responses [11]. Based on the aforementioned findings, we hypothesized, and provided data to support, that transcutaneous immunization by applying plasmid DNA onto a skin area wherein the hair follicles were induced into growth stage by hair plucking elicited a stronger antibody response than when the hair follicles in the application area were in the resting stage [15].
In our previous study, the hair in the application area was plucked by ‘cold’ waxing. In the present study, the immune responses induced by plasmid DNA applied onto a skin area wherein the hair had been plucked using a ‘warm’ waxing technique were evaluated. ‘Cold’ waxing comes in the form of a prewaxed strip, which is placed over the desired, hair-trimmed skin area and is rapidly removed, resulting in significant breakage of the hair at or below the surface of the skin. In contrast, in ‘warm’ waxing, wax is applied directly onto the hair in the desired skin area in a viscous liquid form; and the warmth of the wax is expected to allow the hair follicle pores to expand and the complete removal of the hair from the follicles. Therefore, we reasoned that the ‘warm’ waxing-based hair depilation would allow plasmid DNA applied onto the skin to induce a stronger immune response than the ‘cold’ waxing-based hair depilation, because the former not only induces the hair follicles into growth stage, but also results in the better removal of hair from the hair follicles, and thus, leaves the hair follicles open for penetration by the topically applied plasmid DNA.
Although mouse hair cycling is dependent on genetic background (strain), sex as well as environmental and nutritional factors, in general, after the removal of hair on the dorsal skin of 6–7 week old mice, days 0 through 2 are the early anagen stage, where upregulated genes were mainly related to dermal inflammation [16, 17]. Days 3 through 6 are the mid-anagen stage where up-regulated genes mainly functioned in cell proliferation [16]. Late anagen and early catagen stages start around day 7, and the telogen stage starts around day 25 [17]. To identify the optimal time to apply the plasmid DNA after hair plucking, the dependence of time, at which the plasmid DNA was applied onto the skin following ‘warm’ waxing-based hair depilation, on the resultant immune responses was evaluated. The B. anthracis PA63 protein encoding plasmid, pGPA, was used in the aforementioned studies. The pGPA construct has a signal sequence of human plasminogen activator fused to the N-terminus of the PA63 protein, and thus, resulting in PA63 secretion by transfected cells [18]. To determine the extent to which the secretion of the PA63 protein by the transfected cells contributed to the resultant immune response, pCPA, another PA63 plasmid that does not allow the secretion of the PA63 by transfected cells, was used to immunize mice [19]. Finally, to test whether the ‘warm’ waxing-based hair depilation approach of enhancing the immune response induced by transcutaneous DNA immunization is applicable to an antigen other than the PA63, the immune responses induced by a plasmid that encodes the HIV-1 full-length gp160 env gene (p96ZM651gp160-opt) were evaluated as well [20].
2. EXPERIMENTAL SECTION
2.1. Plasmids
The pGPA plasmid, constructed by inserting the gene fragment encoding amino acids 173–764 of the B. anthracis PA gene into pJW4304, was kindly provided by Dr. Dennis Klinman [18]. This portion of the PA protein represents the protease-cleaved fragment (PA63) of the full-length protein that is active in vivo [18]. The pCPA plasmid was constructed following a previously published method with slight modifications [19]. Briefly, the gene fragment encoding amino acid 173–764 of PA gene was amplified from the pGPA plasmid using polymerase chain reaction (PCR) (primers, 5’-ACAAGTCTCGAGCCTACGCTTCCA-3’ and 5’-CCTAGATCTAGATTATCCTATCTCATAGCC-3’). The PCR product was digested with XhoI and XbaI, ligated into the pCI mammalian expression vector (Promega, Madison, WI), and transferred into Escherichia coli DH5α. The HIV-1 full-length gp160 env geneencoding plasmid, p96ZM651gp160-opt, was from the NIH AIDS Research & Reference Reagent Program (Germantown, MD). The p96ZM651gp160-opt was constructed by ligating codon-optimized full-length gp160 gene into the pcDNA3.1(−) expression vector [20]. The pCMV-β was from the American Type Culture Collection (Manassas, VA) [21]. Plasmid was purified using a QIAGEN Midiprep kit according to the manufacturer’s instruction (Valencia, CA). Large scale plasmid preparation was performed by GenScript (Piscataway, NJ).
2.2. Application of plasmid DNA onto mouse skin
National Institutes of Health guidelines for animal use and care were followed in all animal studies. Animal protocol was approved by the Institutional Animal Care and Use Committee at the University of Texas at Austin. Female BALB/c mice (n = 5–10), 6 weeks of age, were from Charles River Laboratories (Wilmington, MA). The 6-week old mice were used because the hair follicles on the dorsal skin of mice of 35–75 days of age are predominately in the second telogen phase so that they can be induced into growth stage by plucking [22, 23]. The hair in the mid-dorsum of anesthetized mice was plucked with ‘warm’ wax (50–55°C, GiGi® Honee, American International Industries, Los Angeles, CA) in an area of ~1.5 cm2. As controls, hair was either trimmed with an electric clipper, or trimmed and then plucked with ‘cold’ wax (Veet® wax strips, Reckitt Benckiser, Parsippany, NJ). At predetermined time points (0, 2, 5, or 10 days later), the hair plucked area of anesthetized mice was cleaned with 70% ethanol swab, hydrated for 20 min with warm water, and paper-dried. Plasmid DNA (pGPA, pCPA, or p96ZM651gp160-opt, 50 µg) was admixed with cholera toxin (CT, 10 µg, List Biological Laboratories, Campbell, CA) and gently dripped onto the hydrated area using a pipette tip. CT was added into the plasmid DNA solution because data from one of our previous studies showed that CT significantly improved the antibody responses induced by plasmid DNA vaccine applied topically onto mouse skin [5]. The applied area was allowed to air-dry and then carefully covered with a piece of Tegaderm™ self-adhesive dressing film (3M, St. Paul, MN) to keep the plasmid DNA in the application area for an extended period of time [24–26]. Mice in the positive control groups were either injected intramuscularly with 50 µg of plasmid in phosphate buffered saline (PBS, pH 7.4, 10 mM) or subcutaneously injected with protective antigen protein (PA, 5 µg/mouse, List Biological) in 50 µL of PBS admixed with incomplete Freund’s adjuvant (IFA, 100 µL, Sigma-Aldrich, St. Louis, MO). Mice in the negative control group were left untreated. Mice were dosed on days 0, 14, and 28 on three different areas on the dorsal skin, and euthanized and bled on day 49 or where mentioned.
