Abstract
Background
Few studies have associated anthropometric measurements and lipid profile with hypertension in adult populations and to the best of our knowledge none has been done in Turkey
Objectives
To relate anthropometric derivatives of overweight/obesity with hyperlipidemia status in a group of Turkish hypertensive adults.
Methods
Six hundred forty nine (307 male, 342 female) hypertensive adults aged between 20 and 64 yearswere included in the study.
Results
The mean systolic and diastolic blood pressure (BP) of participants were measured as 147.6±17.2 and 91.4±10.4 mmHg for males and 149.9±16.3 and 91.1±9.4 mmHg for females, respectively. With respect to BMI classification systolic BP was significantly higher in obese males and females, and diastolic BP was only higher in obese females (p<0.05). According to BMIs for lipid profile, high-density lipoprotein-cholesterol (HDL-C), total cholesterol (TC) levels were found to be lower in normal females than other BMI groups. Age and waist circumference (WC) in particular was the most related factor for systolic and diastolic BP in both genders (p<0.05).
Conclusions
This study indicates most hypertensive adults surveyed were overweight and obese. Furthermore, age and WC were the important factors that affects the systolic and diastolic BP in both genders.
Keywords: Hypertension, body mass index, waist circumference, lipid profiles
Introduction
Hypertension, as defined by Joint National Committee-7, is an important public health problem worldwide and is the most widely recognized modifiable risk factor for cardiovascular disease, cerebrovascular disease (stroke) and end-stage renal disease1,2. Worldwide, prevalence estimates for hypertension may be as much as one billion individuals per year, and approximately 7.1 million deaths per year may be attributable to it3. In particular, Turkey has a high prevalence figure of hypertension: age- and gender-adjusted prevalence was 31.8% 4.
Obesity is a major independent risk factor for hypertension5. The performance of different anthropometric measurements and indices in predicting obesity-related outcomes has been addressed in several reports6–8. There is, however, controversy regarding which anthropometric indicator best defines obesity and conveys the highest risk of hypertension5. Cross-sectional and prospective epidemiological studies have shown that blood pressure (BP) and, worse still, hypertension increases significantly with higher body mass index (BMI) and waist circumference (WC) 7,8.
Hypertension is also positively associated with a cluster of risk factors characteristic of the metabolic syndrome, of which overweight/central obesity could be the cornerstone. Indeed it is recommended that management of arterial hypertension should focus both on lowering high BP and correcting associated lipid disorders9.
The present study was therefore undertaken to determine and evaluate the overweight/obesity and hiperlipidemia status in a group of hypertensive adults.
Methods
This study was conducted among 649 (307 male, 342 female) hypertensive adults with an age range of 20 to 64 years between November 2009 and May 2010 in Ankara, Turkey. The participants were chosen randomly from the nephrology clinics of governmental hospitals. All subjects were hypertensive and they had no chronic diseases. The study design was case series. In total, 931 individuals were admitted to the clinics but the individuals who had not had lipid profile analyses in the last month were excluded from the study sample. We used data of individuals who had had lipid profile analyses in the last month. The lipid profile included total cholesterol (TC), high-density lipoprotein-cholesterol (HDL-C), low-density lipoprotein-cholesterol (LDL-C) and triacylglycerols (TG). Early-morning venous blood samples had been obtained from each participant for biochemical screening tests, following a twelve-hour overnight fasting. Professional staff had performed venipuncture by using vacutainers to obtain 15 ml of whole blood. Blood had been centrifuged for plasma separation at the governmental hospitals where the actual biochemical analyses were performed. Roche Diagnostic Kits were used for TG, HDL-C and TC analysis. The LDL-C was calculated by Friedewald and colleagues' formula; LDL-C= TC − (HDL-C + (TG/5)) 10.
