Abstract
Smith–Magenis syndrome (SMS) is a complex disorder whose clinical features include mild to severe intellectual disability with speech delay, growth failure, brachycephaly, flat midface, short broad hands, and behavioral problems. SMS is typically caused by a large deletion on 17p11.2 that encompasses multiple genes including the retinoic acid induced 1, RAI1, gene or a mutation in the RAI1 gene. Here we have evaluated 30 patients with suspected SMS and identified SMS-associated classical 17p11.2 deletions in six patients, an atypical deletion of ∼139 kb that partially deletes the RAI1 gene in one patient, and RAI1 gene nonsynonymous alterations of unknown significance in two unrelated patients. The RAI1 mutant proteins showed no significant alterations in molecular weight, subcellular localization and transcriptional activity. Clinical features of patients with or without 17p11.2 deletions and mutations involving the RAI1 gene were compared to identify phenotypes that may be useful in diagnosing patients with SMS.
Keywords: Smith–Magenis syndrome, 17p11.2, RAI1, arrayCGH, mutation, deletion
Introduction
Smith–Magenis syndrome (SMS, MIM 182290) is a multiple congenital anomalies and intellectual disability syndrome associated with a deletion of chromosome 17p11. 2. The incidence of SMS is estimated to be ∼1:15 000–1:25 000 births.1 SMS is most commonly characterized by a variable degree of intellectual disability including speech and motor delay, craniofacial and skeletal anomalies, sleep disturbance, self-injurious and attention-seeking behaviors.1, 2 Craniofacial features include brachycephaly, midface hypoplasia, tented upper lip, relative prognathism with age and deep-set and hypoteloric eyes.3, 4 Skeletal features include brachydactyly, short stature and short/broad hands.3, 4 The behavioral phenotype includes onychotillomania, polyembolokoilamania, ‘hand licking and page flipping', ‘self-hugging' and hyperactivity.5 Sleep disturbance is present in 88% of SMS patients and is characterized by difficulty getting to sleep, frequent nocturnal awakenings, early sleep offset and daytime sleepiness with a need for daytime naps.6, 7 SMS clinical features overlap with other intellectual disability syndromes such as Prader–Willi, Williams and Down's syndromes, which often complicate its clinical diagnosis.
A majority, ∼90%, of SMS patients have a deletion of chromosome 17p11.2 that includes the RAI1 gene.3 The classical SMS deletions span ∼3.5 Mb of 17p11.2 and are present in ∼70% of affected individuals.3, 8, 9 Atypical (smaller or larger) deletions, including the 17p11.2 band, occur in ∼20% of other affected individuals.3, 8, 9 Mutations in the RAI1 gene have been observed in ∼10% of all reported SMS patients.10, 11, 12, 13, 14
To date, little is known about the function of human RAI1. RAI1 appears to be a nuclear protein and exhibits transcription factor activity.15 The transcription factor activity of RAI1 has been linked to its N-terminal half and the C-terminal half directs it to the nucleus.15 However, all SMS-associated missense mutations analyzed till date did not produce proteins that differed from the wild-type RAI1 protein either in their subcellular localization or in their transcription factor activity function,15, 16 suggesting that there are other essential RAI1 functions related with the SMS clinical phenotype. A functional network module for SMS has been suggested based on a genome-wide gene expression study using RAI1 haploinsufficient HEK293T cells.17
We have analyzed 30 patients of Brazilian origin that were clinically suspected to have SMS. Fluorescence in situ hybridization (FISH) analyses revealed six patients with a classical 17p11.2 deletion. Using arrayCGH analyses, we mapped the approximate locations of the deletion boundaries in these six patients and identified an atypical small deletion of ∼139 kb that included exons 1 and 2 of the RAI1 gene in one additional patient. Mutation screening of the coding region of the RAI1 gene in the remaining patients identified two patients with novel heterozygous nonsynonymous alterations of unknown significance.
Materials and methods
Subjects
The study was approved by the Research Ethics Committee of Botucatu Medical School, São Paulo State University/UNESP, Brazil. A standardized clinical data collection form was used. A total of 30 patients suspected of having SMS were ascertained from different clinical centers and included in this study using a predetermined inclusion/exclusion criteria. The inclusion criteria were the presence of at least three craniofacial/skeletal muscle system abnormalities, at least one of specific behavior stereotypes, presence or history of sleep disturbance, and presence or history of at least one self-injurious behavior. The exclusion criteria were suspicion/diagnosis of another genetic disease, severe malformation of the central nervous system, a perinatal injury or clinical status compatible with cerebral palsy, and insufficient information on the study inclusion criteria.
The frequency of clinical features from this study (Table 1) and the frequency described in the literature were compared. Statistical analysis was performed using the two-tailed Fisher's exact test.
