Abstract
In order to understand how culture influences Hispanic women's views about their health care provider (HCP), we examined the relationship between acculturation and fatalism in the HCP control expectations of Hispanic women. (A HCP control expectation is the extent to which an individual believes that her HCP has control over her health.) We predicted that acculturation would be negatively associated with HCP control expectations and fatalism would be positively associated with HCP control expectations. A group of 1,027 young Hispanic women (mean age 21.24 years; SD = 2.46) who were University of Texas Medical Branch clinic patients completed a comprehensive survey. Structural equation modeling was employed and as predicted, acculturation was negatively associated with HCP control expectations (p < .001) and fatalism was positively associated (p < .001). Understanding fatalism, acculturation, and their influence on HCP control expectations will help us understand this population's perceptions of their HCPs. This knowledge will assist HCPs in providing culturally competent care which will increase adherence to medical treatment and screening guidelines.
Keywords: Health care provider control, fatalism, acculturation, Latina, Hispanic
It is well established that Hispanic women face many barriers to health care such as lower incomes, lower education, and lack of health insurance.1,2,3,4,5 Other culturally related barriers such as unfamiliarity with navigating the U.S. medical system and limited use of the English language not only affect obtaining care, but also influence medical adherence.6 Given that adherence to medical treatment and screening guidelines is central to maintaining health, it is vital to identify and understand its barriers.
Health locus of control (HLC) is a theoretical framework frequently employed to examine health beliefs and behaviors. It proposes that individuals engage in different health behaviors depending on their beliefs of whether internal or external forces control their health. The powerful others health locus of control (PHLC) is a dimension of HLC that measures the extent to which other people control one's health.7–9 A component of the PHLC dimension is health care provider (HCP) control expectations. This measures the extent to which individuals believe that their HCPs have control over their health.
Research suggests that HCP control expectations and adherence are positively associated.7 For example, HIV patients who were adherent with their treatment regimens scored higher on the HCP control expectation items than non-adherent patients.8 We also know that HCPs' recommendations positively influence Hispanic patients' breast cancer screening rates9 and that patients' perceptions of their HCPs predict their satisfaction with care and their adherence to HCP recommendations.10 While the link between HCP control expectations and adherence to medical treatment and screening guidelines has been established, we know very little about the psychosocial factors that predict HCP control expectations.
When examining HCP control expectations in an ethnic minority population, it is essential to understand the role that culture and culturally-related beliefs play. Fatalism and acculturation are two such factors that should be examined. Fatalism, like HCP control expectations, is a component of an HLC dimension, in this case chance health locus of control (CHLC). It is most often defined as the belief that health and illness are predestined.11 From this point of view, if a person is meant to get sick, he or she will get sick, regardless of any measures taken to avoid illness. Researchers have found that among Hispanic women, high levels of fatalism are negatively associated with adherence with breast cancer and colorectal cancer screening.12,13 Although we do not yet understand the nature of the relationship between fatalism and HCP control expectations, high levels of both entail the belief that someone or something external controls your health. We need to understand further the relationship between fatalism and HCP control expectations given that the former is negatively associated with adherence and the latter is positively associated with adherence.
Acculturation can be understood as the extent to which an individual from a non-dominant ethnic group (e.g., Hispanics in the U.S.) adopts different aspects of the culture of the dominant ethnic group (Whites in the U.S.).14,15 A person who is highly acculturated has adopted many of the values, beliefs, and traditions—including the language—of the dominant culture while a person with a low level of acculturation has not. Acculturation is important because adherence to medical treatments and screenings along with feelings regarding one's HCP may be influenced by level of acculturation.
In fact, it has been found that highly acculturated Hispanic parents are more likely to adhere to physician-prescribed asthma treatments for their children than less acculturated Hispanic families.12 However, researchers have not yet investigated the relationship between acculturation and HCP control expectations among Hispanic women. The limited available research on acculturation and HCP control expectations indicates that less acculturated Hispanics are more likely to endorse the belief that their physician controls their health.13
Understanding these predictors is important in understanding the complex relationship between Hispanic female patients and their HCPs and ultimately increasing adherence. Therefore, in the present study, we examined the relationship between fatalism, acculturation, and HCP control expectations among a group of young Hispanic women. We hypothesize that acculturation is negatively associated with the HCP control expectations and fatalism is positively associated with HCP control expectations.