2.3. Enzyme-linked immunosorbent assay (ELISA)
The levels of anti-PA and anti-gp160 in serum samples were determined using ELISA [15]. Briefly, EIA/RIA flat bottom, medium binding, polystyrene, 96-well plates (Corning-Costar, Corning, NY) were coated with 100 ng of PA (List Biological) or the gp140 protein (NIH AIDS Research & Reference Reagent Program) dissolved in 100 µL carbonated buffer (0.1 M, pH 9.6) at 4°C overnight. The plates were washed with PBS/Tween 20 (10 mM, pH 7.4, 0.05% Tween 20) and blocked with 4% (w/v) bovine serum albumin (BSA) in PBS/Tween 20 for 1 h at 37°C. Serum samples were diluted two-fold serially (or as indicated) in 4% BSA/PBS/Tween 20, added to the plates following the removal of the blocking solution, and incubated for additional 4 h at 37°C. The serum samples were removed, and the plates were washed 5 times with PBS/Tween 20. Horseradish peroxidase-labeled goat anti-mouse immunoglobulins (IgG, IgG1, or IgG2a, 5,000-fold dilution in 1% BSA/PBS/Tween 20, Southern Biotechnology Associates Inc., Birmingham, AL) were added into the wells, followed by another hour of incubation at 37°C. Plates were again washed five times with PBS/Tween 20. The presence of bound antibody was detected following a 30 min incubation at room temperature in the presence of 3, 3’, 5, 5’-tetramethyl benzidine solution (TMB, Sigma-Aldrich), followed by the addition of 0.2 M sulfuric acid as the stop solution. The absorbance was read at 450 nm. Antibody titers were derived by comparing the OD450 nm values of the samples with the OD450 nm plus 2 × S.D. of the untreated mice.
2.4. Anthrax lethal toxin neutralization activity assay
To evaluate the functionality of the anti-PA antibodies against anthrax lethal toxin, a toxin neutralization assay was performed as previously described [27]. Briefly, confluent J774A.1 cells (1 × 104) were plated into sterile, 96-well, clean-bottom plates and incubated at 37°C, 5% CO2 for 24 h. A solution (50 µL) containing PA (400 ng/mL) and lethal factor (LF, List Biological, 100 ng/mL) was mixed with 50 µL of diluted serum samples and incubated for 2 h at 37°C. The cell culture medium was removed, and 100 µL of the serum/lethal toxin mixture was added into each well. After 6 more h of incubation at 37°C, 5% CO2, the cell viability was determined using an MTT kit, with untreated and lethal toxin alone treated cells as controls. The PA protein is required for the LF to enter cells to cause cell death [28]. Neutralization of the PA by anti-PA antibodies prevents the entrance of LF into cells and thus protects the cells from being killed by LF [29].
2.5. Quantification of plasmid in skin samples
Mice were euthanized 24 h after plasmid application, and the skin in the application area was washed and collected. Total DNA was extracted from the skin samples using the DNAzol reagent (Invitrogen). PCR was carried out to semi-quantify the amount of plasmid remaining in the skin samples [15]. Mouse β-actin gene was also amplified as an internal control. The primers for the β-actin were 5’-AGCCATGTACGTAGCCATCC-3’ (forward) and 5’-CTCTCAGCTGTGGTGGTGAA-3’ (reverse), which amplify a 228 bp fragment of the mouse β-actin gene. The primers for the PA gene were 5’-CCTACGGTTCCAGACCGTGACAATG-3’ (forward) and 5’-AGCCCAAGTTCTTTCCCCTGCTA-GAGATAG-3’ (reverse), which amplify a 525 base pair fragment of the PA gene. A 50 µL PCR reaction contained 1 U platinum taq DNA polymerase, 0.2 mM of each dNTP, 0.2 µM of each primer, and 1 µg DNA. PCR cycling conditions included an initial step of 5 min at 94°C, followed by 35 cycles of 30 s at 94°C to denature the DNA, 30 s at 55°C for primer annealing, and 30 s at 72°C for extension. A final cycle with a further 5 min extension at 72°C concluded the reaction. The PCR product was analyzed using 1% agarose gel containing ethidium bromide and quantified by measuring the DNA band intensity using the GeneSnap software from Syngene G-box (Syngene, Frederick, MD). The relative amount of plasmid remaining in each skin sample was calculated by dividing the band intensity of the PA gene by that of the β-actin gene. This experiment was repeated using three mice per group.
2.6. Histology
Skin samples were collected immediately or 2, 5, and 10 days after ‘warm’ waxing-based hair plucking, fixed in formalin, embedded in paraffin, sectioned vertically, and stained using antibody against 5-bromo-2’-deoxyuridine (BrdU). Mice were injected intraperitoneally with BrdU (100 µg/g body weight) in PBS 30 min prior to euthanization to collect the skin samples. To examine the expression of the transfected gene in the skin, pCMV-β, a plasmid that encodes the β-galactosidase gene, was applied onto a skin area where the hair was removed by ‘cold’ or ‘warm’ waxing 2 days prior to the plasmid DNA application. Twenty-four hours later, the skin area was harvested, fixed in formalin, embedded in paraffin, sectioned vertically, and stained against β-galactosidase protein. To visualize the retention of plasmid DNA in mouse skin, fluorescein-labeled pGPA plasmid was used. The pGPA was labeled with fluorescein using a Label IT® Nucleic Acid labeling kit from Mirus Bio LLC (Madison, WI). The hair on the back of mice was trimmed using a clipper or plucked by ‘warm’ waxing. Two days later, fluorescein-labeled pGPA plasmid (50 µg) was applied onto the treated area, which was allowed to air-dry and then covered with Tegaderm® film. After 6 h, the treated area was washed extensively with water and paper-dried. The skin was harvested immediately and cut into two halves. One half was examined horizontally under a Nikon Eclipse Ti Fluorescence Microscope (Nikon Instrument Inc., Melville, NY); the other half was frozen, sectioned vertically, stained with 4’,6-diamidino-2-phyenylindole (DAPI), and examined under a fluorescence Olympus BX60 Microscope (Olympus America, Inc., Center Valley, PA). All immunohistostaining was performed in the Histology Core at the UT MD Anderson Cancer Center Science Park Research Division (Smithville, TX).
2.7. Transepidermal water loss (TEWL)
Hair in the mid-dorsum of anesthetized mice was either trimmed, trimmed and plucked with ‘cold’ wax, or plucked with ‘warm’ wax (n = 3). TEWL measurements were taken using a VapoMeter from Delfin Technologies, Inc. (Stamford, CT) following the manufacturer’s instructions. At least three readings were taken from each mouse at each time point (0 and 48 h).