Table 1. Clinical features of SMS and SMS-like groups.
| 17p11.2 classical deletion, n=6 (a) | 17p11.2 small deletion, n=1 (b) | RAI1 variant, n=2 (c) | SMS (a+b+c)a | SMS-like n=21b | P-valuec | |
|---|---|---|---|---|---|---|
| Age average | 16.16 | 28.00 | 8.30 | 14.7 | 13.4 | 0.5986 |
| Gender | 3M/3F | 1M | 2M | 6M/3F | 9M/12F | 0.4348 |
| Craniofacial | ||||||
| Brachycephaly | 4/6 | 0/1 | 1/2 | 5/9 | 8/21 | 0.4434 |
| Midface hypoplasia | 5/5 | 0/1 | 1/1 | 5/7 | 15/21 | 0.6391 |
| Broad, square-shaped face | 6/6 | 1/1 | 1/2 | 8/9 | 12/18 | 0.3748 |
| Deep-set, close-spaced eyes | 5/6 | 0/1 | 1/2 | 6/9 | 11/21 | 0.6908 |
| Everted, ‘tented' upper lip | 6/6 | 0/1 | 2/2 | 8/9 | 15/21 | 0.3816 |
| Relative prognathism with age | 5/5 | 0/1 | 2/2 | 7/8 | 12/21 | 0.2008 |
| Dental anomalies | 4/4 | 0/1 | 2/2 | 6/8 | 7/15 | 0.1649 |
| Skeletal | ||||||
| Short broad hands | 5/5 | 1/1 | 2/2 | 8/8 | 8/19 | 0.0095 |
| Brachydactyly | 4/4 | — | 0/1 | 4/5 | 1/11 | 0.0128 |
| Short stature | 5/6 | 0/1 | 1/2 | 6/9 | 7/18 | 0.2177 |
| Scoliosis | 2/6 | 1/1 | 0/1 | 3/8 | 9/21 | 1.0000 |
| Neurological | ||||||
| Cognitive impairment/developmental delay | 6/6 | 1/1 | 2/2 | 9/9 | 20/21 | 1.0000 |
| Speech delay | 6/6 | 0/1 | 2/2 | 8/9 | 19/20 | 0.5320 |
| Motor delay | 4/4 | — | 2/2 | 6/6 | 9/9 | 1.0000 |
| Infantile hypotonia | 3/5 | 0/1 | 2/2 | 5/8 | 16/20 | 0.3715 |
| Sleep disturbance | 4/5 | 1/1 | 2/2 | 7/8 | 15/18 | 1.0000 |
| Oral sensorimotor dysfunction | 3/3 | 0/1 | 1/1 | 4/5 | 8/11 | 1.0000 |
| Hyporeflexia | 1/5 | 0/1 | 0/1 | 1/7 | 5/16 | 0.6214 |
| Epilepsia | 2/6 | 0/1 | 1/2 | 3/9 | 10/17 | 0.3999 |
| Generalized complacency/lethargy (infancy) | 4/4 | 0/1 | 1/1 | 5/6 | 9/14 | 0.6129 |
| Behavior | ||||||
| Self-hug | 5/6 | 0/1 | 2/2 | 7/9 | 13/21 | 1.0000 |
| Onychotillomania | 3/5 | 1/1 | 2/2 | 6/8 | 15/20 | 1.0000 |
| Polyembolokoilamania | 4/5 | 0/1 | 2/2 | 6/8 | 8/19 | 0.0809 |
| Head banging/face slapping | 0/1 | 1/1 | 2/2 | 3/4 | 6/9 | 1.0000 |
| Hand biting | 3/4 | 0/1 | 2/2 | 5/7 | 7/10 | 1.0000 |
| Attention seeking | 4/4 | 1/1 | 1/1 | 6/6 | 11/13 | 1.0000 |
| Aggressive behavior | 5/5 | 1/1 | 2/2 | 8/8 | 17/20 | 0.5453 |
| Lick and flip | 2/4 | 1/1 | 2/2 | 5/7 | 8/15 | 1.0000 |
| Self-injurious behaviors | 6/6 | 1/1 | 2/2 | 9/9 | 18/20 | 1.0000 |
| Hyperactivity | 3/3 | 1/1 | 2/2 | 6/6 | 4/4 | 1.0000 |
| Other features | ||||||
| Hearing loss | 2/5 | — | — | 2/5 | 3/10 | 1.0000 |
| Myopia | 1/1 | — | — | 1/1 | 1/5 | 0.3333 |
| Strabismus | 3/3 | — | — | 3/3 | 0/1 | 0.2500 |
| Iris abnormalities | 3/3 | — | — | 3/3 | 0/6 | 0.0119 |
| History of constipation | 2/4 | 1/1 | 0/1 | 3/6 | 9/16 | 1.0000 |
| Inverted circadian rhythm of melatonin | 0/1 | 1/1 | 1/1 | 2/3 | 6/9 | 1.0000 |
| Velopharyngeal insufficiency | 1/1 | 0/1 | — | 1/2 | 1/7 | 0.4167 |
| Cardiac defects | 0/5 | 0/1 | 0/1 | 0/7 | 6/14 | 0.0609 |
| Renal/urinary tract abnormalities | 1/2 | 0/1 | — | 1/3 | 2/6 | 1.0000 |
| Cleft lip/palate | 0/5 | — | 0/2 | 0/7 | 0/16 | 1.0000 |
| Hypogonadism (in males) | 1/2 | — | 1/1 | 2/3 | 0/7 | 0.6670 |
| Obesity | 2/4 | 0/1 | 0/2 | 2/7 | 3/16 | 0.6214 |
Abbreviation: SMS, Smith–Magenis syndrome.
