Abstract
Adult spinal deformity may occur as the result of a number of conditions and patients may present with a heterogeneous group of symptoms. Multiple etiologies may cause spinal deformity; however, symptoms are associated with progressive and asymmetric degeneration of the spinal elements potentially leading to neural element compression. Symptoms and clinical presentation vary and may be related to progressive deformity, axial back pain, and/or neurologic symptoms. Spinal deformity is becoming more common as adults 55–64 years of age are the fastest growing proportion of the U.S. population. As the percentage of elderly in the United States accelerates, more patients are expected to present with painful spinal conditions, potentially requiring spinal surgery. The decision between operative and nonoperative treatment for adult spinal deformity is based on the severity and type of the patient’s symptoms as well as the magnitude and risk of potential interventions.
Keywords: Spine deformity, Adult, Scoliosis, Kyphosis, Spine surgery, Sagittal imbalance, Osteotomy, Posterior-only surgery, Spine reconstruction
Introduction
Adult spinal deformity is becoming increasingly prevalent in the elderly population. Multiple etiologies may be involved; however, symptoms are associated with progressive and asymmetric degeneration of the discs, facet joints, and other spinal elements potentially leading to neural element compression. Symptoms and clinical presentation vary and may be related to progressive deformity, axial back pain, or neurologic symptoms. Spinal deformity is defined as a curvature in the spine where the alignment is outside of defined normal limits.
Adult spinal deformity may occur as a result of a number of conditions, each of which ultimately lead to an imbalance of the structural support of the spinal column. Abnormal curvature may occur in the sagittal plane (kyphosis, lordosis) causing imbalance to the patient’s front or back or in the coronal plane (scoliosis) causing imbalance to the patient’s right or left side. The magnitude of the curvature of the spine is measured using Cobb angle measurements. Axial plane deformity is measured by degrees of rotation from the frontal or sagittal plane.
Curvatures may be defined as structural or compensatory. Structural curves are defined as rigid inflexible curves, often referred to as major curves. Compensatory curves occur in response to structural curves as the body attempts to maintain postural balance. Compensatory curves, also called minor curves, are usually smaller and flexible on dynamic x-rays. Spinal deformities usually progress and multiple factors may accelerate this process. Patients with preexisting spinal deformity or with weakened vertebra due to osteoporosis or osteopenia are at increased risk for rapid curve progression as these factors decrease the resiliency of the spine and increase the lever arm amplifying the magnitude of the forces across the spine.
Osteoporosis may occur as the result of decreased bone formation with associated continued or accelerated bone resorption leading to relative decrease in overall bone mass. In a more advanced setting, osteoporosis may lead to collapse of the vertebral bodies which may lead to rapid progression of spinal deformity. Increasing magnitude of the spinal deformity leads to increasing stress on the weakened vertebral bodies. This weakening or loss of support of the spine may also play a role in the increased magnitude of the symptoms, related to the spinal deformity. Additionally, paraspinal muscles typically atrophy with age, thus further weakening any secondary dynamic support for the aging spine.
Scheuermann’s disease is a well known cause of thoracic kyphosis that occurs as a result of loss of ventral vertebral body height and narrowing of the disc interspaces. Although the exact etiology is still unknown, spinal deformity along with accelerated disc degeneration and increased intradiscal pressure may lead to progressive spinal deformity and pain.
Nonoperative treatment for adult spinal deformity includes a physical conditioning program, spinal manipulation, pharmacologic agents for symptoms management, the use of orthotics or braces, and more invasive modalities including epidural steroid injections and joint injections. Operative treatment may be contemplated for patients with progressive symptoms despite nonoperative conservative treatment. Surgical treatment options usually include decompression and instrumented stabilization with either an anterior, posterior, or a combined approach. The details of the surgical procedure must be based on the location of the pathology and the symptoms for each specific patient. The incidence of complication is significant and patient comorbidities and risk for complications must be considered when discussing potential for surgical intervention.
In the previous decades most attention was given to treatment of scoliosis during childhood and adolescent years with most surgeons avoiding surgical intervention for adult spinal deformities. Treatment of adult spinal deformity has been associated with increased perioperative morbidity and higher incidence of neurologic deficits. In the past, the risk/benefit ratio has trended toward nonoperative conservative treatment for most surgeons, however; recent advances in surgical technique, instrumentation, neurologic monitoring, as well as improved diagnostic imaging, perioperative anesthesia, and intensive care have led toward increasing utilization of surgical treatment for patients with adult deformity.
