Abstract
Context
The clinical syndrome of lumbar spinal stenosis (LSS) is a common diagnosis in older adults presenting with lower extremity pain.
Objective
To systematically review the accuracy of the clinical examination for the diagnosis of the clinical syndrome of LSS.
Data Sources
MEDLINE, EMBASE, and CINAHL searches of articles published from January 1966 to September 2010.
Study Selection
Studies were included if they contained adequate data on the accuracy of the history and physical examination for diagnosing the clinical syndrome of LSS, using a reference standard of expert opinion with radiographic or anatomic confirmation.
Data Extraction
Two authors independently reviewed each study to determine eligibility, extract data, and appraise levels of evidence.
Data Synthesis
Four studies evaluating 741 patients were identified. Among patients with lower extremity pain, the likelihood of the clinical syndrome of LSS was increased for individuals older than 70 years (likelihood ratio [LR], 2.0; 95% confidence interval [CI], 1.6–2.5), and was decreased for those younger than 60 years (LR, 0.40; 95% CI, 0.29–0.57). The most useful symptoms for increasing the likelihood of the clinical syndrome of LSS were having no pain when seated (LR, 7.4; 95% CI, 1.9–30), improvement of symptoms when bending forward (LR, 6.4; 95% CI, 4.1–9.9), the presence of bilateral buttock or leg pain (LR, 6.3; 95% CI, 3.1–13), and neurogenic claudication (LR, 3.7; 95% CI, 2.9–4.8). Absence of neurogenic claudication (LR, 0.23; 95% CI, 0.17–0.31) decreased the likelihood of the diagnosis. A wide-based gait (LR, 13; 95% CI, 1.9–95) and abnormal Romberg test result (LR, 4.2; 95% CI, 1.4–13) increased the likelihood of the clinical syndrome of LSS. A score of 7 or higher on a diagnostic support tool including history and examination findings increased the likelihood of the clinical syndrome of LSS (LR, 3.3; 95% CI, 2.7–4.0), while a score lower than 7 made the diagnosis much less likely (LR, 0.10; 95% CI, 0.06–0.16).
Conclusions
The diagnosis of the clinical syndrome of LSS requires the appropriate clinical picture and radiographic findings. Absence of pain when seated and improvement of symptoms when bending forward are the most useful individual findings. Combinations of findings are most useful for identifying patients who are unlikely to have the diagnosis.
CLINICAL SCENARIO
In the following cases, the clinician would like to know if the patient has the clinical syndrome of lumbar spinal stenosis (LSS).
Case 1
A 67-year-old woman for the past year reports low lumbar pain while she is standing or walking. She also develops dull, aching right posterior thigh pain after ambulating for several minutes, as well as mild tingling on the soles of both feet. Her pain is typically relieved when she bends forward while standing. On examination, no abnormalities are found on provocative maneuvers, sensory, motor, reflex, or balance testing.
Case 2
A 74-year-old man with no major medical problems reports right-sided low back and right calf pain that are worse with prolonged sitting and standing. Walking neither improves nor worsens his leg pain, and no particular position provides relief. On examination, the patient has no change in pain with bending forward or backward, excellent peripheral pulses, and a positive right straight leg raise. The neuromuscular examination findings are otherwise normal.
WHY IS THE DIAGNOSIS IMPORTANT?
Lower extremity pain in the setting of low back pain affects 12% of older men in the general community1 and 21% of older adults in retirement communities.2 The clinical syndrome of LSS involves lower extremity pain, numbness, or weakness, which is frequently seen in the setting of low back pain. However, other causes of lower extremity pain with or without low back pain abound. Because the clinical syndrome of LSS may require specific medical advice and treatment, the accuracy of the stenosis diagnosis is paramount. Given that the characteristic signs and symptoms of this clinical syndrome are common, the primary care clinician is left with the question: “Which patients with lower extremity and back pain have the clinical syndrome of LSS, and which do not?”
A diagnosis of the clinical syndrome of LSS requires both the presence of characteristic symptoms and signs and radiographic or anatomic confirmation of narrowing or stenosis of the lumbar spinal canal.3 Because many individuals with radiographic or anatomic lumbar spinal canal stenosis may not demonstrate the symptoms and signs of the clinical syndrome of LSS, the radiographic or anatomic finding of stenosis is necessary, but not sufficient, to establish a diagnosis of the clinical syndrome. The primary care clinician should have the objective of recognizing the clinical syndrome of LSS, while keeping in mind the fact that, in common practice, the general term stenosis may be used by other clinicians without specifying whether they are referring to the clinical syndrome of LSS, or radiographic LSS alone. This may lead to confusion for both clinicians and patients. In this article, we systematically review the accuracy of the clinical examination for the diagnosis of the clinical syndrome of LSS. We use the terms radiographic or anatomic LSS when referring specifically to the pathoanatomic changes of spinal canal narrowing, which may occur with or without the symptoms manifested in the clinical syndrome. The terminology used in this article is defined in the Box.
Box. Common Terminology Used in Reference to the Clinical Syndrome of Lumbar Spinal Stenosis (LSS).