2.8. Statistics
Statistical analyses were completed using ANOVA followed by Fisher’s protected least significant difference procedure. Logarithmic regression was used to compare the rate of change of the relative OD450 value over 10-fold serial serum dilutions to compare the anti-gp160 antibodies between the intramuscularly injected group and the transcutaneously immunized group. A p-value of ≤ 0.05 (two-tail) was considered statistically significant.
3. RESULTS
3.1. Transcutaneous immunization by application of pGPA onto a skin area wherein the hair had been plucked using a ‘warm’ waxing technique led to a stronger anti-PA immune response than using a ‘cold’ waxing technique
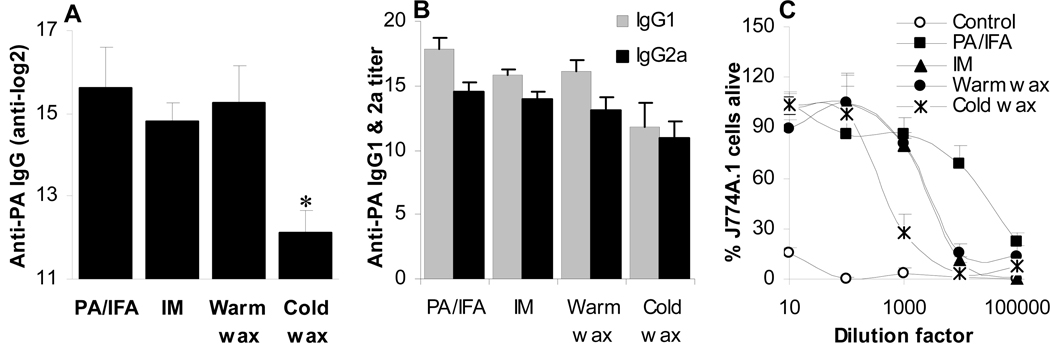
Previously, our group showed that strong and functional immune responses were induced by applying a plasmid DNA topically onto a skin area wherein the hair follicles have been induced into anagen-onset stage by plucking with ‘cold’ wax [15]. In the present study, the immune responses induced by transcutaneous immunization with the B. anthracis PA63 gene encoding pGPA plasmid on a skin area where the hair was plucked two days earlier using ‘cold’ vs. ‘warm’ waxing techniques were evaluated and compared. Plucking the hair by ‘warm’ waxing resulted in an anti-PA IgG titer that was significantly higher than by ‘cold’ waxing (p < 0.001) (Fig. 1A). In fact, the level of the anti-PA IgG detected in the ‘warm’ waxing group was not different from that in mice intramuscularly injected with the pGPA or when mice were subcutaneously injected with PA protein adjuvanted with incomplete Freund’s adjuvant (PA/IFA) (p = 0.33, ANOVA) (Fig. 1A). Similar to intramuscular injection of pGPA and subcutaneous administration of PA adjuvanted with IFA, transcutaneous immunization after the hair in the application area was plucked using both waxing techniques induced strong anti-PA IgG1 and IgG2a antibodies (Fig. 1B). Finally, the anti-PA antibodies in mice transcutaneously immunized with the pGPA were able to protect macrophages (J774A.1) against anthrax lethal toxin challenge (Fig. 1C). However, the serum from mice transcutaneously immunized following ‘warm’ waxing had a 50% neutralizing concentration value of 5.1-fold greater than that from mice transcutaneously immunized following ‘cold’ waxing (p = 0.02). PCR was carried out to semi-quantify the amount of pGPA retained in the skin area 24 h after the application of the pGPA. Relatively more PA63 gene fragments were recovered from the skin area wherein the hair was plucked by ‘warm’ waxing than by ‘cold’ waxing (Figs. 2A, B, p = 0.003), indicating that ‘warm’ waxing led to more DNA uptake or retention in the skin than ‘cold’ waxing.
Figure 1.
Comparison of the anti-PA antibody responses induced by topically applied pGPA plasmid when the hair in the application area was plucked by ‘warm’ or ‘cold’ waxing 2 days earlier. (A) Anti-PA IgG titer (*, p < 0.001, warm wax vs. cold wax). (B) Anti-PA IgG1 vs. IgG2a titers. (C) The anti-serum from the immunized mice protected J774A.1 macrophages from anthrax lethal toxin. Data reported as mean ± S.D. (n = 5–10). IM indicates intramuscular injection of pGPA.
Figure 2.
Potential mechanisms of immune response enhancement after transcutaneous DNA immunization following hair removal by ‘warm’ waxing. (A–B) The uptake or retention of the pGPA plasmid in the skin. Shown in A are the PA63 and β-actin gene fragments after PCR amplification; data in B are the ratios of the band intensity in A. (C) The expression of β-galactosidase (brown color) 24 h after the pCMV-β plasmid was applied on a skin area where the hair was plucked by ‘cold’ waxing vs. ‘warm’ waxing 2 days earlier (bar = 200 µm). (D) TEWL values in mouse skin area (n = 3) (*, the value of the Trim+cold wax was different from that of the others). (E) Interfollicular epidermal thickness (n = 21–26) (**, the value of Trim is different from that of the others).
To examine the expression of plasmid-encoding gene in the skin, pCMV-β, instead of pPGA, was applied onto the skin area where the hair was removed by ‘cold’ or ‘warm’ waxing 2 days prior to the plasmid DNA application. The pCMV-β was used for easy detection of the expression of the β-galactosidase by immunohistostaining, which revealed a strong expression of β-galactosidase in both follicular and interfollicular epidermis in the skin area that received the ‘warm’ waxing (Fig. 2C). However, only weak β-galactosidase expression was detected in the follicular and interfollicular epidermis in the skin area that received the ‘cold’ waxing (Fig. 2C).
In order to evaluate whether the hair plucking may have physically damaged the skin, the TEWL values on the skin area immediately after the plucking and at the time of the plasmid DNA application were measured. Immediately after plucking (day 0), the TEWL value on the skin area that received ‘warm’ waxing was slightly greater than on the skin area where the hair was simply trimmed, indicating that the ‘warm’ waxing caused minor damages to the skin (Fig. 2D). However, two days later (i.e., at the time of DNA application), the TEWL value on the skin area that received ‘warm’ waxing was no longer greater than on the skin area where the hair was trimmed (Fig. 2D). In contrast, hair trimming followed by ‘cold’ waxing led to a TEWL value increase by up to 4-fold, as compared to hair trimming alone (Fig. 2D).