Evaluation and diagnosis
Adult spinal deformity is typically studied with standing full length 36″ posterior-anterior, and lateral radiographs and may need to be repeated over time to monitor for curve progression. Cobb angles are measured on these radiographs providing coronal and sagittal alignment and global alignment is measured using plumb line. Dynamic radiographs including flexion-extension views, supine, and prone films also help to assess flexibility of curves and the ability for adjacent segments to compensate. Additional information relating to bony anatomy may be obtained in CT scan, while magnetic resonate imaging of the spine provides additional information about the neural elements, discs and other soft tissues.
Selection of appropriate treatment can be challenging because patients with adult spinal deformity may complain of a heterogeneous group of symptoms. In addition, multiple medical, social, and environmental factors must also be evaluated to determine the best treatment option for each particular patient. Patients with a history of tobacco use, pulmonary, coronary, or vascular disease, diabetes, nutritional deficiencies, osteoporosis, psychiatric disease, or lack of social support have been shown to correlate with increased surgical risk and poor clinical outcomes. When evaluating patients with spinal deformity, it is always important to rule out other potential causes of spinal deformity including traumatic, neuromuscular, or inflammatory etiologies.
Non operative treatment versus operative treatment
Clinical management of patients with adult spinal deformity is becoming increasingly important because of the increasing number of the older patients in our population as well as increased expectations for activity levels and function in these patients. There has been increasing utilization of both nonoperative and operative treatment for patients with adult spinal deformity. The decision between operative and nonoperative treatment for adult spinal deformity may be difficult for surgeons and patients. Decisions are based on multiple issues including progressive deformity, pain, cosmesis, as well as the magnitude of potential intervention. A decision for surgical intervention can be based on clinical symptoms, appearance, pain, functional limitations, and social issues. These are weighed against the potential risks and limitations related to the proposed surgical treatment [1].
Patients with poor general health and increasing risk for surgical treatment are more likely to receive a recommendation for nonoperative management. Patients with increased body mass index (BMI) are also less likely to receive surgical intervention. This may be related to hesitancy on the part of the surgeon to undertake a major reconstruction procedure in an obese patient. This may also be related to the fact that obesity may somewhat hide the clinical appearance of the deformity, therefore diminishing the concern or desire for surgical intervention. Although many patients make their decisions based on their level of pain, some studies have shown similar levels of pain in patients who select nonsurgical and surgical treatment [2]. In one study, Glassman, et al. found that patients with components with radicular leg pain were more likely to proceed with surgical treatment whereas patients with back pain did not show a difference between surgical or nonsurgical treatment. The study also noted that surgical patients were more likely to report a change in their body habitus over the past 10 years or to be dissatisfied with the shape of their spine whereas nonsurgical patients were more likely to report their deformity was stable and did not affect personal relationships [3].
The evidenced-based approach to clinical decision making in medicine has expanded recently. As such, attempts to compare the efficacy of surgical versus nonsurgical treatment for patients with adult spinal deformity have been undertaken. At this point, definitive information regarding differential between the treatments is still not available. At this time few studies have attempted to determine to what extent adult patients are helped with nonoperative and operative treatment for spinal deformity.
The best comparative study at this time was conducted by Bridwell and colleagues who studied patients with adult to scoliosis treated with either nonoperative or operative treatment to determine if treatment improved quality of life at two-year follow-up. In this prospective multicenter evidenced based medicine study [4••], they followed 160 consecutive patients for a period of 2 years after enrollment. At the 2 year follow-up visit, 95% of operative patients and 45% of nonoperative patients were available for follow-up. Quality of life measures including Oswestry Disability Index (ODI) and Scoliosis Research Society (SRS) and numerical back and leg pain scores were followed. The nonoperative patients did not improve during this time period and a non-significant decline in quality of life scores was common. Significant improvement in quality of life measures were noted in the operative group. The authors reported that it appeared that common nonoperative treatment did not change quality of life measures with adult symptomatic lumbar scoliosis at 2 year follow-up. However, their conclusions were limited by the fact that only 45% of the nonoperative group was available at 2 year follow-up despite an extensive effort to locate data for this group. Of note, the demographics for the nonoperative patients who were followed versus those lost to follow-up were identical on initial enrollment into the study.
Non operative treatment
In general, asymptomatic patients with spinal deformities do not require formal treatment although periodic follow-up may be required to monitor for curve progression. Nonsurgical interventions include yoga, physical therapy, chiropractic manipulation and other maintenance routines. However, these treatments have unproven efficacy in patients with adult spinal deformity. Pharmacologic agents may decrease pain and increase quality of life but can be associated with adverse effects. The use of narcotic analgesics must be carefully monitored, especially given the potential need for long term use of the medications. The use of spinal bracing may provide benefit for temporary exacerbation of symptoms; however, long term use has raised concerns for muscle deconditioning/atrophy without any effect on curve progression.
