Abstract
Background
Although the magnitude of obstetric fistulae (OF) is reported to have decreased in industrialized countries, it is still a major problem in developing countries. While the main cause of OF is prolonged obstructed labour without prompt medical attention, misconceptions about OF exist.
Objective
To determine awareness and perceived causes of OF in rural areas of southern Tanzania.
Methods
A cross-sectional survey was conducted among women of reproductive age, men, health personnel, birth attendants, community leaders and OF cases using qualitative and quantitative approaches.
Results
More than 60% of interviewees reported to be aware of OF with a connotation of urine in the names. Perceived causes of OF include sorcery, prolonged labour, delivering by operation where doctors/nurses make mistakes perforate the urinary bladder, physique of the expecting mother, poor skills of doctors/nurses to conduct caesarean section, young or old age of an expecting mother and having sex before recovering from the operation.
Conclusion
Although OF is not reported to exist, most of the interviewees were aware of them. However, were few respondents are able to mention the main cause of OF. Maternal health education is important as a strategy to minimize the spread of misconceptions about causes of OF.
Keywords: Obstetric fistulae, Tanzania
Introduction
Obstetric fistulae (either vesicovaginal or rectovaginal) are types of morbidity that are normally caused by prolonged labour during childbirth without timely medical intervention like a caesarean section. The World Health Organization (WHO), estimates between 50,000 to 100,000 women develop obstetric fistulae (OF) each year and over two million women currently live with OF1, 2.
Although there is enough literature on OF, available data on the magnitude of this condition are diverse and considered severely understated; hence may be unreliable3 – 6. It is estimated that about 2 million women are living with OF worldwide, with a greater proportion being reported from sub-Saharan Africa and South Asian countries7, 8.
While in developed countries the reported aetiology of OF include surgery, malignancy, radiotherapy and coital injury and neglected foreign bodies, in developing countries prolonged labour remains the main reported cause of OF6, 9, 10. From various regions within sub-Saharan Africa, the underlying factors for OF are considered biological, social and cultural, behavioural and environmental11. Some of the examples encircling these factors are young maternal age at delivery, poverty, childhood malnutrition, illnesses a genetics and health seeking behaviour12, 13.
Various misconceptions about causes of OF have previously been reported3. In one study conducted in Uganda, traditional birth attendants associated OF with surgery (caesarean section); either because physicians delay to operate the mother or use of ‘metal forceps to pull out the baby’. Other reported perceived causes of OF include having a full bladder and rectum during labour and birth attendants having nails that are too long or without use of gloves during delivery6.
In this article we use data generated from three rural districts in Southern Tanzania with the aim of getting strategies for improving access and utilization of safe motherhood services in the area. Data related to perceived causes of OF are presented in this paper.
Methods
Study site
Mtwara Region is located in the south-east of Tanzania bordering Mozambique. The region is divided into six districts: Mtwara rural and urban, Masasi, Newala, Tandahimba and Namtumbo. Each district, with the exception of Mtwara rural and Namtumbo, is served with a district hospital. There is also a mission hospital (St Benedict's Ndanda Hospital) in Masasi that serves as a referral hospital besides a Regional hospital at Mtwara regional headquarter. In addition, according to the Ministry of Health and Social Welfare, there are 16 health centres and 163 dispensaries serving the community as part of the primary-health level care. The three districts have a total population for women of reproductive age (15 – 49 years) of 175,468 (25.7% of the total population in these districts)14.
On average, the area is characterized by low fertility maternity indicators. For example, there is a total fertility rate of 4.8 as compared to 6.5 for the rural national figure and 37.6% of expecting mothers are delivered by professional health personnel as compared to the national figure of 46.3%15. Using the average age at first marriage as a proxy for average age at first delivery in the study area, it is estimated to be about 18.4 years not differing significantly from the national figure of 18.6 years15.