Methods
Data for the present study were collected between June 1, 2008 and May 29, 2009 as part of a larger, ongoing, cross-sectional study addressing health behaviors of adolescent and young adult females of reproductive-age. Women who were patients at one of five University of Texas Medical Branch (UTMB) Regional Maternal Child Health Program clinics in southeast Texas were screened for eligibility. In order to be eligible to participate in the study, women were required to have been between 16 and 24 years of age and to have spoken either English or Spanish. Approximately 80% of those meeting eligibility criteria agreed to participate and provided written informed consent. From available refusal data, women who refused to participate did not differ significantly in age from participants (p= .966). Women were paid $5 for their time. All procedures and measures were approved by the UTMB Institutional Review Board.
A total of 2,091 participants completed a comprehensive survey as part of the larger on-going study. As the current analyses focus on Hispanic women, participants who did not self-identify as Hispanic were excluded from the analyses. This resulted in a final sample of 1,027 participants. The survey was available in both English and Spanish. Approximately 62.5% (N = 642) of the sample responded to the English version of the survey and 37.5% (N = 385) responded to the Spanish version. Demographic data concerning age, education, marital status, and income were collected from the participants.
Four items from the language portion of the widely employed and previously validated Short Acculturation Scale for Hispanics16 measured acculturation. The items assessed: language spoken as a child, language spoken at home, language thought in, and language spoken with friends. The response scale ranged from Only Spanish (1) to Only English (5). The reliability of the scale for our sample was α = .961.
The fatalism and HCP control expectation items were selected from the widely employed and validated Multidimensional Health Locus of Control measure (MHLC).17 The fatalism items were chosen from the chance health locus of control (CHLC) subscale of the MHLC while the HCP control expectation items were selected from the powerful others health locus of control (PHLC) subscale. The response scale for all items ranged from Strongly Disagree (1) to Strongly Agree (5). We conducted two separate factor analyses of the CHLC and PHLC subscales using Mplus version 5.1 (Los Angeles, CA). Maximum-likelihood (MLR) and oblique geomin estimation assisted us in identifying the items that measured the concepts of fatalism and HCP control expectations. Only the items from the CHLC subscale that clearly loaded onto one factor and matched the conceptual definitions of fatalism were retained. Similarly, only the items from the PHLC subscale that met the same criteria for HCP control expectations were retained. This resulted in the retention of three items for fatalism and two items for HCP control expectations (all factor loadings were above .42). See Table 1 for the items selected and their factor loadings.
Table 1.
Factor analysis results for fatalism and health care provider control expectancies
| Item | Factor Loading |
|---|---|
| Fatalism | |
| 1. No matter what I do, if I am going to get sick, I will get sick. | .42 |
| 2. No matter what I do, I'm likely to get sick. | .55 |
| 3. If it's meant to be, I will stay healthy. | .44 |
| HCP Control Expectancies | |
| 1. Health professionals control my health | .65 |
| 2. Regarding my health, I can only do what my doctor tells me to do. | .51 |
Descriptive statistics were derived using SPSS 17.0 for Windows (Chicago, IL). In general, less than 10% of the data on each of the variables were missing, with the exception of income (14%). All subsequent analyses were conducted using structural equation modeling (SEM) and the software package Mplus. A two-step modeling procedure was employed to test the full structural model.18 This procedure involved testing a measurement model with the latent variables: acculturation, fatalism, and HCP control expectations in order to establish the construct validity of the latent variables. The second step involved testing the proposed structural model. Multiple regression with maximum-likelihood estimation (MLR) was used to evaluate the relationship between the acculturation, fatalism, and HCP control expectations. Maximum-likelihood estimation was chosen, in part, for its technique for handling missing data. It allows for the retention and use of all cases in the analyses and is considered by field experts to be superior to more commonly employed methods.18,19 The demographic variables age, education, marital status, and income were included in the initial model as covariates to examine and control for their potential influence on HCP control expectations.
The fit of the model was evaluated through the examination of several fit indices: 1. chi-square (low value and non-significant p-value is desired), 2. the comparative fit index (CFI; values greater than .90 indicate good fit), 3. the standardized root mean square residual (SRMR; values < .90 indicate good fit), and 4. the root-mean-square residual (RMSEA; values < .10 indicate good fit).