In a recent systematic review of clinical studies evaluating conservative treatment for adult spinal deformity, Everett et al. [1] concluded that “Surgeons are often very conservative in the treatment of adult scoliosis because of increased complication rate and marginal bone quality in this patient population. At present there is currently a lack of consensus on the indications for conservative treatments for adult spinal deformity.” They found that current evidence is indeterminate with level 4 evidence on the role of physical therapy, chiropractic treatment, and bracing and level 3 evidence on the use of injections for treatment of adult deformity.
Surgical treatment
Patients with spinal deformity present with a number of different clinical presentations and surgical strategies encompass a broad range of approaches and options. Patients commonly have symptoms that result from a combination of degenerative spondylosis, progressive deformity, as well as neurologic symptoms. Each surgical intervention must be tailored based on the specific pathology that is symptomatic for each patient. Careful preoperative planning is important to limit the risks of perioperative complications and maximize the chance for long term clinical success. In some cases surgical management of spinal deformity and degenerative disease cannot be accomplished with one single procedure and in some cases long term management of this medical condition may involve the need for multiple surgical treatments [5].
Yadla et al. recently published adult scoliosis surgery outcomes: a systematic review. In this review [6•], they performed a systematic review of 49 articles on patients undergoing adult spinal deformity surgery. Data for 3,299 patients was included and average follow-up was 3.6 years. Average curve correction with surgery was 26.6° (40.7% improvement) and mean total pre-op ODI was 41.2 with average postoperative reduction to 15.7; mean pre-operative SRS-30 equivalent score was 97.1 with mean postoperative decrease of 23.1. There was 897 complications for 2175 patients (41.2%) and 319 pseudoarthroses (12.9%). Despite the lack of randomized prospective date, this review did conclude that surgery for adult scoliosis was associated with improvement in clinical outcomes and radiographic parameters at 2 years follow-up.
Adults 55 to 64 years of age are projected to be a fast growing proportion of the U.S. population over the next 10 years and as the percentage of elderly in the United States accelerates, more patients are expected to present with painful spinal conditions, potentially requiring spinal surgery. Spinal reconstructive surgery in the older age group has been associated with increased complications [7] with some reports indicating nearly two times greater potential for complications than those undergoing surgery without fusion. In addition, increasing age and increasing number of levels fused have been found to be significant risk factors for complications in patients over the age of 65 years [8].
In many cases, treatment of adult spinal deformity requires a multilevel fusion procedure. These patients also commonly require multilevel decompressive procedures for stenosis or complex spinal osteotomies for correction of spinal deformity. Surgical blood loss, surgical time, length of hospital stay, and length of overall recovery are elevated in these patients when compared with more common single level degenerative conditions. Dobbs, et al. presented their series of 46 patients over the age of 60 who underwent thoracic or lumbar arthrodesis of five levels or greater with a mean follow-up of 4.2 years. Average number of levels fused was 9 (range 5–16) and overall complications in this patient population was 37% with a major complication rate of 20%. Increasing age was a significant risk factor, with patients over the age of 69 years having higher complication rates [9]. In their study, clinical outcome at final follow-up was improved with ODI scores changing from 49 to 25 for a mean improvement of 24 (49%, p-value <0.00001). This study demonstrates the increasing complexity and potential for complications in this patient group while also demonstrating significant improvement in patient reported functional outcomes for patients undergoing these procedures [9].
The rate of complications reported by Dobbs is similar to Benz, et.al, who reported an overall complication rate of 40% with serious complication rate of 12% in patients undergoing lumbar decompression over the age of 70 years [10]. In a similar report, Smith et al. performed a retrospective review of a multicenter database identifying incidence of complications and outcome measurements of adult patients undergoing spinal deformity reconstruction surgery [11•]. The study included 206 patients included with minimum 2 year follow-up. Increasing complication rates were noted with increasing age. Patients aged 24–44 years old had 17% complication rate; 45–64 years old had 42% complication rate; and patients 65–85 years had 71% complication rate (p-value <0.00001). When all age groups were examined together, significant improvement in outcome studies were noted including ODI, SRS-22, back pain, and leg pain at 2 year follow-up. Improvement in ODI and leg pain were significantly greater amongst elderly patients with greater improvement in SF12 and SRS-22 when compared to younger patients. This study demonstrates the potential benefit for surgical treatment for adult scoliosis and suggests that despite having greater risk for complications, the elderly may obtain greater improvement in pain and disability with surgical reconstruction.
Blood loss in adult spinal deformity spine surgery
Intraoperative blood loss is an important concern for patients undergoing spinal deformity reconstructive surgery. Increasing blood loss during surgery may lead to the need for whole blood, platelet, and factor transfusions. Although blood screening has improved the safety of these transfusions, potential reactions and infectious risks persist. Large blood loss can lead to increased surgical time and complications associated with multiple blood transfusions including swelling, increased surgical time, pulmonary edema, or shock.