Bold type is used for headings and statistically significant P-values of <0.05.
del17p11.2 or RAI1 mutation.
No deletion or point mutation.
P-values from two-tailed Fisher's exact tests.
Fluorescence in situ hybridization (FISH)
Metaphase chromosome spreads were obtained from lymphoblasts from patients using the conventional methods. FISH was performed using commercial probes with the RAI1 gene (catalog # LPU019, Cytocell, Cambridge, UK) as the target. The probe was 160 kb in size and includes the distal region of the RAI1 gene (D17S258). Metaphase analyses were performed using a florescence microscope (Leitz DM RBE – LEICA, Wetzlar, Germany).
Whole-genome array CGH and quantitative PCR (qPCR)
Genomic DNA was purified using the Wizard Genomic DNA Purification Kit (Promega, Sunnyvale, CA, USA). Patient DNA was labeled, hybridized to an Affymetrix Genome Wide Human SNP Nsp/Sty 6.0 array and washed according to the manufacturer's protocol (Affymetrix, Santa Clara, CA, USA). Data quality was assessed using the Birdseed v2 algorithm (Broad Institute, Cambridge, MA, USA). Signal intensity and copy number status for each probe set was extracted using Affymetrix Genotyping Console Version 4.0 software. Changes in copy number were confirmed by qPCR using iQ SYBR Green Supermix on a CFX96 Real-Time PCR Detection System (Bio-Rad, Hercules, CA, USA) as described previously .18 Data were analyzed with CFX Manager Software (Bio-Rad).
Mutation screening
The entire coding region and up to 100 bp of flanking intronic sequences of the RAI1 gene were amplified by standard PCR. Amplified products were treated with ExoSAP-IT (USB Corporation, Cleveland, OH, USA), bidirectionally sequenced by the Sanger method using the BigDye Terminator v3.1 Cycle Sequencing Kit and separated on an ABI 3730xl DNA analyzer (Applied Biosystems, Carlsbad, CA, USA). Primer sequences and reaction mixes are available on request. Sequences were analyzed with DNASTAR SeqMan II software (Madison, WI, USA).
Plasmid constructs
The full-length clone of human RAI1-HA cDNA was generated previously.15 The variant RAI1-HA R1217Q was generated using the QuikChange II XL Site-Directed Mutagenesis Kit (Agilent Technologies, Santa Clara, CA, USA) utilizing the primers forward: 5′-GCTCTCTGACCAGCCCCTCCATG-3′ and reverse: 5′-CATGGAGGGGCTGGTCAGAGAGC-3′. The variant RAI1-HA Q1389R was generated by overlapping PCR. The following primers were used : forward 1: 5′-GGAGACAGACTCACCCAGCACG-3′, reverse 1: 5′-GGAGCTTCCGCCCGGTG-3′, forward 2: 5′-CACCGGGCGGAAGCTCC-3′ and reverse 2: 5′-GCGGGCCTTTGGAGAGTCCATG-3′. The mutated fragments were subcloned to replace the wild-type sequence into full-length RAI1 cDNA with the enzymes AfeI and PflMI. All clones were verified by DNA sequencing for the presence of the desired variation and no extra changes in the nucleotide sequence. Wild-type RAI1 and the variant proteins contain the influenza virus hemagglutinin epitope tag (HA) at the C-terminal end to facilitate their detection. For expression analysis, the cDNAs of RAI1 wild-type and mutant forms were subcloned into pALTER-MAX vector (Promega).
Immunofluorescence and western blot analysis
Neuro-2a cells were grown in Dulbecco's modified Eagle's medium supplemented with 10% fetal bovine serum, penicillin (100 units/ml) and streptomycin (100 μg/ml) at 37 °C with 5% CO2 until 95% confluence was attained. To study the expression of the RAI1 proteins, Neuro-2a cells were transfected with Lipofectamine 2000 (Invitrogen, Carlsbad, CA, USA), and the plasmid pALTER-MAX RAI1-HA wild-type, RAI1-HA R1217Q or RAI1-HA Q1389R. All transfections were performed according to the manufacturer's protocols described previously.15
For immunofluorescence, cells were fixed 24 h after transfection with 4% paraformaldehyde followed by permeabilization with 0.2% Triton X-100 in phosphate-buffered saline. Subcellular localization of RAI1-HA wild-type and mutant forms were detected using the anti-HA high-affinity antibody (1:1000, clone 3F10, Roche, Indianapolis, IN, USA). Secondary antibody conjugated to Alexa fluor 488 (1:1000, Invitrogen) was used. Cells were stained with 4′,6-diamidino-2-phenylindole, dihydrochloride (DAPI) and mounted with Dako fluorescent mounting medium.