Finally, both ‘warm’ and ‘cold’ waxing induced local inflammation as shown by epidermal hyperplasia (Fig. 2E) and the increased dermal cellularity (data not shown), but the extent of inflammation induced by ‘warm’ and ‘cold’ waxing were not significantly different, as judged by the interfollicular epidermal thickness (p = 0.14, t-test) (Fig. 2E).
3.2. Plasmid DNA needs to be applied within a certain period of time after hair plucking to induce a strong immune response
Transcutaneous immunization by application of the pGPA plasmid onto a skin area wherein the hair had been plucked by ‘warm’ waxing led to a significantly stronger anti-PA immune response than by ‘cold’ waxing; therefore, subsequent experiments were carried out only using ‘warm’ waxing. To evaluate the extent to which the time of DNA application after waxing impacts the resultant anti-PA immune responses, hair was plucked by ‘warm’ waxing, and pGPA plasmid was applied onto the plucked area immediately or 2, 5, or 10 days later. Applying pGPA onto the skin immediately following hair plucking, or 2 or 5 days later resulted in strong and comparable anti-PA IgG responses (ANOVA days 0, 2 and 5, p = 0.08) (Fig. 3A). However, applying the pGPA onto the skin 10 days after the hair plucking led to a significantly weaker anti-PA IgG response (ANOVA days 0, 2, 5, and 10, p < 0.001) (Fig. 3A). The anti- PA IgG response was balanced between IgG1 and IgG2a when immunized on day 0 or day 2 (IgG1/IgG2a ratio, 1.09 ± 0.08 and 1.09 ± 0.03, respectively, p = 0.86) (Fig. 3B), but more biased towards IgG1 (1.38 ± 0.07, p < 0.001) when immunized 5 days after hair plucking (Fig. 3B). Only weak anti-PA IgG1 and IgG2a responses were induced when the pGPA was applied 10 days after hair plucking (Fig. 3B). Again, the anti-PA antibodies were found to be functional because they were able to protect macrophages from an anthrax lethal toxin challenge (Fig. 3C).
Figure 3.
The effect of the time, at which the pGPA was applied onto the skin after the ‘warm’ waxing-based hair plucking, on the resultant anti-PA antibody responses. (A) Total anti-PA IgG titer (n = 8–10) (*, p < 0.001, AVNOVA). (B) Anti-PA IgG1 vs. IgG2a titers. (C) Anthrax lethal toxin neutralization assay. (D) Photos of skin samples after anti-BrdU staining (bar = 200 micrometers, except that in the day 10 photo, it was 1 mm, and the photo was taken at a lower magnification to visualize the full epidermis and dermis layers). (E) The thickness of the interfollicular epidermis (n = 8–33) 0, 2, 5 and 10 days after ‘warm’ waxing-based hair plucking. (F) Uptake (or retention) of the pGPA plasmid in skin 24 h after DNA application, as indicated by the ratio of band intensity of a PA63 gene fragment to that of the mouse beta-actin gene after PCR amplification (n = 3). (G) Fluorescence images of skin 6 h after fluorescein-labeled pGPA (Green) was applied on a skin area wherein the hair was plucked by ‘warm’ waxing or simply trimmed 2 days earlier. Left: horizontal view of the skin immediately after harvest; Right: view after vertical frozen-sectioning and DAPI staining (Blue). Notes: It is known that the hair shaft has strong auto-fluorescence.
Anti-BrdU staining failed to reveal cell proliferation immediately after hair plucking (Fig. 3D). However, active proliferation was detected in the basal epidermal layers 2 days after plucking (Fig. 3D). Cell proliferation was decreased in the basal epidermal layers 5 days after plucking. Instead, proliferation was increasingly active in the bulb area of the hair follicles (Fig. 3D). Ten days after the hair plucking, cell proliferation was detected only in the bulb area of the hair follicles (Fig. 3D). The significantly thicker interfollicular epidermis in the skin 2 days after hair plucking was also indicative of active cell proliferation and hair follicle growth (Fig. 3E).
Semi-quantitative PCR data showed that similar amounts of pGPA gene fragments were recovered in the skin 24 h after the application of the pGPA, regardless whether the pGPA was applied immediately, 2, or 5 days after the hair plucking (Fig. 3F, p = 0.72), but it was relatively lower when the pGPA was applied 10 days after the plucking (Fig. 3F). Finally, when fluorescein-labeled pPGA plasmid was applied, strong fluorescence signal was readily detected in the skin area wherein the hair was plucked by ‘warm’ waxing 2 days prior to the DNA application, whereas only weaker fluorescence signal was detected in the skin area where the hair was simply trimmed (Fig. 3G), confirming the retention or uptake of plasmid DNA in the skin area when the hair in that area was plucked by ‘warm’ waxing.
3.3. The antibody responses induced by transcutaneous immunization were not different regardless of whether the plasmid DNA encoded secreting PA63 or cell surface-bound PA63
Transcutaneous immunization using the pCPA plasmid or the pGPA plasmid onto a skin area wherein the hair was plucked by ‘warm’ waxing resulted in comparable anti-PA IgG titers (p = 0.63) (Fig. 4A), indicating that the immune response was not significantly affected whether the PA antigen produced by the transfected cells was secreted or cell surface bound. Similar to pGPA, when mice were transcutaneously immunized with pCPA, the anti-PA IgG subtypes (IgG1 and IgG2a), although strong, were slightly IgG1-biased, whereas the anti-PA IgG induced by the intramuscularly injected pCPA was more balanced (Fig. 4B).
Figure 4.
Comparison of the total anti-PA IgG titers (A) and IgG subtypes (B) in mice transcutaneously immunized with pGPA or pCPA two days after ‘warm’ waxing of the hair in the application area. Data shown are mean ± S.D. (n = 10 for pGPA skin and pCPA skin, n = 5 for others). The ‘pGPA T’ means pGPA applied onto a skin area where the hair was trimmed, or the hair follicles were in the 2nd natural telogen stage.