Intraoperative administration of antifibrinolytic agents has gained popularity as a means to manage intraoperative blood loss. The antifibrinolytic agent Aprotinin is a serum protein inhibitor first used to reduce blood loss in major cardiac surgery. Use of Aprotinin in spinal deformity surgery was shown to decrease blood loss. However, more recently its use has become controversial due to the association with significant postoperative complications including renal failure, myocardial infarction, cerebral vascular accident, and death. Other agents including tranexamic acid (TXA) and aminocaproic acid (Amicar) have been utilized to decrease intraoperative blood loss and minimize complications. Tranexamic acid and Amicar have been well tolerated [12].
Recent reports of the use of tranexamic acid and aminocaproic acid have demonstrated that they are safe and effective, potentially reducing not only transfusion related complications but also operative expenses. Elwatidy et al. found the prophylactic use of tranexamic acid led to a 49% reduction of blood loss and 80% reduction of blood transfusion when compared to placebo after cervical and lumbar surgeries with no complications related to the use of TXA [13].
In a recent meta analysis, Elgafy et al. reviewed 90 studies with 17 meeting inclusion criteria. They found a high level of evidence to support the use antifibrinolytic medications to reduced blood loss and limit the need for transfusion during and after adult spine surgery. Based on their review, a recommendation was also made against the use of Amicar in spine surgery due the increased complications. The use of Cell Saver, Recombinant Factor VIIa, activated growth factor platelet gel, and normovolemic hemodilution were all evaluated as methods to prevent blood loss and were found to have very low evidence to support their efficacy [14••].
Biologics in adult spinal deformity surgery
The use of biologic agents to stimulate spine fusion is a major focus in current spinal deformity research. Many surgeons are now trending away from the use of iliac crest bone graft and using a combination of locally harvested autogenous bone and allograft for posterior fusion. Harvesting adequate iliac crest bone graft to achieve fusion is a potentially major limitation, especially for larger multi-level surgeries. The osteoinductive protein rhBMP-2 (Infuse; Medtronic, Spinal and Biologics) has received FDA approval for anterior lumbar interbody fusion and several investigational device exemptions (IDE) and physician directed studies have demonstrated promising outcomes for posterior interbody and posterolateral spine fusion.
Cahill, et. al. published an initial study involving 46 patients who underwent posterolateral lumbar fusion with the use of rhBMP-2. This technique yielded a 95% rate of fusion when compared with 70% fusion rate with iliac crest bone graft [15]. In the same year, Carreon et. al. reviewed the use of rhBMP-2 versus iliac crest bone graft for lumbar spine fusion in patients over 60 years of age. In this randomized clinical trial, patients over 60 years old at the time of the surgery were treated with decompression and posterolateral fusion. Patients were randomized with either iliac crest bone graft or rhBMP-2. Patients treated with iliac crest bone graft had an increased rate of complications and need for additional treatment including the need for revision surgery when compared to rhBMP-2. A lower clinical improvement and higher cost of treatment were seen in patients who received iliac crest bone graft compared with those who received rhBMP-2 for posterolateral lumbar fusion [16].
The use of bone morphogenetic protein may carry the most important benefit for patients undergoing long spinal deformity fusion. One major spinal deformity center published results for patients undergoing long spinal deformity fusion to the sacrum. They report a pseudoarthrosis rate of 28% in patients who received iliac crest bone graft versus only 4% of patients who were treated with rhBMP-2 [17]. In another study, Dimar, et. al. published their results for the use of BMP in 463 patients who underwent scoliosis surgery. Radiographic fusion was achieved in 96% of patients compared to 89% of patients managed with iliac crest bone graft alone [18].
Multiple studies have reviewed the concerns for adverse effects surrounding the use of bone morphogenetic protein. The most commonly reported side effect includes transient radiculitis, vertebral body bone resorption, sterile seroma/fluid collection, and heterotopic bone formation. Many of these local side effects are felt to be related to the dose of BMP. More recent discussion has focused on the use of lower doses of rhBMP-2 in an effort to potentially lower the risk of local side effects. While much focus has remained on the use of the osteoinductive protein, the use of other bone graft substances, such as platelet-rich plasma (PRP) and mesenchymal stem cells for bone healing have been studied. Currently no studies have shown these measures alone are sufficient to achieve spinal fusion.