Study design
A cross-sectional explorative study was conducted to form a baseline survey in addressing the problem of obstetric fistula. This was with the aim of building capacities of health care systems through training of doctors, and nurses/midwives in obstetric fistula awareness creation, prevention, surgical repair and post operative care. For this purpose, three districts of Mtwara region namely Mtwara Rural, Tandahimba and Newala were earmarked as study project sites.
A random sample of households was selected from each district to get adult (above 18 years) men and women to be involved the study. A three-stage multi-cluster sampling design was employed. The first stage involved selection of wards from each of the three districts. An equal allocation of five wards was randomly selected from the existing wards of each district, therefore, a total of 15 clusters (wards) in all three districts were selected. The second stage was a selection of three villages from each district. Following selection of the villages, the third stage involved randomly selecting 10 households falling within the selected villages. Therefore, a total of 150 households from each district were available for interviews.
Data collection
In each household, one randomly selected adult was interviewed using interview guide. Furthermore, a list of all health facilities in the study area was obtained to form another sampling frame. These facilities were categorized by type and ownership (hospital, health centre and dispensary and by public or private wonership). All hospitals and all health centres within the three districts were assessed. Also we used Focus Group Discussions (FGDs) and in-depth interviews (IDIs) among community leaders, traditional and formal health care providers and Districts' health team leaders to assess the perception and attitudes on safe motherhood.
In each district we conducted two FGDs (one for women in the reproductive age and the other with men). There was an additional of one FGD with the Traditional Birth Attendants in Newala District. Furthermore, we performed a total of 32 IDIs with community leaders (both men and women), health facility in-charges including District and Regional Medical Officers and some other health care providers.
Ethical considerations
Ethical clearance for the study was obtained from the National Institute for Medical Research Review Board. Permission to conduct the study was requested from the District Executive Directors and from village leaders. Informed verbal consent to participate in the study was sought from respondents and an assurance of confidentiality of the gathered information was given. Confidentiality was adhered to by conducting interviews in well established private location as suggested by interviewees. During data collection, we used experienced interviewers with a medical or sociology background. Because of cultural sensitivity around reproductive issues, interviewers were sex-matched such that female interviewers interviewed women and male interviewers interviewed men.
Results
We interviewed 334 participants (participation rate of 74.2%). Many of these, (72, 21.9%), belonged to the 25–29 years age group. More than a half of participants had completed primary education. Peasantry was the main occupation employing 294 (88%) of the sample. The majority (293, 87.7%) were Moslems and about three quarters, (242; 72.5) were currently married (table 1).
Table 1.
Characteristics of respondents in the household sample) (n = 334)
| Characteristic | Number (%) |
| Sample origin (District) | |
| Mtwara rural | 110 (32.9) |
| Newala | 106 (31.7) |
| Tandahimba | 118 (35.3) |
| Sex | |
| Male | 31 (9.3) |
| Female | 303 (90.7) |
| Age group (years) | |
| 15 – 19 | 20 (6.1) |
| 20 – 24 | 50 (15.2) |
| 25 – 29 | 72 (21.9) |
| 30 – 34 | 55 (16.7) |
| 35 – 39 | 48 (14.6) |
| 40 – 44 | 27 (8.2) |
| 45 – 49 | 21 (6.4) |
| 50+ | 36 (10.9) |
| Highest education level | |
| Never attended school | 74 (23.6) |
| Some primary education | 55 (17.5) |
| Completed primary education | 179 (57.0) |
| Above primary education | 25 (8.0) |
| Main occupation | |
| Peasantry | 294 (88.0) |
| Housewife | 14 (4.2) |
| Petty business | 8 (2.4) |
| Formal sector | 6 (1.8) |
| Fishing | 6 (1.8) |
| Other (casual, unemployed) | 6 (1.8) |
| Religion | |
| Christian | 39 (11.7) |
| Muslim | 293 (87.7) |
| Other | 2 (0.6) |
| Marital status | |
| Never married | 38 (11.4) |
| Currently married | 242 (72.5) |
| Divorced/separated | 46 (13.8) |
| Widow | 7 (2.1) |
A total of 297 out of 303 women (97.7%) reported to have ever been pregnant, and were therefore, at risk of labourcomplications that include OF. Of these, 179 (60.3%), delivered for the first time at a an age less than 20 years. The first pregnancy was reported by 65 (21.9%) of all women interviewed. Of ‘ever pregnant women’, 94 (31.6%) were of high gravidity (more than three).