3.4. Transcutaneous immunization with a plasmid that encodes the HIV-1 gp160 protein onto a skin area wherein the hair was plucked by ‘warm’ waxing induced a strong anti-gp160 antibody response
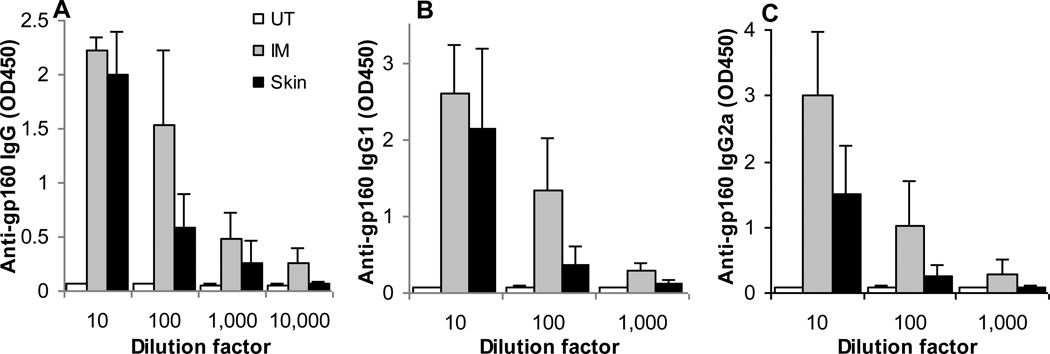
In previous experiments, pGPA and pCPA were used to immunize mice, and both plasmids encode the anthrax PA63 protein. In order to understand whether transcutaneous immunization onto a skin area following hair plucking by ‘warm’ waxing is effective with a plasmid that encodes an antigen other than the PA63, a plasmid that encodes the HIV-1 gp160 env protein, p96ZM651gp160-opt, was used. Transcutaneous immunization with the p96ZM651gp160-opt onto a skin area wherein the hair was plucked by ‘warm’ waxing also induced a strong anti-gp160 IgG response (Fig. 5A), which was not significantly different from the anti-gp160 IgG level in mice intramuscularly injected with the plasmid (logarithmic regression: β1 = −0.302 ± 0.03 and β2 = −0.266 ± 0.06, p = 0.29). Again, both anti-gp160 IgG1 and IgG2a were induced after immunization with the p96ZM651gp160-opt, but they tended to be weaker after transcutaneous immunization than after intramuscular injection (Figs. 5B, C).
Figure 5.
Serum total anti-gp160 IgG (A), anti-gp160 IgG1 (B), and anti-gp160 IgG2a (C) levels in mice transcutaneously immunized with p96ZM651gp160-opt. Data shown are mean ± S.D. (n = 5 for UT and IM, 10 for Skin) (UT, untreated; IM, intramuscular injection; Skin, topical dosing onto the skin).
4. DISCUSSION
Previously, our group reported that transcutaneous immunization with the anthrax PA63-encoding plasmid, pGPA, onto a mouse skin area wherein the hair follicles had been induced into growth stage led to stronger anti-PA immune responses than when the plasmid was applied onto a skin area wherein the hair follicles were predominantly in resting stage [15]. In that study, we used a ‘cold’ waxing technique (with Veet® wax strips) to pluck the hair to induce the hair follicles into growth stage [15]. However, there are several other hair removal methods readily available on the market, including chemicals, tweezing, hard wax, and warm wax. Chemical hair removers generally do not remove the hair below the skin surface, and hard wax, like ‘cold’ wax, leads to significant breakages of the hair at the skin surface (see supplemental Fig. S1). The ‘warm’ waxing technique uses heat to open up the hair follicles, embed the hair in molten wax, and remove the hair more efficiently from the follicles (Supplemental Fig. S1). Therefore, in the first part of the present study, the immune responses induced by transcutaneous immunization using pGPA when the hair in the application area was plucked using a ‘warm’ waxing technique were evaluated.
Applying the pGPA plasmid onto a skin area wherein the hair was plucked using a ‘warm’ waxing technique led to a stronger anti-PA immune response than when using the previously used ‘cold’ waxing technique (Fig. 1A). In fact, the anti-PA IgG response induced by transcutaneous immunization with the pGPA plasmid onto a skin area where the hair was plucked by ‘warm’ waxing was not significantly different from that when the pPGA was injected intramuscularly into mice or when the mice were subcutaneously injected with the PA protein admixed with IFA (Fig. 1A). The anti-PA antibodies induced following the ‘warm’ waxing technique were confirmed to be functional in an in vitro anthrax lethal toxin neutralization assay (Fig. 1C). The anti-PA IgG induced after transcutaneous immunization was biased towards IgG1 (Fig. 1B), suggesting the induction of a slightly CD4+ T helper type 1 (Th1) response. This finding is in agreement with data from previous studies, showing that when plasmid DNA vaccine was given intradermally using a ‘gene gun’, the immune responses induced were slightly Th1-biased as well [30].
The enhancement of immune responses induced by transcutaneous DNA immunization after wax-based hair removal may be due to multiple reasons. Hair plucking is well known to induce hair follicles into growth stage, and hair follicles in their growth stage are open to penetration by foreign objects. It was found that significantly more pGPA plasmid was retained in the skin area where the hair was plucked by ‘warm’ waxing than by ‘cold’ waxing (Figs. 2A, B). The retention of pPGA plasmid in the skin area where the hair was removed by ‘warm’ waxing was also confirmed using fluorescein-labeled pGPA plasmid (Fig. 3G). When the β-galactosidase gene-encoding plasmid pCMV-β was applied onto a skin area where the hair was removed by ‘warm’ waxing 2 days prior to the plasmid DNA application, the strong expression of the β-galactosidase protein in the follicular and interfollicular epidermis of the treated skin area indicated that the ‘warm’ waxing-based hair plucking led to an enhanced expression of the transfected gene in the DNA application area than ‘cold’ waxing. The ‘warm’ waxing-based hair depilation removed the hair, but the integrity of the skin was not compromised at the time of the pGPA application (Fig. 2D). Finally, similar to ‘cold’ waxing, the ‘warm’ waxing also induced inflammation in the plucked area in the skin as shown by epidermal hyperplasia and increased cellularity in the dermis (Fig. 2E), but the inflammation induced by the ‘warm’ waxing was not significantly different from that induced by ‘cold’ waxing. Taken together, although the extent to which each of the aforementioned changes after the ‘warm’ wax-based hair depilation had contributed to the resultant immune responses is unclear, the increased retention of plasmid and the enhanced expression of the antigen gene encoded by the plasmid in the skin after the ‘warm’ waxing-based depilation, as compared to the ‘cold’ waxing-based depilation, was likely responsible for the stronger anti-PA IgG responses induced after transcutaneous DNA immunization (Fig. 1A). This is in agreement with what was recently reported that the extent of the uptake of the plasmid into the skin determines the immune responses induced by a DNA vaccine applied topically onto the skin [26].