Posterior-only surgery for adult spinal deformity
Combined anterior/posterior (A/P) fusion has traditionally been used to treat severe adult scoliosis deformities. These combined procedures include an anterior release with fusion which is performed via a thoracotomy or thoracoabdominal approach followed by a posterior spinal instrumentation and fusion. This combined approach has been promoted to provide increased fusion rates and better deformity correction [19–21], however, the anterior thoracoabdominal approach has been shown to cause significant morbidity and complications in the adult patient [22]. Anterior thoracotomy/thoracoabdominal approaches negatively impact pulmonary function, may require additional operative time and anesthesia [2], and have been associated with significant morbidity and complications [23, 24].
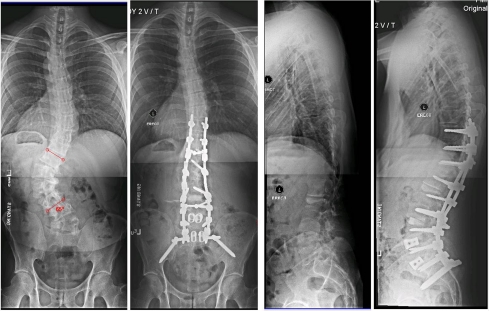
Posterior-only (Post-only) fixation with the use of modern surgical techniques and implants has demonstrated similar correction rates to that of anterior release and posterior fusion in adolescent scoliosis [25]. It has also been shown to have similar deformity correction as combined A/P fusion for the treatment of adolescent idiopathic scoliosis curves more than 90° [26–28]. Post-only surgery with thoracic pedicle screws has also been shown to provide better curve correction in Scheuermann’s kyphosis, with less operating time, less operative blood loss, and fewer complications than circumferential fusion [29]. With the advent of new instrumentation techniques and increasing experience with placing segmental pedicle screws, coupled with multiplanar osteotomies and transforaminal lumbar interbody fusion, our practice has trended away from the use of multilevel anterior surgery for the treatment of adult spinal deformity. In some cases anterior lumbar interbody fusion performed through a small retroperitoneal incision may be utilized to maximize lordosis and interbody fusion at the levels at greatest risk for pseudoarthrosis (Fig. 1). At this point, many adult spinal deformities are treated via an all posterior surgical approach. This includes bilateral implant fixation at nearly all levels, osteotomies, and transforaminal lumbar interbody fusions as needed to correct deformities, and the use of BMP-2 to augment posterior surgical fusions.
Fig. 1.
X-rays of a patient with progressive adult idiopathic scoliosis before and after thoracolumbar reconstruction T10-pelvis. Correction was performed through anterior lumbar interbody fusion L4-Sacrum followed by segmental posterior pedicle screw instrumentation with iliac screw fixation and transforaminal lumbar interbody fusion (TLIF). Post-operative radiographs show significant correction of the deformity with excellent coronal and sagittal imbalance
In a recent series, Posterior-only adult scoliosis surgery was found to avoid the morbidity of a thoracoabdominal approach while achieving similar correction to combined anterior-posterior surgery with decreased blood loss, operative time, and length of stay in the hospital. Complications, radiographic and clinical outcomes were similar at over 2-year follow-up [30•].
Osteotomies in adult spinal deformity
A growing number of studies have compared various osteotomy techniques for correction of coronal and sagittal spinal deformities. The use of multiple posterior column osteotomies, versus three-column osteotomies has been reviewed. While it is clear that greater correction of the deformity is achieved with three column osteotomy (pedicle subtraction osteotomy/vertebral column resection) these techniques are associated with increased complexity, higher complication rate, and greater neurologic risk. The use of multiple single column posterior osteotomy and three column posterior osteotomy has grown, particularly in relation to the surgical treatment of sagittal imbalance where osteotomy has perhaps its greatest importance.
Controversy remains with regard to the impact of thoracolumbar fusion extending up to the upper or lower thoracic spine [31•]. Long term evaluation of the choice of distal fusion level for adult spinal deformity have shown improved long term outcomes favoring an extension of fusion to the sacrum versus stopping at the L5 level for most of the adult population [32]. There are some situations where long deformity fusions ending at L5 are clearly to be avoided which include patients with spondylolisthesis, previous laminectomy, spinal stenosis, or an oblique take-off at the L5/S1 level. Long spinal deformity fusion down to sacrum carries theoretical additional risks and morbidity including prolonged surgical time, higher risk of pseudoarthrosis at L5/S1, greater blood loss, and higher risk of fixation failure. However, including the L5/S1 level at the time of the definitive surgery may alleviate the potential for future breakdown and need for revision surgery.
Complications
The Scoliosis Research Studying Morbidity and Mortality Committee recently analyzed rates of postoperative infection across its members. 108,419 cases were identified with 0.8% of superficial infection and 1.3% rate of deep wound infection. The committee concluded that “post surgical infection, even amongst skilled spine surgeons, is an inherent potential complication.” Higher deep infection rates were noted in patients with degenerative scoliosis and kyphosis.