In this study, BP measurements were performed by specially trained and experienced healthcare workers. Sitting BP was measured after 10 minutes of rest with a standard adult sphygmomanometer at the beginning of the interview and again at the end. The mean BP value was used for analysis. Hypertension was defined on the basis of the Joint National Committee-7 cut-off point of 140 mmHg and above for systolic blood pressure (SBP) and/or 90 mmHg and above for diastolic blood pressure (DBP), and also took into account whether the subject was on antihypertensive medication11. After measurement of SBP and DBP volunteers were included if they met these criteria:
All anthropometric measurements were taken by trained dieticians and with participants wearing light clothes and no shoes. A portable scale was used to measure body weight to the nearest half-kilogram. Height was measured to the nearest 0.1 cm with a wall-mounted stadiometer. Body mass index (kg/m2) was calculated by weight in kilograms divided by the square of height in meters. Adults were classified according to their BMI into three groups: normal weight (BMI: 18.5–24.9 kg/m2), overweight (BMI: 25.0–29.0 kg/m2) and obese (BMI e” 30 kg/m2)12. Waist circumference was measured above the iliac crest and below the lowest rib margin at minimum respiration. Hip circumference (HC) was measured at the widest part of the hip at the level of the greater trochanter to the nearest half-centimetre13. The waist and hip circumferences were measured with a flexible tape.
None of the participants used any vitamins, mineral supplements or oral contraceptives. None of the females were pregnant or breast-feeding. The participants were informed about the subject, purpose and rules of the research. Each participant signed a voluntary participation form.
Data Analysis
The data analysis was carried out using SPSS version 13.0 software (SPSS Inc., Chicago, IL, USA). The descriptive statistics of means with 95% coefficient interval were used to summarise the data collected. Means were compared by using independent, the t-test according to gender. Pearson's correlation coefficients were used for continuous variables. Oneway analysis of variance (ANOVA) was conducted to compare the anthropometric measurements and lipid profiles of the participants on BMI classification. A significance level of 0.05 was used in all statistical analyses done in this study.
Results
Mean age, BP, anthropometric measurements and blood lipid levels of participants according to gender are given in table 1. Mean age of participants was 54.1±12.4 years. Mean SBP and DBP of participants were 147.6±17.2 and 91.4±10.4 mmHg for males and 149.9±16.3 and 91.1±9.4 mmHg for females, respectively. There were significant differences between height, BMI, HC, TC, HDL-C and LDL-C according to gender (p<0.05). No statistically significant differences were found in BP measurements by gender (p>0.05); but SBP was found to be higher in females than in males.
Table 1.
Comparison of general characteristics according to gender
| Male (n:307) Mean ±SD |
Female (n:342) Mean ±SD |
Total (n:649) Mean ±SD |
p | |
| Age (year) | 53.5±12.9 | 54.6±11.9 | 54.1±12.4 | 0.263 |
| SBP (mmHg) | 147.6±17.2 | 149.9±16.3 | 148.8±16.8 | 0.076 |
| DBP (mmHg) | 91.4±10.4 | 91.1±9.4 | 91.3±9.9 | 0.707 |
| Body weight (kg) | 71.2±17.4 | 70.6±16.8 | 70.9±17.1 | 0.652 |
| Height (cm) | 165.6±8.6 | 158.5±10.4 | 161.9±10.2 | <0.001* |
| BMI (kg/m2) | 26.0±5.9 | 28.1±6.4 | 27.1±6.3 | <0.001* |
| WC (cm) | 94.1±16.1 | 93.4±14.9 | 93.7±15.5 | 0.558 |
| HC (cm) | 103.5±10.2 | 107.3±11.0 | 105.5±10.8 | <0.001* |
| WHR | 0.9±0.1 | 0.9±0.1 | 0.9±0.1 | <0.001* |
| TC(mg/dL) | 201.5±46.1 | 216.0±44.4 | 209.1±45.8 | <0.001* |
| HDL-C(mg/dL) | 41.4±12.3 | 44.7±11.6 | 43.1±12.0 | <0.001* |
| LDL-C(mg/dL) | 129.6±54.3 | 138.8±48.8 | 134.6±51.6 | 0.036* |
| TG(mg/dL) | 186.0±111.2 | 179.0±76.2 | 182.2±93.9 | 0.384 |
SBP: Systolic blood pressure, DBP: diastolic blood pressure, BMI: Body mass index, WC: Waist circumference, HC: Hip circumference, WHR: Waist-hip ratio, TC: Total cholesterol, HDL-C: High density lipoprotein-cholesterol, LDL-C: Low density lipoprotein-cholesterol, TG: Triglyceride
p<0.05
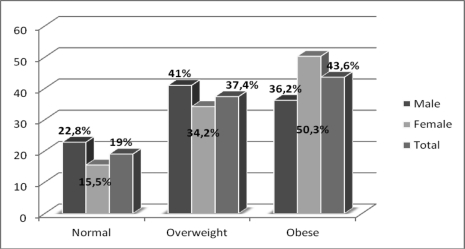
In the evaluation of BMI classification, 43.6% of subjects were classified as obese and 37.4% of them overweight. In terms of gender prevalence obesity was higher in females (50.3%) although prevalence of overweight was higher in males (41.0%) as shown in figure 1.