Clinical Syndrome of LSS
Requires both the presence of
A characteristic clinical presentation, including neurogenic claudication, radicular pain, or both, and
Radiographic or anatomic LSS
Neurogenic claudication
Pain or other discomfort with walking or prolonged standing that radiates into one or both lower extremities and is typically relieved by rest or lumbar flexion
Radicular pain
Unilateral or bilateral radiating pain in the distribution of 1 or more dermatomes that is present irrespective of activity
Radiographic LSSa
The finding of spinal canal narrowing on cross-sectional imaging
Central canal stenosis
Central canal narrowing between the medial edges of the 2 zygapophysial (facet) joints
Lateral recess or subarticular stenosis
Canal narrowing between the medial edge of the zygapophysial (facet) joint and the medial pedicle border4
Neuroforaminal stenosis
Narrowing of the neural foramina defined by the medial and lateral pedicle borders
Anatomic LSS
The finding of spinal canal narrowing noted intraoperatively
Signs and Symptoms of the Clinical Syndrome of LSS
The diagnosis of the clinical syndrome of LSS is complicated by the range of possible clinical presentations. The neurogenic claudication and radicular pain subtypes of the clinical syndrome are best described in the literature,6–9 and have been used as clinical criteria for inclusion in the Spine Patient Outcomes Research Trial (SPORT), the large strandomized trial of treatment for the clinical syndrome of LSS todate.10,11 The most common symptom associated with the clinical syndrome of LSS is neurogenic claudication, a variable pain or discomfort with walking or prolonged standing that radiates beyond the spinal area into one or both buttocks, thighs, lower legs, or feet.3 Neurogenic claudication classically exhibits typical provocative features, such as improvement with sitting or lumbarflexion, and worsening with lumbar extension. Some individuals may not experience marked pain or discomfort but present instead with more subtle symptoms including a subjective feeling of weakness, abnormal sensations, or fatigue affecting the lower extremities, or signs including weakness, sensory loss, and gait changes.12,13 In contrast, radicular pain or polyradicular pain may also be present in the clinical syndrome of LSS6–8 and may often not exhibit the provocative features seen in neurogenic claudication. The neurogenic claudication and radicular subtypes of the clinical syndrome of LSS may overlap, contributing to the heterogeneous presentation of the clinical syndrome.14 Low back pain is often considered a characteristic feature of the clinical syndrome of LSS.15 Indeed, a history of low back pain is sometimes used as a feature to distinguish vascular claudication from neurogenic claudication.16 Nevertheless, surgery for the clinical syndrome of LSS is typically performed to relieve lower extremity pain, and not for the relief of low back pain.17 The role of low back pain as part of the clinical syndrome of LSS is controversial, and it is possible that the association of low back pain and the clinical syndrome of LSS is driven in large part by the common factor of spinal degeneration causal to both conditions.
Radiographic and Anatomic LSS
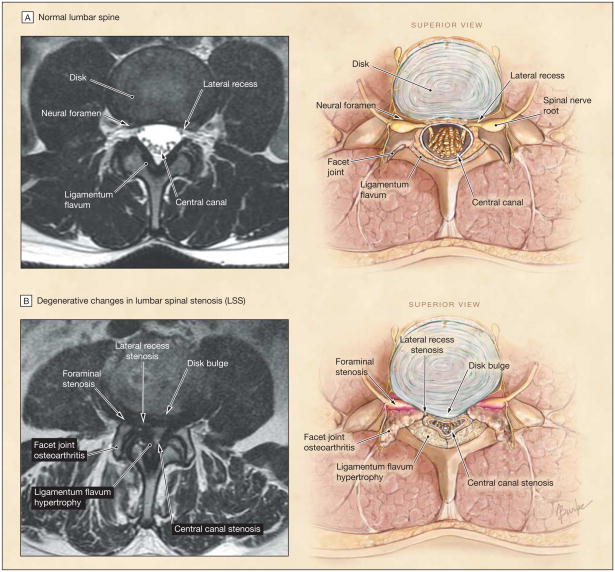
Anatomic stenosis may occur in the central spinal canal, in the area under the facet joints (subarticular or lateral recess stenosis), or more laterally, in the neural foramina (Figure). Acquired degenerative spinal stenosis is the most common type of anatomic LSS and is often due to a combination of disk bulging or herniation, hypertrophy of osteoarthritic facet joints, and hypertrophy or in folding of the ligamentum flavum.3 Biomechanical interrelationships between these spinal structures, as well as supporting muscles and ligaments, are thought to be important to the development of anatomic LSS over time.18,19 Although a commonly held clinical paradigm connects lumbar central canal stenosis to the symptom of neurogenic claudication and lateral recess or for aminal stenosis to radicular symptoms,20–22 diverse clinical presentations can be seen in patients with similar radiographic findings.23
Figure. Radiographic Features of Lumbar Spinal Stenosis.
A, left, axial T2-weighted magnetic resonance image (MRI) at the L3–L4 level; right, normal radiographic appearance of the spinal canal includes patent central canal, lateral recesses, and neural foramina. B, left, axial T2-weighted MRI at L4–L5 level; right, radiographic features seen with lumbar spinal stenosis include intervertebral disk bulging, ligamentum flavum hypertrophy, and facet joint osteorthritis. Stenosis may occur in the central canal, the lateral recess, or the neural foramina.
The available data on radiographic LSS prevalence are limited to assessments of central canal stenosis and by the use of variable definitions of stenosis and small sample sizes. The prevalence of radiographic LSS in a community-based sample of older adults aged 60 to 69 years was 47% for relative radiographic LSS (≤12 mm sagittal diameter) and 19% for absolute radiographic LSS (≤10 mm sagittal diameter).24 Although criteria for qualitative radiographic LSS grading vary between different clinicians, a general guideline classifies mild stenosis as narrowing of the normal central canal cross-sectional area by one-third or less, moderate stenosis by between one-third and two-thirds, and severe stenosis as more than two-thirds.4 The prevalence of radiographic LSS using qualitative criteria in asymptomatic older adults 55 years or older has been estimated at 21% to 30% for moderate stenosis and 6% to 7% for severe stenosis.25 These data make it clear that incidental radiographic LSS on spine magnetic resonance imaging (MRI) is common in asymptomatic patients. This underscores the importance of the history and physical examination in determining whether the clinical presentation reflects the clinical syndrome of LSS or an alternative diagnosis.
Differential Diagnosis of the Clinical Syndrome of LSS
Lower extremity pain with or without low back pain, which is seen in the clinical syndrome of LSS, may also be found in other spinal disorders, extraspinal musculoskeletal disorders, and other medical diagnoses.26 Table 1 depicts common problems that affect older adults with lower extremity pain with or without low back pain. Vascular intermittent claudication due to peripheral arterial disease in particular is often considered when leg pain occurs with walking. Unlike neurogenic claudication, vascular claudication is typically not improved by changes in posture such as lumbar flexion.27 The discomfort of vascular claudication may be more consistently reproducible with a specific distance and time of ambulation than neurogenic claudication.16 When the diagnosis is uncertain by clinical evaluation, it can be confirmed by diagnostic testing including ankle brachial indices (ABIs), duplex ultrasound, computed tomographic angiography, or magnetic resonance angiography.16 Lower extremity pain can also be caused by other spinal and extraspinal musculoskeletal diagnoses, including lumbosacral radicular pain due to nerve root impingement, referred pain from spinal structures including the lumbar intervertebral disks and zygapophysial (facet) joints, lumbar vertebral compression fractures, and hip osteoarthritis.3 Low back pain when present may be conceptualized in terms of specific pain generators28 (Table 1), but it is also influenced by psychosocial factors unrelated to pathoanatomy.29 The differential diagnosis of the clinical syndrome of LSS is complicated by the frequent coexistence of many of the above-described conditions in older adults.