Postoperative blindness has been noted to complicate long spinal deformity surgery performed with patients in the prone position at approximately 1:1000 (0.1%). This is a potentially devastating complication. Current recommendations to minimize risk include keeping the eyes positioned higher than the rest of the body, maintaining all pressure off the eyes and face, and avoiding prolonged periods of hypotension, and extensive blood loss (Table 1).
Table 1.
Complications of adult spinal deformity surgery with avoidance and management options
| Possible Complication | Management |
|---|---|
| Hemorrhage | Careful preoperative patient positioning |
| Meticulous hemostasis during exposure | |
| Intraoperative blood salvage | |
| Preoperative autologous blood donation | |
| Intraoperative administration of antifibrinolytic agents | |
| Cerebrospinal fluid leak | Careful exposure / decompression |
| Repair primarily if possible | |
| Onlay dural graft material | |
| Fibrin glue derivatives | |
| CSF diversion for continued leak | |
| Screw malposition | Maximize visualization of relevant anatomy |
| Intraoperative use of fluoroscopy / x-ray | |
| Feel pedicle boarders through decompression | |
| Ischemic Optic Neuropathy | Preoperative patient counseling |
| Careful prone positioning (eyes higher than the heart) | |
| Avoid pressure on the face / eyes (Gardner Wells Tongs) | |
| Avoid intraoperative hypotension / anemia | |
| Cardiopulmonary Complications | Preoperative medical optimization |
| Diligent multidisciplinary monitoring and management | |
| Early mobilization after surgery | |
| Pulmonary toilet | |
| Thromboembolic Events | Preoperative medical optimization |
| Removable IVC filter for high risk patients | |
| Mechanical DVT prophylaxis intra and postoperatively | |
| Pharmacological thrombosis prophylaxis for high risk | |
| Early mobilization after surgery | |
| Infection | Preoperative antibiotics |
| Careful skin preparation | |
| Irrigate with antibiotic solution frequently | |
| Postoperative wound drainage | |
| Layered wound closure | |
| Excise damaged muscle tissue | |
| Pseudoarthrosis | Pre-operative behavior modification |
| Nicotine cessation | |
| Osteoporosis management | |
| Meticulous arthrodesis technique | |
| Interbody arthrodesis at lower fusion levels | |
| Consider biologic enhancement of fusion | |
| Avoid anti-inflammatory agents |
Conclusion
Adult spinal deformity may occur as the result of a number of conditions and patients may present with a heterogeneous group of symptoms. Multiple etiologies may cause spinal deformity; however, symptoms are associated with progressive and asymmetric degeneration of the spinal elements potentially leading to neural element compression. Symptoms and clinical presentation vary and may be related to progressive deformity, axial back pain, and/or neurologic symptoms. As the percentage of elderly in the United States accelerates, more patients are expected to present with painful spinal conditions, potentially requiring spinal surgery. The decision between operative and nonoperative treatment for adult spinal deformity is based on the severity and type of the patient’s symptoms as well as the magnitude and risk of potential interventions.
In general, asymptomatic patients with spinal deformities do not require formal treatment although periodic follow-up may be required to monitor for curve progression. Nonsurgical interventions include yoga, physical therapy, chiropractic manipulation and other maintenance routines. However, these treatments have unproven efficacy in patients with adult spinal deformity. Multiple studies have shown that reconstructive surgery for adult scoliosis does lead to improvements in patient quality of life and pain levels. Despite having greater risk for complications, the elderly may obtain the highest levels of improvement in pain and disability with surgical reconstruction.
Disclosures
CR Good: none; JD Auerbach: consultant for Paradigm Spine, Synthes Spine, Medacta, MCRA, LLC; PT O’Leary: none; TC Schuler: none.