Results
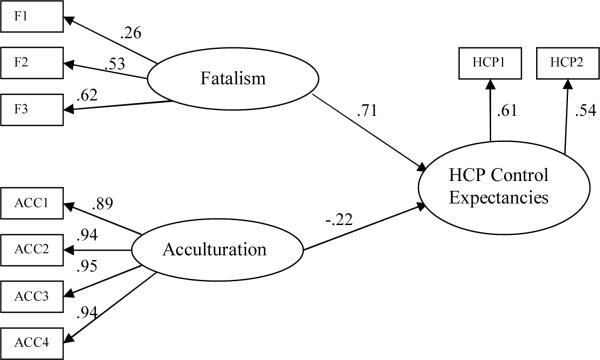
The mean age of the subjects was 21.24 years (SD = 2.46). Other sample demographics are shown in Table 2. The measurement model fit statistics were: χ2 (24) = 210.80, p-value < .001; CFI = .953; RMSEA = .087; SRMR = .053. The fit statistics indicated good model fit and all of the indicators loaded significantly onto their respective latent variables (acculturation, fatalism, and HCP control expectations). Figure 1 presents the factor loadings for the indicators. The latent variables were significantly correlated (Table 3). Next, we examined the proposed structural model. The initial model estimated included age, income, and education to evaluate and control for their influence on HCP control expectations. The model fit statistics indicated good model fit and all path coefficients were significant except for the paths from: 1. age to control expectations (p = .252), 2. income to control expectations (p = .537), and 3. education to control expectations (p = .330). Given the non-significance of these paths, age, income and education were removed from the model in order to maintain parsimony. The new model, without non-significant paths, was estimated. These fit indices indicated good model fit and all path coefficients were significant in the predicted directions (see Figure 1). Specifically, fatalism and HCP control expectations were positively associated, while acculturation and HCP control expectations were negatively associated. Path coefficients are interpreted in the same manner as regression coefficients. For example, each 1 point increase in acculturation is associated with a .22-point decrease in level of HCP control expectations. The proportion of variance (R2) in HCP control expectations accounted for by the variables in the model was .624.
Table 2.
Demographic characteristics of the sample (N=1027)
| N (%) | |
|---|---|
| Education | |
| Did not Complete High School | 307 (31.1%) |
| Currently in High School | 156 (15.8%) |
| High school diploma or equivalent | 319 (32.3%) |
| Completed some college courses | 180 (18.2%) |
| College degree | 25 (2.5%) |
| Marital Status | |
| Single, never married | 423 (42.4%) |
| Married or living with partner | 527 (51.5%) |
| Separated, divorced, or widowed | 63 (6.2%) |
| Income | |
| < $15,000 per year | 515 (58.5%) |
| $15,000 to $29,999 per year | 248 (28.1%) |
| $30,000 to $49,999 per year | 87 (9.9%) |
| $50,000 to $69,999 per year | 20 (2.3%) |
| ≥ $70,000 per year | 11 (1.2%) |
Frequencies that do not sum to total represent missing data
Figure 1. Acculturation, Fatalism and Health Care Provider Control Expectancies Structural Model.
All p < .001. Model fit indices: χ2 (24) = 210.79, p-value = .000; CFI = .953; RMSEA = .087; SRMR = .053; R2 = .624.
Table 3.
Correlations among Latent Variables
| 1 | 2 | 3 | |
|---|---|---|---|
| 1.HCP Control Expectancies | — | ||
| 2. Acculturation | −.384 | — | |
| 3. Fatalism | .761 | −.234 | — |
All correlations are significant at p < .001
Discussion
Our findings provide new insight into how young Hispanic women feel about their health care providers. Compared with less fatalistic Hispanic women, highly fatalistic Hispanics were more likely to believe that HCPs control their health. Additionally, women who were less acculturated were more likely than highly acculturated Hispanic women to believe that HCPs control their health. This information is extremely important given that HCPs have the ability to improve their patients' adherence with screening guidelines and treatment.9, 10
One important implication of our findings is that there appears to be a conflict between fatalism and HCP control expectations. While women who are highly fatalistic express more HCP control expectations, they are also more likely to believe that health is predestined or controlled by a non-human outside force. Consequently, highly fatalistic Hispanic women are less likely than less fatalistic Hispanic women to receive preventive health services and engage in screening behavior, such as colorectal cancer screening.20 However, as mentioned previously, high HCP control expectations are related to increased adherence.7,8 Future research should examine how HCP provider characteristics (e.g., whether the provider is bilingual, knowledge of cultural issues and fatalism), insurance status, and HCP trust influence the relationship between fatalism, and HCP control expectations. Further, researchers should investigate how fatalism and HCP control expectations are related to each other and to adherence to medical treatment and screening guidelines.