Table 1.
Differential Diagnosis for Lower Extremity Pain With or Without Low Back Pain
| Diagnosis | Clinical Characteristics |
|---|---|
| Spinal disorders | |
| Lumbosacral radicular pain secondary to nerve root impingement | Lumbosacral radicular pain (with or without low back pain) in the setting of lumbar disk herniation may be accompanied by a positive straight leg raise test or femoral stretch test |
|
| |
| Referred pain from lumbar spine structures (zygapophysial [facet] joints, intervertebral disks) | Low back pain and proximal lower extremity referred pain in nonradicular pattern, usually not below the knee |
|
| |
| Lumbar vertebral compression fracture | Low back pain or thoracic pain in an older patient, often of acute onset, with or without specific history of recent injury |
|
| |
| Extraspinal disorders | |
| Musculoskeletal diagnoses | |
| Hip joint referred pain | Groin pain, buttock pain, with or without low back pain, or referred symptoms distal to the knee, often with weight bearing; may have limited internal rotation of the hip |
|
| |
| Sacroiliac joint referred pain | Low back pain overlying the posterior superior iliac spine, with or without radiating posterior buttock and lower extremity pain |
|
| |
| Trochanteric bursitis | Lateral hip and thigh pain, with tenderness over the greater trochanter; low back pain may or may not be present |
|
| |
| Piriformis syndrome | Pain localized over the piriformis muscle in the buttocks, with or without radiating posterior buttock and lower extremity pain; tight hip external rotators may be appreciated |
|
| |
| Muscle strain or tears | Strains or tears to hip adductors, hip abductors (gluteus medius and minimus), and hip flexors may present with lower extremity pain, with or without low back pain. |
|
| |
| Myofascial referred pain | Pain can be reproduced by pressing on tender points or trigger points (eg, gluteus medius and minimus) |
|
| |
| Other diagnoses | |
| Intermittent claudication due to peripheral arterial disease | Leg-muscle discomfort, cramping, tightness, or tiredness in the buttock or lower extremity that is induced by exercise, often consistently reproduced after walking a certain distance, relieved rapidly with rest, eased with standing, and not affected by trunk posture12,16; decreased pulses or impaired ankle brachial index may be present |
|
| |
| Compartment syndrome | Tightness in the calf after exercise, induced by strenuous exercise, and relieved slowly with limb elevation |
|
| |
| Peripheral neuropathy | Pain, numbness, and tingling in the distal lower extremities, particularly the feet and ankles, not substantially affected by posture or exertion |
|
| |
| Visceral referred pain | Low back pain, lower extremity pain, or both may be referred from structures in the abdomen and pelvis, including the gastrointestinal tract and genitourinary system |
In common practice, a referral for tests not readily accessible in most primary care clinics may aid in distinguishing the clinical syndrome of LSS from other diagnoses. Bicycle testing and treadmill testing protocols can be performed in physical therapy or rehabilitation centers and may yield useful information about whether the clinical syndrome of LSS is likely.30 Electrodiagnostic testing may also yield information about other potential masqueraders of the clinical syndrome of LSS, including generalized peripheral neuropathies and focal neuropathies.
METHODS
The MEDLINE (1966–2010), EMBASE (1980–2010), and CINAHL (1982–2010) databases were searched for English-language diagnostic accuracy studies of the clinical syndrome of LSS in adults (eMethods available at www.jama.com). Two reviewers (P.S. and L.K.) reviewed all abstracts to assess adherence to review criteria. Inclusion criteria consisted of the following: (1) diagnostic accuracy study of the history, physical examination, or both for the diagnosis of the clinical syndrome of LSS, with or without spondylolisthesis (a displacement of 1 vertebra atop another); (2) reporting of sensitivity, specificity, accuracy, predictive values, likelihood ratios, or prevalence in cases and controls; (3) index tests that were either clearly specified or described or that were used in common practice and could be performed in a routine clinic visit without specialized equipment; and (4) use of an appropriate reference standard that was clearly specified or described. Studies were excluded if they consisted of a mixed population including stenosis in nonlumbar areas or red flag conditions31 (ie, trauma, infection, or malignancy), if they included only patients with scoliosis or congenital stenosis, or if they consisted of case series. We determined quality using levels of evidence for the Rational Clinical Examination.32
The gold standard for diagnosis of the clinical syndrome of LSS is the impression of an expert clinician, with radiographic or anatomic corroboration of spinal canal narrowing. The expert clinician impression is a common reference standard in musculoskeletal medicine because the production of pain cannot be assessed by a single laboratory or imaging test.33 We required expert opinion based on a combination of clinical assessment and imaging evaluation by computed tomography (CT), MRI, or myelography, or expert opinion based on a combination of clinical assessment and a clearly defined, prospectively established protocol for intraoperative evaluation. Simple surgical confirmation or verification of a prior diagnosis without clearly stated pre hoc criteria for inclusion and exclusion was considered insufficient as an intraoperative diagnosis.
Sensitivities and specificities were calculated from the raw data where presented, and contingency tables were created using reported prevalence, sensitivities, and specificities where raw data were not available. Likelihood ratios (LRs) for the diagnosis of the clinical syndrome of LSS were calculated for positive test results [LR+ = (sensitivity/(1 − specificity)] and negative test results [LR− =(1 − sensitivity)/specificity]. We calculated 95% confidence intervals (CIs) according to the method of Simel et al.34 We used Excel 2007 (Microsoft, Redmond, Washington) for statistical analyses and checked these values using SAS version 9.2 (SAS Institute Inc, Cary, North Carolina).
RESULTS
Study Characteristics
The literature review for diagnostic accuracy studies identified 4722 citations with 20 additional citations identified from the bibliographies of review articles and the authors’ libraries (eFigure); 118 full-text articles were retrieved for full assessment. Four articles evaluating 741 patients were included in the final review.35–38 One population was studied in 2 separate reports: the first involved history and physical examination findings, and the second, questionnaire items (Table 2).35,36
Table 2.