Figure 1.
Percentage of BMI classification according to gender
According to BMI classification SBP was significantly higher in obese males and females, and DBP was only higher in obese females (p<0.05). In the evaluation of BMIs for lipid profile HDL-C in normal males, TC in normal females was found to be lower than in other BMI groups (table 2).
Table 2.
Differences in BP and blood lipid level according to BMI classification
| BMI Classification | ||||
| Normal Mean ±SD |
Overweight Mean ±SD |
Obese Mean ±SD |
p | |
| Males | ||||
| SBP (mmHg) | 141.7±12.8a | 148.6±18.4b | 150.1±17.5b | 0.004* |
| DBP (mmHg) | 89.2±7.7 | 91.5±11.0 | 92.7±11.0 | 0.094 |
| TC (mg/dL) | 196.7±53.2 | 202.9±41.0 | 202.8±47.3 | 0.631 |
| HDL-C (mg/dL) | 46.6±10.7a | 40.9±12.8b | 38.8±11.6b | <0.001* |
| LDL-C (mg/dL) | 118.2±31.5 | 128.5±42.9 | 138.3±73.4 | 0.081 |
| TG (mg/dL) | 152.9±52.6a | 190.2±92.1b | 203.4±149.4b | 0.021* |
| Females | ||||
| SBP (mmHg) | 143.8±12.6a | 147.3±15.1a | 153.6±17.2b | <0.001* |
| DBP (mmHg) | 87.1±7.1a | 89.8±8.4a | 3.3±10.0b | <0.001* |
| TC (mg/dL) | 213.1±42.3a | 214.3±42.7b | 230.7±53.6b | 0.048* |
| HDL-C (mg/dL) | 43.8±10.1 | 44.1±11.6 | 45.3±12.1 | 0.627 |
| LDL-C (mg/dL) | 135.9±36.1 | 136.7±39.2 | 141.1±57.4 | 0.713 |
| TG (mg/dL) | 170.0±46.8 | 183.4±64.0 | 178.6±89.9 | 0.617 |
| Total | ||||
| SBP (mmHg) | 142.6±12.7a | 148.0±16.9b | 152.2±17.4c | <0.001* |
| DBP (mmHg) | 88.3±7.5a | 90.7±9.9a | 93.1±10.4b | <0.001* |
| TC (mg/dL) | 210.8±55.7 | 208.5±42.1 | 209.0±44.5 | 0.902 |
| HDL-C (mg/dL) | 45.5±10.5 | 42.5±12.3 | 42.7±12.3 | 0.071 |
| LDL-C (mg/dL) | 125.7±34.5a | 132.6±41.2b | 140.1±63.8b | 0.047* |
| TG(mg/dL) | 160.1±50.7a | 186.8±79.0b | 188.0±116.4b | 0.028* |
SBP: Systolic blood pressure, DBP: diastolic blood, TC: Total cholesterol, HDL-C: High density lipoprotein-cholesterol, LDL-C: Low density lipoprotein-cholesterol, TG: Triglyceride
p<0.05 according to BMI classification
Values bearing different superscript (a,b)represent statistically significiant p<0.05
Values bearing same superscript (a,a)represent statistically not significiant p>0.05
Age and WC in particular were the most related factors for SBP and DBP in both genders (p<0.05). In addition, LDL-C was found to be positively associated with SBP in males and DBP in females and only in males HDL-C level was found to be negatively associated SBP with (p<0.05) (table 3).