Of the 291 mothers who reported to have delivered their youngest child, about two thirds 191 (65.6%), delivered at a health facility. However, data from facility records indicated that a total number of deliveries at the health facilities remained relatively stable in 2006 (3,520 deliveries), 2007 (3,491 deliveries) and in 2008 (3,505 deliveries). Ninety deliveries (30.9%) took place at home and other places, including on the way to the health facility and assisted by an elderly woman. Nevertheless, a high proportion of women, 258 (88.7%) attended ANC before delivery.
Reasons given for delivering at places other than health facilities included lack of money, lack of family support and long distances to the health facility. The reported average distance was 2.4 km (mean travelling time, 1.3 and SD= 1, hours; ranging from 10 minutes to 7 hours). Data from the FGDs and IDIs showed the justification of expecting mothers delivering at places other than health facilities for example, TBAs live in the vicinity of expecting mothers' villages; hence, these women do not incur transport costs, as one woman from Mtwara Rural pointed out: “… you see, because of poverty we cannot afford transport costs to go to a hospital. Therefore, we use our traditional birth attendants who happen to be neighbours. We know them and trust them”. (Interview, Mtwara Rural, February 2009). In addition, health care providers interviewed at health centres reported that TBAs do not charge for some things in cash (for instance, to buy gloves and food) as charged in health facilities.
A health care provider in Newala noted that the number of mothers delivering at home increases during the rainy season when the roads become impassable making transport by bicycles more difficult. Furthermore, some mothers fear being bewitched if bad people knew that they were pregnant when attending clinics. Similarly, mothers who believe that the use of the traditional healing helped them getting pregnant believe that going to the clinic would violate conditions given by a traditional healer. Additionaly, breastfeeding mothers who become pregnant feel shy about going to the clinic as they may be considered fond of sex. However, the demand to know one's sero-status was reported to have increased the number of pregnant women and their significant other seeking health care services.
About a quarter of women, 73 (24.6%), reported experiencing some complications during delivery. Complications mentioned included excessive bleeding, eclampsia, retained placenta and a very delivery canal. It was reported during the FGD with the women that, in few cases mothers die from such complications.
Awareness of obstetric fistulae
Although out of 334 women and men interviewed, 204 (61.1%) reported awareness of OF and this was almost equally distributed between the three districts, few respondents, 56 (18.5%) and 6 (19.4%), among women and men respectively, reported to have actually seen a case of OF. Different local names exist using terms like “Fistula/Kistula/Vistula/Pistula”, “Jolojolo/ Mjolojolo” and other names ending with “mkojo” (urine); for example, “homa ya mkojo, tatizo la mkojo” and “nkojo”. As few as 3 mothers (two from Mtwara Rural District and one from Newala) reported to have ever experienced the OF problem.
On one hand, data from FGDs and IDIs showed that all regional, district and health centre staff interviewed reported that OF is not a big health problem in their areas because few cases have been detected and referred for repair at Ndanda and other two hospitals in the neighbourhood (Lindi and Nyangao). A health-care provider interviewed at Tandahimba hospital, for instance, stated, “I have been at this facility for the past six years … I have never encountered such a case” (Interview, Tandahimba, February 2009). A Health Centre in-charge interviewed at Nanyamba health centre recalled only two OF cases from Mozambique three years back.