For western blot analysis, total protein extracts were prepared 24 h after transfection. Cells were lysed in 100 μl of protein extraction and loading buffer (2% SDS, 2 M urea, 10% glycerol, 10 mM Tris pH 6.8, 0.002% bromophenol blue and 10 mM DTT) plus 1:200 protease inhibitor cocktail (Sigma, St Louis, MO, USA). The samples were homogenized by passing them 20 times through a syringe and incubated at 95 °C for 5 min. Approximately, 20 μl of each cell lysate was loaded onto 4–20% SDS-polyacrylamide gels with Tris/glycine running buffer and transferred to a 0.2 μm poly-vinylidene fluoride (PVDF, Bio-Rad Laboratories) membrane. Immunodetection was performed using rat anti-HA (1:7000, Roche) and rabbit anti-β-tubulin (1:1000, sc-9104 Santa Cruz, Santa Cruz, CA, USA). Results were visualized by chemiluminiscence.
Reporter gene assays
Transient transfections in Neuro-2a cells were performed in 35-mm plates. The amounts of plasmid DNA used were determined according to the manufacturer's protocol. GAL4-BD fusions of human RAI1 wild-type and its mutant forms were co-transfected with the luciferase reporter plasmid pFR-Luc (Agilent Technologies). For normalizing the results in case of transfection efficiency variations, the vector pSV-β-galactosidase (Promega Corporation) was also co-transfected for expression of β-galactosidase. After 48 h post-transfection, the cells were lysed and the luciferase activity was measured using the Luciferase Assay Kit (Agilent Technologies) according to the manufacturer's instructions. The relative lights units (RLUs) were measured in duplicate in a luminometer (Turner BioSystems 20/20n, Promega Corporation).
The β-galactosidase activity of the extracts was measured using the microassay protocol of β-galactosidase Assay kit (Agilent Technologies). Each cell assay was carried out in duplicate.
Results
We have analyzed a cohort of 30 Brazilian patients with clinical features suggestive of SMS to determine if their clinical features are because of a defect in the SMS causative gene, RAI1. These patients have some of the features typically seen in patients with SMS. For example, typical facies (brachycephaly, midface hypoplasia and ‘tented' upper lip), intellectual disability, sleep disturbance, hypotonia, speech delay, and characteristic SMS behaviors (self-injury, self-hugging and aggression; Table 1).
FISH, whole-genome array CGH and qPCR analyses
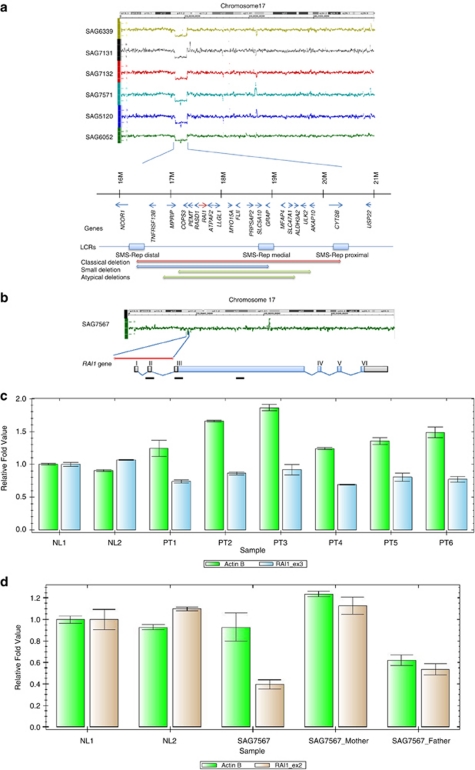
FISH analysis using commercial probes with the RAI1 gene as the target revealed deletions at chromosome 17p11.2. in six patients (data not shown). Whole-genome arrayCGH was performed to determine the size and breakpoints of the deletions. This analysis confirmed all six 17p11.2 deletions and determined that the deletions were ∼3.61–3.67 Mb in sizes (Figure 1a). Additionally, an atypical deletion of 139 kb was identified in one patient (Figure 1b). This deletion included the 5′ end of the RAI1 gene and apparently resulted in the partial loss of the RAI1 gene (Figure 1b). The coordinates and sizes of all seven deletions are shown in Table 2. Of the 30 patients studied, 7 (23%) had a deletion that included all or part of the RAI1 gene.
Figure 1.
(a) Array CGH profiles of chromosome 17 in six patients with the classical deletion of SMS and schematic representation of chromosome 17p11.2. Representative gene content of the 17p11.2 deletion is shown. The RAI1 gene is indicated by a red arrow. Other deletions involving the 17p11.2 region described by Elsea and Girirajan3 are shown below. (b) Array CGH profile of chromosome 17 in SAG7567 and schematic representation of the RAI1 gene transcript. Black bars indicate qPCR amplicons used for confirmation of deletions found by arrayCGH. (c) Analysis by qPCR, which confirmed the occurrence of deletion of exon 3 of the RAI1 gene in six patients of SMS: PT1 (SAG6339) PT2 (SAG7131), PT3 (SAG7132), PT4 (SAG7571), PT5 (SAG5120) and PT6 (SAG6052), along with normal controls (NL1 and NL2). (d) Analysis by quantitative real-time PCR, which confirmed the occurrence of deletion of exon 2 of the RAI1 gene in one patient of SMS. The parental samples do not carry the deletion, shown with two normal controls (NL1 and NL2).