Table 3.
Standardized regression coefficient â, Standard error and p-values from the Multiple linear Regression Model in male and female
| Male | Female | |||||
| B | SE | p | B | SE | p | |
| Systolic blood pressure# | ||||||
| Age (year) | 0.367 | 0.083 | <0.001* | 0.320 | 0.079 | <0.001* |
| TC (mg/dL) | 0.012 | 0.028 | 0.658 | 0.017 | 0.024 | 0.468 |
| HDL-C (mg/dL) | −0.208 | 0.084 | 0.014* | −0.075 | 0.079 | 0.343 |
| LDL-C (mg/dL) | 0.059 | 0.022 | 0.008* | −0.011 | 0.020 | 0.571 |
| TG (mg/dL) | 0.015 | 0.010 | 0.163 | −0.010 | 0.014 | 0.454 |
| WC (cm) | 0.072 | 0.083 | 0.010* | 0.225 | 0.096 | 0.020* |
| HC (cm) | 0.093 | 0.119 | 0.438 | 0.015 | 0.078 | 0.844 |
| BMI (kg/m2) | 0.107 | 0.196 | 0.586 | −0.094 | 0.176 | 0.592 |
| Diastolic blood pressure## | ||||||
| Age (year) | −0.263 | 0.053 | <0.001* | −0.117 | 0.047 | 0.013* |
| TC (mg/dL) | 0.002 | 0.018 | 0.917 | 0.004 | 0.014 | 0.789 |
| HDL-C (mg/dL) | −0.073 | 0.054 | 0.180 | 0.067 | 0.046 | 0.144 |
| LDL-C (mg/dL) | −0.025 | 0.014 | 0.078 | 0.026 | 0.012 | 0.029* |
| TG (mg/dL) | −0.005 | 0.007 | 0.441 | 0.000 | 0.008 | 0.991 |
| WC (cm) | 0.145 | 0.053 | 0.007* | 0.192 | 0.044 | <0.001* |
| HC (cm) | −0.071 | 0.077 | 0.355 | −0.050 | 0.056 | 0.378 |
| BMI (kg/m2) | −0.149 | 0.126 | 0.238 | 0.042 | 0.103 | 0.684 |
TC: Total cholesterol, HDL-C: High density lipoprotein-cholesterol, LDL-C: Low density lipoprotein-cholesterol, TG: Triglyceride, WC: Waist circumference, HC: Hip circumference, BMI: Body mass index
Systolic blood pressure Male R2:0.292; Female R2:0.259
Diastolic blood pressure Male R2:0.247; Female R2:0.272, *p<0.05
Discussion
There is much evidence showing that being overweight and having hypertension are positively associated in developed countries14–16 but only a few published data analysing the relationship betweenbeing overweight and hypertension17–19 are available in developing countries, which have relatively lower overweight rates. We aimed to determine the overweight/obesity and hiperlipidemia status in a group of hypertensive adults in this study.
Generally the studies data indicated that age has a positive correlation with BP14,15,20. Park et al.20 found that there was a significant difference in hypertension prevalence between the age groups: hypertension prevalence rates of 19–29-year-old and 30–49-year-old groups were 3% and 14.6%, respectively (p<0.001). In another study, the prevalence rate of hypertension between 25 and 64 years of age was 18.9 % and between 45 and 64 years it was 33.5 % 15. Similarly, in this study, age was found to be positively related with SBP and DBP (p<0.05).