Another health-care provider interviewed in Newala could remember only two cases in the past six years, adding, “These women came from Mozambique … not from our catchment area” (Interview, Newala, February 2009). A Mahurunga health centre staff interviewed recalled a case from Mozambique three years ago. A regional medical official interviewed at Ligula (Mtwara Regional Hospital) reported, “we have detected several cases of fistula … we refer them to Lindi, Nyangao and Ndanda for repair … Unfortunately, we do not record such cases … we never get feedback on referred cases” (Interview, Mtwara, February 2009).
On the other hand, data from FGDs (with men and women) and IDIs (with OF cases) indicated that there may be many cases of OF in the study area. During the FGDs in Mtwara Rural, for example, four known cases were reported. One woman who participated in the FGD had this problem and shared her experience with the research team and was willing to undergo repair if assisted. Three other cases were reported during an IDI with a case of OF in Nanyamba. An OF-case interviewed in Newala reported that many women in Masasi face this problem. “… as you may know, fistula is a shameful problem to an affected woman … women keep it a secret due to stigma associated with it … Majority of affected women are too poor to afford costs involved [transport and food costs] … Treatment is free. In my view, this might not be a big problem in Luagala but women in Masasi district (her place of origin) are much more affected … My two sisters have a similar problem … they are unable to seek proper treatment as I did” (Interview, Newala, February 5, 2009).
Unfortunately, the two reported sisters reside in Masasi district (outside the study area) and thus could not available for interviewing. Similarly, it was not possible to establish from the recorded interview, the relationship (by blood or member of her extended family) between this woman and those sisters. Hence, this quotation is not suggesting that OF could be genetic.
Sources of information about obstetric fistulae
The majority of the community members were not aware of the term fistula. Among those who were aware, they had information from the clinics and leaflets distributed at the health centres supplied from Ndanda hospital. Some got information from the electronic media (radio, TV) or they had undergone fistula repair. Some of the terms that refer to fistula conditions were captured from FGDs and IDIs conducted in the three districts: homa ya mkojo and mjolojolo, which suggested that fistula cases existed in the study areas.
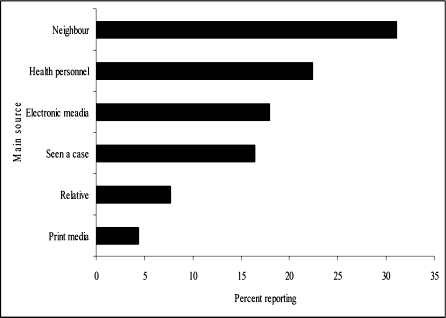
Similar information obtained from the survey concerning sources of information about fistula among reporting women are summarized in figure 1.
Figure 1.
Reported main sources of information about fistula, Mtwara Region, 2009 (n = 183 women)
Perceived causes of obstetric fistulae
Through probing, only 9 (3%) women were able to associate OF with prolonged labour. In general, it was reported that women of very young or advanced age from poor families or those living far from the health facilities (up to 7 km or across the border in Mozambique), those who do not attend ANC or those who deliver but experience prolonged labour were reported to be at higher risk of fistula. Out of 96 women citing possible causes of OF, 23 (24.0%) thought OF was caused by a wrong operation during caesarean section (CS), 11 (11.5%0 thought the baby was too big causing a raptured uterus and 3 (3.1%) said it was caused by poor family planning especially not spacing children properly. Other reported causes include the child passing through the wrong path during delivery, 2 (2.1%), and a woman having sex during the puerperal period, 2 (2.1%).
Similar and additional perceived causes of OF were captured from the FGDs and IDIs. Some of the reasons mentioned were: sorcery, prolonged labour, delivering by an operation where doctors/nurses make mistakes perforating the urinary bladder, doctors/nurses making mistakes when removing catheters puncturing the urinary bladder, physique of expecting mother (less than 150 cm of height and too narrow delivery canal), doctors/nurses have poor skills (they are on training or recently graduated) to conduct ceasarians and having sex before recovering from CS.