Study Characteristics
| Source | No. (%) of Patients With Clinical Syndrome of LSS | Level of Evidencea | Recruitment Method | Presenting Symptoms, Age, y | Setting | Diagnostic Test | Reference Standard |
|---|---|---|---|---|---|---|---|
| Konno et al,35 2007b | 469 (47) | 1 | Consecutive patients | Pain or numbness in the legs, mean (SD), 65 (14) | Specialty and primary care | History and physical examination | Consensus diagnostic impression of expert physicians, confirmation by x-rays and MRI |
| Sugioka et al,36 2008b | 374 (47) | 1 | Consecutive patients | Pain or numbness in the legs, mean (SD), 65 (14)c | Specialty and primary care | Questionnaire items | Consensus diagnostic impression of expert physicians, confirmation by x-rays and MRI |
| Ljunggren,37 1991 | 179 (44) | 3 | Consecutive patients | Low back pain or sciatica | Specialty | Questionnaire items | Diagnosis by history, physical, x-rays, and myelography |
| Katz et al,38 1995 | 93 (46) | 3 | Consecutive patients | Low back pain, 65 (range, 40–91) | Specialty | History and physical examination | Diagnostic impression of expert physicians, with radiologic confirmation by MRI or CT |
Abbreviations: CT, computed tomography; LSS, lumbar spinal stenosis, MRI, magnetic resonance imaging.
From the Rational Clinical Examination series.32
Studies were reported separately on the same study sample.
Estimates from the complete study sample (derivation + validation cohorts).
Prevalence of the Clinical Syndrome of LSS
The prevalence of the clinical syndrome of LSS in the eligible diagnostic accuracy studies varied from 44% to 49%. The highest quality study included approximately one-third of patients recruited directly from primary care clinics and reported a prevalence of the clinical syndrome of LSS of 47% in adults with symptoms of pain or numbness in the lower extremities.35 These patients had a mean (SD) age of 65 (14) years and 54% were women.
Accuracy of Historical Features and Symptoms
The performance characteristics of all clinically relevant tests with LR point estimates of 2.0 and higher or 0.50 or less are listed in Table 3 (eTable 1 and eTable 2 include complete data of all findings and are available at www.jama.com). These thresholds were defined by some authors as producing small but meaningful changes in posttest probability.39
Table 3.
Diagnostic Accuracy of History and Physical Examination
| Test | Sensitivity (95% CI) | Specificity (95% CI) | Positive LR (95% CI) | Negative LR (95% CI) |
|---|---|---|---|---|
| Historical features | ||||
| Age, y | ||||
| Age >65 (vs ≤65)38 | 0.77 (0.64–0.89) | 0.69 (0.53–0.85) | 2.5 (1.4–4.2) | 0.34 (0.19–0.61) |
|
| ||||
| >7035a | NA | NA | 2.0 (1.6–2.5) | |
|
| ||||
| <6035a | NA | NA | 0.40 (0.29–0.57) | |
|
| ||||
| Comorbidities | ||||
| Orthopedic disease36 | 0.18 (0.13–0.24) | 0.91 (0.87–0.95) | 2.0 (1.2–3.5) | 0.90 (0.83–0.98) |
|
| ||||
| Pain locations | ||||
| Bilateral buttock or leg37 | 0.51 (0.40–0.62) | 0.92 (0.87–0.97) | 6.3 (3.1–13) | 0.54 (0.43–0.68) |
|
| ||||
| Pain below buttocks38 | 0.88 (0.79–0.98) | 0.34 (0.18–0.51) | 1.4 (1.0–1.8) | 0.34 (0.13–0.88) |
|
| ||||
| Thigh37 | 0.95 (0.90–1.0) | 0.14 (0.07–0.21) | 1.1 (1.0–1.2) | 0.36 (0.12–1.1) |
|
| ||||
| Gluteal37 | 0.84 (0.75–0.92) | 0.05 (0.01–0.09) | 0.88 (0.79–0.98) | 3.3 (1.2–8.8) |
|
| ||||
| Symptoms reproduced by specific actions | ||||
| No pain when seated38 | 0.47 (0.32–0.61) | 0.94 (0.85–1.0) | 7.4 (1.9–30) | 0.57 (0.43–0.76) |
|
| ||||
| Burning sensation around the buttocks, Intermittent priapism associated with walking, or both35 | 0.06 (0.03–0.09) | 0.99 (0.98–1.0) | 7.2 (1.6–32) | 0.95 (0.92–0.98) |
|
| ||||
| Improvement when bending forward35 | 0.52 (0.45–0.58) | 0.92 (0.88–0.95) | 6.4 (4.1–9.9) | 0.52 (0.46–0.60) |
|
| ||||
| Neurogenic claudication35 | 0.82 (0.77–0.87) | 0.78 (0.73–0.83) | 3.7 (2.9–4.8) | 0.23 (0.17–0.31) |
|
| ||||
| Improve when seated38 | 0.51 (0.36–0.66) | 0.84 (0.72–0.97) | 3.3 (1.4–7.7) | 0.58 (0.41–0.81) |
|
| ||||
| Exacerbation when standing up35 | 0.68 (0.62–0.74) | 0.70 (0.65–0.76) | 2.3 (1.8–2.8) | 0.46 (0.37–0.56) |
|
| ||||
| Exacerbated while standing up36 | 0.92 (0.88–0.96) | 0.21 (0.15–0.27) | 1.2 (1.1–1.3) | 0.38 (0.21–0.69) |
|
| ||||
| Other symptoms | ||||
| Urinary disturbance35 | 0.14 (0.09–0.19) | 0.98 (0.96–1.0) | 6.9 (2.7–17) | 0.88 (0.83–0.93) |
|
| ||||
| Numbness of perineal region35 | 0.05 (0.02–0.07) | 0.99 (0.97–1.0) | 3.7 (1.0–13) | 0.97 (0.94–1.0) |
|
| ||||
| Bilateral plantar numbness35 | 0.27 (0.21–0.33) | 0.87 (0.83–0.92) | 2.2 (1.4–3.2) | 0.84 (0.76–0.92) |
|
| ||||
| Treatment for symptoms needs to be repeated every year36 | 0.40 (0.33–0.47) | 0.80 (0.75–0.86) | 2.0 (1.5–2.8) | 0.75 (0.65–0.86) |
|
| ||||
| Wake up to urinate at night36 | 0.86 (0.81–0.91) | 0.27 (0.21–0.33) | 1.2 (1.1–1.3) | 0.50 (0.33–0.78) |
|
| ||||
| Physical examination | ||||
| Provocative tests | ||||
|
| ||||
| No pain with flexion38 | 0.79 (0.67–0.91) | 0.44 (0.27–0.61) | 1.4 (1.0–2.0) | 0.48 (0.24–0.96) |
|
| ||||
| Symptoms induced by having patients bend forward35 | 0.18 (0.13–0.23) | 0.63 (0.57–0.69) | 0.48 (0.34–0.66) | 1.3 (1.2–1.5) |
|
| ||||
| Neuromuscular tests | ||||
| Wide-based gait38 | 0.42 (0.27–0.57) | 0.97 (0.91–1.0) | 13 (1.9–95) | 0.60 (0.46–0.78) |
|
| ||||
| Abnormal Romberg test result38b | 0.40 (0.25–0.54) | 0.91 (0.81–1.0) | 4.2 (1.4–13) | 0.67 (0.51–0.87) |
|
| ||||
| Vibration deficit38 | 0.53 (0.39–0.68) | 0.81 (0.68–0.95) | 2.8 (1.3–6.2) | 0.57 (0.40–0.82) |
|
| ||||
| Pinprick deficit38 | 0.47 (0.32–0.61) | 0.81 (0.68–0.95) | 2.5 (1.1–5.5) | 0.66 (0.48–0.91) |
|
| ||||
| Weakness38 | 0.47 (0.32–0.61) | 0.78 (0.64–0.92) | 2.1 (1.0–4.4) | 0.69 (0.49–0.96) |
|
| ||||
| Absent Achilles reflex38 | 0.47 (0.32–0.61) | 0.78 (0.64–0.92) | 2.1 (1.0–4.4) | 0.69 (0.49–0.96) |
Abbreviations: CI, confidence interval; LR, likelihood ratio; NA, not applicable.