Contributor Information
Christopher R. Good, Phone: +1-703-7091114, FAX: +1-703-7091117, Email: crgood@SpineMD.com, www.spineMD.com
Joshua D. Auerbach, Phone: +1-718-5185814, FAX: +1-718-4668168
Patrick T. O’Leary, Phone: +1-309-6911400
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Everett CR, Patel RK. A systematic review of nonsurgical treatment in adult scoliosis. Spine. 2007;32(19 Suppl):S130–S134. doi: 10.1097/BRS.0b013e318134ea88. [DOI] [PubMed] [Google Scholar]
- 2.Glassman SD, Berven S, Kostuik J, et al. Nonsurgical resource utilization in adult spinal deformity. Spine. 2006;31:941–947. doi: 10.1097/01.brs.0000209318.32148.8b. [DOI] [PubMed] [Google Scholar]
- 3.Glassman SD, Schwab FJ, Bridwell KH, et al. The selection of operative versus nonoperative treatment in patients with adult scoliosis. Spine. 2007;32:93–97. doi: 10.1097/01.brs.0000251022.18847.77. [DOI] [PubMed] [Google Scholar]
- 4.Bridwell KH, Glassman S, Horton W, et al. Does treatment (nonoperative and operative) improve the two-year quality of life in patients with adult symptomatic lumbar scoliosis: a prospective multicenter evidence-based medicine study. Spine. 2009;34(20):2171–2178. doi: 10.1097/BRS.0b013e3181a8fdc8. [DOI] [PubMed] [Google Scholar]
- 5.Baron EM, Berven SH, Bridwell KH, et al. Adult spinal deformity focus issue: summary statement. Spine. 2006;31(19):S202. doi: 10.1097/01.brs.0000233228.87606.e5. [DOI] [Google Scholar]
- 6.Ylada S, Maltenfort MG, Ratliff JK, et al. Adult scoliosis surgery outcomes: a systematic review. Neurosurg Focus. 2010;28(3):E3. doi: 10.3171/2009.12.FOCUS09254. [DOI] [PubMed] [Google Scholar]
- 7.Deyo RA, Cherkin DC, Loeser, et al. Morbidity and mortality in association with operations on the lumbar spine: the influence of age diagnosis and procedure. J Bone Surg Am. 1992;74:536–543. [PubMed] [Google Scholar]
- 8.Carreon LY, Puno RM, Dimar JR, et al. Perioperative complications of posterior lumbar decompression and arthrodesis in older patients. J Bone Surg Am. 2003;85:2089–2092. doi: 10.2106/00004623-200311000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Dobbs MD, Lenke LG, Cheh G, et al. Adult spinal deformity surgery: complications and outcomes in patients over age 60. Spine. 2007;32(20):2238–2244. doi: 10.1097/BRS.0b013e31814cf24a. [DOI] [PubMed] [Google Scholar]
- 10.Benz RJ, Ibrahim ZK, Afshar P, et al. Predicting complications in elderly patients undergoing lumbar decompression. Clin Orthop. 2001;384:116–121. doi: 10.1097/00003086-200103000-00014. [DOI] [PubMed] [Google Scholar]
- 11.Smith JS, Shaffrey CI, Glassman SD, et al. Risk-benefit analysis assessment of surgery for adult scoliosis: an analysis based on patient age. Spine. 2011;36(10):817–824. doi: 10.1097/BRS.0b013e3181e21783. [DOI] [PubMed] [Google Scholar]
- 12.Urban MK, Beckman J, Gordon M, et al. The efficacy of antifibrinolytics in reduction of blood loss during complex adult reconstructive spine surgery. Spine. 2001;26:1152–1157. doi: 10.1097/00007632-200105150-00012. [DOI] [PubMed] [Google Scholar]
- 13.Elwatidy S, Jamjoom Z, Elgamal E, et al. Efficacy and safety of prophylactic large doses of tranexamic acid in spine surgery. Spine. 2008;33(24):2577–2580. doi: 10.1097/BRS.0b013e318188b9c5. [DOI] [PubMed] [Google Scholar]
- 14.Elgafy H, Bransford RJ, McGuire RJ, et al. Are there effective measures to decrease massive hemorrhage in major spine fusion surgery? Spine. 2010;35(95):S47–S56. doi: 10.1097/BRS.0b013e3181d833f6. [DOI] [PubMed] [Google Scholar]
- 15.Cahill KS, Chi JH, Day A, et al. Prevalance, complications, and hospital charges associated with use of bone-morphogenetic protein in spinal fusion procedures. JAMA. 2009;302:58–66. doi: 10.1001/jama.2009.956. [DOI] [PubMed] [Google Scholar]
- 16.Carreon LY, Glassman SD, Djurasovic M, et al. RhBMP-2 versus iliac crest bone graft for lumbar spine fusion in patients over 60 years of age: a cost utility study. Spine. 2009;34(3):238–243. doi: 10.1097/BRS.0b013e31818ffabe. [DOI] [PubMed] [Google Scholar]
- 17.Maeda T, Buchowski JM, Kim YJ, et al. Long adult spinal deformity fusion to the sacrum using rhBMP-2 versus autogenous iliac crest bone graft. Spine. 2009;34:2205–2212. doi: 10.1097/BRS.0b013e3181b0485c. [DOI] [PubMed] [Google Scholar]
- 18.Dimar JR, Glassman SD, Burkus JK, et al. Clinical and radiographic analysis of an optimized rhBMP-2 formulation as an autograft replacement in posterolateral lumbr spine arthrodesis. JBJS. 2009;91:1377–1386. doi: 10.2106/JBJS.H.00200. [DOI] [PubMed] [Google Scholar]
- 19.Bradford DS, Tay BK, Hu SS. Adult scoliosis: surgical indications, operative management, complications, and outcomes. Spine. 1999;24:2617–2629. doi: 10.1097/00007632-199912150-00009. [DOI] [PubMed] [Google Scholar]
- 20.Byrd JA, III, Scoles PV, Winter RB, et al. Adult idiopathic scoliosis treated by anterior and posterior spinal fusion. J Bone Joint Surg Am. 1987;69:843–850. [PubMed] [Google Scholar]
- 21.Dick J, Boachie-Adjei O, Wilson M. One-stage versus two-stage anterior and posterior spinal reconstruction in adults. Comparison of outcomes including nutritional status, complication rates, hospital costs, and other factors. Spine. 1992;17:S310–S316. doi: 10.1097/00007632-199208001-00017. [DOI] [PubMed] [Google Scholar]
- 22.Horton WC, Bridwell KH, Glassman SD, et al. The morbidity of anterior exposure for spinal deformity in adults: an analysis of patient-based outcomes and complications in 112 consecutive cases. Paper 32, Presented at the Scoliosis Research Society 40th Annual Meeting, Miami, FL, October 2005.