Discussion
Obstetric fistulae are constantly emerging among serious and devastating maternal morbidities especially in resource limited countries16. It is well documented that prolonged obstructed labour without appropriate medical attention is the main cause of obstetric fistula3, 16 – 19.
From this study, although more than 60% of men and women interviewed were aware of obstetric fistula and cited different names of the condition, less than 20% reported having actually ever seen a case of OF. A report from the neighbouring country indicates that there is always a tendency to conceal the existence of this condition7.
In this study, a shockingly very low proportion (3%) of women mentioned obstetric trauma especially prolonged obstructed labour as the main cause of OF, compared to other reports that suggest a higher proportion of women reporting it as the main cause3, 17, 19, 20.
Possibly the discrepancy between these reports and our study is that most of the previous reports were based on hospital data and most of them who had fistula repair are more likely to remember or speculate on the possible cause.
We report false impressions about causes of OF. Such beliefs have been previously reported in the region3, 6, 21. However, in this study a big proportion (24%) of women associated OF with a wrong operation during CS. The linking of OF with results of trauma due to surgery or mishandling of patients by hospital personnel has a strong negative impacton encouraging promptly seeking obstetric care and accessibility to emergency services.
One of the main limitations in this study was the use of the term ‘fistula’ that might not be familiar to most of the respondents. Nevertheless, interviewers used more time to explain the nature of the condition. We think there was no or minor information bias introduced through this process. Furthermore, we could not gather views from any health facility running fistula repairs because there was none.
Few respondents are able to correctly cite the main cause of OF. However, misconceptions on causes of OF exist including a loose uterus, poor use of family planning, the child passing through the wrong path during delivery, a very big baby causing a ruptured uterus, a woman having sex during the puerperal period, sorcery, mistakes of doctors by puncturing the urinary bladder and a woman having sex before recovering from the caesarean section.
Conclusion
Most women and men in rural areas of southern Tanzania are aware of obstetric fistulae. Nevertheless, probably because of stigma associated with the condition, by some people, especially women, the condition is reported not to exist.
These findings may suggest a need for interventions that may improve access to maternal health care and availability of pre-natal services including emergency obstetric care especially in rural areas. Findings also point towards making maternal health education essential not only to women but also to men, family members and the society, a strategy that is likely to minimize spread of misconceptions about causes of obstetric fistulae.
Acknowledgements
Authors thank the African Medical Research Foundation (AMREF) for financial and logistical support. We thank all Districts Health Personnel that were involved in the study and all study participants for their valuable information.
References
- 1.AbouZahr C. Global Burden of Maternal Deaths and Disability. British Medical Bulletin. 2003;67:1–11. doi: 10.1093/bmb/ldg015. [DOI] [PubMed] [Google Scholar]
- 2.Obstetric Fistulae: A Review of Available Information. WHO/MCH/MSM/91.5; 1991. [Google Scholar]
- 3.Hassan MA, Ekele BA. Vesicovaginal fistula: Do the patients know the cause? Annals of African Medicine. 2009;8:122–126. doi: 10.4103/1596-3519.56241. [DOI] [PubMed] [Google Scholar]