Multilevel (ordinal) LR.
Modified Romberg maneuver performed with patient’s feet together and eyes closed for 10 seconds; result abnormal if compensatory movements required to keep feet planted.
Age and Comorbidities
The likelihood of the clinical syndrome of LSS increases with age, especially for individuals older than 70 years (LR, 2.0; 95% CI, 1.6–2.5). Patients younger than 60 years are less likely to have the clinical syndrome of LSS (LR, 0.40; 95% CI, 0.29–0.57). Concurrent orthopedic problems such as osteoarthritis, inflammatory arthritis, and fractures increase the likelihood of the clinical syndrome of LSS (LR, 2.0; 95% CI, 1.2–3.5).
Symptoms
Among the most useful symptoms when examined in isolation were those that described pain location and provocative associations. The most useful symptoms for increasing the likelihood of the clinical syndrome of LSS were having no pain when seated (LR, 7.4; 95% CI, 1.9–30), having an unexplained urinary disturbance (LR, 6.9; 95% CI, 2.7–17), improvement of symptoms when bending forward (LR, 6.4; 95% CI, 4.1–9.9), the presence of bilateral buttock or leg pain (LR, 6.3; 95% CI, 3.1–13), or neurogenic claudication (LR, 3.7; 95% CI, 2.9–4.8). The presence of symptoms thought to be related to cauda equina syndrome, including a burning sensation around the buttocks, intermittent priapism associated with walking, or both increased the likelihood of the clinical syndrome of LSS (LR, 7.2; 95% CI, 1.6–32). However, these symptoms were insensitive and present in only 6% of patients. The absence of neurogenic claudication (LR, 0.23; 95% CI, 0.17–0.31) was the most useful symptom for decreasing the likelihood of the clinical syndrome of LSS when test results were negative.
Accuracy of the Physical Examination
Physical examination tests taken in isolation were not as useful as symptoms (Table 3). A wide-based gait (LR, 13; 95% CI, 1.9–95) and an abnormal Romberg test result (LR, 4.2; 95% CI, 1.4–13) increased the likelihood of the clinical syndrome of LSS. Two separate studies examined the effects of lumbar flexion on pain and reached similar conclusions: one study found pain with lumbar flexion to have an LR of 0.48 (95% CI, 0.24–0.96),38 and a second study found symptoms induced by bending forward to have an LR of 0.48 (95% CI, 0.34–0.66).35
Accuracy of the Clinical Examination in Multivariate Analyses
Certain individual tests may be highly intercorrelated. In these instances, the independent value of the second test is diminished once the value of the first test is accounted for. Multivariate analyses can overcome this problem and identify the independent, incremental value of diagnostic tests in the presence of other tests. Three studies examined tests in multivariate analyses.35,36,38 One study found that increased age (in years), having no pain when seated, a wide based gait, and having thigh pain with 30 seconds of lumbar extension were independently associated with the degree of expert physician confidence in the diagnosis of the clinical syndrome of LSS.38 Two studies examined multivariate predictors of the clinical syndrome of LSS in the same sample of patients and used predictor variables that were independently associated with the diagnosis to create risk scores for diagnosing the clinical syndrome of LSS35,36 (Table 4). A score of 7 or higher on a clinical diagnostic support tool including history and examination findings increased the likelihood of the clinical syndrome of LSS35 (LR, 3.3; 95% CI, 2.7–4.0; eTable 3 available at www.jama.com). Therefore, although sensitivity was optimized by the combination of history and examination findings, a lower overall specificity contributed to a lower positive LR than what was seen with some individual tests. A score of less than 7 on this diagnostic tool made the clinical syndrome of LSS much less likely (LR, 0.10; 95% CI, 0.06–0.16). A score of 5 or higher on a diagnostic tool including only questionnaire-based items produced small increases in the likelihood of the clinical syndrome of LSS36 (LR, 1.9; 95% CI, 1.6–2.3; eTable 3). A score of less than 5 on this tool made the clinical syndrome of LSS less likely (LR, 0.33; 95% CI, 0.23–0.45). On testing in a validation sample, this questionnaire-based diagnostic tool yielded smaller magnitude LRs when positive (LR, 1.5; 95% CI, 1.1–2.1) and when negative (LR, 0.50; 95% CI, 0.28–0.88).
Table 4.