Table 2. 17p11.2 Copy number variation identified in the SMS cohort.
| Patient (no.)° | Start (bp) | End (bp) | Size (Mb) |
|---|---|---|---|
| SAG6339 | 16 658 950 | 20 336 467 | 3.67 |
| SAG7131 | 16 714 862 | 20 325 512 | 3.61 |
| SAG7132 | 16 676 257 | 20 325 512 | 3.64 |
| SAG7571 | 16 712 991 | 20 336 467 | 3.62 |
| SAG5120 | 16 697 860 | 20 325 512 | 3.62 |
| SAG6052 | 16 714 862 | 20 336 467 | 3.62 |
| SAG7567 | 17 507 060 | 17 645 576 | 0.14 |
Abbreviation: SMS, Smith–Magenis syndrome.
To confirm the results obtained by arrayCGH and to identify any additional smaller deletions, all of the SMS group and the SMS-like group of patients were analyzed by qPCR using an amplicon specific to the RAI1 gene. qPCR and arrayCGH results were consistent (Figure 1c) for all six patients with classical SMS deletions. Interestingly, in the patient of the atypical microdeletion, the results obtained by arrayCGH suggested the deletion ends at or near exon 3 of the RAI1 gene. However, using primers for the initial and medial portions of exon 3, qPCR determined that exon 3 was not deleted (data not shown). Furthermore, additional qPCR with exon 2 primers confirmed the presence of a de novo heterozygous deletion in this patient (Figure 1d).
RAI1 gene mutation screening in patients with no 17p11.2. deletion
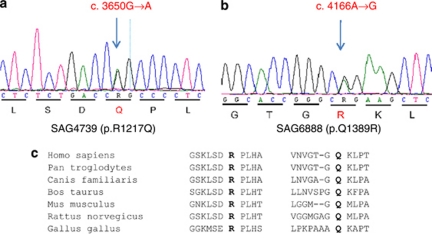
Using direct sequencing of the coding region of the RAI1 gene, we identified two heterozygous nonsynonymous variants in exon 3 of the gene (Figure 2). In patient SAG4739, a c.3650G>A alteration is predicted to cause an amino acid change from a glutamine to an arginine at position 1217 (p.R1217Q, Figure 2a). In patient SAG6888, a c.4166A>G alteration is predicted to cause an arginine to a glutamine substitution at position 1389 (p.Q1389R, Figure 2b). We also identified a new SNP (c.1143C>T; p.A381V) and several previously reported SNPs; allele frequencies of these SNPs in this cohort are shown in Supplementary Table 1.
Figure 2.
Automated sequence chromatograms showing RAI1 variants in patients. Triplet codon (underlined) and translated amino acids are shown. The two RAI1 gene heterozygous variations, (a) a c.3650G>A (p.R1217Q) in patient SAG4739 and (b) a c.4166A>G (p.Q1389R) in patient SAG6888 are shown. (c) Alignment of selected region of human RAI1 showing residues (in bold types) altered in patients that are conserved in other mammals.
The two residues involved in the alterations were found to be highly conserved (Figure 2c). Both alterations were absent in 150 control samples including 50 normal Brazilian controls. The pathogenicity of these two alterations remains to be determined and thus these are considered variants of unknown significance. Bioinformatics analyses were performed using PolyPhen (http://genetics.bwh.harvard.edu/pph/), SIFT (http://sift.bii.a-star.edu.sg/), PMut (http://mmb.pcb.ub.es/PMut/) and Panther (http://www.pantherdb.org/tools/). The variant p.R1217Q was predicted to be damaging by Panther, Pmut and SIFT but Polyphen suggested this to be a benign change. The variant p.Q1389R was predicted to be pathological or damaging by all four methods. The findings are summarized in Supplementary Table 2.
Functional characterization of nonsynonymous alterations identified in patients with SMS phenotype
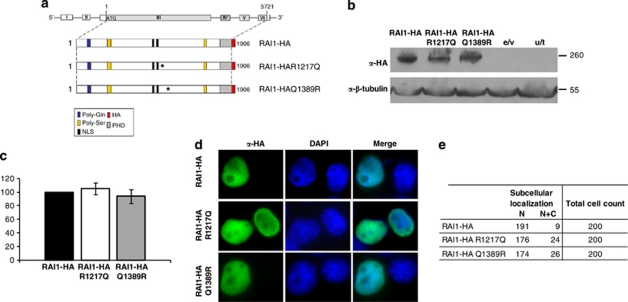
To investigate if the two new nonsynonymous changes present in the RAI1 protein: p.R1217Q. and p.Q1389R alter the molecular weight, subcellular localization or transcription activity function of the RAI1 protein, we generated both variants (Figure 3a) as described in Materials and methods. To determine the molecular weight of the resulting proteins, RAI1-HA, RAI1-HA R1217Q and RAI1-HA Q1389R clones were transiently transfected and 24 h post-transfection the cell lysates were run in a 4–20% gradient SDS-PAGE gel. As shown in Figure 3b, the molecular weight of both variant proteins is ∼260 kDa similar to the wild type.
Figure 3.