- 4.Proceedings of the Workshop on Data Methodologies for Estimating Obstetric Fistula, May 2007, New Delhi. [Google Scholar]
- 5.Semere L, Nour N. Obstetric Fistula: Living with Incontinence and shame. Reviews in Obstetrics and Gynecology. 2008;1:193–197. [PMC free article] [PubMed] [Google Scholar]
- 6.Keri L, Kaye D, Sibylle K. Referral practices and perceived barriers to timely obstetric care among Ugandan traditional birth attendants. African Health Sciences. 2010;10:75–81. [PMC free article] [PubMed] [Google Scholar]
- 7.Murk W. Experiences with obstetric fistula in Rural Uganda. Yale Journal of Biology and Medicine. 2009;82:79–82. [PMC free article] [PubMed] [Google Scholar]
- 8.Wall LL. Obstetric vesicovaginal fistula as an international public-health problem. Lancet. 2006;368:1201–1209. doi: 10.1016/S0140-6736(06)69476-2. [DOI] [PubMed] [Google Scholar]
- 9.Kelly J. Vesico-vaginal and recto-vaginal fistulae. Journal of the Royal Society of Medicine. 1992;85:257–258. doi: 10.1177/014107689208500505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ghatak DP. A study of urinary fistulae in Sokoto, Nigeria. Journal of the Indian Medical Association. 1992;90:285–287. [PubMed] [Google Scholar]
- 11.Miller S, Lester F, Webster M, Cowan B. Obstetric fistula: a preventable tragedy. Journal of Midwifery & Women's Health. 2005;50:286–294. doi: 10.1016/j.jmwh.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 12.Wall LL, Karshima JA, Kirschner C, Arrowsmith SD. The obstetric vesicovaginal fistula: Characteristics of 899 patients from Jos, Nigeria. American Journal of Obstetrics and Gynecology. 2004;190:1011–1019. doi: 10.1016/j.ajog.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 13.Tsui AO, Creanga AA, Ahmed S. The role of delayed childbearing in the prevention of obstetric fistulas. International Journal of Gyaecology and Obstetrics. 2007;99(S1):S98–S107. doi: 10.1016/j.ijgo.2007.06.024. Epub 2007. [DOI] [PubMed] [Google Scholar]
- 14.United Republic of Tanzania, author. Populations Projections, Mainland and Zanzibar 2006 Population and Housing Census. Dar-es-Salaam: Ministry of Planning and Economic Affairs; [Google Scholar]
- 15.National Bureau of Statistics (NBS) [Tanzania] and ORC Macro, author. Tanzania Demographic and Health Survey (TDHS) 2004–05. Dar es Salaam, Tanzania: National Bureau of Statistics; 2005. Calverton, MD, USA: ORC Macro. [Google Scholar]
- 16.Muleta M. Obstetric fistula in developing countries: a review article. Journal of Obstetrics and Gynaecology Canada. 2006;28:962–966. doi: 10.1016/S1701-2163(16)32305-2. [DOI] [PubMed] [Google Scholar]
- 17.Muleta M, Rasmussen S, Kiserud T. Obstetric fistula in 14,928 Ethiopian women. Acta Obstetricia et Gynecologica Scandinavica. 2010;89:945–951. doi: 10.3109/00016341003801698. [DOI] [PubMed] [Google Scholar]
- 18.Sachdev PS, Hassan N, Abbasi RM, Das CM. Genito-urinary fistula: a major morbidity in developing countries. Journal of Ayub Medical College, Abbottabad. 2009;21:8–11. [PubMed] [Google Scholar]
- 19.Melah GS, Massa AA, Yahaya UR, Bukar M, Kizaya DD, El-Nafaty AU. Risk factors for obstetric fistulae in north-eastern Nigeria. Journal of Obstetrics and Gynaecology. 2007;27:819–823. doi: 10.1080/01443610701709825. [DOI] [PubMed] [Google Scholar]
- 20.Gharoro EP, Agholor KN. Aspects of psychosocial problems of patients with vesico-vaginal fistula. Journal of Obstetrics and Gynaecology. 2009;29:644–647. doi: 10.1080/01443610903100609. [DOI] [PubMed] [Google Scholar]
- 21.Nathan LM, Rochat CH, Grigorescu B, Banks E. Obstetric fistulae in West Africa: patient perspectives. American Journal of Obstetrics and Gynecology. 2009;200(5):e40–e42. doi: 10.1016/j.ajog.2008.10.014. Epub 2008 Dec 27. [DOI] [PubMed] [Google Scholar]