The following two procedures were used during the transcutaneous immunization: i) the skin area where the plasmid DNA was applied was covered with the occlusive Tegaderm film, and ii) the DNA application area was hydrated with warm water for 20 min prior to the application of the DNA. Water is the ideal skin penetration enhancer, and occlusion is known to enhance the permeability of skin [31]. Therefore, it is expected that they both have contributed significantly to the uptake of the plasmid into the skin, and thus, the induction of specific strong antibody responses by the plasmid DNA. Moreover, the DNA application area was also cleaned with an alcohol swab prior to hydration. Alcohol is a known skin penetration enhancer as well [31], and may have also contributed to the uptake of the plasmid into the skin. However, the extent to which the 70% alcohol may have contributed to the enhancement of the plasmid uptake/retention is expected to be minimal, if any, because the skin area was simply swiped with the alcohol swab 4–5 times and then immediately hydrated with warm water for 20 min. Any ethanol that was not evaporated from the skin surface would have been diluted significantly by the water hydration. Finally, it is worth pointing out that it is not likely that the occlusion, water hydration, and alcohol cleaning were responsible for the stronger antibody responses induced by the plasmid DNA applied onto the skin area where in the hair was plucked by ‘warm’ waxing, as compared to by ‘cold’ waxing, because all three procedures were applied in both cases.
The hair follicle growth cycle consists of three major phases: (i) anagen – the growth phase where cells proliferate to form the inner root sheath and migrate upward to form the hair shaft; (ii) catagen – the period where cell division ends, and the lower follicle segment dies; and (iii) telogen – the resting phase before the hair is shed [22]. The anagen phase can be divided into subphases, with each being characterized by cell proliferation giving rise to the hair shaft. The last subphase of anagen dictates the length of the hair shaft. Using DNA microarray assays, Ishimatsu-Tsuji et al. (2005) defined points in the hair cycle by different gene expression patterns following hair plucking using a wax and rosin mixture [16]. The period up to two days following hair plucking (early anagen) was defined as the defense response phase, where up-regulated genes were mainly inflammation related [16]. The period of three to six days following hair plucking is the mid-anagen phase and was defined as keratinocyte proliferation related processes [16]. Late anagen and early catagen phase were characterized by multiple processes including keratin intermediate filament formation [16]. Therefore, we sought to identify the optimal time to apply the plasmid DNA after ‘warm’ waxing-based hair depilation to induce the strongest immune responses. Interestingly, in mice the pGPA was applied 0, 2, or 5 days after ‘warm’ waxing-based hair plucking, or when the hair follicles were in the early or middle anagen stages, similar levels of anti-PA IgG responses were induced (Fig. 3A). However, when the pGPA was applied 10 days after the hair plucking, or when the hair follicles were in the late anagen stage, only a very weak anti-PA IgG response was detected (Fig. 3A). The anti-PA IgG responses were slightly biased towards IgG1 when the plasmid was applied onto the skin 0 or 2 days after hair depilation (Fig. 3B). However, when the plasmid was applied onto the skin 5 days following hair depilation, the anti-PA IgG responses were more biased towards IgG1 (Fig. 3 B). It is unclear why this change was observed. Nonetheless, it shows that the plasmid DNA needs to be applied within the early anagen and mid-anagen phases after the ‘warm’ waxing-based hair depilation to induce a strong immune response. The fact that transcutaneous DNA immunization immediately after the ‘warm’ wax-based hair depilation was able to induce a strong immune response is advantageous, because one will not have to wait for two or three days after the hair plucking for the hair follicles to enter the mid-anagen phase to apply the DNA. However, this finding is somewhat not in agreement with the expression of transfected genes at different time after hair removal, as reported by Domashenko et al. [10]. Domashenko and colleague applied a lipoplex composed of pFx-1 and pCMV-β onto skin areas of mice at various time points following hair removal (by Nair®) to test the concept that hair follicle cells express the transfected plasmid only at specific times during the growth cycle and found the expression of β-galactosidase only occurs during the first, second, and third days following the hair removal [10]. We chose not to complex the plasmid with cationic liposomes because data from our previous studies showed that complexing the DNA with cationic liposomes did not significantly improve the resultant immune responses [26]. Our data in Fig. 3A showed that the anti-PA immune responses induced by topically applied pGPA were hair cycle dependent as well, but the plasmid may be applied from day 0 to day 5 after the ‘warm’ waxing-based hair depilation to induce similarly strong antibody responses. When the pGPA was applied 5 days following the depilation, the PA63 gene must have been expressed to induce a strong anti-PA antibody response. It is unclear what lead to the strong immune response when the pGPA was applied 5 days after hair depilation, but as seen in Fig. 3F, a comparable amount of plasmid DNA was retained in skin when the plasmid was applied 5 days following hair depilation as when applied on day 0 and day 2. Of course, Domashenko et al. (2000) focused on the expression of the transfected gene in the hair follicles; they removed hair using Nair®, a chemical hair depilation cream, and complexed the pCMV-β with liposomes [10]. In contrast, the present study was focused on determining the serum antibody responses induced by topically applied plasmid DNA. Immune response is secondary to the expression of the (antigen) gene, and there was a previous report showing that the expression of the gene encoded by a plasmid DNA applied onto the skin was detected in the local draining lymph nodes as well [32].
In all above studies, the pGPA plasmid was used. The plasmid encodes a gene fragment of the B. anthracis protective antigen (PA63) protein and utilizes the mammalian expression vector pJW4303, which has been shown to allow the secretion of the expressed protein [18]. To determine the extent to which the secretion of the antigen protein had contributed to the resultant immune response, the PA63 gene fragment from pGPA was cloned into another mammalian expression vector (pCI), which does not allow the secretion of the expressed protein [19]. When the plasmid pGPA or pCPA was applied onto a skin area where the hair was plucked by ‘warm’ waxing, comparable anti-PA IgG responses were induced (Fig. 4A), indicating that the secretion of the antigen protein by the transfected cells into the intercellular spaces was not required for the PA63 to induce anti-PA responses. Similarly, both pGPA and pCPA induced strong anti-PA IgG responses when injected intramuscularly into mice (Fig. 4A). Although the anti-PA IgG responses induced by transcutaneous immunization were strong, they were both slightly biased towards IgG1, suggesting a CD4+ T-helper (Th2)-biased response (Fig. 4B). However, the anti-PA IgG responses induced by intramuscular injection of the pGPA or pCPA were more balanced between IgG1 and IgG2a (Fig. 4B). Therefore, the secretion of the PA63 protein did not alter the IgG1/IgG2a balance, but the route of administration did. The mechanism(s) of immune induction by the topically applied plasmid DNA are currently under investigation. It was likely by “cross-priming” by antigen-presenting cells (APC) that picked up the antigens expressed by the transfected follicular and interfollicular keratinocytes or by “direct-priming” by APC (e.g., dendritic cells) that directly took up the topically applied plasmid DNA [33]. Apparently, in either case, the antigen protein did not need to be secreted to induce a strong immune response.