Another implication of our findings involves the negative association between acculturation and HCP control expectations. Research shows that less acculturated Hispanic women are less likely than highly acculturated Hispanic women to receive preventive health services and engage in cervical cancer screening.21 However, the association we found between acculturation and HCP control expectations provides important and encouraging information for those interested in increasing adherence among less acculturated Hispanic women since high HCP control expectations predict greater adherence among other populations.7 What remains is to understand why higher HCP control expectations among less acculturated Hispanic women do not translate into increased adherence. This may be due to ineffective cross-cultural communication between less acculturated patients and their HCPs. If this is the case, we should develop strategies to improve cross-cultural communication. Future research should examine further the relationship between acculturation, HCP control expectations, and adherence among Hispanic women.
While this study provides a preliminary look into the relationship of acculturation, fatalism, and HCP control expectations among Hispanic women, it is important to note that the design was cross-sectional and thus we cannot assume causality. However, our study did include a large sample size of Hispanic participants and the multi-site data collection enabled us to sample from a large, diverse population across southeast Texas, thus increasing the generalizability of our findings. Also, all of the data in the current study were obtained via self-report. Therefore, the data were susceptible to self-report bias. Additionally, we measured acculturation using a language-based measure, although language is only one facet of acculturation. However, previous research has found that measures of language acculturation, such as the one employed in the current study, distinguish very well among Hispanics with different levels of acculturation.22 Further, researchers have found language acculturation to be the strongest predicting component of acculturation.23
The current findings indicate that Hispanic women who are less acculturated and those who are highly fatalistic most strongly endorse the belief that their health care provider controls their health. In view of this, HCPs may have more influence over the health behaviors of these women than previously thought. Therefore, effective communication between HCPs and these patients is central to increasing adherence. The Institute of Medicine recommends that provider education in cultural competency should begin early in the educational process and continue throughout the various stages of career development.24 Educating health care professionals on how acculturation and fatalism may affect the care of Hispanic women will enable providers to deliver the most relevant health information to these women. The development of interventions that are sensitive to the differences that exist among Hispanic women is likely to increase adherence with medical treatment and screening guidelines and may aid in the reduction of health care disparities among this population.
Acknowledgments
Drs. Roncancio and Ward are Kirschstein-NRSA postdoctoral fellows supported by an institutional training grant (T32HD055163) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Dr. Abbey B. Berenson is the principal investigator of the above-mentioned grant and is supported by K24HD043659. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health and Human Development or the National Institutes of Health.
References
- (1).Roberts RE, Lee ES. Medical care use by Mexican-American: Evidence from the human population laboratory studies. Medical Care. 1980;18(3):267–281. [PubMed] [Google Scholar]
- (2).Andersen R, Lewis SZ, Giachell AL, Aday LA, Chiu G. Access to medical care among the Hispanic population of the southwestern United States. Journal of Health and Social Behavior. 1981;22(1):78–89. [PubMed] [Google Scholar]
- (3).Ransford HE, Carrillo FR, Rivera Y. Health care-seeking among Latino immigrants: Blocked access, use of traditional medicine, and the role of religion. Journal of Health Care for the Poor and Underserved. 2010;21(3):862–878. doi: 10.1353/hpu.0.0348. [DOI] [PubMed] [Google Scholar]