- 23.Lapp MA, Bridwell KH, Lenke LG, et al. Long-term complications in adult spinal deformity patients having combined surgery a comparison of primary to revision patients. Spine. 2001;26:973–983. doi: 10.1097/00007632-200104150-00025. [DOI] [PubMed] [Google Scholar]
- 24.Newton PO, Faro FD, Gollogly S, et al. Results of preoperative pulmonary function testing of adolescents with idiopathic scoliosis. A study of six hundred and thirty-one patients. J Bone Joint Surg Am. 2005;87:1937–1946. doi: 10.2106/JBJS.D.02209. [DOI] [PubMed] [Google Scholar]
- 25.Luhmann SJ, Lenke LG, Kim YJ, et al. Thoracic adolescent idiopathic scoliosis curves between 70° and 100°: is anterior release necessary? Spine. 2005;30:2061–2067. doi: 10.1097/01.brs.0000179299.78791.96. [DOI] [PubMed] [Google Scholar]
- 26.Dobbs MB, Lenke LG, Kim YJ, et al. Anterior/posterior spinal instrumentation versus posterior instrumentation alone for the treatment of adolescent idiopathic scoliotic curves more than 90 degrees. Spine. 2006;31:2386–2391. doi: 10.1097/01.brs.0000238965.81013.c5. [DOI] [PubMed] [Google Scholar]
- 27.Schwab F, Lafage V, Farcy JP, et al. Surgical rates and operative outcome analysis in thoracolumbar and lumbar major adult scoliosis: application of the new adult deformity classification. Spine. 2007;32:2723–2730. doi: 10.1097/BRS.0b013e31815a58f2. [DOI] [PubMed] [Google Scholar]
- 28.Watanabe K, Lenke LG, Bridwell KH, et al. Comparison of radiographic outcomes for the treatment of scoliotic curves greater than 100 degrees: wires versus hooks versus screws. Spine. 2008;33:1084–1092. doi: 10.1097/BRS.0b013e31816f5f3a. [DOI] [PubMed] [Google Scholar]
- 29.Lee SS, Lenke LG, Kuklo TR, et al. Comparison of Scheuermann kyphosis correction by posterior-only thoracic pedicle screw fixation versus combined anterior/posterior fusion. Spine. 2006;31:2316–2321. doi: 10.1097/01.brs.0000238977.36165.b8. [DOI] [PubMed] [Google Scholar]
- 30.Good CR, Lenke LG, O’Leary PT, Pichelmann M, Keeler KA, Bridwell KH, Baldus C, Koester L. Can posterior only surgery replace combined anterior (thoracotomy/thoracoabdominal) /posterior approaches for adult scoliosis? Spine. 2010;35(2):210–218. doi: 10.1097/BRS.0b013e3181c91163. [DOI] [PubMed] [Google Scholar]
- 31.O’Leary PT, Bridwell KH, Good CR, Lenke LG, Buchowski JM, Kim YJ, Flynn J. Risk factors and outcomes for catastrophic failures at the top of long pedicle screw constructs (FPSC): a matched cohort analysis performed at a single center. Spine. 2009;34(20):2134–2139. doi: 10.1097/BRS.0b013e3181b2e17e. [DOI] [PubMed] [Google Scholar]
- 32.Bridwell KH, Anderson PA, Boden SD, et al. Specialty update: what’s new in spine surgery. JBJS. 2010;92:2017–2028. doi: 10.2106/JBJS.J.00434. [DOI] [PubMed] [Google Scholar]