In order to test whether the hair plucking approach of enhancing the immune responses induced after transcutaneous DNA immunization is applicable to an antigen other than the PA63, a plasmid that encodes the HIV-1 full-length env gp160 gene was applied onto a skin area where the hair was plucked by ‘warm’ waxing, and data in Fig. 5 showed that strong anti-gp160 IgG antibody responses were induced using the p69ZM651gp160-opt plasmid. Therefore, enhancing the immune responses induced by transcutaneous DNA immunization onto a skin wherein the hair had been plucked by ‘warm’ waxing is likely applicable to other antigens of interest as well.
Finally, transcutaneous DNA immunization by modifying the hair follicle growth stage is expected to be amenable to humans. Human hair follicles are considerably larger than mouse hair follicles. The density of the hair follicles on the human body is considerably less than on a mouse, allowing for the heat from the ‘warm’ wax to better open the hair pores and reducing the possibility of hair breakage. Therefore, non-invasive transcutaneous plasmid DNA immunization after ‘warm’ waxing of hair may hold great promise to humans, especially considering that ‘warm’ waxing is routinely used by humans to remove unwanted hair. The preauricular region of a human body has similar hair follicle density as in the lateral forehead [34], and thus may be a potential site for transcutaneous immunization using this approach. Transcutaneous DNA immunization after the waxing of hair may have the slight inconvenience of being a two-step procedure (i.e., hair plucking followed by DNA application), but researches may be initially focused on skin diseases such as acne, allergy, or psoriasis. Of course, the similar approach of transcutaneous DNA immunization is expected to be applicable in other animal models, and the ‘warm’ waxing-based hair depilation may be adopted to enhance follicular and interfollicular epidermal gene transfection for other gene therapy purposes as well.
5. CONCLUSIONS
Transcutaneous DNA immunization by applying plasmid DNA onto a skin area wherein the hair had been plucked by ‘warm’ waxing elicited specific antibody responses that were as strong as that when the plasmid DNA was injected intramuscularly. The ‘warm’ waxing-based hair plucking prior to the transcutaneous immunization enhanced the uptake (or retention) of the plasmid DNA in the skin application area and increased the expression of the transfected gene in follicular and interfollicular epidermis. The plasmid needed to be applied within 5 days after the plucking, or when the hair follicles were in the early or mid-anagen stages, to induce a strong immune response. The immune responses induced were comparable whether the antigen encoded by the plasmid was secreted by the transfected cells or cell surface-bound. Transcutaneous DNA immunization following ‘warm’ waxing-based hair depilation may represent a viable approach for non-invasive DNA immunization.
Supplementary Material
ACKNOWLEDGMENT
This work was supported in part by a NIAID grant (AI078304) to Z.C. The following reagent was obtained through the NIH AIDS Research and Reference Reagent Program, Division of AIDS, NIAID, NIH: p96ZM651gp160-opt from Drs. Y Li, F Gao, and BH Hahn."
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Shi Z, Curiel DT, Tang DC. DNA-based non-invasive vaccination onto the skin. Vaccine. 1999;17:2136–2141. doi: 10.1016/s0264-410x(98)00488-5. [DOI] [PubMed] [Google Scholar]
- 2.Tang DC, Shi Z, Curiel DT. Vaccination onto bare skin. Nature. 1997;388:729–730. doi: 10.1038/41917. [DOI] [PubMed] [Google Scholar]
- 3.Liu LJ, Watabe S, Yang J, Hamajima K, Ishii N, Hagiwara E, Onari K, Xin KQ, Okuda K. Topical application of HIV DNA vaccine with cytokine-expression plasmids induces strong antigen-specific immune responses. Vaccine. 2001;20:42–48. doi: 10.1016/s0264-410x(01)00324-3. [DOI] [PubMed] [Google Scholar]
- 4.Van Kampen KR, Shi Z, Gao P, Zhang J, Foster KW, Chen DT, Marks D, Elmets CA, Tang DC. Safety and immunogenicity of adenovirus-vectored nasal and epicutaneous influenza vaccines in humans. Vaccine. 2005;23:1029–1036. doi: 10.1016/j.vaccine.2004.07.043. [DOI] [PubMed] [Google Scholar]
- 5.Cui Z, Mumper RJ. The effect of co-administration of adjuvants with a nanoparticle-based genetic vaccine delivery system on the resulting immune responses. Eur J Pharm Biopharm. 2003;55:11–18. doi: 10.1016/s0939-6411(02)00129-7. [DOI] [PubMed] [Google Scholar]
- 6.Heckert RA, Elankumaran S, Oshop GL, Vakharia VN. A novel transcutaneous plasmid-dimethylsulfoxide delivery technique for avian nucleic acid immunization. Vet Immunol Immunopathol. 2002;89:67–81. doi: 10.1016/s0165-2427(02)00186-1. [DOI] [PubMed] [Google Scholar]
- 7.Babiuk S, Baca-Estrada ME, Pontarollo R, Foldvari M. Topical delivery of plasmid DNA using biphasic lipid vesicles (Biphasix) J Pharm Pharmacol. 2002;54:1609–1614. doi: 10.1211/002235702289. [DOI] [PubMed] [Google Scholar]
- 8.Cui Z, Mumper RJ. Topical immunization using nanoengineered genetic vaccines. J Control Release. 2002;81:173–184. doi: 10.1016/s0168-3659(02)00051-2. [DOI] [PubMed] [Google Scholar]
- 9.Alexander MY, Akhurst RJ. Liposome-medicated gene transfer and expression via the skin. Hum Mol Genet. 1995;4:2279–2285. doi: 10.1093/hmg/4.12.2279. [DOI] [PubMed] [Google Scholar]
- 10.Domashenko A, Gupta S, Cotsarelis G. Efficient delivery of transgenes to human hair follicle progenitor cells using topical lipoplex. Nat Biotechnol. 2000;18:420–423. doi: 10.1038/74480. [DOI] [PubMed] [Google Scholar]
- 11.Fan H, Lin Q, Morrissey GR, Khavari PA. Immunization via hair follicles by topical application of naked DNA to normal skin. Nat Biotechnol. 1999;17:870–872. doi: 10.1038/12856. [DOI] [PubMed] [Google Scholar]