- (4).Freeman G, Lethbridge-Cejku M. Access to health care among Hispanic or Latino women: United States, 2000–2002. Advance Data: From Vital and Health Statistics. 2006;368:1–26. [PubMed] [Google Scholar]
- (5).Insaf TZ, Jurkowski JM, Alomar L. Sociocultural factors influencing delay in seeking routine health care among Latinas: A community-based participatory research study. Ethnicity and Disease. 2010;20(2):148–154. [PubMed] [Google Scholar]
- (6).Barron F, Hunter A, Mayo R, Willoughby D. Acculturation and adherence: Issues for health care providers working with clients of Mexican origin. Journal of Transcultural Nursing. 2004;15(4):331–337. doi: 10.1177/1043659604268950. [DOI] [PubMed] [Google Scholar]
- (7).Rubio RN, Pearson HC, Clark AA, Breitkopf CR. Satisfaction with care among low-income female outpatients. Psychol Health Med. 2007;12(3):334–345. doi: 10.1080/13548500600864053. [DOI] [PubMed] [Google Scholar]
- (8).Ubbiali A, Donati D, Chiorri C, Bregani V, Cattaneo E, Maffei C, et al. Prediction of adherence to antiretroviral therapy: Can patients' gender play some role? An Italian pilot study. AIDS Care. 2008;20(5):571–575. doi: 10.1080/09540120701867172. [DOI] [PubMed] [Google Scholar]
- (9).Zapka JG, Stoddard A, Barth R, Costanza ME, Mas E. Effects of community health center intervention on breast cancer screening of Hispanic American women. Health Services Research. 1993;28:221–235. [PMC free article] [PubMed] [Google Scholar]
- (10).Sheppard VB, Wang J, Yi B, Harrison TM, Feng S, Huerta EE, et al. Are health-care relationships important for mammography adherence in Latinas? Journal of General Internal Medicine. 2008;23(12):2024–2030. doi: 10.1007/s11606-008-0815-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (11).Davison C, Frankel S, Smith GD. The limits of lifestyle: re-assessing `fatalism' in the popular culture of illness prevention. Soc Sci Med. 1992;34(6):675–685. doi: 10.1016/0277-9536(92)90195-v. [DOI] [PubMed] [Google Scholar]
- (12).Pachter LM, Weller SC. Acculturation and compliance with medical therapy. J Dev Behav Pediatr. 1993;14(3):163–168. [PubMed] [Google Scholar]
- (13).Castro FG, Furth P, Karlow H. The health beliefs of Mexican, Mexican American, and Anglo American women. Hispanic Journal of Behavioral Sciences. 1984;6(4):365–383. [Google Scholar]
- (14).Berry JW. Immigration, acculturation, and adaptation. Applied Psychology: An International Review. 1997;46(1):5–33. [Google Scholar]
- (15).Cuellar I, Arnold B, Maldonado R. Acculturation rating scale for Mexican Americans-II: A revision of the original ARSMA scale. Hispanic Journal of Behavioral Sciences. 1995;17(3):275–304. [Google Scholar]
- (16).Marin G, Sabogal F. Development of a short acculturation scale for Hispanics. Hispanic Journal of Behavioral Sciences. 1987;9(2):183–205. [Google Scholar]
- (17).Wallston KA, Wallston BS. Health locus of control scales. In: Lefcourt HM, editor. Research with the Locus of Control Construct. Volume 1. Academic Press; New York: 1981. pp. 189–243. [Google Scholar]
- (18).Kline RB. Principles and practice of structural equation modeling. The Guilford Press; New York, NY: 2005. [Google Scholar]
- (19).Allison PD. Missing data techniques for structural equation modeling. Journal of Abnormal Psychology. 2003;112(4):545–557. doi: 10.1037/0021-843X.112.4.545. [DOI] [PubMed] [Google Scholar]
- (20).Gorin SS. Correlates of colorectal cancer screening compliance among urban Hispanics. J Behav Med. 2005;28(2):125–137. doi: 10.1007/s10865-005-3662-5. [DOI] [PubMed] [Google Scholar]
- (21).Shah M, Zhu K, Wu H, Potter J. Hispanic acculturation and utilization of cervical cancer screening in the US. Prev Med. 2006;42(2):146–149. doi: 10.1016/j.ypmed.2005.10.002. [DOI] [PubMed] [Google Scholar]
- (22).Felix-Ortiz M, Newcomb MD, Myers H. A multidimensional measure of cultural identity for Latino and Latina adolescents. Hispanic Journal of Behavioral Sciences. 1994;16(2):99–115. [Google Scholar]
- (23).Olmedo EL, Padilla AM., 7 Empirical and construct validation of a measure of acculturation for Mexican-Americans. Journal of Social Psychology. 1978;105:179–187. [Google Scholar]
- (24).Institute of Medicine . Summary. In: Smedley BD, Stith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. The National Academies Press; Washington, D.C.: 2003. pp. 1–27. [PubMed] [Google Scholar]