In vitro evaluation of two point mutations associated with SMS. (a) Schematic representation of RAI1-HA, RAI1-HA R1217Q and RAI1-HA Q1389R. In blue is represented the poly-Gln domain, in yellow: poly-Ser domains, the in silico described nuclear localization signals are depicted in black, in slanted line: the PHD domain. The coding sequence for HA epitope is represented in red. Both generated mutants were confirmed by DNA sequencing (data not shown). (b) The molecular weight of mutated proteins was calculated by western blot analysis with anti-HA antibody in Neuro-2a cells extracts. The obtained molecular weight is depicted and also the controls for the immunoreactivity are shown (e/v, extracts transfected only with the empty vector and u/t represents untransfected cells control). Anti-β-tubulin was used as a loading control. (c) The percentage of the reporter transcription activation is shown for RAI1-HA R1217Q (white) and RAI1-HA Q1389R (gray) compared with RAI1-HA wild-type protein (black). Values represent mean±SEM. (d) Each plasmid was transfected in Neuro-2a cells and immunofluorescence was performed with anti-HA (green) antibody, whereas nuclei staining is shown with DAPI. (e) The subcellular localization of 200 positive cells for the immunodetection is summarized. α, Antibody against.
For both variants, we evaluated the transcription factor activity as performed previously.15 As shown in Figure 3c, both RAI1-HA R1217Q and RAI1-HA Q1389R variant proteins showed an increment of 105.2±8.4 and 93.85±10.1 percentage of activation of luciferase activity respectively, when compared with the wild type as 100% (no significant changes for any variant). These data indicate that the variant polypeptides retained the transcription factor capacity. The subcellular localization of the variant proteins was also evaluated, and nuclear localization was found for both variant proteins (Figure 3d,e). Together these results indicate that the RAI1-HA R1217Q and RAI1-HA Q1389R variants are not affecting the synthesis, transcription factor activity or subcellular localization of the RAI1 protein.
Clinical characteristics of patients with or without the RAI1 gene defect
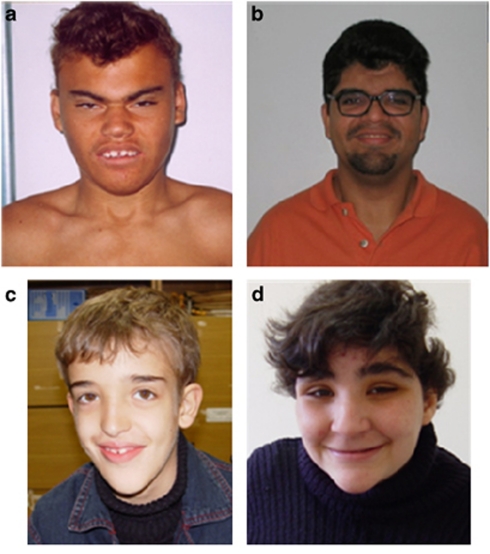
Of 30 patients clinically and molecularly evaluated, 6 had classical deletions (Table 1, column a), 1 had an atypical deletion (Table 1, column b) and 2 showed nonsynonymous alterations in the RAI1 gene (Table 1, column c). Clinical features of these patients are summarized in Table 1. All nine patients showed some intellectual disability and behavior disturbance, with self-injurious behavior and hyperactivity most frequently noted. Facial phenotypes of patients with a classical deletion, an atypical deletion and an RAI1 point mutation and from the SMS-like group are shown in Figure 4. The frequencies of characteristic features in all nine patients (Table 1, column a+b+c) are compared with the frequency of common SMS features analyzed by Edelman et al.19 For clinical comparison, nine patients with the 17p11.2 deletion or a RAI1 mutation were classified as the SMS group (Table 1, a+b+c) and the other 21 patients with some clinical features of SMS, but no chromosome 17p11.2 deletion or a RAI1 mutation were classified as the ‘SMS group' and the ‘SMS-like group', as suggested previously.20 No statistical differences were noted except for short broad hands, brachydactyly and iris abnormalities (Table 1).
Figure 4.
Facial features of patients with (a) a classical deletion (SAG6052), (b) an atypical deletion (SAG7567), (c) a nonsynonymous variant, p.R1217Q (SAG4739) and (d) a patient from the SMS-like group, with no known alteration.
Discussion
SMS is a contiguous gene deletion syndrome associated with multiple physical anomalies, intellectual disability, sleep disturbance and stereotypical behaviors. This combination of traits is associated with a heterozygous deletion at chromosome 17p11.2. Clinical and molecular analyses were performed to evaluate 30 patients suspected of having SMS. The evaluated patients had a broad range of phenotypes, with some characteristics typical of SMS (Table 1). More than 90% of the patients in this study had intellectual disability, delayed speech-language development and self-injurious behavior. Our findings showed that 30% (9/30) had a deletion in the 17p11.2 region or a point mutation in the RAI1 gene. Within this group, we found that 66% (6/9) carried a classic deletion, 11% (1/9) had an atypical deletion and 22% (2/9) had a missense alteration in the RAI1 gene. These data are similar to the proportion previously described by Vlangos et al.9
Normally, the primary transcript of the RAI1 gene is transcribed from exons 3, 4, 5 and part of exon 6. An atypical de novo deletion in one patient caused a loss of the noncoding exon 2, but not of the coding exons. Interestingly, the deleted region is relatively rich in CpG islands11 and thus an impact on transcription regulation of the RAI1 gene is speculated. Unfortunately, analyses to examine the RAI1 gene transcript were not possible because cultured cells from the patient were not available. To our knowledge, this is the first report of a partial deletion of the RAI1 gene in SMS group of patients.