Cross-sectional and prospective epidemiological studies have shown that BP and hypertension risk increase significantly with higher BMI5,7,21–23. The relation between BP and BMI is explained by an increase in body weight and thus BMI is related to increases in body fluid volume, peripheral resistance, and cardiac output23. Individuals with a BMI of 24 kg/m2 or more showed an increase in both SBP and DBP20. A study done in the United States has shown that the risk of hypertension increases by 12% for an increase of 1 kg/m2 in BMI24. In our study, the mean BMI of hypertensive males was 26.0±5.9 kg/m2 and that of females was 28.1±6.4 kg/m2
In this study, we classified obesity according to BMI and we found that SBP of overweight and obese males was higher than for normal-weight males, but only obese females' SBP and DBP were higher than that of normal-weight groups (p<0.05). In both genders SBP and DBP of obese people were significantly higher than for other groups. It was seen that, although the hypertensive adults in this study had antihypertensive medical therapy, their BP tends to increase with an increase of their body weight.
It is known that weight loss moderates activation of the renin-angiotensin-aldosterone axis and the sympathetic nervous system and diminishes sodium retention. Decreases in abdominal visceral fat also improve the functioning of both conduction and resistance of vessels25. The long-term effect of weight control has demonstrated elsewhere that weight reduction could lower the odds of hypertension by 77%26 This is a very important point for our subjects: with the help of a weight-reducing diet , BP would be lower and therefore better than it is now.
Compared with BMI, WC and WHR are good indicators for body fatness in adults at the population level and provide additional information about central fat distribution23,27,28. Men whose WC increased >6 cm had an odds ratio of 1.22 of becoming hypertensive compared with those whose waists decreased7. A follow-up study using casual BP measurement reported that among males with WC-102 cm the odds ratio for hypertension was approximately three times that of males with waist circumference <94 cm and females with WC-88 cm have a risk of hypertension twice that of females with WC<80 cm8. In this study hypertensive females had higher mean WC than risk level, but in males mean WC was at border level. In addition to this, both gender WC were found to be related with both SBP and DBP
Tuan et al.23 studied on 7,336 Chinese adults aged 18 to 65 years in the 2004 China Health and Nutrition Survey and found that the prevalence of hypertension (17% and 23% for women and men, respectively) was significantly and positively related to increased BMI, WC, and WHR (p for trend < 0.001) 23. Similarly, in another study it was found that weight, BMI, and WC were significantly different between normal and hypertensive groups; the hypertensive group had higher weight, BMI, and WC than the normal group (p<0.001) 20. In the present study, in both genders WC were found to be related with both SBP and DBP.
There is evidence of a relationship between serum lipids and blood pressure. Furthermore, a combination of hyperlipidaemia and hypertension increased the risk of cardiovascular disease in a potentiating rather than an additive manner14,27. Research has shown that low HDL-C, high LDL-C and high TG levels are positively associated with an increase in BMI14,18,27. Xu et al.27 indicated that there was a significant upward trend for blood pressure, TG, TC, and LDL-C to increase, whereas HDL-C decreases, with increasing BMI and WC adjustment for age. In the same study, for men and women the age-adjusted means of TC, LDL-C, TG, SBP and DBP were higher. In this study, we observed that hypertensive overweight and obese subjects had lower HDL-C levels than normal-weight hypertensive people, but no statistical significance among BMI classes was noted. In the regression analysis model, LDL-C was found to associate with SBP in male and DBP in female positively and HDL-C was found to associate with SBP in males negatively (p<0.05). Similarly to our study, in another study it was found that significantly more non-medicated and medicated hypertensive subjects had higher LDL-cholesterol and lower HDL-cholesterol than normotensive subjects14.
Study limitations
The main limitation of this study is that we were not able to adjust for, e.g., the physical activity level, dietary food intake and socioeconomic status of participants: Further studies therefore need to be conducted on a large population. Additionaly the blood pressure of participants was taken during the interview three times. These measurements might not reflect the changes in the blood pressure during the day.
Conclusion
Central obesity is a stronger correlation factor than BMI for high blood pressure. This study suggests that earlier prevention of excessive weight gain is needed to reduce hypertension in these populationbeneficial effects of lifestyle modification, and this and the ‘Dietary Approaches to Stop Hypertension’ (DASH) diet should be top priorities for health and government officials. Epidemiological studies are needed to indicate the relation between central obesity and hypertension incidence across the country.
Acknowledgement
We would like to thank all the participants who devoted their time to participate in this study. Their helpful and wholehearted cooperation is warmly acknowledged.