Prediction Rulesa
| History or Examination Characteristic | Risk Score Assigned |
|---|---|
| Konno et al,35 2007 | |
| History | |
| Age, y | |
| 60–70 (reference, <60) | 1 |
|
| |
| >70 (reference, <60) | 2 |
|
| |
| Absence of diabetes | 1 |
|
| |
| Neurogenic claudication | 3 |
|
| |
| Exacerbation of symptoms when standing up | 2 |
|
| |
| Symptom improvement when bending forward | 3 |
|
| |
| Physical examination | |
| Symptoms induced by having patients bend forward | −1 |
|
| |
| Symptoms induced by having patients bend backward | 1 |
|
| |
| Good peripheral artery circulation | 3 |
|
| |
| Abnormal Achilles tendon reflex | 1 |
|
| |
| Straight leg raising positive for reproducing pain | −2 |
|
| |
| Score interpretation | |
| Score range | −2 to 17 |
|
| |
| Positive score | ≥7 |
|
| |
| Questionnaire Item | |
| Sugioka et al,36 2008 | |
| History | |
| Age, y | |
| 60–70 (reference, <60) | 2 |
|
| |
| >70 (reference, <60) | 3 |
|
| |
| Onset over 6 mo | 1 |
|
| |
| Symptoms | |
| Improve when bending forward | 2 |
|
| |
| Improve when bending backward | −2 |
|
| |
| Exacerbated while standing up | 2 |
|
| |
| Intermittent claudication (“If your symptom occurs while walking, does it improve by resting?”) | 1 |
|
| |
| Urinary incontinence | 1 |
|
| |
| Score interpretation | |
| Score range | −2 to 10 |
|
| |
| Positive score | ≥5 |
Results were reported separately based on the same study sample.
Limitations of the Literature
In an effort to capture all possibly relevant studies, we used an initial search strategy favoring sensitivity over specificity and trusted the manual search would remove studies not relevant to the area of research. However, although the topic of the diagnosis of LSS has been widely addressed in expert commentaries, surgical case series and cohort studies of patients with LSS, and a limited number of diagnostic accuracy studies using a purely radiographic reference standard, very few studies examined the accuracy of the history and physical examination using a clearly defined and appropriate reference standard such as the clinical syndrome of LSS. Stringent criteria for quality were applied in this review.
The included studies had methodological differences that did not permit pooling of data in a true meta-analysis, and generally did not allow comparison of individual tests between studies. Three studies of 2 different patient populations excluded some patients with indeterminate findings by the reference standard.35,36,38 However, 2 of these studies excluded only 1 patient out of 469, which we thought was inconsequential.35,36 No studies permitted stratification by subtype of radiographic LSS severity.
Although the prevalence of the clinical syndrome of LSS was high in the included studies of primarily older adults, it is important to note the prevalence of the clinical syndrome of LSS in all patients presenting to a primary clinic with leg pain, back pain, or both may be substantially lower. Only 2 diagnostic accuracy studies, which used the same study sample, included a substantial proportion (one-third) of patients recruited from primary care (Table 2).35,36 Therefore, a greater severity of disease in the specialty clinic populations from which these accuracy estimates were derived may overestimate sensitivity and underestimate specificity when these tests are applied to primary care populations. In addition to this bias induced by the spectrum of disease, there is a problem with incorporation bias whereby the overall clinical findings are taken into account in establishing the diagnosis. Because a diagnosis of the clinical syndrome of LSS requires information from the clinical examination, such bias is unavoidable. Potential incorporation bias may have been mitigated in the included studies by using the consensus diagnosis of multiple expert spine clinicians,35 blinded examiners,35,38 and patient-reported data.36,37
The clinical diagnostic support tool using combinations of history and physical examination findings by Konno et al35 was subsequently tested in a separate validation study that did not meet inclusion criteria for this review, due to the inclusion of non-adults. This study by Kato et al40 found that a positive result on the diagnostic support tool had an LR of 1.6 (95% CI, 1.3–2.0) and a negative result had an LR of 0.13 (95% CI, 0.04–0.41). Taken together, these data demonstrate that this diagnostic tool is most useful for ruling out the clinical syndrome of LSS but is of limited value for ruling in disease. This may reflect the heterogeneity of the clinical syndrome of LSS, for which anatomic stenosis at different locations and multiple lumbar spinal interspaces may interact with person-specific factors to result in a wide spectrum of possible disease presentations and severity on a population level. Estimates from the validation study of the clinical diagnostic tool should be viewed cautiously given methodological differences from the derivation study. In contrast to the clinical diagnostic tool using history and physical examination findings, a validated questionnaire-based diagnostic tool had quite modest diagnostic value that is unlikely to be clinically useful.36
SCENARIO RESOLUTION
Case 1
The primary care clinician should consider the diagnosis of the clinical syndrome of LSS for this woman. Several findings of the history and physical examination suggest the diagnosis, including the history of worsened symptoms with standing (LR, 2.3), neurogenic claudication (LR, 3.7), and report of symptom improvement with bending forward (LR, 6.4). The prevalence of the clinical syndrome of LSS among older adults in primary care is difficult to know with certainty, so it is appropriate to explore the impact of the findings on a range of prevalence estimates. The pretest probability of the clinical syndrome of LSS of 47% in the highest quality study in our review is likely too high to generalize to a primary care setting. Assuming a primary care clinic prevalence of 15% and using only the finding of symptom improvement with bending forward, the probability of the clinical syndrome of LSS increases to 53%. However, if the clinic prevalence of the syndrome of LSS is 30%, the posttest probability would be 73%.
Case 2
This older man with back pain and leg pain is unlikely to have the clinical syndrome of LSS. Using the clinical diagnostic support tool by Konno et al (Table 4), the combined findings of being older than 70 years, absence of diabetes, exacerbation of symptoms with standing up, good peripheral circulation, and a positive straight leg raise yield a risk score of 6, a negative result (LR, 0.10). Assuming a clinic prevalence of 15%, the probability of the clinical syndrome of LSS decreases to 2%. If the prevalence of the clinical syndrome of LSS is as high as 30%, the posttest probability would still be only 4%. An alternative diagnosis such as lumbar disk herniation is likely in this patient who has pain when sitting and a positive straight leg raise test. Other causes of nerve root impingement, including vertebral osteophytosis and facet joint synovial cysts, should also be considered; delineation of specific anatomic factors may require cross-sectional imaging such as MRI.
BOTTOM LINE
The clinical syndrome of LSS is the most frequent indication for spinal surgery in patients older than 65 years of age.41 The presenting symptoms and, to a lesser extent, the physical examination findings, may be useful for the diagnosis of the clinical syndrome of LSS. The absence of pain when seated, the improvement of symptoms when bending forward, and a wide-based gait are the most useful individual findings for ruling in the diagnosis. However, many single clinical examination findings have been elicited in different ways across studies, and thus require standardization and further validation. A simple clinical diagnostic support tool may help synthesize the independent diagnostic value of a range of history and physical examination measures and can be particularly useful for ruling out the clinical syndrome of LSS. For the present, clinicians may find guidance from the sensitivities, specificities, and likelihood ratios presented in this review to refine estimates of the likelihood of the clinical syndrome of LSS and to plan management accordingly.