- 12.Li L, Hoffman RM. The feasibility of targeted selective gene therapy of the hair follicle. Nat Med. 1995;1:705–706. doi: 10.1038/nm0795-705. [DOI] [PubMed] [Google Scholar]
- 13.Wu H, Ramachandran C, Bielinska AU, Kingzett K, Sun R, Weiner ND, Roessler BJ. Topical transfection using plasmid DNA in a water-in-oil nanoemulsion. Int J Pharm. 2001;221:23–34. doi: 10.1016/s0378-5173(01)00672-x. [DOI] [PubMed] [Google Scholar]
- 14.Lademann J, Otberg N, Jacobi U, Hoffman RM, Blume-Peytavi U. Follicular penetration and targeting. J Investig Dermatol Symp Proc. 2005;10:301–303. doi: 10.1111/j.1087-0024.2005.10121.x. [DOI] [PubMed] [Google Scholar]
- 15.Shaker DS, Sloat BR, Le UM, Lohr CV, Yanasarn N, Fischer KA, Cui Z. Immunization by application of DNA vaccine onto a skin area wherein the hair follicles have been induced into anagen-onset stage. Mol Ther. 2007;15:2037–2043. doi: 10.1038/sj.mt.6300286. [DOI] [PubMed] [Google Scholar]
- 16.Ishimatsu-Tsuji Y, Moro O, Kishimoto J. Expression profiling and cellular localization of genes associated with the hair cycle induced by wax depilation. J Invest Dermatol. 2005;125:410–420. doi: 10.1111/j.0022-202X.2005.23825.x. [DOI] [PubMed] [Google Scholar]
- 17.Muller-Rover S, Handjiski B, van der Veen C, Eichmuller S, Foitzik K, McKay IA, Stenn KS, Paus R. A comprehensive guide for the accurate classification of murine hair follicles in distinct hair cycle stages. J Invest Dermatol. 2001;117:3–15. doi: 10.1046/j.0022-202x.2001.01377.x. [DOI] [PubMed] [Google Scholar]
- 18.Gu ML, Leppla SH, Klinman DM. Protection against anthrax toxin by vaccination with a DNA plasmid encoding anthrax protective antigen. Vaccine. 1999;17:340–344. doi: 10.1016/s0264-410x(98)00210-2. [DOI] [PubMed] [Google Scholar]
- 19.Price BM, Liner AL, Park S, Leppla SH, Mateczun A, Galloway DR. Protection against anthrax lethal toxin challenge by genetic immunization with a plasmid encoding the lethal factor protein. Infect Immun. 2001;69:4509–4515. doi: 10.1128/IAI.69.7.4509-4515.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gao F, Li Y, Decker JM, Peyerl FW, Bibollet-Ruche F, Rodenburg CM, Chen Y, Shaw DR, Allen S, Musonda R, Shaw GM, Zajac AJ, Letvin N, Hahn BH. Codon usage optimization of HIV type 1 subtype C gag, pol, env, and nef genes: in vitro expression and immune responses in DNA-vaccinated mice. AIDS Res Hum Retroviruses. 2003;19:817–823. doi: 10.1089/088922203769232610. [DOI] [PubMed] [Google Scholar]
- 21.MacGregor GR, Caskey CT. Construction of plasmids that express E. coli beta-galactosidase in mammalian cells. Nucleic Acids Res. 1989;17:2365. doi: 10.1093/nar/17.6.2365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Paus R. Principles of hair cycle control. J Dermatol. 1998;25:793–802. doi: 10.1111/j.1346-8138.1998.tb02507.x. [DOI] [PubMed] [Google Scholar]
- 23.Wilson C, Cotsarelis G, Wei ZG, Fryer E, Margolis-Fryer J, Ostead M, Tokarek R, Sun TT, Lavker RM. Cells within the bulge region of mouse hair follicle transiently proliferate during early anagen: heterogeneity and functional differences of various hair cycles. Differentiation. 1994;55:127–136. doi: 10.1046/j.1432-0436.1994.5520127.x. [DOI] [PubMed] [Google Scholar]
- 24.Skountzou I, Quan FS, Jacob J, Compans RW, Kang SM. Transcutaneous immunization with inactivated influenza virus induces protective immune responses. Vaccine. 2006;24:6110–6119. doi: 10.1016/j.vaccine.2006.05.014. [DOI] [PubMed] [Google Scholar]
- 25.Zhu C, Yu J, Yang Z, Davis K, Rios H, Wang B, Glenn G, Boedeker EC. Protection against Shiga toxin-producing Escherichia coli infection by transcutaneous immunization with Shiga toxin subunit B. Clin Vaccine Immunol. 2008;15:359–366. doi: 10.1128/CVI.00399-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yu Z, Chung WG, Sloat BR, Lohr CV, Weiss R, Rodriguez BL, Li X, Cui Z. The extent of the uptake of plasmid into the skin determines the immune responses induced by a DNA vaccine applied topically onto the skin. J Pharm Pharmacol. 2011;63:199–205. doi: 10.1111/j.2042-7158.2010.01219.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sloat BR, Cui Z. Nasal immunization with a dual antigen anthrax vaccine induced strong mucosal and systemic immune responses against toxins and bacilli. Vaccine. 2006;24:6405–6413. doi: 10.1016/j.vaccine.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 28.Moayeri M, Leppla SH. Cellular and systemic effects of anthrax lethal toxin and edema toxin. Mol Aspects Med. 2009;30:439–455. doi: 10.1016/j.mam.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Friedlander AM, Little SF. Advances in the development of next-generation anthrax vaccines. Vaccine. 2009;27 Suppl 4:D28–D32. doi: 10.1016/j.vaccine.2009.08.102. [DOI] [PubMed] [Google Scholar]
- 30.Gurunathan S, Klinman DM, Seder RA. DNA vaccines: immunology, application, and optimization. Annu Rev Immunol. 2000;18:927–974. doi: 10.1146/annurev.immunol.18.1.927. [DOI] [PubMed] [Google Scholar]
- 31.Guy RH, Hadgraft J. Transdermal Drug Delivery. 2nd Ed. New York, Basel: Marcel Dekker, Inc.; 2003. [Google Scholar]
- 32.Kang MJ, Kim CK, Kim MY, Hwang TS, Kang SY, Kim WK, Ko JJ, Oh YK. Skin permeation, biodistribution, and expression of topically applied plasmid DNA. J Gene Med. 2004;6:1238–1246. doi: 10.1002/jgm.620. [DOI] [PubMed] [Google Scholar]
- 33.Cui Z. DNA vaccine. Adv Genet. 2005;54:257–289. doi: 10.1016/S0065-2660(05)54011-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pagnoni A, Kligman AM, el Gammal S, Stoudemayer T. Determination of density of follicles on various regions of the face by cyanoacrylate biopsy: correlation with sebum output. Br J Dermatol. 1994;131:862–865. doi: 10.1111/j.1365-2133.1994.tb08590.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.