References
- 1.Fuchs FD, Gus M, Moreira LB, Moraes RS, Wiehe M, Pereira GM, et al. Anthropometric indices and the incidence of hypertension: a comparative analysis. Obes Res. 2005;13:1515–1517. doi: 10.1038/oby.2005.184. [DOI] [PubMed] [Google Scholar]
- 2.Erem C, Hacihasanoglu A, Kocak M, Deger O, Topbas M. Prevalence of prehypertension and hypertension and associated risk factors among Turkish adults: Trabzon Hypertension Study. J Public Health. 2009;31:47–58. doi: 10.1093/pubmed/fdn078. [DOI] [PubMed] [Google Scholar]
- 3.World Health Report 2002: Reducing risks, promoting health life. Geneva, Switzerland: World Health Organization; http://www.who.int/whr/2002/ [Google Scholar]
- 4.Altun B, Arici M, Nergizoglu G, Derici Ü, Karatan O, Turgan Ç, et al. Prevalance, awareness, treatment, and control of hypertension in Turkey (the PatenT study) in 2003. J Hypertens. 2005;23:1817–1823. doi: 10.1097/01.hjh.0000176789.89505.59. [DOI] [PubMed] [Google Scholar]
- 5.Nyamdorj R, Qiao Q, Söderberg S, Pitkäniemi J, Zimmet P, Shaw J, et al. Comparison of body mass index with waist circumference, waist-tohip ratio, and waist-to-stature ratio as a predictor of hypertension incidence in Mauritius. Journal of Hypertension. 2008;26(5):866–870. doi: 10.1097/HJH.0b013e3282f624b7. [DOI] [PubMed] [Google Scholar]
- 6.Dalton M, Cameron AJ, Zimmet PZ, et al. Waist circumference, waist-hip ratio and body mass index and their correlation with cardiovascular disease risk factors in Australian adults. J Intern Med. 2003;254:555–563. doi: 10.1111/j.1365-2796.2003.01229.x. [DOI] [PubMed] [Google Scholar]
- 7.Williams PT. Increases in Weight and Body Size Increase the Odds for Hypertension During 7 Years of Follow-up. Obesity. 2008;16:2541–2548. doi: 10.1038/oby.2008.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guagnano MT, Ballone E, Colagrande V, Della Vecchia R, Manigrasso MR, Merlitti D, et al. Large waist circumference and risk of hypertension. International Journal of obesity. 2001;25:1360–1364. doi: 10.1038/sj.ijo.0801722. [DOI] [PubMed] [Google Scholar]
- 9.Lepira FB, M'Buyamba-Kabangu JR, Kayembe KP, Nseka MN. Correlates of serum lipids and lipoproteins in Congolese patients with arterial hypertension. Cardiovasc J S Afr. 2005;16(5):249–255. [PubMed] [Google Scholar]
- 10.Friedewald WT, Levy RI, Fedickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 11.Chobanian AV, Bakris GL, Black HR, William C, Cushman LA, Green JL, et al. National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. WHO/FAO. Diet, Nutrition and the Prevention of Chronic Diseases, WHO Technical Report Series, 916, Geneva, 2003. [DOI] [PubMed] [Google Scholar]
- 12.WHO/FAO, author. Diet, Nutrition and the Prevention of Chronic Diseases. Geneva: 2003. WHO Technical Report Series, 916. [Google Scholar]
- 13.Lohman TG, Roche AF, Martorell R. Anthropometric Standardization Reference Manual. Champaign, Illinois: Kinetics Books; 1988. pp. 1–12. [Google Scholar]
- 14.Schröder H, Schmelz E, Marrugat J. Relationship between diet and blood pressure in a representative Mediterranean population. Eur J Nutr. 2002;41:161–167. doi: 10.1007/s00394-002-0372-4. [DOI] [PubMed] [Google Scholar]
- 15.Beegom R, Beegom R, Niaz MA, Singh RB. Diet, central obesity and prevalence of hypertension in the urban population of south India. Int J Cardiol. 1995;51:183–191. doi: 10.1016/0167-5273(95)02402-i. [DOI] [PubMed] [Google Scholar]