In the six patients that showed a classic SMS deletion, the breakpoints were recurrent and coincided with the regions described as proximal SMS-REP and distal SMS-REP.12 This fact supports the idea that, in these classic patients, the deletion mechanism may be the erroneous alignment of low copy repeats (LCR), generating a deleterious nonallelic homologous recombination.
Finally, we screened for alterations in exons 3, 4, 5 and the coding portion of exon 6 (primary transcript) of the RAI1 gene in 24 patients. These were the 23 patients in whom no deletions were found in the 17p11.2 region plus the single patient who showed a partial deletion of the RAI1 gene. There are currently 15 reported mutations that have been described in the RAI1 gene.10, 11, 12, 13, 14 We have identified two additional nonsynonymous variants (p.R1217Q, p.Q1389R). The alterations are not located in RAI1 functional domains, but the substituted amino acids have different physical characteristics. One variant, p.Q1389R, was predicted to be pathological or damaging. However, bioinformatic analyses (Supplementary Table 2) did not suggest unequivocally pathological nature for variant p.R1217Q. In vitro functional analyses showed no abnormal molecular weight, subcellular localization or transactivational activity for any of these mutants, suggesting that they may be implicated in the association with other proteins or some other functional role of RAI1 that is not known to date, but fundamental to the SMS clinical phenotype. Further analyses of both variants in ethnically matched normal controls are warranted.
When patients are separated into groups of SMS (9 patients) or SMS-like individuals (21 patients), there were no statistical differences apparent in the distributions of age or gender (data not shown). When craniofacial and skeletal features were analyzed, only the features ‘small and broad hands' and ‘brachydactyly' were more frequent in the SMS group. There were no significant statistical differences between groups in the frequency of otorhinolaryngological, neurological and behavioral features. Iris abnormalities were reported in 30% of patients and it was the only feature with a significant statistical difference (between SMS and SMS-like groupings) among those less frequently reported in patients with SMS. In the study by Williams et al,20 ocular anomalies and brachydactyly also showed significant statistical differences. However, differences described by Williams et al,20 such as stereotypical behavior, seizures, craniofacial anomalies, ear infections, cleft lip and palate, hoarse voice, cardiac defects, digestive problems and short stature were not noted in this study. The analysis of the clinical data corroborated the idea that there are very similar phenotypes among patients with a 17p11.2 deletion and those with a mutation in the RAI1 gene.10, 20, 21
No obvious deletions or duplications were noted in the 21 SMS-like patients in this study. However, recently we have reported a female patient with a deletion at chromosome 1p36.32–1p36.33 and with overlapping clinical symptoms of the 1p36 deletion syndrome and SMS.22 Interestingly, Williams et al20 found monosomy of at least five different autosomal regions including one at 1p36.3 in patients with SMS-like phenotype without a deletion or mutation in the RAI1 gene.20 These findings points to the involvement of other genes that likely contribute to SMS or SMS-like phenotype.20, 22
We conclude that phenotypic similarity exists among patients with deletions in the 17p11.2 region or mutations in the RAI1 gene (SMS group) and patients with only a few features of the SMS phenotype (SMS-like group). Our findings add information toward the etiology of SMS and may facilitate a better diagnosis of SMS.
Acknowledgments
We are grateful to the patients and the parents for participation in this study. We thank Cindy Skinner, Lynn Dukes-Rimsky, Raewyn Lowe, Melissa Cook, Julianne Collins and Carlos Eduardo Frigério Domingues for providing assistance at various stages of this study. We thank Sarah H Elsea for sharing RAI1 gene primer sequences. This study was supported in part by funds from the SC Department of Disabilities and Special Needs, a fund from the Coordination for the Improvement of Higher Education Personnel (CAPES) foundation, Brazil to GHV, and a fund from the Jerome Lejeune Foundation to KW.