Acknowledgments
Funding/Support: Dr Suri is funded by grant K12 HD 01097 from the National Institutes of Health and the Rehabilitation Medicine Scientist Training Program (RMSTP). Dr Katz is also funded in part by grants K24 AR 02124 and P60 AR 47782 from the National Institute of Arthritis and Musculoskeletal and Skin Diseases.
Role of the Sponsor: The National Institutes of Health or its agencies did not participate in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
The Rational Clinical Examination Section Editors: David L. Simel, MD, MHS, Durham Veterans Affairs Medical Center and Duke University Medical Center, Durham, NC; Drummond Rennie, MD, Deputy Editor.
Author Contributions: Dr Suri had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Suri, Rainville, Katz.
Acquisition of data: Suri, Kalichman, Katz.
Analysis and interpretation of data: Suri, Rainville, Katz.
Drafting of the manuscript: Suri.
Critical revision of the manuscript for important intellectual content: Suri, Rainville, Kalichman, Katz.
Statistical analysis: Suri.
Administrative, technical, or material support: Suri, Katz.
Study supervision: Suri, Katz.
Financial Disclosures: None reported.
Online-Only Material: eMethods, eFigure, eTables 1 through 3, and eReferences are available at http://www.jama.com.
Simplified radiographic definitions stated in terms of anatomic zones of canal narrowing.5
Additional Contributions: We thank Nina N. Niu, BS, Harvard Medical School, and Ling Li, MPH, New England Baptist Hospital, for their assistance with data acquisition and statistical calculations. We thank Chris Vaillancourt, BA, MA, MLIS, New England Baptist Hospital for tireless material support. We thank Cory Adamson, MD, Duke University, Kim Huffman, MD, Duke University and Durham Veterans Affairs Medical Center, and Douglas McCrory, MD, MHS, Duke University and Durham Veterans Affairs Medical Center, for critical review of the manuscript. No compensation was received for these contributions.
References
- 1.Vogt MT, Cawthon PM, Kang JD, Donaldson WF, Cauley JA, Nevitt MC. Prevalence of symptoms of cervical and lumbar stenosis among participants in the Osteoporotic Fractures in Men Study. Spine (Phila Pa 1976) 2006;31(13):1445–1451. doi: 10.1097/01.brs.0000219875.19688.a6. [DOI] [PubMed] [Google Scholar]
- 2.Hicks GE, Gaines JM, Shardell M, Simonsick EM. Associations of back and leg pain with health status and functional capacity of older adults: findings from the retirement community back pain study. Arthritis Rheum. 2008;59(9):1306–1313. doi: 10.1002/art.24006. [DOI] [PubMed] [Google Scholar]
- 3.Katz JN, Harris MB. Clinical practice: lumbar spinal stenosis. N Engl J Med. 2008;358(8):818–825. doi: 10.1056/NEJMcp0708097. [DOI] [PubMed] [Google Scholar]
- 4.Lurie JD, Tosteson AN, Tosteson TD, et al. Reliability of readings of magnetic resonance imaging features of lumbar spinal stenosis. Spine (Phila Pa 1976) 2008;33(14):1605–1610. doi: 10.1097/BRS.0b013e3181791af3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fardon DF, Milette PC Combined Task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Nomenclature and classification of lumbar disc pathology: recommendations of the Combined Task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine (Phila Pa 1976) 2001;26(5):E93–E113. doi: 10.1097/00007632-200103010-00006. [DOI] [PubMed] [Google Scholar]
- 6.Genevay S, Atlas SJ. Lumbar spinal stenosis. Best Pract Res Clin Rheumatol. 2010;24(2):253–265. doi: 10.1016/j.berh.2009.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Djurasovic M, Glassman SD, Carreon LY, Dimar JR., II Contemporary management of symptomatic lumbar spinal stenosis. Orthop Clin North Am. 2010;41(2):183–191. doi: 10.1016/j.ocl.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 8.Konno S, Kikuchi S, Tanaka Y, et al. A diagnostic support tool for lumbar spinal stenosis: a self-administered, self-reported history questionnaire. BMC Musculoskelet Disord. 2007;8:102. doi: 10.1186/1471-2474-8-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yamashita K, Aono H, Yamasaki R. Clinical classification of patients with lumbar spinal stenosis based on their leg pain syndrome: its correlation with 2-year surgical outcome. Spine (Phila Pa 1976) 2007;32(9):980–985. doi: 10.1097/01.brs.0000261031.10091.f5. [DOI] [PubMed] [Google Scholar]
- 10.Birkmeyer NJ, Weinstein JN, Tosteson AN, et al. Design of the Spine Patient outcomes Research Trial (SPORT) Spine (Phila Pa 1976) 2002;27(12):1361–1372. doi: 10.1097/00007632-200206150-00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weinstein JN, Tosteson TD, Lurie JD, et al. SPORT Investigators. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med. 2008;358 (8):794–810. doi: 10.1056/NEJMoa0707136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Siebert E, Prüss H, Klingebiel R, Failli V, Einhäupl KM, Schwab JM. Lumbar spinal stenosis: syndrome, diagnostics and treatment. Nat Rev Neurol. 2009;5(7):392–403. doi: 10.1038/nrneurol.2009.90. [DOI] [PubMed] [Google Scholar]
- 13.Simon RW, Simon-Schulthess A, Amann-Vesti BR. Intermittent claudication. BMJ. 2007;334(7596):746. doi: 10.1136/bmj.39036.624306.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Verbiest H. Stenosis of the lumbar vertebral canal and sciatica. Neurosurg Rev. 1980;3(1):75–89. doi: 10.1007/BF01644422. [DOI] [PubMed] [Google Scholar]
- 15.Alvarez JA, Hardy RH., Jr Lumbar spine stenosis: a common cause of back and leg pain. Am Fam Physician. 1998;57(8):1825–1834. 1839–1840. [PubMed] [Google Scholar]
- 16.White C. Clinical practice: intermittent claudication. N Engl J Med. 2007;356(12):1241–1250. doi: 10.1056/NEJMcp064483. [DOI] [PubMed] [Google Scholar]