- 16.Dinç G, Saatli G, Baydur H, Özcan C. Hypertension and overweight among Turkish adolescents in a city in Aegean region of Turkey: a strong relationship in a population with a relatively low prevalence of overweight-Original Investigation. Anadolu Kardiyol Derg. 2009;9:450–456. [PubMed] [Google Scholar]
- 17.Doll S, Paccaud F, Bovet P, Burnier M, Wietlisbach V. Body mass index, abdominal adiposity and blood pressure: consistency of their association across developing and developed countries. Int J Obes Relat Metab Disord. 2002;26:48–57. doi: 10.1038/sj.ijo.0801854. [DOI] [PubMed] [Google Scholar]
- 18.Adedoyin RA, Mbada CE, Bisiriyu LA, Adebayo RA, Balogun MO, Akintomide AO. Relationship of anthropometric indicators with blood pressure levels and the risk of hypertension in Nigerian adults. Int J Gen Med. 2008;30:133–140. doi: 10.2147/ijgm.s3643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aekplakorn W. Asia Pac J Public Health Online First. Prevalence, Treatment, and Control of Metabolic Risk Factors by BMI Status in Thai Adults: National Health Examination Survey III. [DOI] [PubMed] [Google Scholar]
- 20.Park J, Lee J, Kim J. Relationship between dietary sodium, potassium, and calcium, anthropometric indexes, and blood pressure in young and middle aged Korean adults. Nutr Res Pract. 2010;4:155–162. doi: 10.4162/nrp.2010.4.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dong Z, Zhang XG, Zheng LQ, Sun ZQ, Liu SS, Zhang XZ, et al. Correlation between body mass index, waist circumference and blood pressure in rural residents from west part of Liaoning Province. Zhonghua Xin Xue Guan Bing Za Zhi. 2009;37:369–373. [PubMed] [Google Scholar]
- 22.Liao CC, Su TC, Chien KL, Wang JK, Chiang CC, Lin CC, et al. Elevated Blood Pressure, Obesity, and Hyperlipidemia. J Pediatr. 2009;155:79–83. doi: 10.1016/j.jpeds.2009.01.036. [DOI] [PubMed] [Google Scholar]
- 23.Tuan NT, Adair LS, Stevens J, Popkin BM. Prediction of hypertension by different anthropometric indices in adults: the change in estimate approach. Public Health Nutr. 2010;13:639–646. doi: 10.1017/S1368980009991479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huang Z, Willett WC, Manson JE, Rosner B, Stampfer MJ, Speizer FE, et al. Body weight, weight change, and risk for hypertension in women. Ann Intern Med. 1998;128:81–88. doi: 10.7326/0003-4819-128-2-199801150-00001. [DOI] [PubMed] [Google Scholar]
- 25.Sacks FM, Campos H. Dietary Therapy in Hypertension. N Engl J Med. 2010;3:2102–2112. doi: 10.1056/NEJMct0911013. [DOI] [PubMed] [Google Scholar]
- 26.He J, Whelton PK, Appel LJ, Charleston J, Klag MJ. Long-term effects of weight loss and dietary sodium reduction on incidence of hypertension. Hypertension. 2000;35:544–549. doi: 10.1161/01.hyp.35.2.544. [DOI] [PubMed] [Google Scholar]
- 27.Xu C, Yang X, Zu S, Han S, Zhang Z, Zhu G. Association between Serum Lipids, Blood Pressure, and Simple Anthropometric Measures in an Adult Chinese Population. Arch Med Res. 2008;39:610–617. doi: 10.1016/j.arcmed.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 28.Feldstein CA, Akopian M, Olivieri AO, Kramer AP, Nasi M, Garrido DA. Comparison of body mass index and waist-to-hip ratio as indicators of hypertension risk in an urban Argentine population: A hospital-based study. Nutrition, Metabolism & Cardiovascular Diseases. 2005;15:310–315. doi: 10.1016/j.numecd.2005.03.001. [DOI] [PubMed] [Google Scholar]