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies the paper on European Journal of Human Genetics website (http://www.nature.com/ejhg)
Supplementary Material
References
- Greenberg F, Guzzetta V, Montes de Oca-Luna R, et al. Molecular analysis of the Smith-Magenis syndrome: a possible contiguous-gene syndrome associated with del(17)(p11.2) Am J Hum Genet. 1991;49:1207–1218. [PMC free article] [PubMed] [Google Scholar]
- Smith ACM, Magenis RE, Elsea SH. Overview of Smith-Magenis syndrome. J Assoc Genet Technol. 2005;31:163–167. [PubMed] [Google Scholar]
- Elsea SH, Girirajan S. Smith-Magenis syndrome. Eur J Hum Genet. 2008;16:412–421. doi: 10.1038/sj.ejhg.5202009. [DOI] [PubMed] [Google Scholar]
- Smith ACM, Boyd K, Elsea SH, et al. GeneReviews at GeneTests: Medical Genetics Information Resource (database online) Seattle: Copyright, University of Washington; 1997–2010. Smith-Magenis Syndrome. [Google Scholar]
- Dykens EM, Finucane BM, Gayley C. Brief report: cognitive and behavioral profiles in persons with Smith-Magenis syndrome. J Autism Dev Disord. 1997;27:203–211. doi: 10.1023/a:1025800126086. [DOI] [PubMed] [Google Scholar]
- De Leersnyder H, de Blois MC, Vekemans M, et al. beta(1)-adrenergic antagonists improve sleep and behavioural disturbances in a circadian disorder, Smith-Magenis syndrome. J Med Genet. 2001;38:586–590. doi: 10.1136/jmg.38.9.586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith AC, Dykens E, Greenberg F. Sleep disturbance in Smith-Magenis syndrome (del 17 p11.2) Am J Med Genet. 1998;81:186–191. [PubMed] [Google Scholar]
- Potocki L, Shaw CJ, Stankiewicz P, et al. Variability in clinical phenotype despite common chromosomal deletion in Smith-Magenis syndrome [del(17)(p11.2p11.2)] Genet Med. 2003;5:430–434. doi: 10.1097/01.gim.0000095625.14160.ab. [DOI] [PubMed] [Google Scholar]
- Vlangos CN, Yim DK, Elsea SH. Refinement of the Smith-Magenis syndrome critical region to approximately 950 kb and assessment of 17p11.2 deletions. Are all deletions created equally. Mol Genet Metab. 2003;79:134–141. doi: 10.1016/s1096-7192(03)00048-9. [DOI] [PubMed] [Google Scholar]
- Slager RE, Newton TL, Vlangos CN, et al. Mutations in RAI1 associated with Smith-Magenis syndrome. Nat Genet. 2003;33:466–468. doi: 10.1038/ng1126. [DOI] [PubMed] [Google Scholar]
- Bi W, Saifi GM, Shaw CJ, et al. Mutations of RAI1, a PHD-containing protein, in nondeletion patients with Smith-Magenis syndrome. Hum Genet. 2004;115:515–524. doi: 10.1007/s00439-004-1187-6. [DOI] [PubMed] [Google Scholar]
- Bi W, Saifi GM, Girirajan S, et al. RAI1 point mutations, CAG repeat variation, and SNP analysis in non-deletion Smith-Magenis syndrome. Am J Med Genet A. 2006;140:2454–2463. doi: 10.1002/ajmg.a.31510. [DOI] [PubMed] [Google Scholar]
- Girirajan S, Elsas LJ, Devriendt K, et al. RAI1 variations in Smith-Magenis syndrome patients without 17p11.2 deletions. J Med Genet. 2005;42:820–828. doi: 10.1136/jmg.2005.031211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Truong HT, Dudding T, Blanchard CL, et al. Frameshift mutation hotspot identified in Smith-Magenis syndrome: case report and review of literature. BMC Med Genet. 2010;11:142. doi: 10.1186/1471-2350-11-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmona-Mora P, Encina CA, Canales CP, et al. Functional and cellular characterization of human Retinoic acid induced 1 (RAI1) mutations associated with Smith-Magenis Syndrome. BMC Mol Biol. 2010;11:63. doi: 10.1186/1471-2199-11-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmona-Mora P, Walz K. Retinoic acid induced 1, RAI1: a dosage sensitive gene related to neurobehavioral alterations including autistic behavior. Curr Genomics. 2010;11:607. doi: 10.2174/138920210793360952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Girirajan S, Truong HT, Blanchard CL, Elsea SH. A functional network module for Smith-Magenis syndrome. Clin Genet. 2009;75:364–374. doi: 10.1111/j.1399-0004.2008.01135.x. [DOI] [PubMed] [Google Scholar]
- Griggs BL, Ladd S, Decker A, et al. Identification of ectodysplasin-A receptor gene deletion at 2q12.2 and a potential autosomal MR locus. Eur J Hum Genet. 2009;17:30–36. doi: 10.1038/ejhg.2008.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edelman EA, Girirajan S, Finucane B, et al. Gender, genotype, and phenotype differences in Smith-Magenis syndrome: a meta-analysis of 105 cases. Clin Genet. 2007;71:540–550. doi: 10.1111/j.1399-0004.2007.00815.x. [DOI] [PubMed] [Google Scholar]
- Williams SR, Girirajan S, Tegay D, et al. Array comparative genomic hybridisation of 52 subjects with a Smith-Magenis-like phenotype: identification of dosage sensitive loci also associated with schizophrenia, autism, and developmental delay. J Med Genet. 2010;47:223–229. doi: 10.1136/jmg.2009.068072. [DOI] [PubMed] [Google Scholar]
- Toulouse A, Rochefort D, Roussel J, et al. Molecular cloning and characterization of human RAI1, a gene associated with schizophrenia. Genomics. 2003;82:162–171. doi: 10.1016/s0888-7543(03)00101-0. [DOI] [PubMed] [Google Scholar]
- Vieira G, Rodriguez JD, Boy R, et al. Differential diagnosis of Smith-Magenis syndrome: 1p36 deletion syndrome. Am J Med Genet A. 2011;155:988–992. doi: 10.1002/ajmg.a.33960. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.