- 17.Malmivaara A, Slätis P, Heliövaara M, et al. Finnish Lumbar Spinal Research Group. Surgical or non-operative treatment for lumbar spinal stenosis? a randomized controlled trial. Spine (Phila Pa 1976) 2007;32(1):1–8. doi: 10.1097/01.brs.0000251014.81875.6d. [DOI] [PubMed] [Google Scholar]
- 18.Haig AJ. Paraspinal denervation and the spinal degenerative cascade. Spine J. 2002;2(5):372–380. doi: 10.1016/s1529-9430(02)00201-2. [DOI] [PubMed] [Google Scholar]
- 19.Kirkaldy-Willis WH, Wedge JH, Yong-Hing K, Reilly J. Pathology and pathogenesis of lumbar spondylosis and stenosis. Spine (Phila Pa 1976) 1978;3(4):319–328. doi: 10.1097/00007632-197812000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Truumees E. Spinal stenosis: pathophysiology, clinical and radiologic classification. Instr Course Lect. 2005;54:287–302. [PubMed] [Google Scholar]
- 21.Genevay S, Atlas SJ, Katz JN. Variation in eligibility criteria from studies of radiculopathy due to a herniated disc and of neurogenic claudication due to lumbar spinal stenosis: a structured literature review. Spine (Phila Pa 1976) 2010;35(7):803–811. doi: 10.1097/BRS.0b013e3181bc9454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Patel N. Surgical disorders of the thoracic and lumbar spine: a guide for neurologists. J Neurol Neurosurg Psychiatry. 2002;73(suppl 1):i42–i48. doi: 10.1136/jnnp.73.suppl_1.i42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Amundsen T, Weber H, Lillea°s F, Nordal HJ, Abdelnoor M, Magnaes B. Lumbar spinal stenosis: clinical and radiologic features. Spine (Phila Pa 1976) 1995;20(10):1178–1186. doi: 10.1097/00007632-199505150-00013. [DOI] [PubMed] [Google Scholar]
- 24.Kalichman L, Cole R, Kim DH, et al. Spinal stenosis prevalence and association with symptoms: the Framingham Study. Spine J. 2009;9(7):545–550. doi: 10.1016/j.spinee.2009.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tong HC, Carson JT, Haig AJ, et al. Magnetic resonance imaging of the lumbar spine in asymptomatic older adults. J Back Musculoskeletal Rehabil. 2006;19:67–72. [Google Scholar]
- 26.Chou R, Qaseem A, Snow V, et al. Clinical Efficacy Assessment Subcommittee of the American College of Physicians; American College of Physicians; American Pain Society Low Back Pain Guidelines Panel. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147(7):478–491. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 27.Khan NA, Rahim SA, Anand SS, Simel DL, Panju A. Does the clinical examination predict lower extremity peripheral arterial disease? JAMA. 2006;295 (5):536–546. doi: 10.1001/jama.295.5.536. [DOI] [PubMed] [Google Scholar]
- 28.Haig AJ, Tomkins CC. Diagnosis and management of lumbar spinal stenosis. JAMA. 2010;303 (1):71–72. doi: 10.1001/jama.2009.1946. [DOI] [PubMed] [Google Scholar]
- 29.Chou R, Shekelle P. Will this patient develop persistent disabling low back pain? JAMA. 2010;303 (13):1295–1302. doi: 10.1001/jama.2010.344. [DOI] [PubMed] [Google Scholar]
- 30.Yukawa Y, Lenke LG, Tenhula J, Bridwell KH, Riew KD, Blanke K. A comprehensive study of patients with surgically treated lumbar spinal stenosis with neurogenic claudication. J Bone Joint Surg Am. 2002;84-A(11):1954–1959. doi: 10.2106/00004623-200211000-00008. [DOI] [PubMed] [Google Scholar]
- 31.Henschke N, Maher CG, Refshauge KM, et al. Prevalence of and screening for serious spinal pathology in patients presenting to primary care settings with acute low back pain. Arthritis Rheum. 2009;60 (10):3072–3080. doi: 10.1002/art.24853. [DOI] [PubMed] [Google Scholar]
- 32.Holleman DR, Jr, Simel DL. Does the clinical examination predict airflow limitation? JAMA. 1995;273(4):313–319. [PubMed] [Google Scholar]
- 33.Katz JN, Liang MH. Classification criteria revisited. Arthritis Rheum. 1991;34(10):1228–1230. doi: 10.1002/art.1780341004. [DOI] [PubMed] [Google Scholar]
- 34.Simel DL, Samsa GP, Matchar DB. Likelihood ratios with confidence: sample size estimation for diagnostic test studies. J Clin Epidemiol. 1991;44(8):763–770. doi: 10.1016/0895-4356(91)90128-v. [DOI] [PubMed] [Google Scholar]
- 35.Konno S, Hayashino Y, Fukuhara S, et al. Development of a clinical diagnosis support tool to identify patients with lumbar spinal stenosis. Eur Spine J. 2007;16(11):1951–1957. doi: 10.1007/s00586-007-0402-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sugioka T, Hayashino Y, Konno S, Kikuchi S, Fukuhara S. Predictive value of self-reported patient information for the identification of lumbar spinal stenosis. Fam Pract. 2008;25(4):237–244. doi: 10.1093/fampra/cmn031. [DOI] [PubMed] [Google Scholar]
- 37.Ljunggren AE. Discriminant validity of pain modalities and other sensory phenomena in patients with lumbar herniated intervertebral discs versus lumbar spinal stenosis. Neuro-Orthopedics. 1991;11(2):91–99. [Google Scholar]
- 38.Katz JN, Dalgas M, Stucki G, et al. Degenerative lumbar spinal stenosis: diagnostic value of the history and physical examination. Arthritis Rheum. 1995;38(9):1236–1241. doi: 10.1002/art.1780380910. [DOI] [PubMed] [Google Scholar]
- 39.Pinksy LE, Wipf JE, Ramsey SD. Evidence-Based Medicine Glossary. In: Geyman JP, Deyo RA, Ramsey SD, editors. Evidence-Based Clinical Practice: Concepts and Approaches. Boston, MA: Butterworth-Heinemann; 2000. pp. 165–172. [Google Scholar]
- 40.Kato Y, Kawakami T, Kifune M, et al. Validation study of a clinical diagnosis support tool for lumbar spinal stenosis. J Orthop Sci. 2009;14(6):711–718. doi: 10.1007/s00776-009-1391-2. [DOI] [PubMed] [Google Scholar]
- 41.Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA. 2010;303(13):1259–1265. doi: 10.1001/jama.2010.338. [DOI] [PMC free article] [PubMed] [Google Scholar]